Abstract
Purpose
This study was designed to determine the safety and clinical efficacy of metronomic chemotherapy combined with aromatase inhibitors (AIs) for hormone receptor (HR)-positive advanced breast cancer (ABC) patients who cannot tolerate conventional-dose chemotherapy.
Methods
Postmenopausal patients with HR-positive ABC, who exhibited disease progression after first-line AIs treatment and who could not tolerate or rejected conventional chemotherapy, were enrolled in this study. Patients received capecitabine 500 mg PO TID (could be reduced to 500 mg QD in case of adverse effects) and exemestane 25 mg QD (after PD with letrozole) or letrozole 2.5 mg QD (after PD with exemestane). The primary endpoints were safety and tolerance, the secondary endpoints were objective response rate (ORR), clinical benefit rate (CBR), progression-free survival (PFS), and time to treatment failure (TTF).
Results
In our analysis of 44 patients, the median age was 64 years (range 38–90) and 68.2% patients had at least two recurrences or metastatic lesions. Grade 3 toxicities (hand–foot syndrome) were observed only in 4 of the patients. Most patients exhibited no or mild toxicities. After a median follow-up of 14.8 months, ORR was 70.5%, CBR—77.3%, PFS—16.2 months, and TTF—14.4 months.
Conclusions
Metronomic oral capecitabine combined with AIs showed good efficacy, minimal toxicities, and good tolerance in HR-positive patients with ABC. It is a potential treatment option especially for postmenopausal HR-positive ABC patients in poor general condition who cannot tolerate conventional chemotherapy. Trial registration: Clinicaltrials.gov NCT01924078.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hormone receptor (HR)-positive breast cancer is the most common type of breast cancer [1]. Endocrine therapy, including anti-estrogens and aromatase inhibitors (AIs), has been the mainstay of treatment for women with HR-positive breast cancer. However, some of these patients exhibit de novo resistance to endocrine treatment, while even more patients may eventually develop acquired resistance, leading to disease recurrence. While the exact mechanisms of endocrine resistance have yet to be discovered, some drugs that reverse endocrine resistance have been already developed, such as everolimus for aromatase inhibitor-resistant disease [2] and the cyclin-dependent kinase 4/6 (CDK 4/6) inhibitor palbociclib [3]. Vascular endothelial growth factor (VEGF)-induced tumor angiogenesis may be an important factor leading to the failure of first-line or second-line hormonal therapy in HR-positive breast cancer [4, 5]. Metronomic chemotherapy (MC), a regimen of low-dose, continuous, and uninterrupted chemotherapy, is another treatment option that has been gaining increased attention in the recent years, considering its important advantages (low toxicity profile, sufficient efficacy, and cost-effectiveness for public health application) [6,7,8,9,10]. Its main mechanisms of tumor suppression are supposed to be inhibition of the activation of tumor-associated vascular endothelial cells and bone marrow-derived endothelial progenitor cells, inhibition of pro-angiogenic factors (such as VEGF), and promotion of anti-angiogenic factors and angiostatin generation. These effects result in the reduction of the microvessel density, leading to decrease of the oxygen supply and nutritional support of the tumor [6, 11,12,13]. Clinical studies have demonstrated that patients with metastatic breast cancer can benefit from metronomic chemotherapy and suffer no severe adverse effects; MC is well tolerated and results in good compliance. For example, the ORR was 33% and CBR 67% for patients enrolled in VICTOR-1 (metronomic vinorelbine plus capecitabine) study [14]; the clinical benefit rate (complete response, partial response, and stable disease) was 31% in patients that received combination of metronomic methotrexate and cyclophosphamide [15]; CBR was 42% for patients subjected to combination of metronomic docetaxel, capecitabine with concurrent celecoxib [16]. MC often uses oral medications which best embody the desired pharmacokinetic characteristics and offers convenient, safe, and reliable dosing for patients. For some frail patients or those with severe systemic diseases that cannot tolerate conventional-dose chemotherapy, MC may be one of the choices for these patients to overwhelm their endocrine resistance.
Moreover, combination of third-generation aromatase inhibitors with metronomic chemotherapy can improve considerably the overall response rate (by 15.8–21.7%) of aromatase inhibitors and can significantly decrease the proliferation index Ki-67 index as well as the VEGF-A level in the tumor tissue [4, 17]. In detail, the ORR was 71.9% in the patients that received letrozole versus 87.7% in the patients assigned to receive letrozole plus metronomic cyclophosphamide [17].
The consideration about preference of the concomitant over sequential application of chemotherapy and endocrine agents began in the 1970s and it is still under discussion [18, 19]. Former studies revealed a controversy in the advantages of concomitant versus sequential chemo- and antiestrogen therapies [20], whereas later clinical trials showed no significant difference in the benefits using concurrent or sequential chemo- and hormone therapies [21]. Other researchers found sequential treatment as more effective [22], while other investigators found a considerable survival advantage of the combined chemoendocrine therapy of postmenopausal patients with estrogen receptor-positive tumors [23]. Therefore, the query about the priority of concurrent over sequential chemo- and antiestrogen therapies should be studied further in order to clarify whether the concurrent treatment can provide better objective response rate and response duration values compared with the sequential treatment. The potential detrimental consequences of the delay in the beginning of the powerful antiestrogen treatment in sequential chemo- and endocrine therapies should be also estimated for the ER-positive breast cancer patients.
