Abstract
Background
There are concerns regarding local toxicity when IORT is applied in Asian women with a smaller breast volume than that of Western women. Trials are required to develop safety profiles for this technique. The aim of this trial was to evaluate acute toxicity after intra-operative radiotherapy (IORT) with low-energy X-ray plus whole breast irradiation (WBI) in Asian patients with breast cancer.
Methods
This single-arm, single-institute, phase II trial investigated acute toxicity after completion of radiotherapy (targeted IORT followed by WBI) in Korean patients treated with breast-conserving surgery (BCS). In the conventional WBI arm from the TARGIT-A trial, the incidence of acute toxicity within 6 months was 15%. To prove the non-inferiority of the acute toxicity rate, 215 patients were required. This trial is registered with ClinicalTrials.gov (NCT02213991).
Results
Two-hundred and fifteen women were enrolled, and 198 underwent IORT. In 33 patients, clinically significant complications during the acute period were noted. The incidence of acute toxicity was 16.7% (95% CI 11.5–21.9%). There were 29 patients with seroma needing more than 3 aspirations, 4 with wound infection, and 2 with skin breakdown. There was no difference in the rate of complications according to the tumor volume or the tumor-breast volume ratio. Advanced age and high BMI were risk factors for acute complications.
Conclusions
Targeted intra-operative radiotherapy using Intrabeam® is a safe procedure for Korean patients with breast cancer with an acceptable toxicity profile in the acute period.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast-conserving therapy (BCT) has markedly improved the quality of life for patients with breast cancer in terms of psychosocial sequelae as well as body image [1]. Until now, sequential treatment with breast-conserving surgery (BCS) followed by whole breast irradiation (WBI) has been the standard BCT. In light of robust evidence that WBI reduces breast cancer mortality as well as local recurrence [2], WBI is an essential component of BCT for patients undergoing BCS.
Meanwhile, it had been repeatedly observed that most local recurrences in the conserved breast occur in the original tumor cavity [3,4,5,6]. These observations have triggered the idea of accelerated partial breast irradiation (APBI), which focuses the radiation on the tumor-bed and deescalates WBI [7, 8]. Given the results of several randomized clinical trials comparing APBI with conventional WBI [9,10,11,12], the use of APBI outside the framework of a clinical trial is recommended for carefully selected patients with early breast cancer. One alternative to conventional WBI is boost radiotherapy followed by reduced-dose WBI, a risk-reducing approach that is applicable to most patients treated with BCS [13,14,15,16,17].
The TARGIT-A trial showed that APBI using concurrent intra-operative radiotherapy (IORT) with low-energy X-ray and lumpectomy using a risk-adapted approach could be considered as an option for eligible patients with early breast cancer [10, 12]. To introduce IORT in daily practice for Asian breast cancer patients, safety profiles for this new technique are required from clinical trials with Asian women since they have smaller breast volumes than those of Western populations. Acute and late local toxicities after IORT may limit the widespread use of this technique in Asian patients because IORT might affect the wound-healing process.
To evaluate acute toxicity after IORT with low-energy X-ray followed by WBI in Asian patients with breast cancer, a single-arm, phase II trial was conducted in Korean women with breast cancer who were treated with BCS. IORT using a low-energy X-ray device (Intrabeam®) with a dose of 20 Gy replaced boost WBI in this study.
Methods
Study design and participants
In this phase 2, single-arm trial, we investigated short-term local toxicity within 6 months after completion of IORT with low-energy X-ray followed by WBI in Korean patients with breast cancer. The primary end-point was the incidence of local toxicity, evaluated 4–6 months after completion of radiotherapy. Eligible patients were women who were aged 20 years or older, were eligible for lumpectomy, and had ductal carcinoma in situ (DCIS) or invasive carcinoma (Stage I–III). Patients treated with pre-operative chemotherapy or having metastatic disease were excluded. Targeted intra-operative radiotherapy (TARGIT) as a concurrent procedure with lumpectomy or as a secondary procedure after the first lumpectomy was allowed. The presence of invasive carcinoma and DCIS in the resection margin was intra-operatively assessed by the frozen pathologic examination.
The institutional review boards approved the trial according to their local laws and regulations. All patients gave written informed consent, and the trial was conducted in compliance with the Helsinki Declaration. This trial is registered with ClinicalTrials.gov, number NCT02213991.
