Abstract
Purpose
Adjuvant treatment for breast cancer in postmenopausal women is a risk factor for bone loss. However, the association between bone mineral density (BMD) changes in premenopausal breast cancer patients and various adjuvant treatment regimens is not well characterized. In this study, we evaluated the changes in BMD according to adjuvant treatment in premenopausal women with breast cancer.
Methods
Between 2006 and 2010, BMD data of 910 premenopausal women with breast cancer before operation and 1, 2, 3.5, and 5 years post-operation were retrospectively analyzed. The patients were divided according to the type of treatment: observation (O), tamoxifen (T), chemotherapy (C), C followed by T (C → T), and gonadotropin-releasing hormone (GnRH) agonist with T (G + T).
Results
After 5 years of follow-up, BMD changes were similar between the T and O groups (all p > 0.05). Within 1 year of treatment, the C group showed the most significant BMD loss. The C → T and G + T groups showed more significant BMD loss in the lumbar spine and femur than the O and T groups (both p < 0.001, both). After 1 year of treatment, BMD loss in the lumbar spine was significantly greater in the C → T and G + T groups than in the T group; this tendency was maintained for 5 years of treatment (all p < 0.005).
Conclusion
Premenopausal women who received adjuvant treatment which induced menopause showed significant bone loss which lasted for 5 years. Although no significant difference was observed between the O and T groups, tamoxifen treatment during chemotherapy or GnRH agonist treatment might prevent bone loss.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Adjuvant chemotherapy and endocrine therapy for breast cancer can induce bone loss and cause osteoporosis [1,2,3]. Loss of ovarian function results in bone loss regardless of age or etiology. After the onset of menopause, a decrease in estrogen levels is associated with bone loss, and early menopause is one of the strongest predictors of osteoporosis [4,5,6]. Chemotherapy in premenopausal breast cancer patients causes early menopause within 1 year of therapy initiation, which leads to rapid bone loss [2, 7]. Gonadotropin-releasing hormone (GnRH) agonists are efficient suppressors of ovarian function and induce a temporary menopausal status. By inhibiting the peripheral aromatization of gonadal steroids to estrogen, aromatase inhibitors reduce the circulating estrogen levels to values lower than those during natural menopause, predisposing breast cancer patients to bone loss and increased fracture risk [8, 9]. Tamoxifen treatment over a period of 5 years has a positive effect on bone mineral density (BMD) in postmenopausal women, but rapid bone loss ensues after cessation of treatment [1, 6, 10]. Moreover, there is evidence that tamoxifen may decrease BMD in premenopausal women due to its antagonistic effects on the potent activity of endogenous estrogen [6, 11].
Adjuvant chemotherapy followed by tamoxifen is the standard treatment for women with intermediate- or high-risk hormone receptor-positive breast cancer [12], although GnRH agonists are widely used owing to similar oncologic outcomes with few adverse effects compared to that with tamoxifen [13]. A recent study showed the benefits of 5 years of GnRH agonist treatment after chemotherapy in high-risk premenopausal breast cancer patients [14]. Moreover, tamoxifen treatment for 10 years was shown to confer survival benefit when compared to a 5-year course [15]. In premenopausal hormone-sensitive breast cancer patients, endocrine treatments are administered for long durations to ensure complete suppression of estrogen production [15]. However, induction of menopause at an early age may be associated with deleterious and long-term side effects including decreased BMD.
To date, the degree of bone loss after chemotherapy, tamoxifen, and GnRH agonist treatment in premenopausal women has not been investigated in detail. In this study, we examined the changes in BMD according to the type of breast cancer treatment in premenopausal patients.
