Abstract
Purpose
Most cytotoxic drugs are dosed using body surface area (BSA), yet not all cancer patients receive the full BSA-determined dose. Prior work suggests that breast cancer patients who are obese are more likely to experience dose reduction than normal weight patients. However, the factors driving dose reduction remain unclear.
Methods
In 452 women diagnosed with stage I-IIIA primary breast cancer at Kaiser Permanente Northern California, we evaluated the association between obesity and dose reduction, and further explored other factors in relation to dose reduction, including various sociodemographic characteristics, tumor characteristics, and comorbidities. Study participants were a part of the Pathways Study, diagnosed between 2006 and 2013 and treated with cyclophosphamide + doxorubicin, followed by paclitaxel (ACT). Dose reduction was assessed using first cycle dose proportion (FCDP) and average relative dose intensity (ARDI), a metric of dose intensity over the course of chemotherapy.
Results
Overall, 8% of participants received a FCDP < 90% and 21.2% had an ARDI < 90%, with dose reduction increasing with body mass index. In adjusted logistic regression models, obese women had 4.1-fold higher odds of receiving an ARDI < 90% than normal weight women (95% CI: 1.9–8.9; p-trend = 0.0006). Increasing age was positively associated with an ADRI < 90%, as was the presence of comorbidity. Dose reduction was less common in later calendar years.
Conclusion
Results offer insight on factors associated with chemotherapy dosing for a common breast cancer regimen. Larger studies are required to evaluate relevance to other regimens, and further work will be needed to determine whether dose reductions impact outcomes in obese women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Most chemotherapy is dosed according to body surface area (BSA), and therefore obese women are expected to receive a higher absolute dose than their normal weight counterparts. However, due to concerns regarding possible chemotherapy-associated toxicities and other considerations, it has been shown that some clinicians scale back the dose administered to obese women [1,2,3,4,5,6,7]. For example, a 2005 study among 9,672 women receiving care from oncology centers across the United States reported that 20% of women with class I obesity (body mass index (BMI) 30-34.9 kg/m2) and 37% of women with class II or greater obesity (BMI ≥ 35 kg/m2) received less than 90% of their expected BSA-determined dose of cytotoxic drugs cyclophosphamide and doxorubicin in the first cycle of breast cancer treatment, while 9% of normal-weight women were comparably dose reduced [1]. Given this issue, in 2012, the American Society of Clinical Oncology (ASCO) released guidelines stating that obese patients should be given the full BSA determined dose [8].
Research also suggests that older age, Black race, low neighborhood education, and presence of serious comorbidities may be associated with chemotherapy dose reduction; however, obesity appears to remain a strong independent predictor [1, 2, 6, 9,10,11]. However, prior studies have examined a narrow set of potential predictors and it is unknown what other factors may drive dose reductions. Understanding the factors driving dose reduction is an important step to understanding the implications on patient outcomes.
The objective of this study is to understand if the association between obesity and dose-reduction persists in an integrated healthcare delivery system, focusing on patients treated with a common chemotherapy regimen, ACT (cyclophosphamide + doxorubicin, followed by paclitaxel), both overall and by individual drug. In addition to exploring the association between obesity and dose-reduction, we also explore other potential drivers of dose reduction, such as age, stage, race/ethnicity, and comorbidities, both in the first cycle and across the course of chemotherapy.
Methods
Study population
Participants were drawn from the Pathways Study, which has been detailed previously [12,13,14]. Briefly, the Pathways Study is a prospective cohort of 4,505 women with stage I-IV breast cancer diagnosed and treated at Kaiser Permanente Northern California (KPNC) between 2006 and 2013. Eligibility criteria for the Pathways Study included the following: KPNC health plan membership at time of study enrollment, 21 + years of age at diagnosis, and having a first primary invasive breast cancer with no prior history of cancer (except non-melanoma skin cancer). Participants had to speak English, Spanish, Cantonese, or Mandarin and reside within a 65-mile radius of a field interviewer. Passive consent was obtained from the patient’s physician of record to contact the patient for study recruitment. Written informed consent was obtained from all participants. The study was approved by the institutional review boards of Kaiser Permanente Northern California and collaborating institutions. For the analyses presented, additional IRB approval was obtained at the Harvard T.H. Chan School of Public Health and Memorial Sloan Kettering Cancer Center.