Radiation procedures
For adjuvant radiotherapy, all patients underwent TARGIT for boost radiotherapy followed by WBI at 46 Gy in 23 fractions. We utilized the same procedure for TARGIT as that followed in the TARGIT-A trial, which was described in our previous report [18]. Two surgeons conducted all BCS procedures. After lumpectomy and excision of the shaved margins, a single fraction of 20 Gy was delivered to the surface of the tumor-bed using the mobile 50-kV X-ray source (Intrabeam®, Carl Zeiss, Oberkochen, Germany) in the operating room. Isotropy and the output of the unit were verified; the pre-IORT calibration process required by the system was carried out prior to each case. A spherical applicator of an appropriate diameter (ranging from 1.5 to 5.0 cm in 0.5 cm increments) was selected depending on the volume of the cavity, and the applicator was connected over the probe of the X-ray source. With a sterile sheath draped over the IORT device to prevent contamination, the applicator was placed inside the tumor cavity, and a purse-string suture was used to pull the walls of the tumor cavity tightly against the applicator surface. The edges of the skin incision were everted so any part of skin was at least 1 cm away from the applicator surface to avoid excessive radiation exposure. When the skin-to-tumor distance was less than 1 cm, the portion of the skin overlying the tumor was excised to prevent suboptimal radiation dose delivery to the high-risk area due to eversion of the skin edge. The actual beam-on time after radiation site shielding varied from 20 to 30 min, according to the applicator size.
For intra-operative margin assessment, frozen sections of shaved margins in 4 directions (superior, inferior, lateral, and medial) were sent to the Department of Pathology. Re-excision was performed in cases of positive resection margins on frozen examination.
In addition, patients diagnosed with cancer at the first excision of breast lesions were included and treated with TARGIT in the second operation. For those patients, the IORT procedure was identical to that of patients treated with concurrent IORT. For patients with pathologic nodal involvement, regional radiotherapy was simultaneously delivered with WBI.
3D MRI volumetry
All patients underwent pre-operative magnetic resonance imaging (MRI). Based on pre-operative MRI, we obtained breast volume, tumor volume, and the tumor-breast volume ratio by 3D-Doctor software (Able Software Corp, Lexington, USA). The tumor volume and tumor-breast volume ratio were measured in 159 patients who had a single lesion without non-mass enhancement. Volume computation was performed on contrast-enhanced T1-weighted images, subtracting layers thicker than 2 mm. Manual measurements of the breast tissue and tumor portions were performed in each axial image along the outside breast and on the dorsal aspect of the pectoral muscle (Supplementary Fig. 1). After measurement of the breast tissue and the tumor portion on all axial images, the 3D-Doctor software automatically calculated the volume.
Statistics
The principal end-point specified in the protocol was the incidence of local toxicity, evaluated 4–6 months after completion of radiotherapy. In the previous RCT comparing TARGIT with EBRT, the rate of all complications in EBRT group (n = 1119) was 15.5% [12]. We aimed to demonstrate a non-inferiority of IORT with low energy in terms of complications in Korean patients. A sample size of 195 achieves 80% power to detect a non-inferiority proportion (P0) of 0.2300 using a one-sided binomial test for non-inferiority. The target significance level is 0.0250. The actual significance level achieved by this test is 0.0238. These results assume that the actual proportion (P1) is 0.1500. Considering a drop-out rate of 10%, the trial would need to enroll 215 patients in total.
The pre-specified checklist of complications highlighting local toxicity was used in our trial, adopting that of TARGIT-A trial: (i) Hematoma needing surgical evacuation, (ii) Seroma needing more than three aspirations, (iii) Skin breakdown or delayed wound-healing, (iv) Any complication needing surgical intervention, (v) Radiation Therapy Oncology Group (RTOG version 2.0) toxicity grade 3 or 4 for dermatitis, telangiectasia, pain in the irradiated field, or other, and (vi) Any complication of RTOG toxicity grade more than 2.
A multiple logistic-regression model was employed to identify factors affecting local toxicity. Significant factors in the univariate analysis were entered into the multivariate model. SPSS software version 18 (SPSS Inc., Chicago, IL, USA) was used to perform the statistical analyses.
Results
Baseline characteristics
Between August 2014 to September 2016, 215 women with early breast cancer were enrolled, of which 198 underwent IORT (Fig. 1). One-hundred and 85 patients (93.4%) received concurrent TARGIT, while 13 (6.6%) underwent TARGIT as a second procedure. The most common technical reasons for drop-out were insufficient surrounding parenchymal tissue and a large tumor cavity ineligible for TARGIT application. The size of the applicators and the actual beam-on time are presented online (Supplementary Fig. 2).
