Abstract
Purpose
Palbociclib is an approved cyclin-dependent kinase (CDK) 4/6 inhibitor for treatment of patients with ER-positive and HER2-negative breast cancers. While Retinoblastoma protein (pRb), a major substrate of CDK4/6, is a potential target in triple negative breast cancer (TNBC), the usefulness of CDK4/6 inhibitors in this cancer has not been established. This preclinical study investigated the combination effects of palbociclib and the dual mammalian target of rapamycin (mTOR) kinase inhibitor MLN0128 in estrogen receptor (ER)-negative breast cancer in vitro and in vivo.
Methods
The combined effects of two drugs on three TNBC cell lines (MB231, MB468, and CAL148) and an ER-negative and HER2-positive cell line (MB453) were investigated by MTT assay and colony formation analysis. Cell cycle measurements were examined as well as changes in expression of molecules related to G1/S transition and the mTOR pathway. Importantly, a pRb-expressing TNBC patient-derived xenograft (PDX) model was used to assess the effects of the combination in vivo.
Results
A combination of palbociclib and MLN0128 synergistically inhibited the proliferation of pRb-expressing cell lines and induced G1 cell cycle arrest. Western blot analysis revealed that CDK4/6-pRb and mTOR pathways were inhibited by these treatments. In pRb-expressing TNBC PDX, the combination treatment drastically suppressed tumor growth compared to either the control or single drug treatments. In addition, the combination treatment significantly reduced the number of Ki67-positive cells.
Conclusions
We revealed that palbociclib and MLN0128 had synergistic anti-cancer activity in both pRb + ER-negative cell lines and a TNBC PDX model. Our results indicate that such combination therapy is worthy of further investigation in a clinical setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The most common malignancy in women is breast cancer. It represents approximately 29% of all new female cancer cases; one in eight women develops breast cancer in her life [1]. Triple negative breast cancer (TNBC) is defined by (1) the absence of ER and PR expression through immunohistochemistry (IHC) and (2) normal expression levels of HER2 via IHC and/or its amplification via fluorescence in situ hybridization (FISH). TNBC accounts for approximately 13–22% of all breast cancers [2,3,4,5]. Unlike TNBCs, breast cancers that are positive for ER, PR, and/or HER2 are treated with either hormone therapies or anti-HER2 targeted therapies. To date, no targeted therapies have been approved for TNBC. Therefore, TNBC is generally treated with chemotherapy. While TNBC is often more sensitive to chemotherapy than other subtypes of breast cancer, TNBC patients with residual disease after neoadjuvant chemotherapy have an extremely poor prognosis [6,7,8]. Thus, a new therapeutic strategy for TNBC is urgently needed.
Palbociclib is a specific CDK4/6 inhibitor. When the FDA approved a combination of palbociclib and letrozole in 2015, it was deployed as a first line treatment for post-menopausal women with ER-positive and HER2 negative advanced or metastatic breast cancer [9, 10]. The efficacy of palbociclib is associated with its suppression of CDK4/6 activity. CDK4/6 forms complexes with cyclin D and phosphorylates pRb, which is a tumor suppressor protein. Phosphorylation of pRb allows transcription factor E2F to dissociate from the pRb–E2F complex. Subsequent expression of E2F targeted genes plays important roles during the G1/S transition [11]. By preventing pRb phosphorylation and transcription of E2F-targeted genes, treatment with palbociclib results in G1 cell cycle arrest [12]. Importantly, the expression of pRb is key for the response of a CDK4/6 inhibitor [13]. While loss of pRb expression has been often observed in TNBC, it is still expressed in approximately 60% of these cases [14, 15]. Additionally, Rb expression has been associated with poor prognosis after chemotherapy [15,16,17]. As such, the CDK4/6-pRb axis is expected to be an important treatment target for pRB-positive TNBC.
Combinations of a CDK4/6 inhibitor and a phosphatidylinositol 3-kinase (PI3K) inhibitor have undergone preclinical evaluation for TNBC with the PIK3CA mutation [18]. However, the rate of PIK3CA mutation in human TNBC tissue is only 8.3% [19], which limits the utility of the treatment strategy. A downstream component of the PI3K/AKT regulating pathway is mammalian target of rapamycin (mTOR). mTOR integrates signals involving growth factors, nutrients, energy and oxygen levels to regulate cell growth, metabolism, autophagy, protein translation, and angiogenesis [20]. The mTOR pathway is also known to regulate cell cycle [21, 22]. According to a report by Montero et al. mTOR may be one of the most common targets in TNBC [23]. mTOR forms two different protein complexes called mTORC1 and mTORC2. mTORC1 not only regulates growth signaling but also mediates potent negative feedback loops. When the drug selectively inhibits mTORC1, the corresponding loss of a negative feedback loop may activate mTORC2 [24]. MLN0128 is a second-generation dual mTOR kinase inhibitor which suppresses both mTORC1 and 2. MLN0128 exhibited anti-proliferation effects in TNBC cell lines with or without PIK3CA mutation [25]. Thus, MLN0128 has been investigated in several breast cancer clinical trials including ones for patients with everolimus-resistant breast cancer (Supplementary Table S1). Here, we investigated the combination of palbociclib and MLN0128 in TNBC through in vitro and in vivo experiments. The study also included a HER2-positive/ER-negative cell line, MB453.
Methods
Cell lines
Breast cancer cell lines, MB231, MB453, MB468, and CAL148 were purchased from ATCC and DSMZ. There have been conflicting reports about the status of MB453 as a pRb-positive TNBC cell line. As such, we assessed MB453 cells from ATCC to determine HER2 expression levels. Our analysis indicated that MB453 is a HER2-positive/ER-negative cell line. HER2 amplification was validated in MB453 by FISH. Importantly, this cell line has been reported as resistant to HER2 targeted therapies [26]. To help clarify its HER2 status, here we refer to MB453 as a “HER2-positive cell line”; the terms “TNBC” or “ER-negative breast cancer” are used when appropriate. All cell lines were maintained at 37 °C and 5% CO2 in Dulbecco’s Modified Eagle Medium (DMEM) (Genesee Scientific) supplemented with 10% fetal bovine serum (FBS) (Omega Scientific Inc), 1% penicillin–streptomycin (HyClone), and 1% sodium pyruvate (Corning).
