Abstract
Purpose
In recent years, routine excision of papillary neoplasms (PN) of the breast has been questioned and controversy exists over when excision is necessary. The aim of this study was to evaluate the upstage rate to malignancy of core needle biopsy (CNB) diagnosed PNs from multiple diagnostic centers in our area and to identify factors predictive of malignancy.
Methods
Patients presenting to our surgical center between 2013 and 2017 for excision of CNB PN were evaluated. The primary endpoint was upstage to malignancy. The association of age, diagnostic center where CNB performed, type of CNB, palpability, discharge, clinical exam size, imaging size, family history of breast cancer, and presence of atypia, as risk factors for upstaging to cancer were also evaluated.
Results
Of the 317 PN cases, 83 upstaged to malignancy following surgical excision. 77% of patients with CNB of Atypical PN upstaged, 39% of PN with concurrent atypical ductal hyperplasia, and 0% of PN with concurrent atypical lobular hyperplasia/flat epithelial atypia. Of the 206 non-atypical PNs on CNB, 3.4% upstaged to malignancy, but further review demonstrated a 1% upstage rate when atypia excluded. Factors found to be associated with malignancy included: older patient age, larger size, and presence of atypia.
Conclusion
We recommend excision of PN with atypia, concurrent cancerous lesion, or radiologic–pathologic non-concordance, and serial imaging follow up may be considered for image detected PN, less than 1 cm, with no atypia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Management of breast lesions has changed significantly over the past 20 years with the minimally invasive core needle biopsy (CNB) replacing routine surgical biopsy for diagnosis. However, it is recognized that core needle biopsy may under sample an area of abnormality in some circumstances and these are termed high-risk lesions. Although high-risk lesions themselves are benign, due to under sampling there may be an area of associated malignancy that gets missed. As such, these lesions can potentially be “upstaged” to malignancy after surgical removal of the entire area.
Papillary neoplasms (PN) of the breast are classified as one of these high-risk lesions. These lesions are characterized by the presence of epithelial proliferation in the ducts of the mammary glands supported by fibrovascular cores [1]. Although the presence of these fibrovascular cores is the hallmark feature of PNs of the breast, PN represents a heterogenous group of diseases ranging from benign, atypical, and malignant lesions [1].
Traditionally, CNB diagnosed PNs have been surgically excised due to risk of under sampling potentially missing a malignancy. Because surgery poses risks to patients in addition to general discomfort, there is a trend toward less invasive management. More recently, the necessity for routine excision of papillary neoplasms has been called into question; however, controversy still exists regarding under what circumstances excision is required. Current literature reports variable upstage rates following surgical excision of CNB diagnosed PNs, ranging from 0.8 to 33% [2,3,4,5,6,7]. Additionally, many of these studies are single institutional meaning imaging, CNB, and surgical pathology are all done at one location, which limits the generalizability of results. The aim of this study was to evaluate the upstage rates of CNB diagnosed PN from multiple diagnostic centers across our metropolitan region to identify factors predictive of malignancy, and to identify a group of patients at low risk of malignancy.
Methods
Ethics was obtained from Providence Health Care Review Board for this study. Patient information was de-identified and coded
In our region, patients with breast complaints or abnormal screening mammograms have diagnostic workups at multiple diagnostic centers and are then referred by their primary care physician for surgical management. Patients having excision of papillary neoplasms between 2013 and 2017 at Mount St. Joseph Hospital were identified from prospectively collected surgical data. Diagnosis, clinical, and radiological data were confirmed and expanded by chart review. Clinical details were taken from surgeon’s reports. Imaging and CNB pathology details were taken from reports in the surgeon’s chart. Diagnostic work up was performed at 18 breast diagnostic imaging facilities with CNB pathology performed at nine different hospitals in our regional area. The technique for CNB was at the discretion of the radiologist and equipment at different facilities varies. CNB devices include spring loaded and vacuum assisted models ranging in size from 9–16 guage. Stereocore is available at four facilities and US guided CNB at all facilities performing CNB. CNB pathology is not reviewed preoperatively unless there is a particular clinical concern. All surgery and surgical pathology were performed at our regional hospital.
The primary endpoint was the frequency at which malignancy (DCIS or invasive disease) was identified after complete surgical excision. The association of age, diagnostic center where core biopsy was performed, the type of biopsy performed, palpability, discharge, clinical exam size, imaging size, family history of breast cancer, and presence of atypia, as risk factors for upstaging to cancer were also evaluated. Statistical analyses used the Chi square test for categorical variables and the student t test for continuous variables. Multivariate analysis was performed using logistic regression. Significance was set at p < 0.05.