Consort diagram according to REMARK criteria. Two-hundred and fifteen women were enrolled. Seventeen patients dropped out of the trial (withdrawal of consent, 5; conversion to mastectomy, 3; large tumor cavity, 4; insufficient surrounding tissue, 2; refusal of whole breast irradiation, 2). Finally, 198 patients were included in the analysis (185 underwent concurrent intra-operative radiotherapy and 13 underwent intra-operative radiotherapy as a second procedure). IORT intra-operative radiotherapy
Demographic and clinical characteristics are presented in Table 1. The median age and pathologic tumor size were 52 (27–79) years old and 1.5 cm (0.1–4.0), respectively. The distributions of tumor stages were 14.1% for DCIS, 58.1% for stage I, 26.3% for stage II, and 1.5% for stage III. Twenty-five patients (12.6%) had node-positive disease. Adjuvant chemotherapy was administered to 37.4% (74 of 198) of the patients, and 7.1% (14 of 198) underwent concurrent lymph node irradiation. The incidence of ER-positive and HER2-positive disease was 77.8% (154 of 198) and 13.6% (27 of 198), respectively.
The primary end-point
Clinically significant complications developed within 6 months in 33 patients after completion of radiotherapy. Acute toxicity occurred in 16.7% (95% CI 11.5–21.9%) of patients (Table 2). The actual non-inferiority margin of our trial was 21.9%, lower than the pre-specified margin of 23.0% (Fig. 2). In detail, there were 27 seromas needing more than 3 aspirations (aspirated volume was over 10 cc), 4 wound infections, and 2 wound dehiscences. Of all 33 events, the median time gap to complications was 11 days (range 6–94) after TARGIT. Except seroma collections, the acute complication rate was very low (3.0%). Photographs in two cases with wound complications are presented online (Supplementary Fig. 3).
Factors affecting complications
We aimed to identify factors affecting complications during a short-term follow-up period. Age, body mass index (BMI), and underlying diabetes mellitus (DM) were analyzed in relation to the incidence of toxicity. In addition, breast volume, tumor volume, and the tumor-breast volume ratio were assessed by pre-operative breast MRI.
In the univariate analyses using a logistic-regression analysis, these factors were analyzed as continuous variables in relation to complications. Age, BMI, DM, tumor volume, and breast volume were associated with complications (Table 3). However, multivariate analysis showed that only age and BMI were independent factors associated with complications, indicating that advanced age and a high BMI may increase the risk of acute complications (Table 3).
Moreover, we noted that local toxicity frequently developed in patients with a large breast volume. When this complication was analyzed according to the quartiles of breast volume, the 1st (lowest) quartile had no complications, but there was no significant difference between the 2nd, 3rd, and 4th quartiles (Supplementary Table 1).
Furthermore, we compared risk factors according to the complication rate. In the complication group (N = 33), the mean age and BMI were significantly higher. In addition, the mean breast volume was significantly higher in patients with complications than in those without complications, whereas the mean tumor volume and tumor-volume ratio did not differ according to the incidence of acute complications (Supplementary Fig. 4).
Discussion
Our study demonstrated that TARGIT as boost radiotherapy can be a safe procedure for Asian patients with early breast cancer in terms of early toxicity. Although all patients underwent WBI in addition to IORT, the early toxicity rate of our patients was not higher than that of those treated with EBRT. There is a paucity of data, as there are few reports regarding the use of IORT in Asian women. A phase I/II trial reported that IORT using Mobetron® is technically feasible for Japanese women [19]. Another IORT study using Intrabeam® in Chinese women evaluated irradiation to the nipple base in patients undergoing nipple-sparing mastectomy [20]. Our results can mitigate concerns regarding wound complications associated with IORT in patients having small breasts, including Asian women.
In addition, we identified advanced age and high BMI as risk factors for wound complications. Notably, tumor volume and tumor-breast volume ratio did not affect the local toxicity rate, suggesting that TARGIT can be safely applied, even in women with relatively small breasts, when an appropriate applicator is selected and there is sufficient residual tissue after lumpectomy.