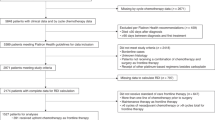
We restricted this analysis to 539 women with stages I-IIIA breast cancer who received the common drug combination, ACT (cyclophosphamide + doxorubicin, followed by paclitaxel). In these analyses, we excluded those who received more than the 4 cycles of cyclophosphamide + doxorubicin, AC, expected per guidelines (n = 6), those who were known to be on a clinical trial or received primary systemic (neoadjuvant) chemotherapy (n = 54), those who were underweight (BMI < 18.5 kg/m2, n = 12), and those whose intended regimens could not be determined (n = 15), resulting in 452 patients for analysis.
Exposures: obesity and other factors
The primary exposure of interest was BMI (kg/m2) at diagnosis (defined as within 6 months prior to 2 months after diagnosis), categorized as normal weight (BMI: 18.5-<25), overweight (BMI: 25-<30), obese (BMI: 30-<35), or severely obese (BMI: 35+).
We also explored sociodemographic factors in relation to dose reduction, including age at diagnosis (categorical: <50y (reference category, ref), 50-<65y, 65y+), year of diagnosis (categorical: 2006–2009 (ref), 2010–2013), race/ethnicity (categorical: non-Hispanic White (ref), non-Hispanic Black, Hispanic, other), household income (categorical: <$50,000 (ref), $50,000-<$90,000, $90,000+), and marital status (married/living with partner (ref) vs. single/divorced/widowed). For race/ethnicity, the ‘other’ group included Asians (n = 66), Pacific Islanders (n = 2), and American Indian and Alaskan Natives (n = 17), as we were not able to present these groups individually, given small numbers. Using a combination of automated, abstracted, and registry data, we also examined disease and clinical factors, including American Joint Committee on Cancer (AJCC) stage (categorical: I (ref), II, IIIA), menopausal status around diagnosis (pre/peri-menopausal (ref) vs. post-menopausal), and several comorbid conditions, including: pre-existing diabetes, cardiovascular disease, neuropathy, renal/liver disease, and neutropenia/ thrombocytopenia (all examined as binary variables, with ‘no’ as the referent group). Renal and liver disease were combined due to small numbers, as were neutropenia and thrombocytopenia. We also examined presence of any of the above comorbidities (none (ref) vs. any) and the Charlson Comorbidity Index (0 (ref) vs. 1+). Last, we examined the impact of white blood cell (WBC) count prior to the first chemotherapy administration, defined as low (< 10 × 103 µL, ref) vs. high (≥ 10 × 103µL).
Dose reduction: overview
Dose reduction was examined in two ways: (1) first cycle dose proportion (FCDP), reflecting dosing in the first cycle (an indication of intended treatment dose), and (2) average relative dose intensity (ARDI), reflecting dosing over the entire regimen. The FCDP differs from the ARDI in that it generally reflects clinician intent [1] without being affected by subsequent toxicity and treatment delays.
Determination of intended regimen
Calculation of the FCDP and ARDI required comparison of chemotherapy received to that expected for a given intended regimen. Although it is relatively straightforward to extract information on the chemotherapy received (dates and dosages) from automated sources, determination of the intended regimen is more challenging, as it may not be readily available and/or available at the specificity needed to determine the intended regimen. We therefore developed a 3-step process to determine the intended regimen. First, among the women receiving ACT, we used strict criteria to classify participants into one of the standard NCCN-defined regimens in which this combination of drugs may be received (e.g., dose-dense AC at 14-day intervals, followed by 12 cycles of weekly paclitaxel vs. dose-dense AC at 14-day intervals, followed by 4 cycles of paclitaxel every 2 weeks). We then manually reviewed the automated electronic chemotherapy administration data of those patients for whom the observed chemotherapy administration did not readily fit one of these expected standard regimens (e.g., by dose, number of cycles, or cycle interval). Finally, when intended regimens were still unclear after manual review, we abstracted clinician notes from medical charts where possible.
Outcome: first cycle dose proportion (FCDP)
To calculate the FCDP, the observed dose was divided by the expected dose based on BSA. The expected dose was calculated by multiplying a woman’s BSA (m2) – a function of weight and height calculated using the Mosteller formula [15] – by the recommended dose (mg/m2) [8, 16]. For example, if the recommended dose of cyclophosphamide is 600 mg/m2, a participant with a BSA of 2m2 would be expected to receive 2 × 600 = 1200 mg of cyclophosphamide. If she received 900 mg, then she received 900/1200 = 75% of the expected dose. The value for each drug received in the first cycle was then averaged to yield the FCDP. For FCDP, the outcome was defined by receipt of < 90% of the expected dose in the first cycle of chemotherapy (as compared to receipt of ≥ 90% of expected dose). A threshold of 90% was selected as a balance of reflecting substantive dose reduction and power to detect association in the context of a small study [1].
