Abstract
Purpose
People with a history of breast cancer are at risk of losing function during and after treatment. Unfortunately, little is known about the individual and additive effects of specific treatment, disease-related, and demographic factors that may contribute to functional decline. This manuscript reports the results of a multi-center study to evaluate the effects of these factors on function.
Methods
In this cross-sectional study, women with a history of breast cancer referred to physical medicine and rehabilitation cancer rehabilitation clinics were administered the PROMIS® Cancer Function Brief 3D Profile to evaluate function in the domains of physical function, fatigue, and social participation. Clinical and demographic information, including treatment history and disease status, was recorded by clinicians. Patients were analyzed in two groups: those with active disease on antineoplastic treatment, and those with no evidence of disease (NED). A multivariable model was constructed to detect associations between clinical and demographic factors.
Results
In patients with NED, the presence of chemotherapy-induced peripheral neuropathy (CIPN) was strongly associated with reduced function in all three domains. In those with active disease, having brain metastases was significantly associated with reduced function in all domains and CIPN with reduced physical function. Radiation was associated with improved function in both cohorts.
Conclusions
Among women seeking rehabilitative care, CIPN and the presence of brain metastases were most strongly associated with a decline in function. The effects of radiation on function were unexpected and may be partially explained by the treatment’s role in symptom management. Clinicians who treat breast cancer should consider a patient’s functional status when providing supportive care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over 3.8 million women in the United States have a history of breast cancer, a number expected to grow at an increasing rate as early detection methods and treatments improve [1]. As a result of tumor and treatment effects, 62–92% of breast cancer survivors develop physical impairments that reduce their function, health-related quality of life, employability, and psychosocial well-being [2,3,4,5,6]. These impairments include chemotherapy-induced peripheral neuropathy (CIPN) [7], soft tissue fibrosis [8], post-mastectomy pain [9], lymphedema [10], fatigue [11], and other neurologic and musculoskeletal pain conditions [12,13,14]. Given the prevalence of breast cancer and associated impairment burden, it is not surprising that women with breast cancer make up roughly 40% of patients seen in cancer rehabilitation clinics nationwide [15].
A growing evidence base supports rehabilitation interventions as a means of improving function, reducing impairment, and managing symptoms associated with treatment for patients with a history of breast cancer [16, 17]. Better understanding mediators and mechanisms of reduced function may help direct treatment and identify at-risk patients. Unfortunately, variables associated with functional decline remain relatively under-researched. Given the variety of potential contributors to functional decline—dynamic and toxic treatment regimens, long-term endocrine therapy, multiple surgeries, advanced disease, and non-cancer factors such as lifestyle choices and psychosocial circumstances—it is essential to address this knowledge gap.
To better identify factors associated with reduced function in breast cancer patients, the Cancer Rehabilitation Medicine Metrics Consortium [18] collected patient- and clinician-reported measures of function, as well as clinical and demographic data, in women with a history of breast cancer referred to physical medicine and rehabilitation cancer rehabilitation clinics. This manuscript reports the results of the analysis of those data.
Methods
This post hoc analysis was part of a larger project to develop, validate, and clinically implement a patient-reported outcome measure (PROM) to assess domains and trait ranges relevant to patients with cancer and their rehabilitation service needs. These efforts and their results have been previously described [15, 18, 19]. Study sites included cancer rehabilitation medicine clinics at five National Cancer Institute and/or American College of Surgeons Commission on Cancer-affiliated hospitals (University of Pittsburgh, Case Western Reserve University, Swedish Cancer Institute, Shirley Ryan Ability Lab, and the University of Michigan). The current and PROMIS® development efforts were approved by the Institutional Review Boards at each site, and the University of Michigan was the coordinating center.