Methods
Patients were selected from the Asan Medical Center database, which is a prospectively maintained web-based system that includes information on all patients who underwent breast cancer operation at the Asan Medical Center. The database provided detailed information on breast tumor type and treatment. A total of 8219 breast cancer patients underwent surgery between 2006 and 2010. We excluded metastatic breast cancer patients and included 3689 patients with available BMD data for retrospective analysis. Other exclusion criteria included postmenopausal status at the time of surgery, receipt of neoadjuvant chemotherapy, history of hormonal replacement therapy, and history of surgical oophorectomy. Finally, 910 premenopausal breast cancer patients were included in this study. Premenopausal status was defined as ongoing menstruation for 6 months after surgery. Bodyweight was classified according to the World Health Organization criteria; body mass index (BMI) < 18.5 and ≥ 25 kg/m2 was considered underweight and overweight, respectively.
All patients underwent surgery with modified radical mastectomy or breast-conserving surgery with sentinel lymph node biopsy. If malignant cells were detected in the sentinel lymph nodes, axillary lymph node dissection was performed. Postoperative radiation therapy was performed as indicated, and the chemotherapy regimen was chosen by the treating oncologist according to established protocols. Hormone receptor-positive patients received 5 years of adjuvant tamoxifen therapy starting at 6 months after the start of chemotherapy. In patients who received GnRH agonist treatment for 2 years, adjuvant tamoxifen therapy was started simultaneously. The patients who had stage 0 breast cancer and underwent mastectomy or small tumor without hormone receptor expression which was not recommend for chemotherapy did not receive systemic treatment. Patients were divided into five groups according to the systemic treatment regimens after surgery without considering radiotherapy: observation (O, surgery only), adjuvant tamoxifen only (T), adjuvant chemotherapy only (C), adjuvant chemotherapy followed by tamoxifen (C → T), and GnRH agonist plus tamoxifen (G + T).
To monitor bone health, BMD was measured before surgery and at 1, 2, 3.5, and 5 years after surgery. Patients who were diagnosed with osteopenia during follow-up received calcium and vitamin D supplements or were educated about lifestyle modifications. Patients with osteoporosis were asked to consult with the endocrinology department or were prescribed osteoporosis treatment.
BMD was tested by dual-energy X-ray absorptiometry (DXA) using a Hologic QDR densitometer (Hologic, Inc., Waltham, MA). BMD was measured at the lumbar spine (L-spine) and femoral neck, femoral trochanter and Ward’s triangle, intertrochanteric area, and total femoral area on the right. The L-spine and femur data were analyzed, and the average T scores were used.
Descriptive statistical analyses were performed for demographic and clinical characteristics. The changes in BMD according to treatment were examined using the χ2 test, and an analysis of variance was used to evaluate the differences among the treatment groups at 1, 2, 3.5, and 5 years. The analysis of covariance (ANCOVA) test was used for comparing the changes in BMD at 1, 2, 3.5, and 5 years. For multiple comparisons, the significance level was divided by the number of comparisons using the Bonferroni correction. Changes in BMD according to age, BMI, and initial T score were calculated by the same methods. A value of p < 0.05 was considered statistically significant. All statistical analyses were performed with SPSS version 21.
Results
Out of 910 premenopausal patients, 58, 130, 69, 346, and 304 patients were in the O group, T group, C group, C → T group, and G + T group, respectively (Table 1). The median age was 44.7 years (range 19–55). The baseline BMDs of the L-spine and femur were not influenced by age but were associated with BMI. Overweight patients had higher baseline BMDs of the L-spine (p < 0.001) and femur (p < 0.001) than underweight patients. At baseline, the C → T and G + T groups had higher BMD than the other treatment groups (Online Resource 1).
Changes in BMD according to age and BMI
After surgery, BMD changes in the L-spine were greater in patients aged ≥ 40 years than in patients aged < 40 years at 2 years (p = 0.010), 3.5 years (p = 0.029), and 5 years (p < 0.001). Although this trend was observed for femur BMD as well, the only significant difference was observed at 5 years after surgery (p = 0.029). There was no significant difference in BMD changes between the different BMI groups (Fig. 1).