Outcome: average relative dose intensity (ARDI)
Calculation of the RDI, a standard measure of chemotherapy dosing [1, 9, 10, 17], requires knowledge of the doses and intervals at which each drug was received (numerator), as well as the planned or expected doses and intervals (denominator). To calculate the dose intensity received over the course of therapy, we calculated the RDI for each drug received, as shown below:
The RDI for each drug received was calculated and then averaged across drugs to obtain the ARDI. The ARDI received over the course of therapy represents the average relative dose intensity across all cycles, averaged for each drug received. Dose reduction was defined by an ARDI < 90%.1
Participants who discontinued therapy early contributed data for both the numerator and denominator in RDI calculation only for the cycles completed, so as not to obscure intentional dose by early treatment discontinuation. For example, if someone discontinued chemotherapy after 2 cycles of AC, then the numerator and denominator would both account for 2 cycles. Notably, by including information on observed and planned treatment duration, the RDI/ARDI inherently account for treatment delays.
Statistical analysis
Logistic regression was used to calculate odds ratios (ORs) and 95% confidence intervals (95% CIs) for the associations between exposures of interest (primarily obesity, but also other patient/clinical factors) and the two dose reduction measures described above (FCDP and ARDI). Those missing information on a given exposure of interest were excluded from OR calculations for that particular exposure using a complete case approach.
Due to the limited number of women with dose reductions in the first cycle, we were unable to examine adjusted effect estimates for the FCDP and thus results for this outcome are unadjusted. However, more people were defined as dose reduced when using the ARDI, for this outcome, we were able to additionally present estimates adjusted for a set of a priori-selected covariates, including age at diagnosis, race/ethnicity, BMI, and initial WBC count.
All statistical analyses were conducted using SAS version 9.4 (Cary, NC).
Results
In this study of 452 breast cancer patients who received ACT, 156 (34.5%) were < 50 years of age and 17% were ages 65–76 years or older (Table 1). 60% were non-Hispanic White, and 71% had stage II cancer. Patients that were non-Hispanic black comprised 4.7% of the normal weight group, as compared to 30.1% of the severely obese women. Of the women who were normal weight, 18.2% had a household income <$50,000, as compared to 30.1% of severely obese women.
In this study, the FCDP ranged from 0.77 to 1.07, and the ARDI ranged from 0.51 to 1.05. Here, 21.9% of severely obese women had a FCDP of < 90%, as compared to 11.4% of obese women, and 7% of overweight women; there were no women with FCDP < 90% in the normal weight group (Table 2). Across all cycles, 38.4% of severely obese women had an ARDI < 90%, compared to 23.9% of obese women, 19.6% of overweight women, and 12.8% of normal weight women.
When examined by individual drug, there were similar patterns of dose reductions by BMI, both for the first cycle and across all cycles. For example, for the first cycle of doxorubicin, none of the normal weight women received < 90% of the expected dose, compared to 20.6% of severely obese women. Similarly, in the first cycle of cyclophosphamide, none of the normal weight women received < 90% of the expected dose, compared to 21.9% of severely obese women. For paclitaxel, 1.4% of normal weight women received < 90% of the expected dose in the first cycle, compared to 23.3% of severely obese women.
Main results: first cycle dose reduction
BMI was strongly associated with first cycle dose reduction. Given that none of the women with a BMI in the normal weight range had a FCDP < 90%, a meaningful OR cannot be calculated. However, the large differences in groups can be illustrated by the fact that 13.7% of women without a FCDR were considered severely obese, as compared to 44.4% of women with a FCDR.
In unadjusted models, older age was associated significantly with increased odds of first cycle dose reduction, with women ages 65 years or older having 5.7-fold higher odds (95% CI:1.7–18.7; p-trend:0.003) of dose reduction than women < 50 years of age (Table 3). Similarly, in these unadjusted models, being post-menopausal was also associated with increased odds of first cycle dose reduction (OR:3.1; 95% CI:1.4-7.0). Presence of comorbidities was also associated with increased unadjusted odds of dose reduction (OR:2.9; 95% CI:1.4–5.8), with significant associations observed for diabetes (OR:3.7; 95% CI:1.5–8.9) and cardiovascular disease (OR:2.6; 95% CI:1.1–6.5).
