Abstract
Purpose
Advances in breast cancer treatment have contributed to marked improvements in patient outcomes over the past three decades. This study aims to chronologically evaluate the survival of patients with breast cancer and investigate the observed changes over time.
Methods
Statistics from the Korean National Cancer Registry, based on all 60,571 patients with invasive breast cancer during the 21 year period, were analyzed. We divided the study interval into four periods (P1: 1988–1992, P2: 1993–1997, P3: 1998–2002, P4: 2003–2008).
Results
The patients treated during P4 showed significantly better 5-year overall survival (OS) than did those treated during P1 (5Y OS; P1 = 79.0 vs. P4 = 92.2, p < 0.001). In the multivariate analyses, younger age, mastectomy, high stage, high tumor grade, lymphovascular invasion, and hormone receptor negativity were poor prognostic factors. The multivariate analysis demonstrated that diagnosis periods significantly and independently associated with OS in the overall group of patients. In our analysis of age-period-interaction models, the hazard ratio (HR) for death for patients who were under 35 years of age, compared to those who were older, tended to decrease over time (HR of age < 35 vs. 35 ~ 50; P1 = 0.739, p = 0.007; P2 = 0.744, p < 0.001; P3 = 0.886, p = 0.041; P4 = 0.983, p = 0.813). The survival rate of patients who underwent breast conserving surgery (BCS) has recently gotten better than that of mastectomy (HR of mastectomy vs. BCS; P1 = 0.957, p = 0.790; P2 = 0.542, p < 0.001; P3 = 0.543, p < 0.001; P4 = 0.425, p < 0.001).
Conclusions
The clinical factors related to the changes in breast cancer survival have improved and increased patient OS over the past 20 years in Korea. In addition, we provided new insights into the effects of age and surgery methods on prognosis in each period.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recently, many studies worldwide have reported that the survival rate of patients with breast cancer is improving. Such observations result from improved nationwide screening programs for early breast cancer detection [1], an increase in the proportion of less aggressive cancers [2], and advances in adjuvant treatment, such as trastuzumab for human epidermal growth factor receptor-2 (HER-2)-positive tumors and aromatase inhibitors for hormone receptor-positive tumors [3,4,5].
The Korean Breast Cancer Society (KBCS) also publishes biennial reports on the characteristics of breast cancer in the country, along with evolving trends [1,2,3,4]. According to the national breast cancer data in the Korean Breast Cancer Registry (KBCR), the overall survival (OS) of female patients with breast cancer in Korea is gradually increasing over time [5]. However, despite the improvements in OS, breast cancer may recur at any time. Depending on the properties of the tumor, such as size, lymph node metastasis, and biological subtype, various clinical outcomes have been seen in patients with breast cancer. Some patients experience recurrences several months after surgery, and some have recurrences after a few years, most of which result in death. Therefore, identifying the prognostic factors for death is very important for predicting the patient outcomes and suggesting the most appropriate supplementary treatment.
In contrast to studies in western countries, very few investigations have reported the underlying cause of the survival improvements that have been observed in Korean patients with breast cancer over time. Thus, it would be clinically relevant to investigate the incremental changes in patients with early-stage cancer and treatment time periods that correlate with the advancements in cancer management.
The main purpose of this study is to analyze the survival of Korean patients with breast cancer over 20 years (1988–2008). We also conducted a data analysis, to identify factors that affect outcomes and changes in survival over time.
Methods
Korean breast cancer registry
The KBCR is a database that has been prospectively maintained by the KBCS since 1996 [6]. Nationwide, 102 general hospitals with at least 400 beds, including 41 university hospitals and 61 surgical training hospitals, have voluntarily participated in this program. In 2001, the Online Korean Breast Cancer Registration Program was launched, which allowed physicians from participating hospitals to input data into the web-based database. Essential items for registration were the patient’s unique Korean resident’s registration number as an identifier, the patient’s sex and age, the surgical method used, and the cancer stage, based on the American Joint Committee on Cancer classification. Patient survival data, including dates and causes of death, were obtained from the Korea Central Cancer Registry, Ministry of Health and Welfare, Korea. The Korean Central Cancer Registry is linked to the Korean National Statistical Office, which maintains complete death statistics, which are recorded with the unique identification numbers that are assigned to all Korean residents [7].