Results
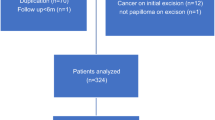
During the study period 317 patients were identified as having CNB diagnosis of PN, with 206 patients having PN without atypia, 92 having an atypical papillary neoplasm (APN), 13 having PN with Atypical Ductal Hyperplasia (ADH), and 6 having PN with either Atypical Lobular Hyperplasia (ALH) or Flat Epithelial Atypia (FEA). Table 1 demonstrates the clinical presentation for each of the four CNB diagnoses and Fig. 1 presents the final diagnosis and the upstage rates.
Core needle biopsy diagnosis and final excision diagnosis. The X-axis represents diagnosis on core needle biopsy, Y-axis represents the number of cases, and each of the stacking bars indicates the final excisional diagnosis. The numbers on top each column represent the number of upstaged cases (DCIS or invasive carcinoma on final diagnosis) along with the percent of upstaged cases., PN papillary neoplasm, ADH atypical ductal hyperplasia, FEA flat epithelial atypia, ALH atypical lobular hyperplasia, DCIS ductal carcinoma in situ
Eighty-three patients were upstaged to malignancy (26.2%), with 21 of these diagnosed with invasive ductal cancer, 14 encapsulated papillary carcinoma, 41 ductal carcinoma in situ (DCIS), and 1 invasive lobular cancer. The upstage rate for patients diagnosed with APN on CNB was 77.2%, 38.5% for CNB diagnosed PN with ADH, and 0% for CNB diagnosed PN with ALH or FEA.
When all APNs, ADH, and ALH/FEA were excluded from analysis, 7 non-atypical PN were found to have upstaged to malignancy, thus the upstage rate of non-atypical PN was 3.4%. On further review of the CNB reports of these seven non-atypical PN cases, it was found that only one of these seven cases had a CNB pathology report that specified the absence of histological atypia, whereas the remaining six cases did not specify on the pathology report the presence or absence of atypia. These 7 cases classified in our initial analysis as no atypia were reviewed by a pathology member of the study team (AO). On review of the CNB slides two lesions were atypical and three had features concerning for atypia, but staining with CK 5/6 had not been done. One “no comment” case was not atypical on review. This was a 77 year old who had a contralateral cancer diagnosed simultaneously. At surgical excision a benign papilloma was identified with an incidental finding of DCIS in the specimen. The one case that the CNB report had indicated “no atypia” was a 15 mm palpable lesion in a 72 year old but we were unable to obtain the CNB slides. Therefore, only two of these upstaged cases can truly be classified as “no atypia”, and thus the upstage rate for PN with no atypia on CNB becomes 1%.
On univariate analysis upstage to malignancy was associated with presence of atypia, a palpable mass, larger lesion size and older age, while family history of breast cancer, presence of discharge and the type of CNB performed was not predictive of malignancy (Table 2). On further analysis of the clinical exam sizes, it was found that the upstage rates of the various sized lesions differed significantly for both physical exam size and imaging size. Analysis of PN upstage rates in association with the diagnostic center at which CNB was performed and revealed a variation ranging from 0 to 73% (p = 0.019) (Table 3). Multivariate analysis was significant for atypia, imaging size of lesion, and older age (Table 4).
Discussion
In recent years, the necessity for routine excision of PN of the breast has been called into question. Current literature reports variable upstage rates to malignancy of CNB diagnosed PN; however, there seems to be an emerging consensus that PN with associated histological atypia require excision because of their high association with malignancy [4, 8, 9]. The management of non-atypical PN still remains controversial, with some studies recommending excision [3, 10,11,12,13] and others favoring conservative management [2, 4,5,6,7,8,9].
Pareja et al. [7] examined the association of imaging size of the PN and upstaging to malignancy and concluded that observation is appropriate for PNs with no atypia and radiologic-pathologic concordance, regardless of size. This study along with Khan et al. [4] both concluded that palpability of the mass and presence of nipple discharge were not predictive of upstaging. In contrast, Han et al. [6] found that the presence of contralateral breast cancer, clinical symptoms manifesting as nipple discharge and/or palpable mass, and multifocality were associated with upstaging to malignancy. Similarly, Hong et al. [5] found that age, size on ultrasound, and density on mammography were associated with upstaging, specifically patients older than 54 years, and a lesion size greater than 1 cm.