It is noteworthy to remark that the previous chemoendocrine therapies have used mainly tamoxifen, which is a selective estrogen receptor modulator (SERM) with considerable side effects (uterus cancer, thromboses, etc.), while the present study is devoted to combination of a cytostatic agent (capecitabine) with a new generation of anti-estrogens, called aromatase inhibitors. AIs have a different mechanism of action compared to SERM agents. AIs are a novel class of drugs that suppress the biosynthesis of estrogens by inhibition of the enzyme aromatase (estrogen synthase) and are found to have superior efficacy and safety for patients [24,25,26,27]. Recent comprehensive reviews about evaluation of the concurrent versus sequential chemo- and endocrine therapies of HR-positive breast cancer patients recommend future clinical trials to clarify this issue with special emphasis upon the combination of cytostatic agents with aromatase inhibitors as recent achievements of the modern medicine [28].
Capecitabine (Xeloda®) is an oral fluoropyrimidine cytostatic drug that is widely used as first- and second-line treatment for advanced breast cancer. Animal experiments have suggested that sustained delivery of low-dose capecitabine can significantly reduce the micro vessel density (MDV) and VEGF levels in vivo, compared with other modes of administration. Some clinical trials have reported that frequent or continuous low-dose capecitabine exhibits good therapeutic activity and safety in the treatment of advanced breast cancer [29,30,31]. In addition, concomitant application of capecitabine plus letrozole in postmenopausal breast cancer xenograft models showed highly improved anti-tumor efficacy of both drugs, used in combination, due to additive or synergistic effects, which scientific result was directed for confirmation to future clinical trials [32].
At present, metronomic chemotherapy is used mainly for the rescue treatment of triple-negative breast cancer or HR-positive breast cancer without combination with endocrine therapy [33, 34]. This study is aimed to explore the efficacy and safety of a synchronous treatment, including metronomic chemotherapy with oral capecitabine in combination with third-generation aromatase inhibitors for postmenopausal HR-positive patients with locally advanced or metastatic breast cancer.
Materials and methods
Patients
In this study, 44 HR-positive advanced or metastatic breast cancer patients treated at Fudan University Shanghai Cancer Center (FUSCC) were enrolled from November 2010 to May 2013 after first- or second-line hormonal therapy failure. The study was approved by the Fudan University Cancer Hospital Ethic Committee for Clinical Investigation. The study was carried out in accordance with the Declaration of Helsinki. All patients signed an informed written consent to be included in the clinical trial.
Eligible patients corresponded to the following criteria: postmenopausal or premenopausal women who underwent prior bilateral oophorectomy, histologically confirmed ER- and/or PR-positive, human epidermal growth factor receptor type 2 (HER2)-nonamplified locally advanced or metastatic breast cancer, refractory disease following letrozole or exemestane treatment. Refractory disease was defined as recurrence or progression of breast cancer during treatment or within 1 month after the end of treatment for advanced disease; other previous anticancer endocrine treatments, prior chemotherapy regimens, and radiotherapy for advanced disease were allowed. In each case, patients were required to exhibit at least one measurable lesion [defined according to Response Evaluation Criteria in Solid Tumors version 1.1 (RECIST v1.1)] or lytic bone lesion in the absence of measurable disease. Patients were also required to have an Eastern Cooperative Oncology Group (ECOG) performance status of 3 or less (on a scale from 0 to 5, with 0 indicating that the patient is fully active, 1 indicating that the patient is restricted in physically strenuous activity but is ambulatory active and able to perform work of a light or sedentary nature, 2 indicating that the patient is ambulatory and capable of all self-care activity but unable to work, and 3 indicating that the patient is capable of only limited self-care, confined to a bed or chair for more than 50% of waking hours, and exhibits adequate organ and hematologic functions). In addition, adequate organ and hematologic functions [35] and a life expectancy of at least 3 months were necessary for inclusion. Exclusion criteria included a history of brain metastases and previous treatment with Xeloda for advanced disease.
Study design and treatment
In this clinical trial, phase 2, single-center, single-arm, prospective study, all patients received capecitabine (Xeloda®) at a dose of 500 mg three times per day/daily in combination with AIs. At present, there is no standard metronomic capecitabine dose, however the dose of capecitabine used in many metronomic clinical trials has been 500 mg tid, 500 mg bid, or 800–1200 mg/m2 per day [36,37,38]. In our study, we selected capecitabine dose of 500 mg tid, which was aimed at achievement of a constant therapeutical concentration, less toxic for the liver and kidneys. In future metronomic chemoendocrine clinical trials, treatment with doses of capecitabine received once a day can be also explored. Patients who experienced refractory disease following letrozole treatment, received exemestane (25 mg daily), while those who experienced refractory disease following exemestane treatment, received letrozole (1 mg daily).