Patient-derived xenograft
Surgically resected tumor pieces (2 × 2 mm2) from a patient with TNBC were implanted into the 4th mammary fat pad of 6 to 8 weeks old female NOD-scid/IL2Rγ−/− (NSG) mice to establish PDX lines. The details were previously described [27]. We used COH_GS6, which is a pRb-expressing TNBC PDX line. The presence of pRb was confirmed by Western blot.
In vivo animal study
Tumor slices (2 × 2 mm2) from an established tumor were implanted into female NSG mice. After tumor sizes reached approximately 50 mm3, mice were randomized and received control vehicle (1:1 ratio of PBS and MLN vehicle), palbociclib (50 mg/kg in the control vehicle) [28], and/or MLN0128 (0.3 mg/kg in the control vehicle) [25]. All drugs and control vehicle were administered 6 days a week by oral gavage. Mouse body weight was monitored at each time of treatment. Tumor volume was monitored once a week and calculated with the following formula: length × width2 × π/6 [29]. Tumor samples were collected 6 h after drug administration. NSG mice were bred and housed at the City of Hope Animal Resources Center in ventilated cage racks with free access to water and food. They were maintained on a 12 h light/dark cycle.
Histological analysis
IHC staining was performed by the Pathology Core facility at City of Hope. Ki67 was scored by manually counting 3 fields of over 500 cells each and then determining the percentage of Ki67 positive cells [30]. Representative images were acquired using an EVOS FL cell imaging system (Thermo Fisher Scientific).
Results
Palbociclib suppresses cell proliferation in pRb-expressing ER-negative breast cancer cell lines
To determine the effect of palbociclib on the proliferation of ER-negative breast cancer cells in vitro, we used 3 TNBC cell lines (MB231, MB468, and CAL148) and an ER-negative and HER2-positive cell line (MB453). MB231 and MB453 were confirmed to be pRb-expressing, and MB468 and CAL148 were pRb-deficient cell lines, as demonstrated by Western blot analysis (Fig. 1a). Cells were treated with palbociclib at 24, 72, or 120 h. Palbociclib-mediated inhibition of cell proliferation was examined via dose- and time-dependent measurements. Palbociclib suppressed cell proliferation in pRb-expressing cell lines; the IC50 values for palbociclib were 106 nM in MB453 cells and 285 nM in MB231 cells following 120 h treatment (Fig. 1b). Drug-mediated inhibitory effects were not observed in either of the pRb-deficient cells when they were treated with at least 1 µM palbociclib for 120 h (Fig. 1c). These results are consistent with a previous report on pRb-deficient cells [31].
Palbociclib suppressed proliferation of pRb-expressing TNBC cells. a Cell lysates were evaluated for phospho-pRb and pRb expression by Western blot. β-actin is shown as loading control. b MB231 and MB453 cells, and c MB468 and CAL148 were treated with palbociclib at the indicated concentrations and cell proliferation was assessed by MTT assay after 24, 72, and 120 h incubation. Results of MTT assay are expressed as the ratio of control at the time, and are mean values ± SD at each palbocilcib concentration, from triplicate measurements for each treatment
Combination of palbociclib and MLN0128 synergistically inhibits cell proliferation, and suppresses colony formation ability in pRb-expressing ER-negative breast cancer cell lines
To investigate the effect of the combination, we performed an MTT assay and combination index analysis using CalcuSyn software. Cells were treated with palbociclib and/or MLN0128; the MTT assay was performed after 120 h of treatment. The combination index analysis revealed that the two drugs acted synergistically in pRb-expressing MB231 and MB453 cells for almost all the concentrations we examined (Fig. 2a, b). However, no effect was observed in pRb-deficient MB468 cells and CAL148 cells (Fig. 2c). We also examined everolimus in combination with palbociclib. When it was used alone, everolimus was a significantly less potent inhibitor than MLN0128. We did not observe synergistic effects when we treated MB231 and MB453 cells with everolimus at 7.8125 nM (Fig. 2d). Synergistic activity was observed when higher concentrations of everolimus were used. Based on these results, we decided to further assess the dual mTOR inhibitor rather than everolimus.
Combination of palbocilclib and MLN0128 synergistically inhibited proliferation of MB231 and MB453. a, c MB231, MB453, MB468, and CAL148 cells were treated with palbociclib and/or MLN0128 for 120 h. The X axis shows palbociclib concentration. b Combination index (CI) was calculated in MB231 and in MB453. CI > 1 means antagonistic effect, = 1 means additive effect, and < 1 means synergistic effect. d MB231 and MB453 cells were treated with palbociclib and/or everolimus at the indicated concentrations. Results of MTT assay are expressed as the ratio of control, and are mean ± SD at each treatment concentration, from triplicate measurements for each treatment
We confirmed the ability of palbociclib + MLN0128 to suppress cell proliferation by assessing its impact on single cell growth into a colony. For these colony formation assays, pRb-expressing MB231 and MB453 cell lines were subjected to sustained treatment with control, single drug, or the two-drug combination. The combination treatment significantly suppressed colony formation in both cell lines compared to the control or single drug treatment (Fig. 3a, b). The colony numbers were reduced over 95% or 85% in both cell lines as compared to the control or palbociclib only, respectively.
The combination treatment suppressed colony formation ability in MB231 and MB453 cells. a MB231 cells were plated into 6-well plates in 2 ml complete media at 1000 cells/well. Cells were treated with or without palbociclib at 250 nM and/or MLN0128 at 31.25 µM for 7 days. MB453 cells were plated at 2000 cells/well and treated with or without palbociclib at 62.5 nM and/or MLN0128 at 7.8125 nM for 21 days. b Colony numbers from the four treatment groups were counted. Data are mean values ± SD, from duplicate measurements for each treatment. Statistic analyses were subjected unpaired t test compared to the combination treatment. *p < 0.05, **p < 0.01
The combination of palbociclib and MLN0128 induces G1 arrest, and suppresses G1/S transition and mTOR pathway
We performed cell cycle analysis on MB231 and MB453 cells using flow cytometry. Palbociclib induced G1 arrest and the combination with MLN0128 enhanced G1 arrest further (Fig. 4a). We also examined the expression of cleaved PARP, which serves as a marker of cells undergoing apoptosis. Both the single drug treatments and the two-drug combination failed to change levels of cleaved PARP in MB231 and MB453 cells (data not shown). According to these results, the effects of the combination are mainly a product of cell cycle arrest rather than cell death.