Participants
A convenience sample of patients undergoing initial or follow-up encounters with Physical Medicine and Rehabilitation (PM&R) physicians was enrolled. Referrals were placed by an oncologist or primary care provider based on their clinical assessment of the patient’s need. Any patient age ≥ 18 with any tumor type, stage, or treatment regimen was eligible for enrollment. Patients with cognitive or communication barriers precluding accurate responses, as assessed by the treating PM&R physician, were excluded from enrollment. Data from participants with a diagnosis of breast cancer were used in this study.
Data
The cross-sectional data were collected in-person over a 12-month interval from March 2018 to March 2019. At the time of their cancer rehabilitation clinic visits, patients completed the items of the PROMIS® Cancer Function Brief 3D Profile; a cancer specific patient-reported measure of function that includes a functional assessment of the past 7 days across three domains (physical function, fatigue, social participation) and has been validated in this population [15, 19]. The PROMIS® was completed either via tablet or paper, depending on the study site. Clinicians recorded demographic and clinical data at the time of a patient’s visit, which included treatment history, age, cancer specifics, extent of disease, and clinician-rated performance status. All data was stored in an electronic REDCap™ database. Statistical analysis was conducted via SAS 9.4 (Cary, North Carolina).
Statistical analysis
Patients were divided into those with active disease and those with no evidence of disease (NED) due to the numerous clinical factors that differed between the groups (e.g. specific sites of disease, different intervention regimens). Within each cohort, univariable analyses were conducted to explore associations between treatment-related factors, disease-related factors, and patient age.
Treatment-related factors included histories (previous, current, never) of chemotherapy, radiation, endocrine therapy, and/or surgery (within 4 weeks, 4+ weeks ago, never), and the presence or absence of CIPN. Those currently receiving radiotherapy (5) or surgery within the previous 4 weeks (5) were excluded from analysis because the small number limited potential for informative analyses. No patients in either cohort received only radiation therapy.
Disease-related factors for those with active disease included the presence of metastases to brain, bone or other sites was assessed by a simple “yes/no” question. To test the additive effects of cancer treatment on function, in the NED cohort, a sum of the three binomial treatments (chemotherapy, radiation therapy, surgery) were derived.
Analysis of variance was conducted for all categorical variables and a linear regression analysis was conducted for age, the only continuous characteristic. A multivariable model was also conducted, using all covariates. Variance inflation factor was examined to check for multicollinearity. In the multivariable analysis, p values < 0.05 served as a threshold for determining a statistically significant association between presence of a given cancer-related factor and increased or decreased patient-reported function.
Results
A total of 202 breast cancer patients were enrolled. Descriptive statistics are in Table 1. Results of univariate and multivariate modeling for the NED and active disease cohorts are presented in Tables 2 and 3, respectively.
NED cohort results
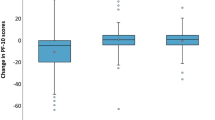
Univariable analysis of the NED cohort (Table 2; n = 142) found that prior radiation (p = 0.02, parameter estimate: 3.24 [95% CI 0.48 to 6.01]) and CIPN (p < 0.01, parameter estimate: -6.28 (95% CI − 9.43 to − 3.13) demonstrated a statistically significant association with lower physical function. Age (p = 0.02, parameter estimate: − 0.16 [95% CI − 0.30 to − 0.02]) and CIPN (p = 0.02, parameter estimate: 5.02 [95% CI 0.80 to 9.24]) demonstrated a statistically significant association with fatigue. CIPN (p = 0.02, parameter estimate: − 4.70 [95% CI − 8.65 to − 0.76]) was the lone objective variable significantly associated with lower social participation scores.
Following the NED univariable analysis, a multivariable analysis was carried out with all predictors identified a priori. For physical function, the a priori multivariable model found prior radiation (p = 0.01, parameter estimate: 3.71 [95% CI 0.83 to 6.58]) and CIPN (p < 0.01, parameter estimate: − 6.19 [95% CI − 9.41 to − 2.98]) associated with lower function. Greater levels of fatigue were associated with CIPN (p < 0.01, parameter estimate: 5.88 [95% CI 1.57 to 10.19]) and age (p = 0.02, parameter estimate: − 0.17 [95% CI − 0.31 to 0.03]). Finally, only CIPN was associated with lower social participation (p = 0.01, parameter estimate: − 5.34 [95% CI − 9.46 to 1.22]). (Table 2).