Main results: dose reduction across all cycles (ARDI)
Given higher frequency of dose reduction (and thus cases) in ARDI analyses, we are able to present unadjusted and adjusted results for this outcome. In unadjusted models, BMI was strongly positively associated with odds of dose reduction (p-trend:<0.0001) with severely obese women having greater likelihood of dose reduction compared to normal weight women (OR:4.2; 95% CI:2.2–8.3). This association persisted with covariate adjustment (p-trend:0.0006): overweight vs. normal weight: 1.6 (95% CI:0.9–3.1), obese (OR:2.1; 95% CI:1.0-4.4), and severely obese (OR:4.1; 95% CI:1.9–8.9).
Older age was associated with increased odds of dose reduction over the course of chemotherapy (ARDI < 90%), which persisted after covariate adjustment (OR 65 + years vs. < 50 years:3.7; 95% CI:1.8–7.6; p-trend:0.0004). In unadjusted models, women with breast cancer who were non-Hispanic Black were more likely to experience dose reduction over the course of chemotherapy than non-Hispanic White patients (OR:2.1; 95% CI:1.1–4.1); however, this association attenuated with covariate adjustment (OR:1.5; 95% CI:0.7–3.1). Calendar time was significantly associated with odds of dose reduction, with patients treated in 2010–2013 having lower odds of dose reduction than those treated in 2006–2009 (OR:0.5; 95% CI:0.3–0.9). This association remained after accounting for other covariates. The presence of any comorbidity was associated with the odds of dose reduction, and maintained significance in adjusted models (OR:1.7; 95% CI:1.0-2.8). While diabetes, cardiovascular disease, and the Charlson Comorbidity Index were associated with ARDI in unadjusted models, notably, none of these associations maintained statistical significance in adjusted models.
To address concern that the BMI-ARDI association may be residually confounded by factors associated with ARDI, but not included in the a priori set of covariates (age, race/ethnicity, WBC count), we conducted a sensitivity analysis further adjusting the adjusted BMI-ARDI association for the two additional covariates found to maintain statistical significance in adjusted models: calendar time and any pre-existing comorbidity. As shown in eTable 1, findings were robust, with BMI still very strongly associated with the ARDI (p-trend:0.006), albeit with a weaker effect estimate (OR severely obese vs. normal weight:3.3; 95% CI: 1.5–7.4).
Discussion
In a cohort of women receiving ACT for treatment of breast cancer at KPNC from 2006 to 2013, BMI was strongly associated with dose reduction, and the prevalence of dose reduction increased with increasing BMI. This was observed for both FCDP and the ARDI, overall and by each individual drug. Associations between obesity and the ARDI persisted in multivariable models, including age, race/ethnicity, WBC count. Dose reduction was more common in older individuals, individuals with comorbid conditions, and individuals who were treated in earlier years, and it should be noted that the significant BMI-ARDI association persisted even after adjustment for these other significantly associated factors.
Among patients receiving ACT, first cycle dose reductions were more common in obese patients, with a strong gradient observed across BMI categories, consistent with prior studies [1,2,3,4,5,6]. Because no normal weight patients received dose reductions > 10% in the first cycle, we were unable to calculate an OR for first cycle dose reduction, reflecting the shear strength of association. It is possible that association between BMI and first cycle dose reduction may have been, in part, driven by comorbid conditions or other factors. However, because the association with obesity was so strong, it is unlikely to be entirely explained by confounding. Notably, in analyses of the ARDI (where we were able to conduct multivariable adjustment), we observed strong associations between BMI and ARDI, after adjusting for a priori selected covariates (age, race/ethnicity, and white blood cell count). Furthermore, this finding was robust and maintained significance when further adjusting for additional factors found to be significantly associated with the ARDI in our adjusted models (calendar time and any comorbidity). Thus, it seems unlikely that the association between BMI and dose reduction is reflecting confounding. Even so, further work is needed to assess the extent to which these associations persist in a larger sample that can carefully adjust for a range of covariates, including individual comorbidities. In future studies, it would be helpful to see if these associations hold in contemporary data and in additional community settings.
Interestingly, we found that the pattern of dose reduction with increasing BMI holds across individual drugs, indicating that these dose reductions are not drug-specific but rather indicate a consistent pattern of dose reducing obese patients. Future studies, using data on a wider range of drug combinations, should examine whether this pattern holds across individual drugs in different regimens, as well.