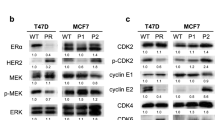
The combination induced G1 arrest and reduced G1/S transition related molecules and mTOR pathway. MB231 cells were treated for 48 h with or without palbociclib at 250 nM and/or MLN0128 at 31.25 µM. MB453 cells were treated for 48 h with or without palbociclib at 62.5 nM and/or MLN0128 at 7.8125 nM. a Flow cytometric analyses were performed in MB231 and MB453. Data are expressed as cell population (%) and mean values ± SD, from duplicate measurements for each treatment. Statistic analyses of G1 cell population were subjected unpaired t test compared to control or combination treatment. *p < 0.05, **p < 0.01. b, c Lysates were prepared from cells from each treatment and evaluated through Western blot analysis. Arrows indicate the target bands. β-actin is shown as the loading control. d Cyclin E1 mRNA levels in MB231 and MB453 were measured by realtime PCR. ACTB was used as a reference. Data are expressed as the ratio of control and mean values ± SD, from triplicate measurements for each treatment. **p < 0.01
To investigate molecular changes related to the G1/S transition and mTOR pathway, we performed Western blot analysis in MB231 and MB453 cells. Both palbociclib and MLN0128 reduced the levels of phopho-pRB (Fig. 4b). The level of total pRB in MB231 cells was decreased as well by the treatment of palbociclib. Treatment with palbociclib also suppressed phopho-p70S6K, which is used as a marker of mTOR activity, although it did not suppress phospho-mTOR (Fig. 4c). The cyclin D1/CDK4 complex has been reported to interact with TSC2. Correspondingly, CDK4/6 inhibitors have been shown to reduce TSC2 phosphorylation and attenuate mTOR activity in breast cancer cell lines [32]. According to a study by Herrea-Abreu et al. treatment with a CDK4/6 inhibitor increased cyclin D1 expression levels; whereas a combination of a CDK4/6 inhibitor and PI3K inhibitor reduced cyclin D1. The reduction may be the mechanism that underlies synergism between CDK4/6 and PI3K inhibitors [33]. As such, we also assessed here how our single drugs and two-drug combination affected the expression of cyclin D1. According to our results and those of others, palbociclib increased levels of cyclin D1, more clearly in MB231 cells. The treatment with palbociclib alone also slightly increased the expression of cyclin E1 protein. However, the two-drug combination reduced protein levels of cyclin E1 in both cell lines by comparing to those in cells treated with palbociclib alone (Fig. 4b). The combination of MLN0128 and palbociclib decreased cyclin E1 mRNA levels (Fig. 4d). Additionally, both palbociclib alone and the combination suppressed cyclin E2, which may also reflect G1 arrest.
Palbociclib in combination with MLN0128 shows a cooperative anti-tumor effect in pRb-expressing TNBC PDX tumor
To examine the effects of the combination in vivo, a TNBC PDX model was used. We performed Western blot analysis to identify a TNBC PDX line that expresses pRb. COH_GS6 consistently expressed pRb although the levels of phospho-pRb were more variable (Fig. 5a). PDX tumors often show different molecular expression in each tumor. We used the highest phosho-pRb expressing COH_GS6 tumor for our study.
Palbociclib in combination with MLN0128 showed a cooperative anti-tumor effect in pRb-expressing TNBC PDX tumors. a Expressions of phospho-pRb and pRb were examined by Western blot in 3 different untreated tumors of COH_GS6. b Mice bearing COH_GS6 tumor received control vehicle, MLN0128, and/or palbociclib. All vehicle and drugs were administered 6 days each week. Data of tumor growth rate are expressed as the percentage of each tumor size on day 0, and are mean ± SEM. Tumor volume was monitored once a week. (n = 7). c Tumors were collected and their weights were measured on day 39. Black bars show mean values and the error bars represent SEM. d Pictures of tumors were taken when tumors were collected. The scale (cm) has been placed below the tumors. e Mice body weight was monitored at the time of treatment. Each color shows the body weight of each group of mice. Data are mean values ± SEM. f Tumor lysates were prepared. Tumors were collected 6 h after oral gavage of drugs at the last day. Western blot was performed using indicated antibodies. β-actin is shown as the loading control. g Representative image of IHC of Ki67 are shown for each treatment condition. A scale bar of 200 µm is shown below the images. h Data are expressed as the percentage of Ki67 positive cells in harvested tumors receiving each treatment [palbociclib group (n = 3), and other groups (n = 4)]. The boxes show the first quartile and third quartile of data and the lines in the box show median values. The bars at the end of box show 1.5 IQR. Statistic analyses were subjected to one-way ANOVA with Tukey’s multiple comparison post-hoc test for data of (b), (c), and (h), and unpaired t test for data of (e). *p < 0.05, **p < 0.01, ***p = 0.001
Mice bearing COH_GS6 tumors were treated 6 days a week with vehicle, palbociclib, MLN0128, or a combination of palbociclib and MLN0128. Both palbociclib and MLN0128 alone suppressed tumor growth; but the combination treatment induced further suppression of tumor growth compared to control or single treatment (Fig. 5b–d). No significant changes in mouse body weight were found in these treatment groups compared to vehicle control during the treatment period (Fig. 5e).
To investigate the mechanism of growth suppression, we performed both Western blot and IHC analyses. Consistent with our in vitro results, phosphorylation of pRb and S6 were inhibited by MLN0128, palbociclib, and the combination, compared to the vehicle control (Fig. 5f). The expression of phopho-p70 S6K was too weak to detect in this tumor (data not shown). To confirm that the drug combination inhibited cell proliferation, we performed IHC analysis to examine the Ki67 score in the PDX tumors. As we expected, the Ki67 score was significantly decreased by the combination treatment compared to control or single treatment (Fig. 5g, h). These results confirm that the combination of palbociclib and MLN0128 has a synergistic suppressive effect on the growth of pRb-expressing TNBC tumors in vivo.