Intriguingly, contrary to our expectations, local toxicity developed more frequently in women with a high BMI or a large breast volume. A high rate of acute complications in patients with large breasts was also observed in previous studies investigating acute skin reactions and late adverse effects on breast appearance from WBI in relation to breast size [21,22,23,24,25]. The inhomogeneity of the radiation dose partly accounts for long-term changes in breast shape in women with large breasts [26]. More toxicity from radiation in large breasts was also observed in studies on acute radiation dermatitis associated with intensity-modulated radiation therapy [27]. Although breast volume was not significantly associated with acute toxicity in the multivariate analysis, our findings on the relationship between acute toxicity and breast volume in women treated with IORT could be supported by these previous reports [21,22,23,24,25,26,27].
In principle, delivering radiation directly to the tumor-bed may evoke wound problems. Although seroma collection is the most common complication and is easily manageable, six patients in our study suffered significant wound complications, four with surgical site infections and two with wound dehiscence. Additionally, another phase I/II study on IORT using another low-energy device in Japanese women also reported wound complications such as hypertrophic scarring [19]. The risk of IORT for wound problems should be explained to both physicians and patients prior to applying this technique, and an effort to avoid skin toxicity during IORT is mandatory. One of the principles to avoid wound complications is that the minimum distance from the skin to the tumor cavity should be greater than 1 cm [28]. In our procedure, the skin edges were everted to ensure that any part of skin was more than 1 cm distant from the applicator surface.
Currently, it is recognized that IORT techniques are insufficient to suppress local recurrence after BCS compared to conventional WBI. Two large prospective studies (TARGIT-A and ELIOT trials) showed inferior local control rates of IORT compared to WBI [10, 11]. The most recent consensus of the American Brachytherapy Society for APBI states that IORT, including low-energy and electron techniques, is not the standard of care and should not be offered to patients outside prospective clinical trials because it lacks data demonstrating equivalent local control compared with WBI [29]. However, as emerging data suggest low rates of recurrence and toxicity with an application of IORT as tumor-bed boost, this consensus noted that IORT has the potential to be used for such an approach [29].
In light of this, we planned to deliver IORT as a boost in our protocol. As a result, we enrolled patients with risk factors including lobular carcinoma (2.5%) and those less than 40 years of age (6.1%). Despite a short-term follow-up period and enrollment of high-risk patients, the local control rate was excellent (99.2% at 2.2 years). The TARGIT-B trial aiming to show a superiority of local control by IORT with WBI is underway and will confirm the role of IORT as boost radiation [30].
A major limitation of our study is its single-arm design that did not directly compare IORT with WBI. In addition, we used the toxicity rate of WBI from the EBRT group of the TARGIT-A trial as a control, in which the majority were western women. They might have experienced toxicity of WBI at a higher rate than Asian, because high BMI and large breast volume were risk factors for local toxicity of EBRT. Thus, it is possible that the WBI-induced toxicity rate of Korean women is lower than that was used in our statistics. This issue should be solved by two-arm randomized control study in the future. The oncologic safety and late toxicity of our patients should be confirmed and requires long-term follow-up. Despite the inherent limitation of a non-randomized control study, our single-institute, single-arm study has advantages that it is the first report primarily focusing on the early toxicity of IORT in Asian women.
Conclusions
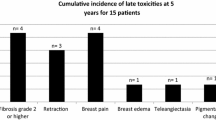
Targeted intra-operative radiotherapy using Intrabeam® as boost radiation can be a safe procedure for Asian patients with breast cancer with an acceptable toxicity profile in the acute period. Long-term follow-up is needed for prospective monitoring of late toxicity and local control.
