Abstract
Purpose
Controversy surrounds management of lobular neoplasia (LN), [atypical lobular hyperplasia (ALH) or lobular carcinoma in situ (LCIS)], diagnosed on core needle biopsy (CNB). Retrospective series of pure ALH and LCIS reported “upgrade” rate to DCIS or invasive cancer in 0–40%. Few reports document radiologic/pathologic correlation to exclude cases of discordance that are the likely source of most upgrades, and there is minimal data on outcomes with follow-up imaging and clinical surveillance.
Methods
Cases of LN alone on CNB (2001–2014) were reviewed. CNB yielding LN with other pathologic findings for which surgery was indicated were excluded. All patients had either surgical excision or clinical follow-up with breast imaging. All cases included were subject to radiologic–pathologic correlation after biopsy.
Results
178 cases were identified out of 62213 (0.3%). 115 (65%) patients underwent surgery, and 54 (30%) patients had surveillance for > 12 months (mean = 55 months). Of the patients who underwent surgical excision, 13/115 (11%) were malignant. Eight of these 13 found malignancy at excision when CNB results were considered discordant (5 DCIS, and 3 invasive lobular carcinoma), with the remainder, 5/115 (4%), having a true pathologic upgrade: 3 DCIS, and 2 microinvasive lobular carcinoma. Among 54 patients not having excision, 12/54 (22%) underwent subsequent CNB with only 1 carcinoma found at the initial biopsy site.
Conclusions
Surgical excision of LN yields a low upgrade rate when careful consideration is given to radiologic/pathologic correlation to exclude cases of discordance. Observation with interval breast imaging is a reasonable alternative for most cases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lobular carcinoma in situ (LCIS) found on breast biopsy has increased in incidence (2.75/100,000) over time with broader uptake of screening mammography [1]. Long-term follow-up demonstrates an increased risk of subsequent breast cancer after diagnosis of ALH and LCIS [2,3,4,5]. Management of patients with LCIS or ALH on image-guided core needle biopsy, however, remains controversial, as both are incidental findings, not detected as either calcifications or mass. Over the last two decades, advances in imaging technology such as digital, contrast-enhanced, 3D mammography, and increased utilization of MRI for high risk surveillance (including those with LCIS as a risk factor), has resulted in increased identification of imaging findings, with many consequently warranting biopsy. When CNB demonstrates LN, the main rationale for surgical excision is the possibility of pathologic upgrade to malignancy found in surrounding tissue. Numerous studies have reported series of patients undergoing surgical excision for LN, reporting upgrade to DCIS or invasive carcinoma with a wide range: from 0 to 40% [6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26]. These collective series indicate a large number of patients undergo surgical excision for no benefit, finding only more LCIS/ALH or other benign findings. Furthermore, few authors have examined outcomes in patients with LN on CNB with particular attention to correlation of CNB pathology to clinical and radiologic findings. Even fewer have described outcomes for patients undergoing radiologic follow-up without surgical excision. In this study we examined patients with pure LN on CNB with extended clinical follow-up or immediate surgical excision, each case having had careful clinical radiologic/pathologic correlation at its outset.
Methods
This study was approved by the Mount Sinai Institutional Review Board. Cases of pure LN on CNB between 2001 and 2014 were identified through search of surgical pathology records for diagnoses including LCIS or ALH. CNB yielding LN and any additional pathologic findings for which surgery was indicated (invasive carcinoma, DCIS, papilloma, radial scar, atypical ductal hyperplasia) were excluded. Patients were included only if they had either surgical excision or follow-up breast imaging (mammogram, ultrasound, or breast MRI) within 24 months of the original CNB. All cases included had been subject to radiologic–pathologic correlation after biopsy that included communication and imaging review between pathologist and radiologist who performed the biopsy. In stereotactic CNB performed for mammographic calcifications, the specimen radiographs were submitted with the biopsies, examined, and correlated at the time of slide review by the pathologist. Cases were determined to be discordant when histopathologic diagnosis did not correlate with findings on imaging that stimulated the biopsy (Fig. 1). All breast CNB results were read by 1 of 3 dedicated breast pathologists at our institution; biopsies were performed both at our center as well as surrounding affiliated radiology practices. Clinical and demographic information was collected from the medical record to determine data on follow-up imaging for patients who did not have surgical excision of LN. Strict criteria were used to define LN, and cases with pathologic features consistent with pleomorphic-type LCIS (presence of cytologic atypia, enlarged cells, mitoses, necrosis, and E-cadherin negative) were identified and excluded from determination of “upgrade rate” as excision was clearly indicated based on higher likelihood of malignancy than conventional LCIS. These cases are discussed separately in the results section below.