Discussion
Despite its sensitivity to cytotoxic drugs, TNBC typically has a poor prognosis. For patients with TNBC, this poor outlook can be partly attributed to a lack of effective targeted therapies. Palbociclib, a CDK4/6 inhibitor, is well tolerated in a clinical setting. In combination with hormone therapy, it has been investigated in many clinical trials for patients with ER-positive breast cancer. However, to the best of our knowledge, few clinical trials have assessed palbociclib in patients with TNBC. The few clinical studies of the drug for TNBC have probed palbociclib in combination with either paclitaxel or bicalutamide (NCT01320592, NCT02605486). For example, a combination of palbociclib and paclitaxel exhibited prolonged tumor responses but also an accompanying grade 3/4 neutropenia, which frequently led to either dose reduction or interruption. These results prompted a currently ongoing Phase 1 study of a reduced palbociclib regimen. Similarly, a Phase 1/2 trial is currently recruiting to study a combination of palbociclib and bicalutamide for AR + TNBC. Combinations of palbociclib with other agents, such as PI3K inhibitors, have been also considered [18]. For the most part, such regimens are too toxic. For example, a Phase 3 randomized BELLE2 study investigated the efficacy of BKM120 (a panisoform PI3K inhibitor) plus fulvestrant in post-menopausal women with advanced ER-positive HER2-negative breast cancer. The addition of BKM120 improved progression free survival (PFS) from 5.0 to 6.9 months; but the study did not support the use of BKM120 because the magnitude of benefit was small, considering the toxicity [34]. Four Phase 1 and 2 clinical trials have investigated a combination of 3 drugs—hormone therapy, palbociclib, and a PI3K inhibitor—in patients with ER-positive and HER2-negative breast cancer (NCT03006172, NCT03128619, NCT03377101, NCT02684032). However, patients with TNBC were not assessed.
In addition to examining these combinations of CDK4/6 and PI3K inhibitors, several preclinical studies have assessed how CDK4/6 inhibitors interact with everolimus; the combinations have been probed in glioblastoma and head and neck squamous cell carcinoma [35, 36]. Everolimus is a selective mTORC1 inhibitor that has been approved for ER-positive HER2-negative breast cancer. Here, we assessed the in vitro effects of palbociclib plus everolimus in three TNBC cell lines and a HER2 positive/ER-negative cell line. According to our results, the combination produced weak synergistic effects in MB231 and MB453 cells, but only at very high concentrations. The IC50 values of everolimus were over 1 µM in MB231 and 76.0 nM in MB453. In contrast, the IC50 values of MLN0128 were 72.7 nM in MB231 and 16.1 nM in MB453 for 3 days of treatment. These results indicate that the potency of the mTOR inhibitor is critical for the combination to work effectively. In a previously reported in vivo study, everolimus produced variable responses in TNBC [37]. In a Phase 2 clinical trial, everolimus failed to produce either partial or complete responses; nor did it elicit 6 months stable disease in any of the five ER-negative HER2-negative patients with metastatic breast cancer [38]. Several reports (including in vitro studies) have described how combinations of various CDK4/6 and mTOR inhibitors impacted pancreatic cell lines and TNBC cell lines; also, a study of the combination plus hormone therapy was performed in ER-positive breast cancer [18, 39,40,41]. Here, a combination of palbociclib and the dual mTORC inhibitor MLN0128 had synergistic suppressive effects at almost all concentrations we examined (Fig. 2). We are encouraged by the synergism we observed between palbociclib and MLN0128 for TNBC. Taken altogether, the combination of a CDK4/6 inhibitor and MLN0128 may hold potential for treating patients with TNBC.
Inhibition of CDK4/6 has been reported to (1) suppress phosphorylation of AKT and ERK in head and neck squamous cell carcinoma [36]; and (2) upregulate phosphorylation of AKT in malignant pleural mesothelioma cells and TNBC cell lines [42, 43]. Thus, we also examined the effect of palbociclib on phosphorylation of AKT and ERK in TNBC as well as a HER2+/ER− cell line. We did not observe any changes for these cell lines (data not shown). There also have been conflicting reports about the effect of CDK4/6 inhibitors on the mTOR pathway. On the one hand, CDK4/6 inhibitors are thought to upregulate the mTOR pathway in pancreatic cancer and ER+ breast cancer [39, 44]. On the other hand, they appear to suppress the mTOR pathway in glioblastoma and lymphoblastic leukemia [35, 45]. Previous studies from our laboratory have found that CDK4/6 inhibitor treatment is not effective in everolimus-resistant MCF-7aro [46]. Thus, the effectiveness of CDK4/6 inhibitors depends on molecular features of cancers. In our study, the mTOR pathway was blocked by palbociclib in ER-negative breast cancer cell lines, including TNBC and HER2+/ER- cell lines (Fig. 4c). We also confirmed this mTOR suppression by palbociclib in vivo (Fig. 5f). Similarly, the two-drug combination effectively suppresses the mTOR pathway.
Tolerated doses of palbociclib are different in different in vivo preclinical studies. Published dosages range from 25 to 150 mg/kg/day [28, 31, 35, 39]. Vijayaraghavan et al. reported that 25 or 50 mg/kg/day doses were well tolerated in nude mice; however, 75 and 150 mg/kg/day doses were not tolerated [28]. We decided to use palbociclib at 50 mg/kg/day for 6 days a week, which was well tolerated. MLN0128 at 1 mg/kg/day has been reported to decrease Ki67 positive cells in Merkel cell carcinoma [47]. In our study, Ki67 positive cells in COH_GS6 PDX tumors were not significantly decreased by MLN0128 at 0.3 mg/kg/day or palbociclib at 50 mg/kg/day. However, they were significantly decreased by the combination treatment. Thus, our in vitro and in vivo data demonstrated that the combination of palbociclib and MLN0128 can suppress cell proliferation and tumor growth synergistically.