Active disease cohort
For the active breast cancer cohort (n = 60), univariable analysis (Table 3) found that brain metastases served as the only predictor significantly associated with a decreased score in the physical function domain (p = 0.02, parameter estimate: − 9.44 [95% CI − 17.11 to − 1.77]) and increased score in the fatigue domain (p = 0.04, parameter estimate: 7.65 [95% CI 0.33 to 14.97]). There were no predictors that reached statistical significance within the category of social participation.
Multivariate analysis with all predictors identified a priori was then conducted for each domain. For the physical function domain, brain metastases (p ≤ 0.01, parameter estimate: − 12.23 [95% CI − 19.80 to − 4.66]) and CIPN (p = 0.03, parameter estimate: − 5.24 [95% CI − 9.94 to − 0.54]) were significantly associated with reduced levels. Similar results were found in the fatigue domain, with brain metastases (p = 0.01, parameter estimate: 9.62 [95% CI 2.28 to 16.96]) being associated with greater degrees of fatigue. Brain metastases (p = 0.04, parameter estimate: − 7.44 [95% CI − 14.50 to − 0.37]) were also associated with significantly reduced social participation. Conversely, prior radiation was associated with less fatigue (p = 0.01, parameter estimate − 6.77 [95% CI − 12.04 to − 1.50]) and greater physical function (p ≤ 0.01, parameter estimate: 7.44 [95% CI 2.03 to 12.85]) and social participation (p = 0.02, parameter estimate: 6.00 [95% CI 0.93 to 11.07]). (Table 3).
Discussion
This study examined the association of treatment and cancer-related factors with function in patients with a history of breast cancer who are receiving rehabilitation care. While many factors influence ability to participate in desired and needed activity, these findings provide valuable insight that may help identify patients most at risk for functional decline.
Within the NED cohort, the presence of CIPN was most strongly associated with decline in physical function. CIPN is prevalent in the breast cancer population, particularly with the use of taxane-based therapy, and leads to higher risk of falling, anxiety, depression, insomnia, and psychological distress [20, 21]. Results of this study further demonstrate the association of CIPN with lower physical function in breast cancer survivors, thus supporting the need for effective cancer rehabilitation intervention. In addition to CIPN, age was associated with higher patient reported fatigue; this may indicate less resilience to treatment effects, possibly due to frailty or pre-morbid non-cancer impairments. Age and CIPN were most predictive of decreased social participation, perhaps in part due to age-related functional decline or fear of ambulating in the community. Since all treatment factors analyzed can potentially cause functional decline, identifying CIPN as the strongest predictor of reduced function in this subgroup helps identify at-risk patients.
While CIPN was also associated with reduction in function in patients with active disease (physical function and fatigue domains), active chemotherapy was not. Possible explanations for this include that active chemotherapy does not necessarily mean a patient has or will develop CIPN and that there are different chemotherapy regimens depending on disease status that may cause greater toxicities. This underscores the importance of evaluating toxicities in the context of a person’s global function; intervention studies based on the development of CIPN are warranted.
Conversely, radiation was found to have a small but significant association with increased physical function in the NED cohort, though no effect on fatigue or social participation. This is an unexpected finding and may be the result of selection bias. For example, the inclusion of patients who had higher performance status or given the risk of complications from radiation had received physical rehabilitation prior to this study (e.g., physical therapy, occupational therapy, lymphedema therapy). Another possible explanation is that radiation in the absence of surgery portends better function than surgery alone or a combination of the two; this is consistent with prior data suggesting that surgery and chemotherapy has a greater impact on quality of life than radiation [22].