BMD changes according to the initial T score
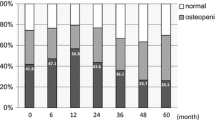
At 5 years after surgery, patients who had normal BMD at baseline had a greater decline in L-spine BMD than those who had osteopenia or osteoporosis at baseline (9.3% vs. 5.8% for L-spine BMD, 5.3% vs. 2.9% for femur BMD, all p < 0.001). Despite losing a higher percentage of their bone mass, patients with normal BMD at baseline consistently maintained higher T scores than those who had osteopenia or osteoporosis at baseline. These trends were more obvious in the L-spine than in the femur.
BMD changes according to treatment for 5 years
There was no significant difference in BMD changes in the L-spine or femur between the O and T groups at 5 years (Fig. 2). There was no significant difference in BMD changes in the L-spine between the C → T and G + T groups at 5 years.
Changes in BMD over 5 years according to the treatment group. Regarding the L-spine, the chemotherapy group showed a significantly lower BMD than the observation group at 1, 2, and 3.5 years after surgery (p < 0.005) and the C → T and G + T groups showed significantly lower BMD than the observation group at 1 and 2 years after surgery (p < 0.005). BMD bone mineral density, C → T chemotherapy followed by tamoxifen, G + T gonadotropin-releasing hormone agonist with tamoxifen
One year after surgery, BMD of the L-spine was significantly lower in the C group than in the other treatment groups (p < 0.001). The BMD decline in the C → T group (− 0.079) and G + T group (− 0.073) was less than that in the C group (p < 0.001, both) but more than that in the O and T groups (p < 0001, both). Similarly, the decline in femoral BMD in the C group was significantly higher than that in the O, C + T, and G + T groups (all p < 0.001) (Fig. 2, Online Resource 2). BMD change in the femur was significantly lower in the C → T and G + T groups than in the T group (both p < 0.001) (Online Resource 3).
At 2 years after surgery, there was a significant decline in BMD of the L-spine in the C, C → T, and G + T groups compared with that in the O group (p < 0.005, all). At 3.5 years after surgery, there was no significant difference in BMD changes in the L-spine among C, C → T, and G + T groups (C vs. C → T, p = 0.012; C vs. G + T, p = 0.349; C → T vs. G + T, p = 0.149) (Fig. 2, Online Resource 2). At 5 years, the degree of BMD change in the L-spine was significantly lower in the C → T group than in the O group (p = 0.002) and T group (p < 0.001) (Fig. 2, Online Resource 2). At 5 years, the degree of BMD change in the femur was not significantly different among the treatment groups (p = 0.058) (Online Resource 3).
Among patients who received chemotherapy, BMD in the first year of treatment was significantly lower in the C group than in the C → T group for both the L-spine and femur (p < 0.005, both), but the decrease in BMD became similar between these groups after 2 years of treatment.
In patients who received tamoxifen, the C → T and G + T groups showed significant BMD loss in the L-spine from the first year to the fifth year (Online Resource 2).
Discussion
Breast cancer and osteoporosis are important public health problems that have a major impact on life expectancy and quality of life [3, 4, 8, 16,17,18]. As screening programs and new treatments continue to increase the survival of patients with breast cancer, negative consequences of treatment such as bone loss are becoming increasingly important. Osteoporotic fractures represent a substantial clinical and economic burden for society [19]. In hormone receptor-positive premenopausal breast cancer patients, studies on endocrine therapy have addressed the advantages of prolonged treatment duration and combination therapy with aromatase inhibitors and GnRH agonists [14, 15, 20]. In these new endocrine therapy regimens, bone loss is a critical factor that should be balanced with the survival benefit. This 5-year retrospective analysis shows that both chemotherapy and GnRH agonist treatment, which can induce amenorrhea, result in decreased BMD and accelerated bone loss in premenopausal women with breast cancer. When compared with the observation group, tamoxifen treatment alone did not result in a protective effect on bone loss; however, compared with chemotherapy alone, treatment with tamoxifen after chemotherapy or along with a GnRH agonist resulted in the attenuation of bone loss. The degree of bone loss associated with GnRH agonist plus tamoxifen was comparable to that with chemotherapy followed by tamoxifen treatment.