Additionally, many of these studies are single institutional [3,4,5,6,7, 10] which limits the generalizability of results to other regions and centers.
Because our regional center is uniquely set up to serve as a central intake for breast complaints across our regional area, this current study serves as a multi-centered analysis of CNB diagnoses from different diagnostic centers, thus providing us a sample more representative of the population across our region. Furthermore, the multi-centered design of this study takes into account that each diagnostic center has its own staff of several radiologists and pathologists who are reviewing the cases. This minimizes potential confounding effects of individual radiologist/pathologist bias on review of cases at a single institution. The results from this study are similar to conclusions drawn from the single-centered studies [4, 6, 7, 10] which aids in validating the external validity of these studies. Most importantly, this study will be useful to guide management of PNs in our region.
In our study, we looked at a sample of 317 patients diagnosed with PN on CNB and sorted these patients into four groups (APN, PN + ADH, PN + ALH/FEA, PN with no atypia) in order to accurately assess the upstage rates by eliminating potential confounding variables. The results from this study are largely in agreement with the general consensus that APN and PN + ADH have a high association with upstage to malignancy, while PN with no atypia have a low risk of upstaging [2, 4,5,6,7,8,9]. Rakha et al. [1] noted that “the presence of atypia in the form of ADH, FEA, or lobular neoplasm in papilloma is expected to have a relative risk of invasive malignancy similar to that of atypia elsewhere in the breast when they occur as pure forms.” The data reported from our regional center are in agreement with this statement as the upstage rates of PN + ADH were found to be high and very similar to the upstage rates of ADH alone reported both in literature and from our center [14, 15]. Similarly, PN + ALH/FEA upstage rates in this study were also found to be low and similar to the upstage rates of ALH/FEA alone reported in both literature and from our center [15, 16].
As mentioned previously, of the 83 cases that were found to upstage, seven of these did not have atypia reported on the CNB. On further analysis of these 7 cases by in house pathology review, it was found that only two of these cases really met the criteria for no atypia. Review of the two cases without atypia that upstaged to cancer revealed that both patients had presenting features that would have made them higher risk to upstage (older age, palpable lesion over 1 cm, contralateral cancer). Because of these risk factors [6] these PNs would have been flagged for removal at our center regardless of associated radiological and histological features. The CNB pathology of the six “no atypia comment” cases were from a time when there was routine excision of PNs, and therefore comments about atypia and staining to assess for atypia was not done. On review, these five cases were found to have histology of concern that currently would prompt additional staining that would have defined the lesions as atypical. This information is interesting to note as it reflects how trends in the management of certain breast lesions can influence the reporting on pathology notes, which can then influence the surgeon’s final decision on whether to excision the lesion.
An in-depth review of papillary lesions from a pathologic perspective is beyond the scope of this article but has been reviewed by Agoumi [17]. In the past, most institutions employed reflex excisions for almost any papillary lesion in a core needle biopsy (CNB). Currently, using routine staining with additional specific immunohistochemistry and correlation with imaging, pathologists can now identify “atypical” papillary lesions that require excisional biopsy, sparing many patients surgery [18,19,20,21,22,23]. The more specific the diagnosis on CNB, the more useful the information for management decisions; for example, a generic “atypical” papillary lesion is less informative than papillary lesion with ADH or DCIS. However, even the generic atypical papillary lesion is better than no qualification of papillary lesions that does not allow triaging for management. The minimal histology required to call a lesion papillary is a fibrovascular core lined by epithelium. The presence or absence of a myoepithelial cell layer (MEC) and presence or absence of atypical epithelial cyto/architectural features define and, in some cases, allow more specific subclassification of atypical papillary lesions [24, 25].
Intraductal papillomas typically are composed of fibrovascular structures lined by two layers of cells, luminal ductal epithelium and a basal MEC. Epithelial proliferation in the form of usual ductal hyperplasia can be present in papillomas. The presence of atypical epithelial cyto/architectural features especially if combined with lack of high molecular weight keratin staining and strong ER staining suggest either ADH or DCIS in a papilloma. There is controversy in the definition of ADH vs. DCIS in both papillary and non-papillary breast pathology. The WHO consensus statement recommends a cut-off of 3 mm [26,27,28,29].