Conclusions
In this study, we showed that a combination of the CDK4/6 inhibitor palbociclib and the dual mTOR kinase inhibitor MLN0128 had synergistic anti-cancer activity in pRb + ER-negative breast cancer cell lines and a TNBC PDX model. This drug combination has a potent synergistic inhibitory effect on pRb-expressing TNBC and does not appear to have severe associated toxicity. Palbociclib has already been used clinically and MLN0128 has been investigated in breast cancer clinical trials (Supplementary Table S1). In addition, one of the advantages of such treatment is that both drugs are orally active. Our study suggests that the combination of a CDK4/6 inhibitor and dual mTOR inhibitor, such as those described, may offer a new targeted therapy for patients with TNBC, and this combination therapy is worthy of further investigation in a clinical setting.
Abbreviations
- CDK:
-
Cyclin-dependent kinase
- DMSO:
-
Dimethyl sulfoxide
- EMT:
-
Epithelialmesenchymal transition
- FBS:
-
Fetal bovine serum
- IHC:
-
Immunohistochemistry
- mTOR:
-
The mammalian target of rapamycin
- MTT:
-
3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide
- NSG:
-
NOD-scid/IL2Rγ−/−
- PBS:
-
Phosphate-buffered saline
- PDX:
-
Patient-derived xenograft
- PI3K:
-
Phosphatidylinositol 3-kinase
- pRb:
-
Retinoblastoma protein
- TNBC:
-
Triple negative breast cancer
References
Siegel RL, Miller KD, Jemal A (2016) Cancer statistics, 2016. CA Cancer J Clin 66(1):7–30. https://doi.org/10.3322/caac.21332
Yang XR, Chang-Claude J, Goode EL, Couch FJ, Nevanlinna H, Milne RL, Gaudet M, Schmidt MK, Broeks A, Cox A, Fasching PA, Hein R, Spurdle AB, Blows F, Driver K, Flesch-Janys D, Heinz J, Sinn P, Vrieling A, Heikkinen T, Aittomaki K, Heikkila P, Blomqvist C,Lissowska J, Peplonska B, Chanock S, Figueroa J, Brinton L, Hall P, Czene K, Humphreys K, Darabi H, Liu J, Van ‘t Veer LJ, van Leeuwen FE, Andrulis IL, Glendon G, Knight JA, Mulligan AM, O’Malley FP, Weerasooriya N, John EM, Beckmann MW, Hartmann A, Weihbrecht SB, Wachter DL, Jud SM, Loehberg CR, Baglietto L, English DR, Giles GG, McLean CA,Severi G, Lambrechts D, Vandorpe T, Weltens C, Paridaens R, Smeets A, Neven P, Wildiers H, Wang X, Olson JE, Cafourek V, Fredericksen Z, Kosel M, Vachon C, Cramp HE, Connley D, Cross SS, Balasubramanian SP, Reed MW, Dork T, Bremer M, Meyer A, Karstens JH,Ay A, Park-Simon TW, Hillemanns P, Arias Perez JI, Menendez Rodriguez P, Zamora P,Benitez J, Ko YD, Fischer HP, Hamann U, Pesch B, Bruning T, Justenhoven C, Brauch H, Eccles DM, Tapper WJ, Gerty SM, Sawyer EJ, Tomlinson IP, Jones A, Kerin M, Miller N, McInerney N, Anton-Culver H, Ziogas A, Shen CY, Hsiung CN, Wu PE, Yang SL, Yu JC,Chen ST, Hsu GC, Haiman CA, Henderson BE, Le Marchand L, Kolonel LN, Lindblom A, Margolin S, Jakubowska A, Lubinski J, Huzarski T, Byrski T, Gorski B, Gronwald J, Hooning MJ,Hollestelle A, van den Ouweland AM, Jager A, Kriege M, Tilanus-Linthorst MM, Collee M, Wang-Gohrke S, Pylkas K, Jukkola-Vuorinen A, Mononen K, Grip M, Hirvikoski P, Winqvist R, Mannermaa A, Kosma VM, Kauppinen J, Kataja V, Auvinen P, Soini Y, Sironen R, Bojesen SE, Orsted DD, Kaur-Knudsen D, Flyger H, Nordestgaard BG, Holland H, Chenevix-Trench G, Manoukian S, Barile M, Radice P, Hankinson SE, Hunter DJ, Tamimi R, Sangrajrang S, Brennan P, McKay J, Odefrey F, Gaborieau V, Devilee P, Huijts PE, Tollenaar RA,Seynaeve C, Dite GS, Apicella C, Hopper JL, Hammet F, Tsimiklis H, Smith LD, Southey MC, Humphreys MK, Easton D, Pharoah P, Sherman ME, Garcia-Closas M (2011) Associations of breast cancer risk factors with tumor subtypes: a pooled analysis from the Breast Cancer Association Consortium studies. J Natl Cancer Inst 103(3):250–263. https://doi.org/10.1093/jnci/djq526
Bauer KR, Brown M, Cress RD, Parise CA, Caggiano V (2007) Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-negative invasive breast cancer, the so-called triple-negative phenotype: a population-based study from the California cancer Registry. Cancer 109(9):1721–1728. https://doi.org/10.1002/cncr.22618
Parise CA, Bauer KR, Brown MM, Caggiano V (2009) Breast cancer subtypes as defined by the estrogen receptor (ER), progesterone receptor (PR), and the human epidermal growth factor receptor 2 (HER2) among women with invasive breast cancer in California, 1999–2004. Breast J 15(6):593–602. https://doi.org/10.1111/j.1524-4741.2009.00822.x
Kim EK, Noh WC, Han W, Noh DY (2011) Prognostic significance of young age (< 35 years) by subtype based on ER, PR, and HER2 status in breast cancer: a nationwide registry-based study. World J Surg 35(6):1244–1253. https://doi.org/10.1007/s00268-011-1071-1
Liedtke C, Mazouni C, Hess KR, Andre F, Tordai A, Mejia JA, Symmans WF, Gonzalez-Angulo AM, Hennessy B, Green M, Cristofanilli M, Hortobagyi GN, Pusztai L (2008) Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J Clin Oncol 26(8):1275–1281. https://doi.org/10.1200/JCO.2007.14.4147