The initial BMD did not correlate with age in this group of premenopausal women. However, women aged < 40 years experienced less bone loss than older women. Disruption of the gonadal axis may be permanent in women aged > 40 years who undergo ovarian suppression treatment [21, 22]. In a previous study, young premenopausal women who experienced amenorrhea after receiving adjuvant breast cancer treatment had a higher menstruation restoration rate than older women, and only minor BMD changes were observed [21]. Generally, the greater the degree of obesity, the higher the initial BMD; notably, the osteoporotic fracture risk is known to decrease in overweight patients [16, 23]. High BMI is thought to increase chronic strain on the bones, and the large stores of adipose tissue increase the production of estrogen [16].
Tamoxifen is known to have a bone-sparing effect in postmenopausal women or when it is used concurrently with ovarian suppression treatment; however, it can induce bone loss when used as a monotherapy in premenopausal patients [1]. In a tamoxifen chemoprevention trial, tamoxifen was associated with significant BMD loss in premenopausal women, whereas it prevented bone loss in postmenopausal women [11]. This obvious menstrual status-dependent effect can be explained by the differences in the endocrine milieu in which tamoxifen antagonizes the potent activity of endogenous estrogen [24]. In this study, BMD did not increase in the tamoxifen or observation groups; however, adding tamoxifen to GnRH agonist treatment and administration of tamoxifen after chemotherapy, both of which can decrease estrogen and mimic a postmenopausal status, demonstrated a bone protective effect.
Ovarian suppression or selective estrogen receptor modulators are used to treat premenopausal women with hormone receptor-positive breast cancer. Ovarian suppression causes immediate and artificial menopause. Moreover, chemotherapy can lead to ovarian failure [7]. In this study, the BMD in the C, C + T, and G + T groups seemed to decrease at all time points compared to that in the O group, and the decrease in BMD lasted for 5 years. Treatment-induced ovarian suppression or failure can dramatically decrease estrogen production, resulting in increased osteoclast-mediated bone resorption and subsequently decreased BMD [25]. Chemotherapy-induced ovarian dysfunction results from the depletion of ovarian follicles and damage to steroid-producing granulosa and theca cells that leads to decreased estradiol and inhibin B production [21]. The consequent loss of feedback inhibition in the pituitary gonadotrophs increases follicle-stimulating hormone levels. In women aged > 40 years, disruption of the gonadal axis may be temporary or permanent, and the type and duration of chemotherapy are the primary determinants of ovarian failure after breast cancer therapy [21, 22]. Several studies have analyzed the decrease in BMD in response to ovarian suppression treatments in breast cancer. Gnant et al. studied 401 premenopausal breast cancer patients who were treated with a GnRH agonist plus tamoxifen or a GnRH agonist plus anastrozole. After 3 years of treatment, overall bone loss was significantly more severe in patients who received the anastrozole/GnRH agonist combination than in those who received the tamoxifen/GnRH agonist combination [26]. Shapiro et al. showed that premenopausal women with chemotherapy-associated ovarian failure had significant bone loss in the L-spine at 6 months and a further decrease in bone density at 12 months [27]. In a study by Delmas et al., 36 premenopausal breast cancer patients who were treated with chemotherapy plus tamoxifen showed a significant decrease in BMD of the L-spine and hip at 1 year [28].
In this study, the decline in BMD was less with tamoxifen after chemotherapy than with chemotherapy alone, suggesting that tamoxifen may at least partially counteract the deleterious effect of chemotherapy on BMD. Although the mechanism underlying this effect remains unknown, it is likely that in patients with chemotherapy-induced premature menopause, the addition of tamoxifen after chemotherapy exerts estrogen agonist effects on the bone that are similar to those observed in postmenopausal women.