The KBCR data do not include the type or date of tumor recurrence, because the Korean Central Cancer Registry only provides mortality data. The KBCR data also do not provide the patient’s name and unique Korean resident registration number, to protect the privacy of each patient.
Patients and follow-up
From the database, we identified 68,070 patients who underwent breast cancer surgery between January 1988 and December 2008. Among them, 5541 patients who had pure carcinoma in situ were excluded. Patients who received neoadjuvant chemotherapy were also excluded; ultimately, we enrolled 60,571 patients. Estrogen receptor (ER), progesterone receptor (PR), and HER-2 statuses were determined immunohistochemically. For HER-2 overexpression analysis, cases that were graded as 0, 1 +, or 2 + were considered negative. Cases graded as 2 + were evaluated by fluorescence in situ hybridization, and cases graded as 3 + were regarded positive. We divided the study period into four phases, according to significant changes in anti-hormonal therapy and chemotherapy, as follows: P1, 1988–1992; P2, 1993–1997; P3, 1998–2002; and P4, 2003–2008.
Statistical analyses
The correlation between the four cohorts, according to the date of surgery and clinicopathological parameters, was analyzed using chi-squared and t tests. OS was defined as the time from the date of surgery to the date of death or last follow-up.
The Kaplan–Meier method was used to estimate the survival outcomes of all patients, from the date of surgery. Groups were compared using log-rank statistics. Cox proportional hazards models were used for both univariable and multivariable analyses. We calculated the hazard ratios (HRs) from each period to determine the interaction effect between period and age group or surgery methods. The HRs (95% confidence interval [CI]) and p values were reported. p < 0.05 was used to signify statistical significance. We conducted our analyses using the SPSS statistical software, version 21.0 (SPSS Inc., Chicago, USA).
Results
Patient characteristics
The clinical characteristics of the patients are shown in Table 1. For the age at diagnosis, the number of patients in the 35–50 year age group of was the highest across all periods. However, the proportions of patients under 35 years of age at diagnosis were 13.9% in P1, 10.9% in P2, 8.5% in P3, and 6.6% in P4, and the proportion decreased from P1 to P4 (p < 0.001). There was also a change in the frequency of operations according to period. The proportion of mastectomies decreased, and the proportion of BCS increased, from P1 to P4. The frequencies of BCS were 6.3% in P1, 18.2% in P2, 29.8% in P3, and 46.8% in P4 (p < 0.001). With respect to T stage, the frequency of patients with T1 cancer was 29.3%, of T2 was 56.9% and of T3 and 4 was 13.8% in P1. However, the frequency of T1 increased from P1 to P4 by 52.9% and that of T2 and T3 and 4 decreased by 40.4 and 6.7% in P4, respectively. The proportion of patients without lymph node metastasis was 48.8% in P1, but this statistic increased from P1 to P4 and was 59.7% in P4 (p < 0.001). When the breast cancer HRs were examined in each period, the percentage of patients with ER positive tumors was 46.5% in P1, and this number increased to 62.2% in P4 (p < 0.001).
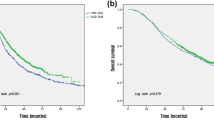
Survival
Overall 5- and 10-year survival rates were 89.5 and 81.7%, respectively. The 5-year survival rate was 79.0% in P1, 82.7% in P2, 86.8% in P3, and 92.2% in P4 and gradually increased from P1 to P4 (p < 0.001). The 10-year survival rate for each period was 66.1, 73.1, 79.4, and 87.5%, from P1 to P4, respectively, and also significantly and gradually increased from P1 to P4 (Fig. 1, p < 0.001).
The univariate Cox regression results for each variable are shown in Table 2. The patients in the 35–50 year age range showed the most favorable factors, followed by those over 50 years, and patients under 35 years of age showed the least favorable outcomes (p < 0.001). Patients who underwent BCS had better prognoses than those who underwent mastectomy (p < 0.001). We found that larger tumor size, node metastasis, advanced stage, higher nuclear and histologic grades, lymphovascular invasion, hormone receptor negativity, and HER2 amplification had negative effects on survival (p < 0.001).