Radiation was again found to have a small positive effect on function in those with active disease, similar to the NED cohort. For this group, it may reflect the benefits on pain and function conveyed by radiation in the setting of metastatic disease. As a symptom modulator, radiotherapy improving function is not necessarily unexpected, although this cohort also includes women receiving curative-intent treatment who already completed radiation. Of note, only 30.1% of patients receiving curative intent treatment in this cohort had received prior radiation, compared to 82.4% of those with metastatic disease, suggesting that radiation may have provided symptom relief in this cohort. The lack of patients actively receiving radiation in this study, due to a low accrual number, suggests that acute toxicities of radiation are not well accounted for, but that the benefits of radiation in those with active tumors is.
Interestingly, a combination of surgery, radiation, and chemotherapy was not associated with a greater decline in function in patients with NED in this analysis. One explanation for this includes that simply having one of these treatments was enough to reduce function (e.g. chemotherapy causing CIPN); having a combination of treatments may not have a significant additive effect on reduced function. Of course, standardizing assessments at specific points following completion of treatment may provide more granular insight into the effect of treatment timing on function. In addition, endocrine therapy, which can cause arthralgia as well as other musculoskeletal and neuromuscular impairments (e.g., trigger finger, carpal tunnel syndrome, arthralgia) was not significantly associated with reduced function. This may be because impairments from endocrine therapy, while bothersome and limiting in some ways, may not reduce a person’s overall function and ability to participate in social roles.
For those with active disease, brain metastases were most associated with decline in physical function and greater fatigue. Although the association was strong, the underlying cause of this finding is uncertain. It could be the result of neurologic deficits and/or the fact that brain metastases signify later stage disease and, thus, overall increased disease/treatment-related burden and, in turn, impacting downstream physical function, such as increased sedentary activity and deconditioning.
Of note, only 10% of patients in this cohort had brain metastases. This is consistent with previous research reporting that less than 10% of breast cancer patients with metastatic disease are clinically identified as having brain metastases [23]. That said, brain metastases are far more prevalent in breast cancer patients evaluated post-mortem with prevalence ranging from 15 to 30% [23] The impact of hidden brain metastases may underlie a rapid decline in health and therefore low number with brain metastases presenting to rehabilitation clinics. Alternatively, there may be breast cancer patients with small and asymptomatic central nervous system disease that do not require rehabilitation related to the metastases.
The presence of metastatic disease in the active disease subgroup alone did not independently predict low function in patients with active disease, nor did active or prior chemotherapy, or prior surgery. This suggests there may be additional factors leading to functional decline in patients within this population that were not accounted for in this study. Such unexplored factors may cause impairment and reduced function in this population to a higher degree than these treatments.
Cancer rehabilitation care must be held to rigorous evidence-based standards to demonstrate value to patients, payers, and the oncology providers. This poses a challenge in a heterogenous population to which care is often individualized. The results in this study have multiple strengths towards that end. First, it includes patients from multiple sites increasing the generalizability and external validity of the findings. The data included high quality and complete information regarding participants’ demographic characteristics and cancer histories. Additionally, the independent variables were assessed with a well-validated PROMIS® instrument vetted specifically for this population. As PROMs become essential for cancer research, this paper enhances understanding function as an endpoint for future clinical trials. With functional status playing an important role in treatment decision-making, understanding treatment effects on function is essential in oncology practice and clinical trials.