Other malignant papillary lesions that can be at least suggested on CNB are encapsulated papillary carcinoma, solid papillary carcinoma and much less common, true invasive papillary carcinoma. The first demonstrates papillary architecture without MEC staining, both within papillae and at lesion margin, the second, similar but predominantly solid architecture and frequent neuroendocrine marker positivity and the last a variant of invasive ductal carcinoma.
Diagnosis of papillary lesions on CNB is challenging with a small sample and classification of papillary lesions on CNB into papillary lesions with ADH, atyptical papillary lesions, and malignant papillary lesions is controversial. Although we reported atypical papillary lesions and papillary lesions with ADH on CNB separately these entities are not always separated. As our CNB pathology comes from nine pathology departments there may be differences in reporting these two categories and even though the papillary lesions with ADH did not show significance on the multivariate analysis we would still recommend excision of these lesions for this reason. Knowledge of institutional upgrade rates allows surgeons and patients to make decisions with a better understanding of specific risks.
This study has some limitations. First, although much of the data for this study were collected prospectively, some of the earlier data were filled in by chart review which introduces the limitations of retrospective data. However, the process of chart review allowed us to gather the information that the surgeons had for decision making and gave us a more complete data set than using only the prospectively collected information. We did not arrange for central review of all imaging and pathology as we wanted to look at the upstage risk based on information surgeons’ use in clinical practice.
For both prospectively collected and chart reviewed data there was information missing for some of the cases such as a quantitative value for clinical exam size and imaging size. This has to due in part with the variability of reporting between surgeons and the different diagnostic centers as some reports will simply say “small mass” or “mass” without providing a size specification. This limitation is very much a reflection of real time clinical practice as there is often missing information from reports. Since this study has shown that the larger palpable lesions are associated with upstaging, it is especially important to educate the centers to report size information to help determine course of management. Having this information available at the time of surgical consultation will avoid surgeons needing to go back to radiology and pathology to get more details and therefore facilitate management of patients. We did note that many of the unknown sizes and no comments on atypia were in reports from 2013 to 2014. More recent radiology and pathology reports tend to be more detailed and this is an indication of evolving practices that play an important role in surgical decision making.
Additionally, this study did not follow patients who did not have surgical excision of their PNs or other patients in the region that had surgery at different centers. The study group was defined by patients having surgical excision at our center, so we do not know how many patients were managed non-operatively and we do not know the outcomes for those patients who did not have a surgical excision. Although our center has a large breast surgical volume (more than 20% of procedures in our province [30]), referral patterns are not fixed so not all patients in our region would have surgery at our center, and we do not have the outcomes for those patients.
Following multidisciplinary discussion of our findings across our region, we have developed a clinical approach for patients with CNB diagnosis of PN. We are recommending surgical excision of PN with histological atypia, ADH, a concurrent cancerous lesion, or radiologic-pathologic non-concordance. Serial imaging follow up may be considered for image detected PN, less than 1 cm, with no histological atypia. Applying this clinical rule to the population of this study, even considering the varying radiologists and pathologists from different institutions, none of the cases that upstaged to cancer would have been missed. This includes the non-atypical PN case and the six “no atypia comment” cases, as each was either greater than 1 cm in size or had a concurrent contralateral cancer. However, it is recommended that the absence of atypia be explicitly confirmed by the pathologist before considering conservative management as the presence of atypia was the strongest association with upstaging to malignancy.
Conclusion
Traditionally, CNB diagnosed PNs have been surgically excised due to risk of under sampling potentially missing a malignancy. This study demonstrated that while APN and PN with concurrent ADH have a high rate of malignancy (77.2% and 38.5%, respectively), non-atypical PN and PN with concurrent ALH/FEA in contrast have a low rate of malignancy (1% and 0%, respectively). Based on the results of this study we recommend surgical excision of PN with histological atypia, ADH, concurrent cancerous lesion, or radiologic-pathologic non-concordance, and serial imaging follow up may be considered for image detected PN, less than 1 cm, with no histological atypia. To optimize surgical decision making we recommend that diagnostic imaging reports comment on the size of the lesion identified, details of the CNB including size, number of passes, and completeness of removal and that the pathology reports specifically comment on the presence or absence of Atypia.