References
Arndt V, Stegmaier C, Ziegler H et al (2008) Quality of life over 5 years in women with breast cancer after breast-conserving therapy versus mastectomy: a population-based study. J Cancer Res Clin Oncol 134(12):1311–1318. https://doi.org/10.1007/s00432-008-0418-y
Darby S, McGale P, Correa C et al (2011) Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet 378(9804):1707–1716. https://doi.org/10.1016/s0140-6736(11)61629-2
Veronesi U, Luini A, Del Vecchio M et al (1993) Radiotherapy after breast-preserving surgery in women with localized cancer of the breast. N Engl J Med 328(22):1587–1591. https://doi.org/10.1056/nejm199306033282202
Fisher ER, Anderson S, Redmond C et al (1992) Ipsilateral breast tumor recurrence and survival following lumpectomy and irradiation: pathological findings from NSABP protocol B-06. Semin Surg Oncol 8(3):161–166
Clark RM, McCulloch PB, Levine MN et al (1992) Randomized clinical trial to assess the effectiveness of breast irradiation following lumpectomy and axillary dissection for node-negative breast cancer. J Natl Cancer Inst 84(9):683–689
Boyages J, Recht A, Connolly JL et al (1990) Early breast cancer: predictors of breast recurrence for patients treated with conservative surgery and radiation therapy. Radiother Oncol 19(1):29–41
Baum M, Vaidya JS, Mittra I (1997) Multicentricity and recurrence of breast cancer. Lancet 349(9046):208. https://doi.org/10.1016/s0140-6736(05)60950-6
Vaidya JS, Vyas JJ, Chinoy RF et al (1996) Multicentricity of breast cancer: whole-organ analysis and clinical implications. Br J Cancer 74(5):820–824
Strnad V, Ott OJ, Hildebrandt G et al (2016) 5-year results of accelerated partial breast irradiation using sole interstitial multicatheter brachytherapy versus whole-breast irradiation with boost after breast-conserving surgery for low-risk invasive and in-situ carcinoma of the female breast: a randomised, phase 3, non-inferiority trial. Lancet 387(10015):229–238. https://doi.org/10.1016/s0140-6736(15)00471-7
Vaidya JS, Wenz F, Bulsara M et al (2014) Risk-adapted targeted intraoperative radiotherapy versus whole-breast radiotherapy for breast cancer: 5-year results for local control and overall survival from the TARGIT-A randomised trial. Lancet 383(9917):603–613. https://doi.org/10.1016/s0140-6736(13)61950-9
Veronesi U, Orecchia R, Maisonneuve P et al (2013) Intraoperative radiotherapy versus external radiotherapy for early breast cancer (ELIOT): a randomised controlled equivalence trial. Lancet Oncol 14(13):1269–1277. https://doi.org/10.1016/s1470-2045(13)70497-2
Vaidya JS, Joseph DJ, Tobias JS et al (2010) Targeted intraoperative radiotherapy versus whole breast radiotherapy for breast cancer (TARGIT-A trial): an international, prospective, randomised, non-inferiority phase 3 trial. Lancet 376(9735):91–102. https://doi.org/10.1016/s0140-6736(10)60837-9
Fastner G, Reitsamer R, Ziegler I et al (2015) IOERT as anticipated tumor bed boost during breast-conserving surgery after neoadjuvant chemotherapy in locally advanced breast cancer—results of a case series after 5-year follow-up. Int J Cancer 136(5):1193–1201. https://doi.org/10.1002/ijc.29064
Fastner G, Sedlmayer F, Merz F et al (2013) IORT with electrons as boost strategy during breast conserving therapy in limited stage breast cancer: long term results of an ISIORT pooled analysis. Radiother Oncol 108(2):279–286. https://doi.org/10.1016/j.radonc.2013.05.031
Forouzannia A, Harness JK, Carpenter MM et al (2012) Intraoperative electron radiotherapy boost as a component of adjuvant radiation for breast cancer in the community setting. Am Surg 78(10):1071–1074
Vaidya JS, Baum M, Tobias JS et al (2011) Long-term results of targeted intraoperative radiotherapy (Targit) boost during breast-conserving surgery. Int J Radiat Oncol Biol Phys 81(4):1091–1097. https://doi.org/10.1016/j.ijrobp.2010.07.1996
Blank E, Kraus-Tiefenbacher U, Welzel G et al (2010) Single-center long-term follow-up after intraoperative radiotherapy as a boost during breast-conserving surgery using low-kilovoltage X-rays. Ann Surg Oncol 17(Suppl 3):352–358. https://doi.org/10.1245/s10434-010-1265-z
Lee JJB, Choi J, Ahn SG et al (2017) In vivo dosimetry and acute toxicity in breast cancer patients undergoing intraoperative radiotherapy as boost. Radiat Oncol J 35(2):121–128. https://doi.org/10.3857/roj.2017.00150
Kawamura M, Itoh Y, Sawaki M et al (2015) A phase I/II trial of intraoperative breast radiotherapy in an Asian population: 5-year results of local control and cosmetic outcome. Radiat Oncol 10:150. https://doi.org/10.1186/s13014-015-0469-6
Pan L, Zheng W, Ye X et al (2014) A novel approach of INTRABEAM intraoperative radiotherapy for nipple-sparing mastectomy with breast reconstruction. Clin Breast Cancer 14(6):435–441. https://doi.org/10.1016/j.clbc.2014.04.002