Two cases of lobular neoplasia found on stereotactic core needle biopsy. In the first case (left), biopsy of an irregular density yielding lobular neoplasia is discordant. In the second case (right) biopsy of microcalcifications yielding lobular neoplasia is concordant with significant sampling of calcifications noted on specimen images
Results
During the 14-year study period, 178 patients were identified who met inclusion criteria (Fig. 2). Mean age of the study population was 54 years (36–82). ALH was diagnosed in 56%; LCIS was diagnosed in 50% of 178 patients. Presentation was by a mass on imaging in 20% of patients while 80% presented with microcalcifications. Abnormal imaging was by mammogram in 75%, ultrasound in 17%, and MRI in 8%. Surgical excision was performed in 115 (65%). 54 (30%) patients were followed with imaging for > 12 months (mean = 55 months; 48 > 2 years, 34 > 3 years, 25 > 4 years, 21 > 5 years), and 9 (5%) patients were followed for < 12 months (mean = 8.2 months). Mean age of patients electing imaging follow-up was similar to that for surgical excisions (57 vs. 53) (Table 1). Similar proportions of patients were seen between the two groups when stratified by diagnosis: 65% of ALH had excision and 68% of LCIS patients had excision. The majority of study patients had calcifications on mammogram and underwent stereotactic core biopsy for diagnosis. In this group 58 and 42% had excision or imaging follow-up, respectively. Patients diagnosed by biopsy via ultrasound or MRI were more likely to undergo excision (78% vs. 22%). Of the 115 patients, 26 had a mass on imaging. Of these 26 most had fibrocystic change or fibroadenomatous change in addition to LN on core biopsy indicating concordance. Four cases (of the 26) had no associated finding with LN on core biopsy of the mass suggesting discordance. At surgical excision these cases revealed LN + fibrocystic change (2 cases), LN alone, and DCIS. Of the patients who underwent surgical excision, biopsy site changes were noted in all specimens confirming excision of the targeted biopsy site. 102/115 (89%) had benign results and 13/115 (11%) malignant. Of these 13 cases, however, 4 demonstrated cytologic features of pleomorphic LCIS on core biopsy mandating excision, resulting in final diagnosis of DCIS (3), or invasive lobular carcinoma (1). In two cases a new segment of calcification led to CNB finding pleomorphic LCIS and fibrocystic change associated with calcifications. Excision was read as low/intermediate DCIS; however, it was noted that differentiation from LCIS was difficult. Features that favored DCIS were larger cell size, acini formation, greater degree of nuclear atypia, mitosis, single cell necrosis, and E-cadherin positivity. The third case involved a small mass that on CNB found pleomorphic LCIS, fibrocystic change, benign cysts, duct ectasia, and calcifications. Excision revealed low-to-intermediate grade DCIS. The fourth case in this category was a CNB of regional pleomorphic calcifications finding pleomorphic LCIS and fibrocystic change with and without calcifications. At surgical excision it was upgraded to a 4 mm invasive lobular carcinoma with a significant amount of residual LCIS throughout the mastectomy specimen, but no DCIS.
Of the remaining 9 cases, 4 found malignancy at excision when CNB results were considered discordant (2 DCIS, and 2 invasive ductal/lobular carcinoma). In this scenario imaging findings were not felt to correlate with pathology results on core biopsy and excision was recommended. In two cases a small mass was identified on mammography and core needle biopsy found LCIS and ALH, respectively. Surgical excision revealed mixed invasive ductal and lobular carcinoma in one case (1 cm) and low grade DCIS involving fibroadenoma in the other. Two additional patients had abnormal MRI enhancement that led to core biopsy with ALH/LCIS. Surgical excision in these cases found a 6 mm invasive ductal carcinoma (with papilloma) and low grade DCIS with fibroadenomatoid change.