Abbreviations
- ADH:
-
Atypical ductal hyperplasia
- ALH:
-
Atypical lobular hyperplasia
- APN:
-
Atypical papillary neoplasms
- CNB:
-
Core needle biopsy
- DCIS:
-
Ductal carcinoma in situ
- FEA:
-
Flat epithelial atypia
- MEC:
-
Myoepithelial cell layer
- PN:
-
Papillary neoplasms
References
Rakha EA, Ellis IO (2018) Diagnostic challenges in papillary lesions of the breast. Pathology 50:100–110. https://doi.org/10.1016/j.pathol.2017.10.005
Menes TS, Rosenberg R, Balch S, Jaffer S, Kerlikowske K, Miglioretti DL (2014) Upgrade of high-risk breast lesions detected on mammography in the breast cancer surveillance consortium. Am J Surg 207:24–31. https://doi.org/10.1016/j.amjsurg.2013.05.014
Shiino S, Tsuda H, Yoshida M et al (2015) Intraductal papillomas on core biopsy can be upgraded to malignancy on subsequent excisional biopsy regardless of the presence of atypical features. Pathol Int 65:293–300. https://doi.org/10.1111/pin.12285
Khan S, Diaz A, Archer KJ et al (2018) Papillary lesions of the breast: to excise or observe? Breast J 24:350–355. https://doi.org/10.1111/tbj.12907
Hong YR, Song BJ, Jung SS et al (2016) Predictive factors for upgrading patients with benign breast papillary lesions using a core needle biopsy. J Breast Cancer 19:410–416. https://doi.org/10.4048/jbc.2016.19.4.410
Han SH, Chung YR, Yun BL et al (2018) Benign Intraductal Papilloma without atypia on core needle biopsy has a low rate of upgrading to malignancy after excision. J Breast Cancer 21:80–86. https://doi.org/10.4048/jbc.2018.21.1.80
Pareja F, Corben A, Brennan S et al (2016) Breast intraductal papilloma without atypia in radiologic-pathologic concordant core needle biopsies: rate of upgrade to carcinoma at excision. Cancer 122:2819–2827. https://doi.org/10.1002/cncr.30118
Padilla-Thornton A, Farrell J, Gordon P et al (2018) Current evaluation of breast health concerns and diagnosis of breast cancer. BCMJ 60:27–32
Wen X, Cheng W (2013) Nonmalignant breast papillary lesions at core-needle biopsy: a meta analysis of underestimation and influencing factors. Ann Surg Oncol 20:94–101. https://doi.org/10.1245/s10434-012-2590-1
Boin DP, Baez JJ, Guajardo MP et al (2014) Breast papillary lesions: an analysis of 70 cases. Ecancermedicalscience 8:461. https://doi.org/10.3332/ecancer.2014.461
Rizzo M, Lund MJ, Opera G, Schniederjan M, Wood WC, Mosunjac M (2008) Surgical follow-up and clinical presentation of 142, breast papillary lesions diagnosed by ultrasound-guided core-needle biopsy. Ann Surg Oncol 15:1040–1047. https://doi.org/10.1245/s10434-007-9780-2
Ashkenazi I, Ferrer K, Sekosan M et al (2007) Papillary leisons of thebreast discovered on percutaneous large core vacuum-assisted biopsies: reliability of clinical and pathological parameters in identifying benign lesions. Am J Surg 194:183–188. https://doi.org/10.1016/j.amjsurg.2006.11.028
Cyr AE, Novack D, Trinkaus K et al (2011) Are we overtreating papillomas diagnosed on core needle biopsy? Ann Surg Oncol 18:946–951. https://doi.org/10.1245/s10434-010-1403-7
Sidhu R, MacKay E, Warburton R, Pao J, Kuusk U, Dingee C, McKevitt E (2018) Upstage to breast cancer after excision of atypical ductal hyperplasia on core needle of the breast-a regional experience. Ann Surg Oncol 25(2_suppl):341–342
The American Society of Breast Surgeons (2016) Consensus guidelines on concordance assessment of image-guided breast biopsies and management of borderline or high-risk lesions. The American Society of Breast Surgeons. https://www.breastsurgeons.org/docs/statements/Consensus-Guideline-on-Concordance-Assessment-of-Image-Guided-Breast-Biopsies.pdf. Accessed Mar 2019
Becker AK, Gordon PB, Harrison DA, Hassell PR, Hayes MM, Niekerk D, Wilson CM (2013) Flat ductal intraepithelial neoplasia IA diagnosed at stereotactic core needle biopsy: is excisional biopsy indicated? AJR Am J Roentgenol 200:682–688. https://doi.org/10.2214/AJR.11.8090