In this study, we observed less significant bone loss in the femoral neck than in the L-spine. This may be explained, at least in part, by the fact that the L-spine consists largely of cancellous bone, which is characterized by rapid bone turnover. Cortical bone, such as that found in the femur, is metabolically slower than cancellous bone, and therefore, it is less affected by alterations in bone turnover [1]. Overall, studies have confirmed that tamoxifen significantly decreases bone loss in the L-spine and to a lesser degree, in the femoral neck in postmenopausal women [1].
This study had several limitations. First, it was a retrospective study. Second, patients who underwent bone density testing in their hometown were not included. Third, all patients in this study were Asian, and ethnic variation can influence BMD. Particularly, in Asian women, the unadjusted risk for osteoporosis was reported to be higher than that in Caucasian women, and it showed a similar trend after multivariate adjustment, including adjustment for weight [29].
To the best of our knowledge, this is the first study to investigate the relationship between the 5-year quantitative changes in BMD, as measured by DXA, and the type of adjuvant treatment in premenopausal breast cancer patients. Although the present study was retrospective, we compared the effects of different breast cancer treatments on BMD loss in premenopausal patients, including those who did not undergo systemic treatment (O group). The L-spine BMDs at all time points decreased in the C, C → T, and G + T groups compared to those in the O group. The degree of BMD reduction in both the L-spine and femur at 1 year was the greatest in the C group compared with that in the C → T and G + T groups. From 2 years after surgery, there was no significant difference between these groups.
In conclusion, premenopausal women with breast cancer experience similar degrees of significant bone loss after adjuvant chemotherapy and GnRH agonist treatment, and this effect lasts for 5 years. Although the BMD decrease was not different between the observation and tamoxifen monotherapy groups, tamoxifen treatment during chemotherapy or GnRH agonist treatment might exert a protective effect on BMD. In premenopausal women receiving adjuvant therapy for breast cancer, efforts should be focused on optimizing BMD assessment and appropriate bone loss prevention.
References
Vehmanen L, Elomaa I, Blomqvist C, Saarto T (2006) Tamoxifen treatment after adjuvant chemotherapy has opposite effects on bone mineral density in premenopausal patients depending on menstrual status. J Clin Oncol 24(4):675–680. https://doi.org/10.1200/JCO.2005.02.3515
Cameron DA, Douglas S, Brown JE, Anderson RA (2010) Bone mineral density loss during adjuvant chemotherapy in pre-menopausal women with early breast cancer: is it dependent on oestrogen deficiency? Breast Cancer Res Treat 123(3):805–814. https://doi.org/10.1007/s10549-010-0899-7
Doo L, Shapiro CL (2013) Skeletal manifestations of treatment of breast cancer on premenopausal women. Curr Osteoporos Rep 11(4):311–318. https://doi.org/10.1007/s11914-013-0181-0
NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis and Therapy (2001). JAMA 285(6):785–795. https://doi.org/10.1001/jama.285.6.785
Richelson LS, Wahner HW, Melton LJI, Riggs BL (1984) Relative contributions of aging and estrogen deficiency to postmenopausal bone loss. N Engl J Med 311(20):1273–1275. https://doi.org/10.1056/nejm198411153112002