The primary endpoints of this study were safety and tolerance, including the following criteria: (1) treatment toxicity classification and (2) the proportion of patients requiring dose reduction or early termination of the treatment. Secondary endpoints included: overall response rate (ORR), clinical benefit rate (CBR), progression-free survival (PFS), and time to treatment failure (TTF). The ORR was defined as the proportion of the number of patients who achieved a complete response (CR) or partial response (PR) assessed by RECIST version 1.1 criteria [39]. The CBR was defined as the percentage of patients with CR + PR + SD ≥ 24 weeks, determined by RECIST v. 1.1. PFS was defined as the time from the day when the treatment was started to the first evidence of progression as defined by RECIST (v. 1.1) guidelines or to the time of death from any cause. TTF was defined as the time from study entry to removal from the study for any cause, including disease progression, drug toxicity, or refusal of further therapy.
Treatment was continued until either disease progression, development of unacceptable toxicity, or withdrawal of consent. The protocol provided detailed guidelines for dose interruptions or reductions of Xeloda in case of adverse events. In such cases, two reductions of the Xeloda dose were permitted: an initial reduction to 500 mg twice per day and a subsequent reduction to 500 mg daily. AIs were not applied with reduction of the doses.
The trial was registered in ClinicalTrials.gov (identifier NCT01924078) at the U.S. National Institutes of Health.
Efficacy and safety assessments
Tumor assessment included computed tomography (CT) scanning, magnetic resonance imaging (MRI), or ultrasound examination that were performed at baseline of the treatment and every 8 weeks until disease progression. A bone scan or skeletal survey was required within 4 weeks before starting metronomic therapy. Abnormalities revealed by the bone scans were assessed by either X-ray, CT scanning with bone windows, or MRI before beginning of the metronomic therapy and were assessed using the same method every 8 weeks. Hematologic function, biochemical analyses, and vital signs were assessed at baseline of the treatment and at each visit. Adverse events were monitored continuously throughout the study and graded according to National Cancer Institute Common Terminology Criteria for Adverse Events, version 4.0.
Statistical analysis
Patient data were recorded as numbers and percentages, and were quantitatively described as medians with minimum and maximum values. PFS and TTF were measured from the starting date of the treatment to the date of progression or to the date of last follow-up due to death or withdrawal, respectively. PFS and TTF were assessed using the Kaplan–Meier product limit estimate method. Graphs were created using GraphPad Prism software, version 5.01 (GraphPad Software, Inc.).
Results
Patients
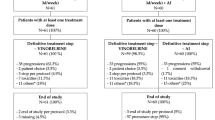
A total of 44 patients were enrolled and assigned to treatment with the combination of Xeloda and AIs: 23 patients received exemestane and 21 patients received letrozole. The patients’ median age was 64 years, and the maximum age was 90 years. The patients’ baseline characteristics are presented in Table 1. There was 1 premenopausal woman with a bilateral oophorectomy and 43 postmenopausal patients. Twenty-two patients (50.0%) exhibited two or more systemic diseases (hypertension, diabetes, cerebral infarction, myocardial infarction, renal insufficiency), and 30 patients (68.2%) exhibited at least two metastatic sites or recurrence. Twenty-five patients (56.8%) experienced prior failure of the first-line endocrine therapy; 8 patients (18.2%) received the combined therapy as first-line rescue treatment, including newly diagnosed advanced breast cancer patients (3 patients) or patients who failed in adjuvant endocrine therapy (5 patients); 11 patients (25%) received multi-line chemotherapy prior to enrollment in this study (Table 1). 36 patients (81.8%) have received prior adjuvant endocrine therapy, and 27 patients (61.4%) have received previous adjuvant chemotherapy. Median length of the treatment follows up was 14.8 months, during which no patient was lost to follow-up of the treatment.
Safety and tolerance
The observed treatment-related toxicities were evaluated in all 44 patients, as presented in Table 2. The most common adverse event was hand–foot syndrome (19 patients, 43.2%), where 4 patients (9.1%) exhibited grade 3 hand–foot syndrome, and no patients exhibited grade 4 hand–foot syndrome. One patient suffered from bone fracture, and cerebral infarction occurred in 1 patient. All other adverse events were either grade 1 or 2 and did not exceed grade 3. Treatment reductions due to adverse events occurred in 2 patients (4.5%): The first patient was a 51-year-old female, whose capecitabine dosage was reduced to 500 mg twice per day, at 18 months after initiation of the metronomic chemotherapy, due to grade 3 hand–foot syndrome. Her symptoms were relieved after dose reduction. The second patient was a 76-year-old female, whose capecitabine dosage was reduced to 500 mg twice per day, at 1 month after initiation of the metronomic chemotherapy due to soreness/numbness and dry skin, in both lower extremities. The reduced dose was continued until detection of progression of the disease. Treatment discontinuation due to adverse events occurred in 1 patient (2.3%). Thus, treatment-related toxicities were generally modest and manageable. Almost all patients (95.5%) attended regularly the follow-up appointments and regularly took their medications, no patients were lost during follow-up—all these facts indicated that patient compliance and tolerance were sufficient.