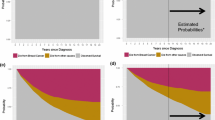
Figure 2 shows the changes in postoperative mortality risk over each period. Over all periods, the postoperative mortality risk had the greatest increase after 2–3 years of surgery. However, this risk decreased from P1 to P4. The postoperative mortality risk at 3 years was 0.037 in P1, 0.022 in P2, 0.012 in P3, and 0.003 in P4. In agreement with the univariate analysis, the multivariate analysis using the Cox model showed that younger age, mastectomy, advanced stage, higher nuclear and histological grades, lymphovascular invasion, and hormone receptor negativity were common prognostic factors for breast cancer and had statistically significant negative impacts on prognosis and survival (Table 3, p < 0.001). As with the univariate analysis, the time period had a positive and statistically significant impact on patient survival. Based on P1, the HR at P2 was 0.909 (p = 0.041), the HR at P3 was 0.717 (p < 0.001), and the HR at P4 was 0.514 (p < 0.001). In the univariate analysis, hormonal therapy and radiotherapy had positive effects on survival, and adjuvant chemotherapy had a negative effect. However, the multivariate analysis showed that all three of these variables had positive effects on survival (p < 0.001).
We also analyzed the trends in hazard ratios that were calculated from each period, to determine the associations between periods and age groups. Compared with patients under 35 years of age, the risk of death among patients aged 35–50 was lower. Compared to patients under 35 years of age, the risk of death in patients aged 35–50 years has increased from past to recent periods. The HR for death of patients 35 ~ 50 years of age compared to patients under 35 years at P1 was 0.739 (p = 0.007), the HR at P2 was 0.744 (p < 0.001), the HR at P3 was 0.886 (p = 0.041), and the HR at P4 was 0.983 (p = 0.813). The differences in risks with respect to age at diagnosis decreased from P1 to P4. According to the results of the operation methods, the risk of mastectomy and BCS did not differ between the two groups at P1 (HR 0.957, p = 0.790); but after P2, the risk of death for BCS compared to mastectomy reduced. Finally, in period 4, BCS was associated with a statistically significant lower risk of death than mastectomy (in P2, HR 0.542, p < 0.001; in P3, HR 0.543, p < 0.001; and in P4, HR 0.425, p < 0.001) (Table 4).
Discussion
The survival rate of patients with breast cancer has improved over the past five decades [8, 9]. The age-standardized 5-year relative survival rate for American patients with breast cancer who were diagnosed from 2003 to 2009 was 89.2%, in the Surveillance, Epidemiology, and End Results (SEER) database [6]. In the present study, the OS rate of patients with breast cancer, from 2003 to 2008, was 92.2%, which is also a significant improvement from previous periods.
What factors are responsible for recent improvements in survival rates? Until now, it was thought that the survival rate improvements were caused by an increase in the proportion of early-stage cancer detection and the application of newly developed chemotherapies and endocrine therapies [2]. Our study also showed that the proportion (38.7%) of patients diagnosed with early-stage (stage I) cancer after 2003 increased, compared to the previous period (p < 0.001) (Table 1). This was possible because of the development of early detection of cancer systems, such as opportunistic screening, in Korea [7].
In addition, the survival rate increased through the development of and changes in treatment methods. The administration of adjuvant chemotherapy has been associated with better prognoses in previous studies [3, 10, 11]. Henderson et al. reported that the addition of paclitaxel to AC (Adriamycin + cyclophosphamide) reduced the recurrence risk by 17% (p = 0.001) and the risk of death by 18% (p = 0.010). In patients who were treated with only AC, the 5-year DFS was 65% and the 5-year OS was 77%. However, when AC was combined with paclitaxel B, the 5-year DFS increased to 70% and the 5-year OS increased to 80% [12]. In our study, we did not identify the therapies that led to the increased survival rates, but the main opinion is that survival rates have increased, in general, with the development of adjuvant chemotherapy. Although CMF (cyclophosphamide, methotrexate, and fluorouracil) was mainly used during P1 (83.6%), this therapy gradually decreased in usage towards P4 (23.9%), and new medicines, such as taxane and anthracycline, began to be used in the 2000s [anthracycline- and taxane-based P1(0.3%) vs. P4 (30.7%)]. In addition to adjuvant chemotherapy, one of other factors that affected the survival of patients with breast cancer patients was anti-hormone therapy. Previously, tamoxifen was the anti-hormonal agent that was primarily used for patients with breast cancer. Around 2003, significant changes were observed in the use of aromatase inhibitors and/or LHRH agonists. During P1, only 0.1% of the patients received aromatase inhibitors, but during P4, at least one of these drugs was used in 14.2% of patients. Trastuzumab also improved the survival rate of patients with HER-2-positive breast cancer [10]; however, we did not include trastuzumab in our analysis, as trastuzumab insurance was not covered by the Korean National Health Insurance during this study period. In our study, 46 (0.1%) of the patients received trastuzumab (data not shown).