We did not observe a statistically significant association between race/ethnicity and dosing, as was observed in an earlier study of 489 breast cancer patients treated with cyclophosphamide-containing adjuvant chemotherapy for localized or regional (stages I-III) breast cancer at one of 10 treatment sites in New York and Michigan [9]. The observed difference in findings could be due to a difference in study years (1985–1997 vs. 2006–2013 in the current study). It is also possible that there is less dose reduction of underrepresented patients in a large integrated healthcare delivery system, where we might expect more standardization of patient care, although it should be noted that an association between race/ethnicity and chemotherapy dosing was observed in KPNC ovarian cancer patients diagnosed between 2000 and 2013 [17]. Even though not statistically significant, the OR suggests that non-Hispanic Black women may be more likely to receive a dose reduction, particularly in the first cycle; this small study may be underpowered to detect a modest association between race/ethnicity and dosing, and thus this association needs to be evaluated in a larger study.
For the first time, we observed that older adults were more likely to be dose reduced, including at the outset of chemotherapy, which could potentially reflect concerns about toxicity, frailty, comorbidity, or concern about decreased bone marrow reserve with increasing age, particularly since we observed evidence of increased dose reduction among those with comorbidities. That said, no significant associations were observed for individual comorbidities, especially after adjustment, possibly given the small sample size and limited power. Importantly, dose reduction as characterized by FCDP and ARDI decreased over time, which may be expected given the release of the 2012 ASCO guidelines stating that obese patients should be given the full BSA determined dose [8]. Further work might examine whether this pattern is a reflection of the release of the 2012 ASCO guidelines, the implementation oncology-specific modules streamlining electronic chemotherapy prescribing, or other factors. It would also be informative to better understand the extent to which patients remain dose reduced in current clinical practice and how the associations between dosing and obesity, age, and comorbidity have changed over time. Given the time period of this study, we were unable to address these questions in the current study, but we are currently conducting expanded research, using more recent data, to examine these questions.
This study has several important strengths. KPNC is an integrated healthcare delivery system with clinical databases that captured detailed information on chemotherapy, including the drugs, dates, and dosages received, detailed sociodemographic information, and clinical factors, including measures of height and weight, as well as detailed data about the cancer diagnosis and patient comorbidities; thus, relevant data were available in this real-world healthcare setting. Medical chart review was also possible when it was needed to determine intended regimens. However, as no normal weight patients experienced first cycle dose reduction, we were unable to obtain estimates using this as a reference category. We were able to examine impacts of select covariates on ARDI estimates. However, further well-powered analyses will be needed, particularly for individual comorbidities and race/ethnicity, where we were not well-powered to detect modest associations and had to collapse groups for analyses. Contemporary analyses will be needed to also examine whether these observations are relevant for other breast cancer chemotherapy regimens, and to examine whether dose reduction and these associations occur in recent years. With increasing awareness of dose optimization to reduce toxicity which may influence initial dosing strategies, these patterns may be more complex in recent data. In analyses of the ARDI, we did not examine toxicities occurring over the course of chemotherapy, which would affect subsequent dosing and provide clinical rationale for such dose reduction. Even so, we observed the same clear pattern with obesity and first cycle dose reduction, albeit in a smaller proportion of patients, before any such toxicity would have occurred. Future work will be needed to assess the impact of toxicity on ARDI.
In summary, this study demonstrates the usefulness of data from integrated healthcare delivery systems to extract and determine precise chemotherapy variables. Results suggest that obese women were more likely to receive dose reductions, as were older women, women with comorbid conditions, and women diagnosed in earlier years- suggesting potential impact of the release of the ASCO guidelines in 2012 [8]. Further work is needed to assess whether these associations persist in other breast cancer regimens and in more recent years, particularly after the release of the ASCO guidelines. Whether dose reductions impact patient outcomes, including toxicity, recurrence, and survival, is important to better understand the impact of decision making on outcomes for patients.
Data Availability
The datasets generated and analyzed for the results presented here are available in de-identified format by contacting the corresponding author.