Efficacy
After a median follow-up period of 14.8 months (range 1.0–63.9 months), all 44 patients were enrolled in the preliminary efficacy analysis. The overall objective response rate (ORR) was 70.5%, the clinical benefit rate (CBR) was 77.3%, and the median PFS was 16.2 months (95% CI 6.24–26.17), as shown in Fig. 1a. The median TTF was 14.4 months (95% CI 7.25–21.55), as shown in Fig. 1b. Two patients have been treated by the combined therapy for more than 5 years (one patient with bone and liver metastasis, the other one with bone metastasis). For the patients treated in our study after previous multi-line chemotherapy, the median PFS was 18.0 months (Fig. 1c), the median TTF was 15.3 months (Fig. 1d). For the patients treated after prior endocrine therapy, the PFS was 16.2 months and the median TTF was 9.6 months (Fig. 1c, d, resp.). There was no significant difference in our study between the above two groups of patients. A comparative analysis of the PFS and TTF of other clinical trials concerning famous drugs that reverse endocrine resistance in breast cancer patients is presented in Table 3.
Kaplan–Meier plot of progression-free survival (PFS) and time to treatment failure (TTF) results of combined therapy with metronomic capecitabine plus AIs (a, b) in comparison with the corresponding PFS/TTF values after foregoing endocrine therapy or chemotherapy (c, d). Cap capecitabine, AI aromatase inhibitors, PFS progress-free survival, TTF time to treatment failure, 95% CI 95% confidence interval
Discussion
For postmenopausal women with hormone receptor-positive breast cancer, the third-generation aromatase inhibitors play an important role, as they are well tolerated by elderly breast cancer patients and exhibit relatively few side effects [40, 41]. Although breast cancer is relatively sensitive to chemotherapy, severe adverse effects often limit the treatment, especially in elderly patients with poor overall condition, including those with severe systemic cardiovascular diseases. In addition, advanced breast cancer patients often suffer from cachexia, and many of them are unable to tolerate conventional chemotherapy; therefore, they must choose to cease, reduce, or suspend treatment. In recent years, metronomic therapy has been gaining increased attention. With its low therapeutical doses, less serious side effects, and easy drug administration, metronomic therapy showed improvement of the patient tolerability and compliance. In our study, the majority of patients were elderly patients with multiple systemic diseases and even with a maximum age of 90 years, yet despite this most patients showed no serious adverse reactions during treatment. Consistent with previous reports [4, 15, 17], our patients showed an overall well tolerance and high compliance, with no patient lost during the treatment. Our study and the results from several other clinical trials suggest that metronomic chemotherapy combined with aromatase inhibitors can be a promising treatment option for advanced postmenopausal breast cancer.
Metronomic chemotherapy resynchronization therapy with AIs also showed good efficacy, e.g., the overall objective response rate in our study reached 70.5%. We compared this metronomic chemoendocrine therapy with our results about metronomic chemotherapies. The response rate of the therapy with capecitabine plus AIs is higher than the ORR value, observed in a domestic research (ORR 60%), using 500 mg capecitabine three times daily. Additionally, treatment of metastatic breast cancer with capecitabine from days 1 to 14 in combination with docetaxel (25 mg m−2, intravenously, administered on days 1 and 8) for every 21 days resulted in a similar response rate (77.3% vs. 80%), which is higher than the ORR reported in the literature (16.7–34%) for similar metronomic chemotherapy studies with clinical benefit rates of 31–42% [15, 16]. This discrepancy may be due to the HR-positive status of the patients enrolled in our study. In addition, the median PFS after initial or first-line endocrine therapy failure was 9.6 months in our study, comparable to the results reported by the BOLERO-2 trial [2], which studied treatment with exemestane combined with everolimus after first-line endocrine therapy failure (PFS 10.6 months) and PALOMA-3 trial, which studied treatment with palbociclib and fulvestrant (PFS 9.5 months) [42]. Everolimus and palbociclib have both been shown to be effective in reversing endocrine resistance, and it is intriguing to note that our results showed that metronomic chemotherapy combined with AIs may achieve similar efficacy with less serious adverse effects. The adverse reactions in our treatment are lighter than those in the latter two studies. It should be considered that because of our small patient number range, it is not enough to prove whether the effect in our treatment is equivalent to the above-mentioned clinical trials, considering that the combined therapy with metronomic capecitabine plus AIs has fewer side effects. We need further clinical experiments with greater number of patients for confirmation of these results.
It is worthy of note that several previous studies have shown that conventional chemotherapy combined with endocrine therapy may affect the efficacy of chemotherapy and even the long-term clinical benefit of patients [22, 43]. However, these studies failed to reveal advantage of the concurrent over sequential application of antiestrogen treatment (tamoxifen) and chemotherapy (epirubicin plus cyclophosphamide [43]; cyclophosphamide, doxorubicin, and fluorouracil [22]). In this connection, it should be underlined that these chemoendocrine studies have used a SERM agent (tamoxifen), while the present clinical trial explores the advantages of a recent generation of anti-estrogens, namely, aromatase inhibitors, in combination with a metronomic cytostatic drug (capecitabine). AIs have different mechanisms of action in comparison with SERM agents and are found to possess superior efficacy and safety.