Sverrisdóttir Á, Fornander T, Jacobsson H, von Schoultz E, Rutqvist LE (2004) Bone mineral density among premenopausal women with early breast cancer in a randomized trial of adjuvant endocrine therapy. J Clin Oncol 22(18):3694–3699. https://doi.org/10.1200/jco.2004.08.148
Bruning PF, Pit MJ, de Jong-Bakker M, van den Ende A, Hart A, van Enk A (1990) Bone mineral density after adjuvant chemotherapy for premenopausal breast cancer. Br J Cancer 61(2):308–310
Lester J, Coleman R (2005) Bone loss and the aromatase inhibitors. Br J Cancer 93(Suppl 1):S16–S22. https://doi.org/10.1038/sj.bjc.6602691
Rodriguez-Sanz M, Prieto-Alhambra D, Servitja S, Garcia-Giralt N, Garrigos L, Rodriguez-Morera J, Albanell J, Martinez-Garcia M, González I, Diez-Perez A, Tusquets I, Nogues X (2016) AI-related BMD variation in actual practice conditions: a prospective cohort study. Endocr Relat Cancer. https://doi.org/10.1530/erc-16-0025
Love RR, Mazess RB, Barden HS, Epstein S, Newcomb PA, Jordan VC, Carbone PP, DeMets DL (1992) Effects of tamoxifen on bone mineral density in postmenopausal women with breast cancer. N Engl J Med 326(13):852–856. https://doi.org/10.1056/NEJM199203263261302
Powles TJ, Ashley S, Tidy VA, Nevantaus A, McCloskey E, Kanis J, Paterson AHG, Rosenqvist K (1998) Oral clodronate and reduction in loss of bone mineral density in women with operable primary breast cancer. J Natl Cancer Inst 90(9):704–708. https://doi.org/10.1093/jnci/90.9.704
Burstein HJ, Lacchetti C, Griggs JJ (2016) Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: American Society of Clinical Oncology clinical practice guideline update on ovarian suppression summary. J Oncol Pract 12(4):390–393. https://doi.org/10.1200/jop.2016.011239
Sohn G, Ahn SH, Kim HJ, Son B-H, Lee JW, Ko BS, Lee Y, Lee SB, Baek S (2016) Survival outcome of combined GnRH agonist and tamoxifen is comparable to that of sequential adriamycin and cyclophosphamide chemotherapy plus tamoxifen in premenopausal patients with lymph-node-negative, hormone-responsive, HER2-negative, T1–T2 breast cancer. Cancer Res Treat 48(4):1351–1362. https://doi.org/10.4143/crt.2015.444
Francis PA, Regan MM, Fleming GF, Láng I, Ciruelos E, Bellet M, Bonnefoi HR, Climent MA, Da Prada GA, Burstein HJ, Martino S, Davidson NE, Geyer CEJ, Walley BA, Coleman R, Kerbrat P, Buchholz S, Ingle JN, Winer EP, Rabaglio-Poretti M, Maibach R, Ruepp B, Giobbie-Hurder A, Price KN, Colleoni M, Viale G, Coates AS, Goldhirsch A, Gelber RD (2015) Adjuvant ovarian suppression in premenopausal breast cancer. N Engl J Med 372(5):436–446. https://doi.org/10.1056/NEJMoa1412379
Davies C, Pan H, Godwin J, Gray R, Arriagada R, Raina V, Abraham M, Alencar VHM, Badran A, Bonfill X, Bradbury J, Clarke M, Collins R, Davis SR, Delmestri A, Forbes JF, Haddad P, Hou M-F, Inbar M, Khaled H, Kielanowska J, Kwan W-H, Mathew BS, Mittra I, Müller B, Nicolucci A, Peralta O, Pernas F, Petruzelka L, Pienkowski T, Radhika R, Rajan B, Rubach MT, Tort S, Urrútia G, Valentini M, Wang Y, Peto R (2013) Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet 381(9869):805–816. https://doi.org/10.1016/S0140-6736(12)61963-1
Armstrong MEG, Spencer EA, Cairns BJ, Banks E, Pirie K, Green J, Wright FL, Reeves GK, Beral V, for the Million Women Study C (2011) Body mass index and physical activity in relation to the incidence of hip fracture in postmenopausal women. J Bone Miner Res 26(6):1330–1338. https://doi.org/10.1002/jbmr.315
Siris ES, Miller PD, Barrett-Connor E et al (2001) Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women: results from the national osteoporosis risk assessment. JAMA 286(22):2815–2822. https://doi.org/10.1001/jama.286.22.2815