von Minckwitz G, Untch M, Blohmer JU, Costa SD, Eidtmann H, Fasching PA, Gerber B, Eiermann W, Hilfrich J, Huober J, Jackisch C, Kaufmann M, Konecny GE, Denkert C, Nekljudova V, Mehta K, Loibl S (2012) Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol 30(15):1796–1804. https://doi.org/10.1200/JCO.2011.38.8595
Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, Bonnefoi H, Cameron D, Gianni L, Valagussa P, Swain SM, Prowell T, Loibl S, Wickerham DL, Bogaerts J, Baselga J, Perou C, Blumenthal G, Blohmer J, Mamounas EP, Bergh J, Semiglazov V, Justice R, Eidtmann H, Paik S, Piccart M, Sridhara R, Fasching PA, Slaets L, Tang S, Gerber B, Geyer CE Jr, Pazdur R, Ditsch N, Rastogi P, Eiermann W, von Minckwitz G (2014) Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet 384(9938):164–172. https://doi.org/10.1016/S0140-6736(13)62422-8
Beaver JA, Amiri-Kordestani L, Charlab R, Chen W, Palmby T, Tilley A, Zirkelbach JF, Yu J, Liu Q, Zhao L, Crich J, Chen XH, Hughes M, Bloomquist E, Tang S, Sridhara R, Kluetz PG, Kim G, Ibrahim A, Pazdur R, Cortazar P (2015) FDA approval: palbociclib for the treatment of postmenopausal patients with estrogen receptor-positive, HER2-negative metastatic breast cancer. Clin Cancer Res 21(21):4760–4766. https://doi.org/10.1158/1078-0432.CCR-15-1185
Dhillon S (2015) Palbociclib: first global approval. Drugs 75(5):543–551. https://doi.org/10.1007/s40265-015-0379-9
Harbour JW, Dean DC (2000) The Rb/E2F pathway: expanding roles and emerging paradigms. Genes Dev 14(19):2393–2409
Ehab M, Elbaz M (2016) Profile of palbociclib in the treatment of metastatic breast cancer. Breast Cancer (Dove Med Press) 8:83–91. https://doi.org/10.2147/BCTT.S83146
Dean JL, Thangavel C, McClendon AK, Reed CA, Knudsen ES (2010) Therapeutic CDK4/6 inhibition in breast cancer: key mechanisms of response and failure. Oncogene 29(28):4018–4032. https://doi.org/10.1038/onc.2010.154
Stefansson OA, Jonasson JG, Olafsdottir K, Hilmarsdottir H, Olafsdottir G, Esteller M, Johannsson OT, Eyfjord JE (2011) CpG island hypermethylation of BRCA1 and loss of pRb as co-occurring events in basal/triple-negative breast cancer. Epigenetics 6(5):638–649. https://doi.org/10.4161/epi.6.5.15667
Trere D, Brighenti E, Donati G, Ceccarelli C, Santini D, Taffurelli M, Montanaro L, Derenzini M (2009) High prevalence of retinoblastoma protein loss in triple-negative breast cancers and its association with a good prognosis in patients treated with adjuvant chemotherapy. Ann Oncol 20(11):1818–1823. https://doi.org/10.1093/annonc/mdp209
Ertel A, Dean JL, Rui H, Liu C, Witkiewicz AK, Knudsen KE, Knudsen ES (2010) RB-pathway disruption in breast cancer: differential association with disease subtypes, disease-specific prognosis and therapeutic response. Cell Cycle 9(20):4153–4163. https://doi.org/10.4161/cc.9.20.13454
Witkiewicz AK, Ertel A, McFalls J, Valsecchi ME, Schwartz G, Knudsen ES (2012) RB-pathway disruption is associated with improved response to neoadjuvant chemotherapy in breast cancer. Clin Cancer Res 18(18):5110–5122. https://doi.org/10.1158/1078-0432.CCR-12-0903
Asghar US, Barr AR, Cutts R, Beaney M, Babina I, Sampath D, Giltnane J, Lacap JA, Crocker L, Young A, Pearson A, Herrera-Abreu MT, Bakal C, Turner NC (2017) Single-cell dynamics determines response to CDK4/6 inhibition in triple-negative breast cancer. Clin Cancer Res 23(18):5561–5572. https://doi.org/10.1158/1078-0432.CCR-17-0369
Stemke-Hale K, Gonzalez-Angulo AM, Lluch A, Neve RM, Kuo WL, Davies M, Carey M, Hu Z, Guan Y, Sahin A, Symmans WF, Pusztai L, Nolden LK, Horlings H, Berns K, Hung MC, van de Vijver MJ, Valero V, Gray JW, Bernards R, Mills GB, Hennessy BT (2008) An integrative genomic and proteomic analysis of PIK3CA, PTEN, and AKT mutations in breast cancer. Cancer Res 68(15):6084–6091. https://doi.org/10.1158/0008-5472.CAN-07-6854
Meric-Bernstam F, Gonzalez-Angulo AM (2009) Targeting the mTOR signaling network for cancer therapy. J Clin Oncol 27(13):2278–2287. https://doi.org/10.1200/JCO.2008.20.0766
Ramirez-Valle F, Badura ML, Braunstein S, Narasimhan M, Schneider RJ (2010) Mitotic raptor promotes mTORC1 activity, G(2)/M cell cycle progression, and internal ribosome entry site-mediated mRNA translation. Mol Cell Biol 30(13):3151–3164. https://doi.org/10.1128/MCB.00322-09
Cuyas E, Corominas-Faja B, Joven J, Menendez JA (2014) Cell cycle regulation by the nutrient-sensing mammalian target of rapamycin (mTOR) pathway. Methods Mol Biol 1170:113–144. https://doi.org/10.1007/978-1-4939-0888-2_7
Montero JC, Esparis-Ogando A, Re-Louhau MF, Seoane S, Abad M, Calero R, Ocana A, Pandiella A (2014) Active kinase profiling, genetic and pharmacological data define mTOR as an important common target in triple-negative breast cancer. Oncogene 33(2):148–156. https://doi.org/10.1038/onc.2012.572