The findings reported in this study are generally consistent with other studies evaluating functional decline in cancer patients, while adding greater detail to the breast cancer population. Additionally, this study is novel in that it uses an item-response theory-based PROM specific to function in cancer patients. This approach is widely accepted as the gold standard for PROM use [24], and previous studies often use instruments specific to only one aspect of function (e.g. activities of daily living) or subsets of larger quality of life instruments (e.g. the physical function component of the SF-36). Two of the strongest predictors of functional decline, age and systemic chemotherapy, have consistently been associated with functional decline across multiple cancers [25,26,27,28,29]. This study, however, provides breast-cancer-specific functional information stratified by those actively receiving treatment and long-term survivors, which is a novel and potentially important contribution to the literature. Additionally, our findings that both surgery and radiation therapy are not strongly linked to functional decline are in line with other studies that evaluated these treatments in other cancer types. Of note, the existing data about the impact of surgery and radiation therapy in the breast cancer population are limited in the literature, enhancing the importance of these findings. Few studies exist evaluating the effect of surgery on function, including in esophageal cancer or patients already experiencing functional decline and admitted to nursing facilities [30]. Studies on radiation do not include breast cancer nor anatomic-specific information, with authors of a recent review article to concluding that radiotherapy is “…likely to have less impact on functional status than their systemic counterparts.” [30] Though not evaluated in breast cancer, brain metastases have been linked to functional decline in lung cancer patients [31].
This study has several limitations. First, its focus on patients already referred to cancer rehabilitation clinics narrows its scope and creates the potential for selection bias. The results should not be interpreted to suggest, for example, that patients receiving endocrine therapy are not at risk for impairment or functional decline. Rather, the results only draw associations between what treatment- and disease-related factors are most strongly associated with low function in patients already experiencing symptoms requiring rehabilitation. Additionally, the average age of the study population was below the average age of the general population of people with breast cancer, suggesting a possible bias toward healthier, more active patients at baseline. It should also be noted that information regarding race/ethnicity and social determinants of health was not included in this analysis, both of which may have implications related to function. Second, treatment covariates were binary. For example, the data only reflected whether a patient had previously had surgery, not how many, what type of surgery, if there was breast reconstruction, among other characteristics. The radiation covariate did not distinguish the effects of active from prior radiation or quantify radiation fields or dosage. Additional research is needed to determine the effect of more specific surgical or radiation interventions on function. Third, use of PROMs as the only functional measure may be a limitation. While patients’ perceptions are a crucial dimension of functional assessment, PROMs are susceptible to recall bias and differential item functioning. Their pairing with objective measures of function (e.g., activity monitors) may offer a more comprehensive assessment of a patient’s capabilities. Last, the cross-sectional nature of this study provides only a snapshot of participants’ function. Additionally, timing from diagnosis to measurement varied significantly among patients in this study and they were not stratified based on timeline within cancer care continuum. Longitudinal evaluation would potentially provide greater clarity into the mechanisms of functional decline. A larger and longitudinal study may confirm these results and add additional detail.
Conclusion
Older age and presence of CIPN were most strongly associated with poorer function in breast cancer patients without evidence of disease. In those with active disease, having brain metastases was the strongest factor associated with low function. This study provides important insight into what most contributes to functional decline in breast cancer patients, which may inform the type and timing of rehabilitation service delivery. Future studies should prospectively follow patients and identify trends in function based on disease- and treatment-related factors.
Data availability
Available upon request. Currently curated by the University of Michigan.