The results of our study showed that the efficacy of metronomic chemotherapy combined with endocrine therapy was similar to other clinical studies concerning combination therapies directed to reversal of the endocrine resistance [2, 42], which may be related to the fact that the anti-tumor mechanism of metronomic chemotherapy in combination with AIs is different from the mechanism of the conventional-dose chemotherapy.
Currently, most types of the metronomic therapy consist of several chemotherapy drugs administered in metronomic dosage, metronomic chemotherapy combined with immunotherapy or targeted therapy [14, 44,45,46]. There are only few clinical trials of metronomic chemotherapy combined with endocrine therapy for HR-positive advanced breast cancer [17, 47]. In this regard, high therapeutical efficacy (overall response rate 87.7%) was achieved by treatment of ER-positive breast cancer patients (T2-4 N0-1) that obtained letrozole (AI) in combination with metronomic cyclophosphamide (50 mg/daily, 6 months) [17]. Recently, we reported a case report about high efficiency of a concomitant application of low doses of taxanes or capecitabine with anastrozole (AI) for achievement of a rapid and long-lasting remission of advanced (pT4bpN2Mx infiltrative ductal) breast carcinoma [48]. This case report explored feasible additive and synergy effects of the combination of cytostatic agents (taxanes or capecitabine) with AI as achievements of the modern medicine [32]. The metronomic chemoendocrine therapy, employed in the case report, was aimed also at prevention of detrimental consequences, considered for the advanced breast cancer patient, in case of delay of the start of the therapy with powerful AI and cytostatic agents (if they were applied consequently) and needs further confirmation in clinical trials.
Our present study suggests that the treatment with metronomic capecitabine plus AIs is highly efficient. Additional randomized controlled phase III clinical trials is envisaged in the future to explore the feasibility of the advantages of the metronomic chemotherapy combined with endocrine therapy, including combination with novel endocrine resistance reversing drugs.
Conclusion
The present clinical trial is focused on the combination of metronomic chemotherapy with aromatase inhibitors as achievements of the modern medicine in the treatment of breast cancer patients. Metronomic oral capecitabine combined with AIs showed good efficacy, minimal toxicities, and good tolerance in HR-positive patients with metastatic breast cancer. The combination of metronomic chemotherapy and AIs is a potential treatment option especially for postmenopausal HR-positive metastatic breast cancer patients in poor general condition who cannot tolerate conventional chemotherapy. Our results suggest that this therapeutical approach is perspective to be investigated in a next phase III clinical trial in response to the requirements of the clinical practice. Metronomic chemoendocrine therapy has high potential benefit in induction of long-lasting tumor dormancy by delay and prevention of metastases dissemination in advanced breast cancer. In perspective, future clinical trials are expected to clarify also the query whether the efficacy of metronomic chemoendocrine therapy can be better therapeutical approach in comparison with chemo- or endocrine therapies (applied alone, in consecutive order) in achievement of long-lasting disease remission when applied at earlier stages of ER-positive breast cancer patients. Further scientific studies are required also to clarify whether combinations of cytostatic and endocrine drugs, explored in metronomic chemoendocrine therapies, exhibit synergy or additive antiproliferative effects aimed at more efficient prevention of the genesis and dissemination of metastases in breast cancer patients.
Abbreviations
- PO TID:
-
Ter in die per os; 3 times a day per oral
- QD:
-
Quaque die; every day
- PD:
-
Progression of the disease
References
Tang LC, Yin WJ, Di GH, Shen ZZ, Shao ZM (2010) Unfavourable clinicopathologic features and low response rate to systemic adjuvant therapy: results with regard to poor survival in young Chinese breast cancer patients. Breast Cancer Res Treat 122(1):95–104. https://doi.org/10.1007/s10549-009-0537-4
Baselga J, Campone M, Piccart M, Burris HA 3rd, Rugo HS, Sahmoud T et al (2012) Everolimus in postmenopausal hormone-receptor-positive advanced breast cancer. N Engl J Med 366(6):520–529. https://doi.org/10.1056/NEJMoa1109653