Chrischilles EA, Butler C, Davis CS, Wallace RB (1991) A model of lifetime osteoporosis impact. Arch Intern Med 151(10):2026–2032. https://doi.org/10.1001/archinte.1991.00400100100017
Siris ES, Chen Y, Abbott TA et al (2004) Bone mineral density thresholds for pharmacological intervention to prevent fractures. Arch Intern Med 164(10):1108–1112. https://doi.org/10.1001/archinte.164.10.1108
Pagani O, Regan MM, Walley BA, Fleming GF, Colleoni M, Láng I, Gomez HL, Tondini C, Burstein HJ, Perez EA, Ciruelos E, Stearns V, Bonnefoi HR, Martino S, Geyer CE, Pinotti G, Puglisi F, Crivellari D, Ruhstaller T, Winer EP, Rabaglio-Poretti M, Maibach R, Ruepp B, Giobbie-Hurder A, Price KN, Bernhard J, Luo W, Ribi K, Viale G, Coates AS, Gelber RD, Goldhirsch A, Francis PA (2014) Adjuvant exemestane with ovarian suppression in premenopausal breast cancer. N Engl J Med 371(2):107–118. https://doi.org/10.1056/NEJMoa1404037
Tabatabai LS, Bloom J, Stewart S, Sellmeyer DE (2016) FSH levels predict bone loss in premenopausal women treated for breast cancer more than one year after treatment. J Clin Endocrinol Metab 101(3):1257–1262. https://doi.org/10.1210/jc.2015-3149
Cauley JA (2015) Estrogen and bone health in men and women. Steroids 99:11–15. https://doi.org/10.1016/j.steroids.2014.12.010
Compston J (2013) Obesity and bone. Curr Osteoporos Rep 11(1):30–35. https://doi.org/10.1007/s11914-012-0127-y
Osborne CK (1998) Tamoxifen in the treatment of breast cancer. N Engl J Med 339(22):1609–1618. https://doi.org/10.1056/nejm199811263392207
Gnant M, Mlineritsch B, Luschin-Ebengreuth G, Kainberger F, Kässmann H, Piswanger-Sölkner JC, Seifert M, Ploner F, Menzel C, Dubsky P, Fitzal F, Bjelic-Radisic V, Steger G, Greil R, Marth C, Kubista E, Samonigg H, Wohlmuth P, Mittlböck M, Jakesz R (2008) Adjuvant endocrine therapy plus zoledronic acid in premenopausal women with early-stage breast cancer: 5-year follow-up of the ABCSG-12 bone-mineral density substudy. Lancet Oncol 9(9):840–849. https://doi.org/10.1016/S1470-2045(08)70204-3
Gnant MFX, Mlineritsch B, Luschin-Ebengreuth G, Grampp S, Kaessmann H, Schmid M, Menzel C, Piswanger-Soelkner JC, Galid A, Mittlboeck M, Hausmaninger H, Jakesz R (2007) Zoledronic acid prevents cancer treatment-induced bone loss in premenopausal women receiving adjuvant endocrine therapy for hormone-responsive breast cancer: a report from the Austrian Breast and Colorectal Cancer Study Group. J Clin Oncol 25(7):820–828. https://doi.org/10.1200/jco.2005.02.7102
Shapiro CL, Manola J, Leboff M (2001) Ovarian failure after adjuvant chemotherapy is associated with rapid bone loss in women with early-stage breast cancer. J Clin Oncol 19(14):3306–3311
Delmas PD, Balena R, Confravreux E, Hardouin C, Hardy P, Bremond A (1997) Bisphosphonate risedronate prevents bone loss in women with artificial menopause due to chemotherapy of breast cancer: a double-blind, placebo-controlled study. J Clin Oncol 15(3):955–962
Leslie WD (2012) Ethnic differences in bone mass—clinical implications. J Clin Endocrinol Metab 97(12):4329–4340. https://doi.org/10.1210/jc.2012-2863
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the Ethical Standards of the Institutional and/or National Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kim, M., Kim, H., Ahn, S.H. et al. Changes in bone mineral density during 5 years of adjuvant treatment in premenopausal breast cancer patients. Breast Cancer Res Treat 180, 657–663 (2020). https://doi.org/10.1007/s10549-020-05566-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05566-w