References
American Cancer Society (2022) Cancer facts and figures 2022. American Cancer Society, Atlanta
Hidding JT, Beurskens CH, van der Wees PJ, van Laarhoven HW, Nijhuis-van der Sanden MW (2014) Treatment related impairments in arm and shoulder in patients with breast cancer: a systematic review. PLoS ONE 9(5):e96748
Cheville AL, Troxel AB, Basford JR, Kornblith AB (2008) Prevalence and treatment patterns of physical impairments in patients with metastatic breast cancer. J Clin Oncol 26(16):2621
Kaya T, Karatepe AG, Günaydn R, Yetiş H, Uslu A (2010) Disability and health-related quality of life after breast cancer surgery: relation to impairments. South Med J 103(1):37–41
Rietman JS, Dijkstra PU, Hoekstra HJ, Eisma WH, Szabo BG, Groothoff JW, Geertzen JH (2003) Late morbidity after treatment of breast cancer in relation to daily activities and quality of life: a systematic review. Eur J Surg Oncol 29(3):229–238
Visnjevac O, Matson B (2013) Postmastectomy pain syndrome: an unrecognized annual billion dollar national financial burden. J Pain 14(4):S33
Kamgar M, Greenwald MK, Assad H, Hastert TA, McLaughlin EM, Reding KW, Paskett ED, Bea JW, Shadyab AH, Neuhouser ML, Nassir R (2021) Prevalence and predictors of peripheral neuropathy after breast cancer treatment. Cancer Med 10(19):6666–6676
Stubblefield MD (2017) Clinical evaluation and management of radiation fibrosis syndrome. Phys Med Rehab Clin 28(1):89–100
Chang PJ, Asher A, Smith SR (2021) A targeted approach to post-mastectomy pain and persistent pain following breast cancer treatment. Cancers 13(20)
Pereira AC, Koifman RJ, Bergmann A (2017) Incidence and risk factors of lymphedema after breast cancer treatment: 10 years of follow-up. The Breast 1(36):67–73
Juvet LK, Thune I, Elvsaas IØ, Fors EA, Lundgren S, Bertheussen G, Leivseth G, Oldervoll LM (2017) The effect of exercise on fatigue and physical functioning in breast cancer patients during and after treatment and at 6 months follow-up: a meta-analysis. The Breast 1(33):166–177
Hayes SC, Johansson K, Stout NL, Prosnitz R, Armer JM, Gabram S, Schmitz KH (2012) Upper-body morbidity after breast cancer: incidence and evidence for evaluation, prevention, and management within a prospective surveillance model of care. Cancer 118(8 Suppl):2237–2249. https://doi.org/10.1002/cncr.27467. (PMID: 22488698)
McNeish BL, Zheutlin AR, Richardson JK, Smith SR (2020) Primary cancer location predicts predominant level of brachial plexopathy. Muscle Nerve 62(3):386–389
Oza S (2021) Aromatase Inhibitor-induced Musculoskeletal Syndrome: a Review of Rehabilitation Interventions. Curr Phys Med Rehabil Rep 9(3):119–126
Smith SR, Vargo M, Zucker D, Shahpar S, Gerber L, Henderson M, Jay G, Lee M, Cheville A (2021) Psychometric characteristics and validity of the PROMIS cancer function brief 3D profile. Arch Phys Med Rehab
Leclerc AF, Foidart-Dessalle M, Tomasella M, Coucke P, Devos M, Bruyère O, Bury T, Deflandre D, Jerusalem G, Lifrange E, Kaux JF (2017) Multidisciplinary rehabilitation program after breast cancer: benefits on physical function, anthropometry and quality of life. Eur J Phys Rehabil Med 53(5):633–642
Sleight AG, Gerber LH, Marshall TF, Livinski A, Alfano CM, Harrington S, Flores AM, Virani A, Hu X, Mitchell SA, Varedi M (2022) A systematic review of functional outcomes in cancer rehabilitation research. Arch Phys Med Rehab
Smith SR, Vargo M, Zucker DS, Henderson M, Shahpar S, Wisotzky EM, Custodio C, Basford J, Jay G, Gerber L, Cheville A (2021) The Cancer Rehabilitation Medicine Metrics Consortium: a path to enhanced, multi-site outcome assessment to enhance care and demonstrate value. Front Oncol 10:625700
Smith SR, Vargo M, Zucker DS, Shahpar S, Gerber LH, Henderson M, Jay G, Cheville AL (2022) Responsiveness and interpretation of the PROMIS Cancer Function Brief 3D profile. Cancer
Bao T, Basal C, Seluzicki C, Li SQ, Seidman AD, Mao JJ (2016) Long-term chemotherapy-induced peripheral neuropathy among breast cancer survivors: prevalence, risk factors, and fall risk. Breast Cancer Res Treat 159(2):327–333