Finn RS, Crown JP, Lang I, Boer K, Bondarenko IM, Kulyk SO, Ettl J, Patel R, Pinter T, Schmidt M, Shparyk Y, Thummala AR, Voytko NL, Fowst C, Huang X, Kim ST, Randolph S, Slamon DJ (2015) The cyclin-dependent kinase 4/6 inhibitor palbociclib in combination with letrozole versus letrozole alone as first-line treatment of oestrogen receptor-positive, HER2-negative, advanced breast cancer (PALOMA-1/TRIO-18): a randomised phase 2 study. Lancet Oncol 16(1):25–35. https://doi.org/10.1016/S1470-2045(14)71159-3
Wolf C, Blohmer JU, Ortmann O, Krainick U, Eiermann W (2006) Neoadjuvant exemestan alone or combined with metronomic chemotherapy (epirubicine; paclitaxel; docetaxel): efficacy plus tolerability. Final results of a multicenter phase I/II study (GENARI: German neoadjuvant aromasin initiative). Breast Cancer Res Treat 100(Suppl. 1):S151. https://doi.org/10.1007/s10549-006-5678-0; Special issue: 29th Annual San Antonio Breast Cancer Symposium, Texas, USA
Hyder SM, Stancel GM (2000) Regulation of VEGF in the reproductive tract by sex-steroid hormones. Histol Histopathol 15(1):325–334. https://doi.org/10.14670/HH-15.325
Browder T, Butterfield CE, Kräling BM, Shi B, Marshall B, O’Reilly MS, Folkman J (2000) Antiangiogenic scheduling of chemotherapy improves efficacy against experimental drug-resistant cancer. Cancer Res 60(7):1878–1886. http://cancerres.aacrjournals.org/content/60/7/1878.full-text.pdf
Hanahan D, Bergers G, Bergsland E (2000) Less is more, regularly: metronomic dosing of cytotoxic drugs can target tumor angiogenesis in mice. J Clin Invest 105(8):1045–1047. https://doi.org/10.1172/JCI9872
Montagna E et al (2014) Metronomic therapy and breast cancer: a systematic review. Cancer Treat Rev 2014. 40(8):942–950. https://doi.org/10.1016/j.ctrv.2014.06.002
Banys-Paluchowski M, Schutz F, Ruckhaberle E, Krawczyk N, Fehm T (2016) Metronomic chemotherapy for metastatic breast cancer - a systematic review of the literature. Geburtshilfe Frauenheilkd 2016 76(5):525–534. https://doi.org/10.1055/s-0042-105871
Liu Y, Gu F, Liang J, Dai X, Wan C, Hong X, Zhang K, Liu L (2017) The efficacy and toxicity profile of metronomic chemotherapy for metastatic breast cancer: a meta-analysis. PLoS ONE 12(3): article e0173693. https://doi.org/10.1371/journal.pone.0173693
Emmenegger U, Morton GC, Francia G, Shaked Y, Franco M, Weinerman A, Man S, Kerbel RS (2006) Low-dose metronomic daily cyclophosphamide and weekly tirapazamine: a well-tolerated combination regimen with enhanced efficacy that exploits tumor hypoxia. Cancer Res 66(3):1664–1674
Colleoni M, Rocca A, Sandri MT, Zorzino L, Masci G, Nolè F, Peruzzotti G, Robertson C, Orlando L, Cinieri S, de BF, Viale, Goldhirsch G A (2002) Low-dose oral methotrexate and cyclophosphamide in metastatic breast cancer: antitumor activity and correlation with vascular endothelial growth factor levels. Ann Oncol 13(1):73–80
Vacca A, Iurlaro M, Ribatti D, Minischetti M, Nico B, Ria R, Pellegrino A, Dammacco F (1999) Antiangiogenesis is produced by nontoxic doses of vinblastine. Blood 94(12):4143–4155. http://www.bloodjournal.org/content/bloodjournal/94/12/4143.full.pdf
Cazzaniga ME, Torri V, Riva F, Porcu L, Cicchiello F, Capici S, Cortinovis D, Digiacomo N, Bidoli P (2017) Efficacy and safety of vinorelbine-capecitabine oral metronomic combination in elderly metastatic breast cancer patients: VICTOR-1 study. Tumori 103(1):e4–e8. https://doi.org/10.5301/tj.5000543
Salem DA, Gado NM, Abdelaziz NN, Essa AE, Abdelhafeez ZM, Kamel TH (2008) Phase II trial of metronomic chemotherapy as salvage therapy for patients with metastatic breast cancer. J Egypt Natl Canc Inst 20(2):134–140. http://www.nci.cu.edu.eg/Journal/June2008/can_5.pdf
Young SD, Lafrenie RM, Clemons MJ (2012) Phase II trial of a metronomic schedule of docetaxel and capecitabine with concurrent celecoxib in patients with prior anthracycline exposure for metastatic breast cancer. Curr Oncol 19(2):e75–e83. https://doi.org/10.3747/co.19.879
Bottini A, Generali D, Brizzi MP, Fox SB, Bersiga A, Bonardi S et al (2006) Randomized phase II trial of letrozole and letrozole plus low-dose metronomic oral cyclophosphamide as primary systemic treatment in elderly breast cancer patients. J Clin Oncol 24(22):3623–3628. https://doi.org/10.1200/JCO.2005.04.5773
Pritchard KI (2007) Combining endocrine agents with chemotherapy: which patients and what sequence? Cancer 112(Suppl. 3):718–722. https://doi.org/10.1002/cncr.23189