The time period, age at diagnosis, and surgical methods also affected survival, as revealed by the multivariate survival analysis, in addition to changes in treatment methods. Previous studies have also shown that the time of diagnosis affects survival. Ahn et al. found that the time period played an important role in improving the survival rate of Korean patients with breast cancer [13]. Hideo Shigematsu et al. also found that the time period was a significant prognostic factor that affected survival in the multivariate analysis, and survival durations have been recently prolonged [14]. Similar to previous reports, our study also confirmed, in a multivariate analysis, that the time period was a significant prognostic factor that affects the survival of patients with breast cancer in Korea. The survival time has been prolonged in recent years (Fig. 1), which might be considered a selection bias because of the development of new therapies and earlier breast cancer discovery through extensive screening, despite the multivariate analysis. However, prolonged survival may be associated with income level increases and improvements in living environments, which were factors that could not be analyzed.
The age at diagnosis has also been considered as a factor that affects the survival of patients with breast cancer in previous studies. Wingo et al. [15] reported a lower survival rate for women under 25 years of age and Yancik et al. [16] reported a lower survival rate for women over 55 years of age, indicating that age at diagnosis also affects survival and recurrence. Since there have been no screening tests for women under 40 years of age, breast cancer in younger patients could be more aggressive. Furthermore, endocrine therapy is important for patients with hormone receptor-positive breast cancer. Younger patients with breast cancer may refuse endocrine therapy due to concerns about family planning, decreased sexual function, and menopausal symptoms. These observations agree with our findings, as younger patients with breast cancer were diagnosed with more advanced cancer and aggressive biology than older patients (data not shown). Furthermore, in our study, the multivariate analysis showed that young patient age was associated with an increased risk of death, and young age was found to be a poor prognostic factor across all four periods. However, the risk has gradually decreased over time, from P1 to P4. Compared to the 35–50 years of age group, the risk of death was higher for patients under 35 years of age. The HR at P1 was 0.739 (p = 0.007), at P2 was 0.744 (p < 0.001), at P3 was 0.886 (p = 0.041), and at P4 was 0.983 (p = 0.813) (Table 4). This was due to the fact that patients and medical staff have changed their perceptions, due to the availability of active treatments for patients with early-stage breast cancer at diagnosis, and the development of new treatment methods. Yoon et al. reported that the DFS of young patients with hormone receptor-positive and HER2-negative tumors improved significantly over time (p = 0.032) [17]. They reported that young patients with hormone receptor-positive breast cancer have experienced recent survival improvements using tamoxifen and ovarian suppression.