The remaining cases, 5/115 (4%), had a true pathologic upgrade in the absence of discordance: 3 DCIS, and 2 invasive lobular carcinoma (Table 2). Incidental microinvasive lobular carcinoma (0.1 cm) was found at lumpectomy in a 50-year-old patient after a 3 cm span of punctate calcifications indicated LCIS with retrieval of numerous calcifications on CNB; however, numerous calcifications remained on post-biopsy mammogram. The excision specimen also contained ADH with calcifications and ALH. All margins were negative. The other upgrade to invasive lobular carcinoma (0.2 cm) occurred in a 54-year-old patient who underwent core needle biopsy for a 3 cm span of new microcalcifications finding fibrocystic changes with calcifications and incidental ALH and LCIS, not associated with calcifications. At lumpectomy multiple foci of invasive lobular carcinoma (max 2 mm) were identified with a close lateral margin as well as calcifications associated with LCIS, ALH, and DCIS extending to the medial margin. A post-excision mammogram indicated additional clusters of microcalcifications in the breast including pleomorphic microcalcifications 6 cm away from the postoperative seroma. This finding led to MRI and ultimate diagnosis of additional invasive lobular carcinoma.
The remaining three cases that we would consider true upgrades involved an ultimate diagnosis of DCIS. One occurred in a 55-year-old patient undergoing CNB for indeterminate microcalcifications yielding ALH (not associated with calcifications) and fibrocystic change with calcifications. At lumpectomy pathology revealed low grade DCIS with LCIS both with calcifications. A second case involved a 53-year-old patient with CNB that indicated ALH with fibrocystic change associated with calcifications. Subsequent lumpectomy showed low grade DCIS and fibrocystic change, both associated with calcifications. The third case was a 49-year-old patient with a history of LCIS 7 years prior who underwent screening MRI with a small focal area of enhancement (normal mammogram and ultrasound) that on CNB revealed LCIS and sclerosing adenosis. The patient elected to have total mastectomy with low-to-intermediate grade DCIS at the biopsy site admixed with LCIS, radial scar, and fibrocystic change.
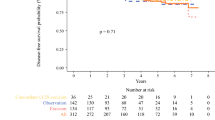
Among 54 patients not having excision, all patients continued to have yearly mammograms. Twenty-one patients (39%) had combination mammogram and US yearly while 7 (13%) had mammogram, US, and MRI. During the observation/surveillance period 12/54 (22%) required subsequent CNB (8 ipsilateral and 4 contralateral) with 3 being in the same location as the initial CNB (2 benign, 1 invasive carcinoma 3 years later). One patient developed an asymmetry on imaging 5 years later at the same location as initial CNB. Repeat CNB revealed scarring, fibrosis, and reactive changes. Another patient with subsequent CNB in the same location was noted to have increased calcifications, some linear, on mammography. Stereotactic biopsy of this site found invasive lobular carcinoma, LCIS, DCIS, and calcifications. The third patient having subsequent CNB in the same location was noted to have “persistent” 1.4 cm mass with central increased echogenicity on ultrasound and a persistent 1 cm mass on mammogram 15 months after initial diagnosis of LN. Biopsy of this area found fibrosis and biopsy site changes. In the imaging follow-up group one other patient developed invasive cancer at a different site in the ipsilateral breast. Thus of the imaging only group, 2/54 (4%) were subsequently diagnosed with an ipsilateral cancer, with only 1 (2%) in the index location, and 3 years later. Fourteen patients not having excision were taking anti-hormonal medication (aromatase inhibitor, tamoxifen, or raloxifene) during the follow-up period. Of note, neither of the two patients who subsequently developed carcinoma during observation were on endocrine therapy.