Barrios C, Forbes JF, Jonat W, Conte P, Gradishar W, Buzdar A et al (2012) The sequential use of endocrine treatment for advanced breast cancer: where are we? Ann Oncol 23(6):1378–1386. https://doi.org/10.1093/annonc/mdr593
Kumar KS, Vogel CL, Moore MR, Bartolucci AA (1982) Sequential versus concomitant chemo-hormonal therapy in breast cancer. Breast Diseases of the Breast 8(2):2–7
Bedognetti D, Sertoli MR, Pronzato P, Del Mastro L, Venturini M, Taveggia P et al (2011) Concurrent vs sequential adjuvant chemotherapy and hormone therapy in breast cancer: a multicenter randomized phase III trial. J Natl Cancer Inst 103(20):1529–1539. https://doi.org/10.1093/jnci/djr351
Albain KS, Barlow WE, Ravdin PM, Farrar WB, Burton GV, Ketchel SJ et al (2009) Adjuvant chemotherapy and timing of tamoxifen in postmenopausal patients with endocrine-responsive, node-positive breast cancer: a phase 3, open-label, randomised controlled trial. Lancet 374(9707):2055–2063. https://doi.org/10.1016/S0140-6736(09)61523-3
Kiang DT, Gay J, Goldman A, Kennedy BJ (1985) A randomized trial of chemotherapy and hormonal therapy in advanced breast cancer. N Engl J Med 313(20):1241–1246. https://doi.org/10.1056/NEJM198511143132001
Nabholz JM, Buzdar A, Pollak M, Harwin W, Burton G, Mangalik A et al (2000) Anastrozole is superior to tamoxifen as first-line therapy for advanced breast cancer in postmenopausal women: results of a North American multicenter randomized trial. Arimidex Study Group. J Clin Oncol 18(22):3758–3767. https://doi.org/10.1200/JCO.2000.18.22.3758
Eiermann W, Paepke S, Appfelstaedt J, Llombart-Cussac A, Eremin J, Vinholes J et al (2001) Preoperative treatment of post menopausal breast cancer patients with letrozole: a randomized double blind multicenter study. Ann Oncol 12(11):1527–1532
Ellis MJ, Coop A, Singh B, Tao Y, Llombart-Cussac A, Jänicke F et al (2003) Letrozole inhibits tumor proliferation more effectively than tamoxifen independent of HER1/2 expression status. Cancer Res 2003 63(19):6523–6531
Margolese RG, Cecchini RS, Julian TB, Ganz PA, Costantino JP, Vallow LA, Albain KS et al (2016) Anastrozole versus tamoxifen in postmenopausal women with ductal carcinoma in situ undergoing lumpectomy plus radiotherapy (NSABP B-35): a randomized, double-blind, phase 3 clinical trial. Lancet 387(10021):849–856. https://doi.org/10.1016/S0140-6736(15)01168-X
Poggio F, Ceppi M, Lambertini M, Bruzzi P, Ugolini D, Bighin C et al (2017) Concurrent versus sequential adjuvant chemo-endocrine therapy in hormone-receptor positive early breast cancer patients: a systematic review and meta-analysis. Breast 33:104–108. https://doi.org/10.1016/j.breast.2017.03.011
Hennessy BT, Gauthier AM, Michaud LB, Hortobagyi G, Valero V (2005) Lower dose capecitabine has a more favorable therapeutic index in metastatic breast cancer: retrospective analysis of patients treated at M. D. Anderson Cancer Center and a review of capecitabine toxicity in the literature. Ann Oncol 16(8):1289–1296. https://doi.org/10.1093/annonc/mdi253
Dellapasqua S, Bertolini F, Bagnardi V, Campagnoli E, Scarano E, Torrisi R et al (2008) Metronomic cyclophosphamide and capecitabine combined with bevacizumab in advanced breast cancer. J Clin Oncol 26(30):4899–4905. https://doi.org/10.1200/JCO.2008.17.4789
Cazzaniga ME, Cortesi L, Ferzi A, Scaltriti L, Cicchiello F, Ciccarese M et al (2016) Metronomic chemotherapy with oral vinorelbine (mVNR) and capecitabine (mCAPE) in advanced HER2-negative breast cancer patients: is it a way to optimize disease control? Final results of the VICTOR-2 study. Breast Cancer Res Treat 160(3):501–509. https://doi.org/10.1007/s10549-016-4009-3
Kataoka M, Yamaguchi Y, Moriya Y, Sawada N, Yasuno H, Kondoh K, Evans DB, Mori K, Hayashi S (2012) Antitumor activity of chemoendocrine therapy in premenopausal and postmenopausal models with human breast cancer xenografts. Oncol Rep 27(2):303–310. https://doi.org/10.3892/or.2011.1541
Di Desidero T, Kerbel RS, Bocci G (2016) Metronomic chemotherapy for triple negative breast cancer? AGING 8(4):573–574. https://doi.org/10.18632/aging.100947
Munzone E, Bertolini F, Colleoni M (2014) Metronomic chemotherapy in breast cancer. In: Bocci G, Francia G (eds) Metronomic chemotherapy: pharmacology and clinical applications. Springer, Berlin, Heidelberg, pp 93–100. https://doi.org/10.1007/978-3-662-43604-2
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP (1982) Toxicity and response criteria of the Eastern-Cooperative-Oncology-Group. Am J Clin Oncol 5(6):649–655