The survival rate of patients with breast cancer has not been significantly affected by differences in surgical methods. Prior to the 1980s, mastectomy was performed primarily when surgical treatment was needed for patients with breast cancer. In the 1980s, randomized controlled clinical trials were performed that combined BCS with radiotherapy for the topical treatment of early breast cancer, and such regimens showed survival rates that were similar to non-radiation mastectomy [18, 19]. Some recent studies have also shown that BCS and radiotherapy are associated with improved survival, compared to mastectomy [20,21,22]. Maaren et al. provided clear evidence that BCS and radiotherapy were associated with improved OS in patients with early breast cancer [23]. In our study, BCS was found to be prognostic factor, rather than mastectomy, in comparison with the other adjusted factors in the multivariate analysis (Table 3). Through comparing these factors with time periods, only the BCS survival rate showed recent improvements. The risk of mastectomy and BCS was no different between the two groups at P1 (HR 0.957, p = 0.790), but at P2 and after, the risk of death for BCS was reduced, compared to that for mastectomy. Finally, in P4, BCS had a statistically significant lower risk of death than mastectomy (in P2, HR 0.542, p < 0.001; in P3, HR 0.543, p < 0.001; and in P4, HR 0.425, p < 0.001) (Table 4). The survival rate of patients treated with BCS plus radiotherapy was found to be better than that of patients who underwent mastectomy, which could be explained by advances in cancer diagnosis, surgical treatment, and radiation therapy in the last 30 years. Onitilo et al. reported that the survival rates of BCS without radiotherapy and mastectomy were similar, but the survival rate of patients who underwent BCS plus radiotherapy was better than that of patients who underwent mastectomy [22]. In addition, patients who underwent mastectomy had a wider surgical site than BCS, which leads to more tissue inflammation and consequent increased inflammatory cytokines. This promotes tumorigenesis and increases the likelihood of cancer recurrence [24].
Our study has some limitations that should be considered when interpreting our results. There is a likelihood of referral and screening biases that are commonly encountered in retrospective, observational cohort studies. In addition, biases due to the rapid increase in the number of patients in the P4 period and the change to lower cancer stages could have affected survival outcomes. Additionally, we speculate that differences in the follow-up durations between the investigated periods might be another limitation; therefore, we adjusted the follow-up period to 72 months (median follow-up duration of patients diagnosed in P4), and similar results were obtained (OS p < 0.001, data not shown).
In conclusion, we have provided important evidence of factors that have increased the survival rate of Korean patients with breast cancer over the past 21 years. In addition, we provided new insights into the effects of age and surgery methods on prognosis in each period.
References
Dawood S, Broglio K, Gonzalez-Angulo AM, Buzdar AU, Hortobagyi GN, Giordano SH (2008) Trends in survival over the past two decades among white and black patients with newly diagnosed stage IV breast cancer. J Clin Oncol 26:4891–4898. https://doi.org/10.1200/jco.2007.14.1168
You JM, Kim YG, Moon HG, Nam SJ, Lee JW, Lim W, Lee MR, Noh DY, Han W (2015) Survival improvement in Korean breast cancer patients due to increases in early-stage cancers and hormone receptor positive/HER2 negative subtypes: a nationwide registry-based study. J Breast Cancer 18:8–15. https://doi.org/10.4048/jbc.2015.18.1.8
Early Breast Cancer Trialists’ Collaborative Group (2005) Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15 year survival: an overview of the randomised trials. Lancet 365:1687–1717. https://doi.org/10.1016/s0140-6736(05)66544-0
Trudeau M, Charbonneau F, Gelmon K et al (2005) Selection of adjuvant chemotherapy for treatment of node-positive breast cancer. Lancet Oncol 6:886–898. https://doi.org/10.1016/s1470-2045(05)70424-1
Piccart-Gebhart MJ, Procter M, Leyland-Jones B et al (2005) Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. N Engl J Med 353:1659–1672. https://doi.org/10.1056/NEJMoa052306
Howlader N, Noone AM, Krapcho M et al (2013) SEER cancer statistics review, 1975–2010. http://seer.cancer.gov/csr/1975_2010. Accessed 11 April 2017
Kim Z, Min SY, Yoon CS, Jung KW, Ko BS, Kang E, Nam SJ, Lee S, Hur MH (2015) The basic facts of Korean breast cancer in 2012: results from a nationwide survey and breast cancer registry database. J Breast Cancer 18:103–111. https://doi.org/10.4048/jbc.2015.18.2.103