Laplante M, Sabatini DM (2012) mTOR signaling in growth control and disease. Cell 149(2):274–293. https://doi.org/10.1016/j.cell.2012.03.017
Gokmen-Polar Y, Liu Y, Toroni RA, Sanders KL, Mehta R, Badve S, Rommel C, Sledge GW Jr (2012) Investigational drug MLN0128, a novel TORC1/2 inhibitor, demonstrates potent oral antitumor activity in human breast cancer xenograft models. Breast Cancer Res Treat 136(3):673–682. https://doi.org/10.1007/s10549-012-2298-8
Jernstrom S, Hongisto V, Leivonen SK, Due EU, Tadele DS, Edgren H, Kallioniemi O, Perala M, Maelandsmo GM, Sahlberg KK (2017) Drug-screening and genomic analyses of HER2-positive breast cancer cell lines reveal predictors for treatment response. Breast Cancer (Dove Med Press) 9:185–198. https://doi.org/10.2147/BCTT.S115600
Kanaya N, Somlo G, Wu J, Frankel P, Kai M, Liu X, Wu SV, Nguyen D, Chan N, Hsieh MY, Kirschenbaum M, Kruper L, Vito C, Badie B, Yim JH, Yuan Y, Hurria A, Peiguo C, Mortimer J, Chen S (2017) Characterization of patient-derived tumor xenografts (PDXs) as models for estrogen receptor positive (ER+ HER2− and ER+ HER2+) breast cancers. J Steroid Biochem Mol Biol 170:65–74. https://doi.org/10.1016/j.jsbmb.2016.05.001
Vijayaraghavan S, Karakas C, Doostan I, Chen X, Bui T, Yi M, Raghavendra AS, Zhao Y, Bashour SI, Ibrahim NK, Karuturi M, Wang J, Winkler JD, Amaravadi RK, Hunt KK, Tripathy D, Keyomarsi K (2017) CDK4/6 and autophagy inhibitors synergistically induce senescence in Rb positive cytoplasmic cyclin E negative cancers. Nat Commun 8:15916. https://doi.org/10.1038/ncomms15916
Tomayko MM, Reynolds CP (1989) Determination of subcutaneous tumor size in athymic (nude) mice. Cancer Chemother Pharmacol 24(3):148–154
Dowsett M, Nielsen TO, A’Hern R, Bartlett J, Coombes RC, Cuzick J, Ellis M, Henry NL, Hugh JC, Lively T, McShane L, Paik S, Penault-Llorca F, Prudkin L, Regan M, Salter J, Sotiriou C, Smith IE, Viale G, Zujewski JA, Hayes DF, International Ki-67 in breast cancer working G (2011) assessment of Ki67 in breast cancer: recommendations from the International Ki67 in Breast Cancer working group. J Natl Cancer Inst 103 (22):1656–1664. https://doi.org/10.1093/jnci/djr393
Fry DW, Harvey PJ, Keller PR, Elliott WL, Meade M, Trachet E, Albassam M, Zheng X, Leopold WR, Pryer NK, Toogood PL (2004) Specific inhibition of cyclin-dependent kinase 4/6 by PD 0332991 and associated antitumor activity in human tumor xenografts. Mol Cancer Ther 3(11):1427–1438
Goel S, Wang Q, Watt AC, Tolaney SM, Dillon DA, Li W, Ramm S, Palmer AC, Yuzugullu H, Varadan V, Tuck D, Harris LN, Wong KK, Liu XS, Sicinski P, Winer EP, Krop IE, Zhao JJ (2016) Overcoming therapeutic resistance in HER2-positive breast cancers with CDK4/6 inhibitors. Cancer Cell 29(3):255–269. https://doi.org/10.1016/j.ccell.2016.02.006
Herrera-Abreu MT, Palafox M, Asghar U, Rivas MA, Cutts RJ, Garcia-Murillas I, Pearson A, Guzman M, Rodriguez O, Grueso J, Bellet M, Cortes J, Elliott R, Pancholi S, Baselga J, Dowsett M, Martin LA, Turner NC, Serra V (2016) Early adaptation and acquired resistance to CDK4/6 inhibition in estrogen receptor-positive breast cancer. Cancer Res 76(8):2301–2313. https://doi.org/10.1158/0008-5472.CAN-15-0728
Baselga J, Im SA, Iwata H, Cortes J, De Laurentiis M, Jiang Z, Arteaga CL, Jonat W, Clemons M, Ito Y, Awada A, Chia S, Jagiello-Gruszfeld A, Pistilli B, Tseng LM, Hurvitz S, Masuda N, Takahashi M, Vuylsteke P, Hachemi S, Dharan B, Di Tomaso E, Urban P, Massacesi C, Campone M (2017) Buparlisib plus fulvestrant versus placebo plus fulvestrant in postmenopausal, hormone receptor-positive, HER2-negative, advanced breast cancer (BELLE-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol 18(7):904–916. https://doi.org/10.1016/S1470-2045(17)30376-5
Olmez I, Brenneman B, Xiao A, Serbulea V, Benamar M, Zhang Y, Manigat L, Abbas T, Lee J, Nakano I, Godlewski J, Bronisz A, Abounader R, Leitinger N, Purow B (2017) Combined CDK4/6 and mTOR inhibition is synergistic against glioblastoma via multiple mechanisms. Clin Cancer Res 23(22):6958–6968. https://doi.org/10.1158/1078-0432.CCR-17-0803
Ku BM, Yi SY, Koh J, Bae YH, Sun JM, Lee SH, Ahn JS, Park K, Ahn MJ (2016) The CDK4/6 inhibitor LY2835219 has potent activity in combination with mTOR inhibitor in head and neck squamous cell carcinoma. Oncotarget 7(12):14803–14813. https://doi.org/10.18632/oncotarget.7543
Euceda LR, Hill DK, Stokke E, Hatem R, El Botty R, Bieche I, Marangoni E, Bathen TF, Moestue SA (2017) Metabolic response to everolimus in patient-derived triple-negative breast cancer xenografts. J Proteome Res 16(5):1868–1879. https://doi.org/10.1021/acs.jproteome.6b00918
Ellard SL, Clemons M, Gelmon KA, Norris B, Kennecke H, Chia S, Pritchard K, Eisen A, Vandenberg T, Taylor M, Sauerbrei E, Mishaeli M, Huntsman D, Walsh W, Olivo M, McIntosh L, Seymour L (2009) Randomized phase II study comparing two schedules of everolimus in patients with recurrent/metastatic breast cancer: NCIC Clinical Trials Group IND.163. J Clin Oncol 27(27):4536–4541. https://doi.org/10.1200/JCO.2008.21.3033