References
Griggs JJ, Sorbero ME, Lyman GH (2005) Undertreatment of obese women receiving breast cancer chemotherapy. Arch Intern Med 165:1267–1273
Lyman GH, Dale DC, Crawford J (2003) Incidence and predictors of low dose-intensity in adjuvant breast cancer chemotherapy: a nationwide study of community practices. J Clin Oncology: Official J Am Soc Clin Oncol 21:4524–4531
Madarnas Y, Sawka CA, Franssen E, Bjarnason GA (2001) Are medical oncologists biased in their treatment of the large woman with breast cancer? Breast Cancer Res Treat 66:123–133
Carroll JP, Protani MM, Nguyen L, Cheng ME, Fay M, Saleem M, Pillay PS, Walpole E, Martin JH (2014) Toxicity and tolerability of adjuvant breast cancer chemotherapy in obese women. Med Oncol 31:881
Gouerant S, Leheurteur M, Chaker M, Modzelewski R, Rigal O, Veyret C, Lauridant G, Clatot F (2013) A higher body mass index and fat mass are factors predictive of docetaxel dose intensity. Anticancer Res 33:5655–5662
Griggs JJ, Culakova E, Sorbero ME, van Ryn M, Poniewierski MS, Wolff DA, Crawford J, Dale DC, Lyman GH (2007) Effect of patient socioeconomic status and body mass index on the quality of breast cancer adjuvant chemotherapy. J Clin Oncology: Official J Am Soc Clin Oncol 25:277–284
Greenman CG, Jagielski CH, Griggs JJ (2008) Breast cancer adjuvant chemotherapy dosing in obese patients: dissemination of information from clinical trials to clinical practice. Cancer 112:2159–2165
Griggs JJ, Mangu PB, Anderson H, Balaban EP, Dignam JJ, Hryniuk WM, Morrison VA, Pini TM, Runowicz CD, Rosner GL, Shayne M, Sparreboom A et al (2012) Appropriate chemotherapy dosing for obese adult patients with cancer: American Society of Clinical Oncology clinical practice guideline. J Clin Oncology: Official J Am Soc Clin Oncol 30:1553–1561
Griggs JJ, Sorbero ME, Stark AT, Heininger SE, Dick AW (2003) Racial disparity in the dose and dose intensity of breast cancer adjuvant chemotherapy. Breast Cancer Res Treat 81:21–31
Bandera EV, Lee VS, Rodriguez-Rodriguez L, Powell CB, Kushi LH (2015) Impact of Chemotherapy Dosing on Ovarian Cancer Survival according to body Mass Index. JAMA Oncol 1:737–745
Shayne M, Crawford J, Dale DC, Culakova E, Lyman GH, Group ANCS (2006) Predictors of reduced dose intensity in patients with early-stage breast cancer receiving adjuvant chemotherapy. Breast Cancer Res Treat 100:255–262
Kwan ML, Ambrosone CB, Lee MM, Barlow J, Krathwohl SE, Ergas IJ, Ashley CH, Bittner JR, Darbinian J, Stronach K, Caan BJ, Davis W et al (2008) The Pathways Study: a prospective study of breast cancer survivorship within Kaiser Permanente Northern California. Cancer Causes Control 19:1065–1076
Mandelblatt JS, Luta G, Kwan ML, Makgoeng SB, Ergas IJ, Roh JM, Sternfeld B, Adams-Campbell LL, Kushi LH (2011) Associations of physical activity with quality of life and functional ability in breast cancer patients during active adjuvant treatment: the Pathways Study. Breast cancer research and treatment ;129: 521-9
Ergas IJ, Cespedes Feliciano EM, Bradshaw PT, Roh JM, Kwan ML, Cadenhead J, Santiago-Torres M, Troeschel AN, Laraia B, Madsen K, Kushi LH (2021) Diet quality and breast Cancer recurrence and survival: the Pathways Study. JNCI Cancer Spectr ;5
Mosteller RD (1987) Simplified calculation of body-surface area. N Engl J Med 317:1098
National Comprehensive Cancer Network
Bandera EV, Lee VS, Rodriguez-Rodriguez L, Powell CB, Kushi LH (2016) Racial/Ethnic disparities in Ovarian Cancer Treatment and Survival. Clin Cancer Res 22:5909–5914
Acknowledgements
This work has been supported by grants from the NCI (U24 CA171524, R37CA222793, R01 CA105274, U01 CA195565, R50CA211115) as well as the Geoffrey Beene Cancer Research Center at Memorial Sloan Kettering Cancer Research Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Bandera serves in an Advisory Board for Pfizer Clinical Trial Diversity Initiative. Other authors have no conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kantor, E.D., O’Connell, K., Ergas, I.J. et al. Assessment of breast cancer chemotherapy dose reduction in an integrated healthcare delivery system. Breast Cancer Res Treat 203, 565–574 (2024). https://doi.org/10.1007/s10549-023-07126-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-07126-4