Yoshimoto M, Tada K, Hori H et al (2004) Improvement in the prognosis of Japanese breast cancer patients from 1946 to 2001—an institutional review. Jpn J Clin Oncol 34:457–462. https://doi.org/10.1093/jjco/hyh076
Ueno M, Kiba T, Nishimura T et al (2007) Changes in survival during the past two decades for breast cancer at the Kyoto University Hospital. Eur J Surg Oncol 33:696–699. https://doi.org/10.1016/j.ejso.2007.01.029
Goldhirsch A, Gelber RD, Coates AS (2005) What are the long-term effects of chemotherapy and hormonal therapy for early breast cancer? Nat Clin Pract Oncol 2:440–441. https://doi.org/10.1038/ncponc0296
Henderson IC, Berry DA, Demetri GD et al (2003) Improved outcomes from adding sequential Paclitaxel but not from escalating Doxorubicin dose in an adjuvant chemotherapy regimen for patients with node-positive primary breast cancer. J Clin Oncol 21:976–983. https://doi.org/10.1200/jco.2003.02.063
Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL (1987) Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 235:177–182
Ahn SG, Lee HM, Lee SA, Jeong J, Lee HD (2014) Long-term survival analysis of korean breast cancer patients at a single center: improving outcome over time. Yonsei Med J 55:1187–1195. https://doi.org/10.3349/ymj.2014.55.5.1187
Shigematsu H, Kawaguchi H, Nakamura Y et al (2011) Significant survival improvement of patients with recurrent breast cancer in the periods 2001–2008 vs. 1992–2000. BMC Cancer 11:118. https://doi.org/10.1186/1471-2407-11-118
Wingo PA, Ries LA, Parker SL, Heath CW Jr (1998) Long-term cancer patient survival in the United States. Cancer Epidemiol Biomark Prev 7:271–282
Yancik R, Wesley MN, Ries LA, Havlik RJ, Edwards BK, Yates JW (2001) Effect of age and comorbidity in postmenopausal breast cancer patients aged 55 years and older. JAMA 285:885–892
Yoon TI, Hwang UK, Kim ET et al (2017) Survival improvement in hormone-responsive young breast cancer patients with endocrine therapy. Breast Cancer Res Treat 165:311–320. https://doi.org/10.1007/s10549-017-4331-4
Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, Jeong JH, Wolmark N (2002) Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 347:1233–1241. https://doi.org/10.1056/NEJMoa022152
Litiere S, Werutsky G, Fentiman IS, Rutgers E, Christiaens MR, Van Limbergen E, Baaijens MH, Bogaerts J, Bartelink H (2012) Breast conserving therapy versus mastectomy for stage I–II breast cancer: 20 year follow-up of the EORTC 10801 phase 3 randomised trial. Lancet Oncol 13:412–419. https://doi.org/10.1016/s1470-2045(12)70042-6
Hwang ES, Lichtensztajn DY, Gomez SL, Fowble B, Clarke CA (2013) Survival after lumpectomy and mastectomy for early stage invasive breast cancer: the effect of age and hormone receptor status. Cancer 119:1402–1411. https://doi.org/10.1002/cncr.27795
Agarwal S, Pappas L, Neumayer L, Kokeny K, Agarwal J (2014) Effect of breast conservation therapy vs. mastectomy on disease-specific survival for early-stage breast cancer. JAMA Surg 149:267–274. https://doi.org/10.1001/jamasurg.2013.3049
Onitilo AA, Engel JM, Stankowski RV, Doi SA (2015) Survival comparisons for breast conserving surgery and mastectomy revisited: community experience and the role of radiation therapy. Clin Med Res 13:65–73. https://doi.org/10.3121/cmr.2014.1245
van Maaren MC, de Munck L, de Bock GH, Jobsen JJ, van Dalen T, Linn SC, Poortmans P, Strobbe LJA, Siesling S (2016) 10 year survival after breast-conserving surgery plus radiotherapy compared with mastectomy in early breast cancer in the Netherlands: a population-based study. Lancet Oncol 17:1158–1170. https://doi.org/10.1016/s1470-2045(16)30067-5
Indelicato D, Grobmyer SR, Newlin H, Morris CG, Haigh LS, Copeland EM 3rd, Mendenhall NP (2007) Association between operative closure type and acute infection, local recurrence, and disease surveillance in patients undergoing breast conserving therapy for early-stage breast cancer. Surgery 141:645–653. https://doi.org/10.1016/j.surg.2006.12.011
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was waived because the study was based on retrospective clinical data.
Rights and permissions
About this article
Cite this article
Lee, S.B., Ko, S.S., Park, C.H. et al. Chronologically changing patterns in the survival of korean patients with breast cancer and related clinical factors: a nationwide registry-based study. Breast Cancer Res Treat 172, 273–282 (2018). https://doi.org/10.1007/s10549-018-4892-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-018-4892-x