Agoumi M, Giambattista J, Hayes MM (2016) Practical considerations in breast papillary lesions: a review of the literature. Arch Pathol Lab Med 140:770–790. https://doi.org/10.5858/arpa.2015-0525-RA
Tse GM, Tan PH, Lui PC et al (2007) The role of immunohistochemistry for smooth-muscle actin, p63, CD10, and cytokeratin 14 in the differential diagnosis of papillary lesions of the breast. J Clin Pathol 60:315–320. https://doi.org/10.1136/jcp.2006.036830
Zhang H, Xiong Y, Zhang S, Zhang Y, Wang YH, Li T (2011) Clinicopathologic and immunohistochemical study of 187 cases of intraductal papillary neoplasm of breast [in Chinese]. Zhonghua Bing Li Xue Za Zhi 40:726–731. https://doi.org/10.3760/cma.j.issn.0529-5807.2011.11.002
Omi Y, Yamamoto T, Okamoto T, Obara T, Kobayashi M (2011) A useful immunohistochemical approach to evaluate intraductal proliferative lesions of the breast and to predict their prognosis. Histol Histopathol 26:79–86. https://doi.org/10.14670/HH-26.79
Tse GM, Tan PH, Moriya T (2009) The role of immunohistochemistry in the differential diagnosis of papillary lesions of the breast. J Clin Pathol 62:407–413. https://doi.org/10.1136/jcp.2008.06301
Tan PH, Aw MY, Yip G et al (2005) Cytokeratins in papillary lesions of the breast: is there a role in distinguishing intraductal papilloma from papillary ductal carcinoma in situ? Am J Surg Pathol 29:625–632. https://doi.org/10.1097/01.pas.0000157941.88161.39
Grin A, O’Malley FP, Mulligan AM (2009) Cytokeratin 5 and estrogen receptor immunohistochemistry as a useful adjunct in identifying atypical papillary lesions on breast needle core biopsy. Am J Surg Pathol 33:1615–1623. https://doi.org/10.1097/PAS.0b013e3181aec446
Schnitt S, Collins L (2008) Papillary lesions. In: Epstein JI (ed) Biopsy interpretation of the breast. Wolters Kluwer, Philadelphia, pp 205–235
Tavassoli F, Devilee P (1999) Papillary lesions. In: Tavassoli F (ed) Pathology of the Breast, 2nd edn. McGraw-Hill, New York, pp 325–372
Tan PH, Schnitt SJ, van der Vijver MJ, Ellis IO, Lakhani SR (2015) Papillary and neuroendocrine breast lesions: the WHO stance. Histopathology 66:761–770. https://doi.org/10.1111/his.12463
Page DL, Salhany KE, Jensen RA, Dupont WD (1996) Subsequent breast carcinoma risk after biopsy with atypia in a breast papilloma. Cancer 78:258–266. https://doi.org/10.1002/(SICI)1097-0142(19960715)78:2%3c258:AID-CNCR27%3e3.0.CO;2-V
Lewis JT, Hartmann LC, Vierkant RA et al (2006) An analysis of breast cancer risk in women with single, multiple, and atypical papilloma. Am J Surg Pathol 30:665–672
Putti TC, Pinder SE, Elston CW, Lee AH, Ellis IO (2005) Breast pathology practice: most common problems in a consultation service. Histopathology 47:445–457. https://doi.org/10.1111/j.1365-2559.2005.02246.x
McKevitt E, Warburton R, Pao J, Kuusk U, Dingee C, Brown C (2017) Breast cancer surgery wait times exceeding targets with current OR allocation methodology. Meeting of the British Columbia Surgical Society, Parksville, BC, May 2017
Acknowledgements
The authors would like to acknowledge the input of the physicians in the Departments of Pathology, Surgery, and Radiology in our area that contributed to the development of our clinical pathways. We would also like to acknowledge Guilaine Boyce who helped with manuscript preparation and Kaidi Liu, Leo Chen, and Amy Wang who helped with data analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors of this manuscript have no conflicts of interest to declare for this publication.
Ethical approval
This study was approved by the Research Ethics Board by the University of British Columbia and Providence Health Care. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained as appropriate from all participants in the study as per the Research Ethics Board Standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, C., Sidhu, R., Ostry, A. et al. Risk of malignancy in papillary neoplasms of the breast. Breast Cancer Res Treat 178, 87–94 (2019). https://doi.org/10.1007/s10549-019-05367-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-019-05367-w