Franco J, Balaji U, Freinkman E, Witkiewicz AK, Knudsen ES (2016) Metabolic reprogramming of pancreatic cancer mediated by CDK4/6 inhibition elicits unique vulnerabilities. Cell Rep 14(5):979–990. https://doi.org/10.1016/j.celrep.2015.12.094
Franco J, Witkiewicz AK, Knudsen ES (2014) CDK4/6 inhibitors have potent activity in combination with pathway selective therapeutic agents in models of pancreatic cancer. Oncotarget 5(15):6512–6525. https://doi.org/10.18632/oncotarget.2270
Michaloglou C, Crafter C, Siersbaek R, Delpuech O, Curwen JO, Carnevalli LS, Staniszewska AD, Polanska UM, Cheraghchi-Bashi A, Lawson M, Chernukhin I, McEwen R, Carroll JS, Cosulich SC (2018) Combined inhibition of mTOR and CDK4/6 is required for optimal blockade of E2F function and long-term growth inhibition in estrogen receptor-positive breast cancer. Mol Cancer Ther 17(5):908–920. https://doi.org/10.1158/1535-7163.MCT-17-0537
Bonelli MA, Digiacomo G, Fumarola C, Alfieri R, Quaini F, Falco A, Madeddu D, La Monica S, Cretella D, Ravelli A, Ulivi P, Tebaldi M, Calistri D, Delmonte A, Ampollini L, Carbognani P, Tiseo M, Cavazzoni A, Petronini PG (2017) Combined inhibition of CDK4/6 and PI3K/AKT/mTOR pathways induces a synergistic anti-tumor effect in malignant pleural mesothelioma cells. Neoplasia 19(8):637–648. https://doi.org/10.1016/j.neo.2017.05.003
Cretella D, Ravelli A, Fumarola C, La Monica S, Digiacomo G, Cavazzoni A, Alfieri R, Biondi A, Generali D, Bonelli M, Petronini PG (2018) The anti-tumor efficacy of CDK4/6 inhibition is enhanced by the combination with PI3K/AKT/mTOR inhibitors through impairment of glucose metabolism in TNBC cells. J Exp Clin Cancer Res 37(1):72. https://doi.org/10.1186/s13046-018-0741-3
Jansen VM, Bhola NE, Bauer JA, Formisano L, Lee KM, Hutchinson KE, Witkiewicz AK, Moore PD, Estrada MV, Sanchez V, Ericsson PG, Sanders ME, Pohlmann PR, Pishvaian MJ, Riddle DA, Dugger TC, Wei W, Knudsen ES, Arteaga CL (2017) Kinome-wide RNA interference screen reveals a role for PDK1 in acquired resistance to CDK4/6 inhibition in ER-positive breast cancer. Cancer Res 77(9):2488–2499. https://doi.org/10.1158/0008-5472.CAN-16-2653
Pikman Y, Alexe G, Roti G, Conway AS, Furman A, Lee ES, Place AE, Kim S, Saran C, Modiste R, Weinstock DM, Harris M, Kung AL, Silverman LB, Stegmaier K (2017) Synergistic drug combinations with a CDK4/6 inhibitor in T-cell acute lymphoblastic leukemia. Clin Cancer Res 23(4):1012–1024. https://doi.org/10.1158/1078-0432.CCR-15-2869
Petrossian K, Kanaya N, Lo C, Hsu PY, Nguyen D, Yang L, Yang L, Warden C, Wu X, Pillai R, Bernal L, Huang CS, Kruper L, Yuan Y, Somlo G, Mortimer J, Chen S (2018) ERalpha-mediated cell cycle progression is an important requisite for CDK4/6 inhibitor response in HR+ breast cancer. Oncotarget 9(45):27736–27751. https://doi.org/10.18632/oncotarget.25552
Kannan A, Lin Z, Shao Q, Zhao S, Fang B, Moreno MA, Vural E, Stack BC Jr, Suen JY, Kannan K, Gao L (2016) Dual mTOR inhibitor MLN0128 suppresses Merkel cell carcinoma (MCC) xenograft tumor growth. Oncotarget 7(6):6576–6592. https://doi.org/10.18632/oncotarget.5878
Acknowledgements
Research reported in this publication included works performed in the Analytical Cytometry Core, Pathology Research Services Pathology Core, and Animal Resource Center supported by the NCI (P30CA033572). We also want to thank the patient who donated her tumor tissue for us to generate the PDX, COH_GS6. In addition, we would like to thank Ian Talisman, PhD for editing the manuscript.
Funding
This work was supported by the Panda Charitable Foundation and the National Cancer Institute (P30CA033572) for the use of Analytical Cytometry Core, Pathology Research Services Pathology Core, and Animal Resource Center. SC is the Lester M. and Irene C. Finkelstein Chair in Biology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
All animal research procedures in this study were approved by the Institutional Animal Care and Use Committee at City of Hope. Facilities are credited by Association for Assessment and Accreditation of Laboratory Animal Care and operated according to NIH guidelines. This study was approved by the City of Hope Institutional Review board
Informed consent
Informed consent was obtained from all individual patients prior to tissue collection.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yamamoto, T., Kanaya, N., Somlo, G. et al. Synergistic anti-cancer activity of CDK4/6 inhibitor palbociclib and dual mTOR kinase inhibitor MLN0128 in pRb-expressing ER-negative breast cancer. Breast Cancer Res Treat 174, 615–625 (2019). https://doi.org/10.1007/s10549-018-05104-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-018-05104-9