Bulman AS, Cassoni AM, Ellis H (1985) The functional results following primary treatment of breast cancer with breast conservation. Eur J Surg Oncol 11(3):247–249
Habibollahi F, Mayles HM, Mayles WP et al (1988) Assessment of skin dose and its relation to cosmesis in the conservative treatment of early breast cancer. Int J Radiat Oncol Biol Phys 14(2):291–296
Fernando IN, Ford HT, Powles TJ et al (1996) Factors affecting acute skin toxicity in patients having breast irradiation after conservative surgery: a prospective study of treatment practice at the Royal Marsden Hospital. Clin Oncol (R Coll Radiol) 8(4):226–233
Vrieling C, Collette L, Fourquet A et al (2000) The influence of patient, tumor and treatment factors on the cosmetic results after breast-conserving therapy in the EORTC ‘boost vs. no boost’ trial. EORTC Radiotherapy and Breast Cancer Cooperative Groups. Radiother Oncol 55(3):219–232
Twardella D, Popanda O, Helmbold I et al (2003) Personal characteristics, therapy modalities and individual DNA repair capacity as predictive factors of acute skin toxicity in an unselected cohort of breast cancer patients receiving radiotherapy. Radiother Oncol 69(2):145–153
Moody AM, Mayles WP, Bliss JM et al (1994) The influence of breast size on late radiation effects and association with radiotherapy dose inhomogeneity. Radiother Oncol 33(2):106–112
Pignol JP, Olivotto I, Rakovitch E et al (2008) A multicenter randomized trial of breast intensity-modulated radiation therapy to reduce acute radiation dermatitis. J Clin Oncol 26(13):2085–2092. https://doi.org/10.1200/jco.2007.15.2488
Vaidya JS, Baum M, Tobias JS et al (2001) Targeted intra-operative radiotherapy (Targit): an innovative method of treatment for early breast cancer. Ann Oncol 12(8):1075–1080
Shah C, Vicini F, Shaitelman SF et al (2017) The American Brachytherapy Society consensus statement for accelerated partial-breast irradiation. Brachytherapy. https://doi.org/10.1016/j.brachy.2017.09.004
Vaidya JS (2017) A comparison of intra-operative radiotherapy boost with external beam radiotherapy boost in early breast cancer (TARGIT-B). https://clinicaltrials.gov/ct2/show/NCT01792726. Accessed 26 Dec 2017
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The institutional review boards approved the trial according to their local laws and regulations (IRB No 3-2013-0299). All patients gave written informed consent, and the trial was conducted in compliance with the Helsinki Declaration.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10549_2018_5038_MOESM1_ESM.tif
Volumetry by preoperative magnetic resonance imaging. a Manual measurement of breast and tumor portion on axial breast MRI images. b 3D volume of breast tissue portion. c 3D volume of tumor portion. Supplementary material 1 (TIF 2341 KB)
10549_2018_5038_MOESM3_ESM.tif
Two cases with complications. a Wound dehiscence. A 52-year-old female did not have a medical history of diabetes mellitus and had a low body mass index (18.68) and low breast volume (401.703 cc). Wound dehiscence with discharge was first noted on POD #15. Wound revision under local anesthesia was performed on POD #27. b Wound infection. A 76-year-old female had a medical history of diabetes mellitus, a high body mass index (33.85), and a high breast volume (1441.18 cc). A wound infection was first noted after the 2nd cycle of docetaxel-cyclophosphamide chemotherapy. This patient was treated with antibiotics for 1 week. Supplementary material 3 (TIF 4989 KB)
10549_2018_5038_MOESM4_ESM.tif
Comparison of age and body mass index (BMI) according to the incidence of complications using the Student t-test. a Comparison of mean age between the non-complication and complication groups (p < 0.001). b Comparison of mean BMI between the non-complication and complication groups (p = 0.001). c Comparison of mean breast volume between the non-complication and complication groups (p = 0.017). d Comparison of mean tumor volume between the non-complication and complication groups (p = 0.094). e Comparison of the mean tumor-volume ratio between the non-complication and complication groups (p = 0.696). Supplementary material 4 (TIF 1054 KB)
Rights and permissions
About this article
Cite this article
Ahn, S.G., Bae, S.J., Lee, H.W. et al. A phase II study investigating the acute toxicity of targeted intraoperative radiotherapy as tumor-bed boost plus whole breast irradiation after breast-conserving surgery in Korean patients. Breast Cancer Res Treat 174, 157–163 (2019). https://doi.org/10.1007/s10549-018-5038-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-018-5038-x