Masuda N, Higaki K, Takano T et al (2014) A phase II study of metronomic paclitaxel/cyclophosphamide/capecitabine followed by 5-fluorouracil/epirubicin/cyclophosphamide as preoperative chemotherapy for triple-negative or low hormone receptor expressing/HER2-negative primary breast cancer. Cancer Chemother Pharmacol 74(2):229–238. https://doi.org/10.1007/s00280-014-2492-y
Yoshimoto M, Takao S, Hirata M et al (2012) Metronomic oral combination chemotherapy with capecitabine and cyclophosphamide: a phase II study in patients with HER2-negative metastatic breast cancer. Cancer Chemother Pharmacol 70(2):331–338. https://doi.org/10.1007/s00280-012-1826-x
El-Arab LR, Swellam M, El Mahdy MM (2012) Metronomic chemotherapy in metastatic breast cancer: impact on VEGF. J Egypt Natl Canc Inst 24(1):15–22. https://doi.org/10.1016/j.jnci.2011.12.002
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L et al (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92(3):205–216
Howell A, Cuzick J, Baum M, Buzdar A, Dowsett M, Forbes JF et al (2005) Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years’ adjuvant treatment for breast cancer. Lancet 365(9453):60–62. https://doi.org/10.1016/S0140-6736(04)17666-6
Semiglazov VF, Semiglazov VV, Dashyan GA, Ziltsova EK, Ivanov VG, Bozhok AA, Melnikova OA, Paltuev RM, Kletzel A, Berstein LM (2007) Phase 2 randomized trial of primary endocrine therapy versus chemotherapy in postmenopausal patients with estrogen receptor-positive breast cancer. Cancer 110(2):244–254. https://doi.org/10.1002/cncr.22789
Cristofanilli M, Turner NC, Bondarenko I, Ro J, Im SA, Masuda N et al (2016) Fulvestrant plus palbociclib versus fulvestrant plus placebo for treatment of hormone-receptor-positive, HER2-negative metastatic breast cancer that progressed on previous endocrine therapy (PALOMA-3): final analysis of the multicentre, double-blind, phase 3 randomised controlled trial. Lancet Oncol 17(4):425–439. https://doi.org/10.1016/S1470-2045(15)00613-0
Pico C, Martin M, Jara C, Barnadas A, Pelegri A, Balil A et al (2004) Epirubicin-cyclophosphamide adjuvant chemotherapy plus tamoxifen administered concurrently versus sequentially: randomized phase III trial in postmenopausal node-positive breast cancer patients. A GEICAM 9401 study. Ann Oncol 15(1):79–87
Gnoni A, Silvestris N, Licchetta A, Santini D, Scartozzi M, Ria R, Pisconti S, Petrelli F, Vacca A, Lorusso V (2015) Metronomic chemotherapy from rationale to clinical studies: a dream or reality? Crit Rev Oncol Hematol 95(1):46–61. https://doi.org/10.1016/j.critrevonc.2015.01.008
Montagna E, Palazzo A, Maisonneuve P, Cancello G, Iorfida M, Sciandivasci A et al (2017) Safety and efficacy study of metronomic vinorelbine, cyclophosphamide plus capecitabine in metastatic breast cancer: a phase II trial. Cancer Lett 400:276–281. https://doi.org/10.1016/j.canlet.2017.01.027
Berruti A, Fazio N, Ferrero A, Pia Brizzi M, Volante M, Nobili E et al (2014) Bevacizumab plus octreotide and metronomic capecitabine in patients with metastatic well-to-moderately differentiated neuroendocrine tumors: the xelbevoct study. BMC Cancer 14:184. https://doi.org/10.1186/1471-2407-14-184
Schwartzberg LS, Wang G, Somer BG, Blakely LJ, Wheeler BM, Walker MS, Stepanski EJ, Houts AC (2014) Phase II trial of fulvestrant with metronomic capecitabine for postmenopausal women with hormone receptor-positive, HER2-negative metastatic breast cancer. Clin Breast Cancer 14(1):13–19. https://doi.org/10.1016/j.clbc.2013.09.003
Li J, Jia X, Ivanova D (2018) Chemoendocrine metronomic therapy of estrogen receptor-positive breast cancer by taxanes or capecitabine in combination with aromatase inhibitors. J Pharm Res 17(2): 78–82. https://doi.org/10.18579/jpcrkc/2018/17/2/127179; The 4th Mediterranean Symposium on Medicinal and Aromatic Plants (MESMAP-4), April 18–22, 2018, Antalya, Turkey, ISBN 978-605-61261-5-4, p. 125
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interests.
Ethical approval
This study was approved by an independent ethics committee at FUSCC. Written informed consent was obtained from all patients before enrollment in the study. The clinical trial complies with the current laws of China.
Rights and permissions
About this article
Cite this article
Li, Jw., Zuo, Wj., Ivanova, D. et al. Metronomic capecitabine combined with aromatase inhibitors for new chemoendocrine treatment of advanced breast cancer: a phase II clinical trial. Breast Cancer Res Treat 173, 407–415 (2019). https://doi.org/10.1007/s10549-018-5024-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-018-5024-3