Rivera DR, Ganz PA, Weyrich MS, Bandos H, Melnikow J (2018) Chemotherapy-associated peripheral neuropathy in patients with early-stage breast cancer: a systematic review. J Natl Cancer Inst 110(2):140
Park J, Rodriguez JL, O’Brien KM, Nichols HB, Hodgson ME, Weinberg CR, Sandler DP (2021) Health-related quality of life outcomes among breast cancer survivors. Cancer 127(7):1114–1125
Martin AM, Cagney DN, Catalano PJ, Warren LE, Bellon JR, Punglia RS, Claus EB, Lee EQ, Wen PY, Haas-Kogan DA, Alexander BM (2017) Brain metastases in newly diagnosed breast cancer: a population-based study. JAMA Oncol 3(8):1069–1077
Fries JF, Bruce B, Cella D (2005) The promise of PROMIS: using item response theory to improve assessment of patient-reported outcomes. Clin Exp Rheumatol 23(5):S53
Pergolotti M, Deal AM, Lavery J, Reeve BB, Muss HB (2015) The prevalence of potentially modifiable functional deficits and the subsequent use of occupational and physical therapy by older adults with cancer. J Geriatric Oncol 6(3):194–201
Decoster L, Kenis C, Schallier D, Vansteenkiste J, Nackaerts K, Vanacker L, Vandewalle N, Flamaing J, Lobelle JP, Milisen K, De Greve J (2017) Geriatric assessment and functional decline in older patients with lung cancer. Lung 195(5):619–626
Galvin A, Helmer C, Coureau G, Amadeo B, Rainfray M, Soubeyran P, Dartigues JF, Pérès K, Bellera C, Delva F, Mathoulin-Pélissier S (2019) Determinants of functional decline in older adults experiencing cancer (the INCAPAC study). J Geriatric Oncol 10(6):913–920
Kenis C, Decoster L, Bastin J, Bode H, Van Puyvelde K, De Grève J, Conings G, Fagard K, Flamaing J, Milisen K, Lobelle JP (2017) Functional decline in older patients with cancer receiving chemotherapy: a multicenter prospective study. J Geriatric Oncol 8(3):196–205
Hoppe S, Rainfray M, Fonck M, Hoppenreys L, Blanc JF, Ceccaldi J, Mertens C, Blanc-Bisson C, Imbert Y, Cany L, Vogt L (2013) Functional decline in older patients with cancer receiving first-line chemotherapy. J Clin Oncol 31(31):3877–3882
Muhandiramge J, Orchard SG, Warner ET, van Londen GJ, Zalcberg JR (2022) Functional decline in the cancer patient: a review. Cancers 14(6):1368
Cheville AL, Basford JR, Parney I, Yang P, Diehn FE (2017) Nested cohort study to identify characteristics that predict near-term disablement from lung cancer brain metastases. Arch Phys Med Rehabil 98(2):303–311
Acknowledgements
None.
Funding
This study was funded in part by a grant from the Foundation for Physical Medicine and Rehabilitation.
Author information
Authors and Affiliations
Contributions
Conceptualization, methodology, formal analysis, writing, data curation; SRS: conceptualization, methodology, formal analysis, investigation, writing, visualization, supervision, data acquisition, funding acquisition; MV: conceptualization, investigation, data acquisition, writing; DZ: conceptualization, methodology, data acquisition, investigation, writing; BR: statistical analysis, visualization; SS: conceptualization, data acquisition, investigation, writing; LG: conceptualization, methodology, writing; MH: conceptualization, investigation, writing; GJ: validation, data curation, project administration; AC: conceptualization, data acquisition, methodology, writing.
Corresponding author
Ethics declarations
Conflict of interest
This was reviewed with all authors, and there are no relevant financial or commercial conflicts of interest.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee at each institution that participated in data collection.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stoyles, N., Cheville, A., Zucker, D. et al. Risk factors for reduced function in women with a history of breast cancer. Breast Cancer Res Treat 197, 613–621 (2023). https://doi.org/10.1007/s10549-022-06838-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-022-06838-3