Discussion
Our review of a large long-term experience with management of lobular neoplasia on core needle biopsy indicates that upgrade at surgical excision is uncommon when discordant cases are excluded. Careful radiologic–pathologic correlation after the initial biopsy is critical in identifying patients in whom surgical excision is warranted. There are no imaging features that correlate with a diagnosis of LCIS/ALH, and it is usually detected incidentally on core needle biopsy for microcalcifications. An example of discordance would be the patient presenting with a new indeterminate nodule on mammogram which yields LCIS on core needle biopsy. LCIS cannot be accepted as the cause of a new mass. This was demonstrated in 4 cases in our series which were biopsies done for masses that could not be explained by the finding of LCIS only on core biopsy. On excision, in 2 cases the mass finding was revealed and explained by invasive lobular carcinomas measuring 0.6 and 1.0 cm, respectively, and in 2 other cases by DCIS involving fibroadenoma. This conclusion has been noted in multiple previous studies. As an example, a report by Menon indicated that 7 of 8 upgrades in a series of 47 patients were the result of discordance (core needle biopsy missing a mass or calcifications) [15]. Likewise, in the largest series of excisions reported that excluded cases of discordance, the upgrade rate was 3.6%, essentially the same as in the present study [29].
In our study we also elected to exclude cases of pleomorphic LCIS from determination of true upgrade rate. In this series 4 of the total 178 patients in the study had pleomorphic LCIS on core needle biopsy. This diagnosis clearly represents a distinct biologic entity different from classic type LCIS at a radiologic and pathologic level [27]. Unlike classic LCIS, pleomorphic LCIS may be associated with calcifications and may not be incidental in its clinical presentation. Characterized by large cells that are dyscohesive and pleomorphic, with eosinophilic cytoplasm and atypical nuclei, pleomorphic LCIS shares histologic characteristics with pleomorphic invasive lobular carcinoma. It is also difficult to distinguish from ductal carcinoma in situ. Features that would favor DCIS include nuclear atypia, mitosis, necrosis, cribriform architecture, E-cadherin positivity, and unifocal continuous growth pattern. Because of these diagnostic uncertainties, pleomorphic LCIS should be excised when identified by core needle biopsy. Of note, in all 4 cases in our series with features of pleomorphic LCIS, malignancy was found at excision.
If we conclude that the rate of true upgrade from classic lobular neoplasia is low, what then are the reasons for these true upgrades? This can only be determined through careful review of individual cases. The cohort described here contains too few upgrades to offer a definitive answer. The 2 upgrades to invasive lobular carcinoma were too small (< 2 mm) to be detected on imaging and were incidental findings. It is also debatable whether or not these microscopic invasive carcinomas would have made any impact on the survival of these patients if they had not undergone excision for the ALH/LCIS. In the other three cases of upgrade, a significant amount of calcifications remained on mammogram after core needle biopsy despite the sampling of large numbers of representative calcifications which were either associated with FCC and or ALH/LCIS, raising the question of sampling. The large size and heterogeneity of the target (field of calcifications) was clearly a factor concealing additional pathology and contributing to sampling error. If we establish that if the proportion of calcifications removed is estimated to be less than 50% of the total amount as a criterion for undersampling, and undersampling is reclassified as discordance, then the true pathologic upgrade rate in our study would be less than 2%. Screening for additional calcifications and or masses was also important in the cohort that did not undergo excision and detected invasive carcinoma in 2 cases.
One of the larger series of patients (n = 164) undergoing surgery after core biopsy with LN did not identify lesion size as a predictor of upgrade [28]. Alternatively, a cohort of 106 patients with LN revealed that discordance or extensive LCIS (> 4 foci) predicted all upgrades in the study [23]. This predictor was confirmed by Middleton et al. who found that when three or more terminal duct lobular units (TDLU) were involved in the initial cores, upgrade at surgical excision was more likely [16]. While none of the upgrades in our study were characterized by extensive LCIS on core biopsy, it seems likely that surgical excision of lesions considered to have extensive LN may be recommended. It should also be noted that our study highlights the need for meticulous clinical/radiologic/pathologic correlation. Our specialized center afforded access to all studies and correlations readily available to be made by surgeons, radiologists, and pathologists highly specialized in breast disease. Implementation of similar analysis may not be feasible in all practice settings.
Determination of appropriateness of imaging follow-up for patients with LN on core biopsy requires years of follow-up data in terms of subsequent screening imaging studies. While our average length of follow-up approaches 5 years, it is important to note that 9 patients in the observation cohort with recent diagnosis of LN and no imaging follow-up serves as a limitation in our ability to make any conclusions regarding subsequent cancer development. Our findings in this report support recent NCCN guidelines as well as American Society of Breast Surgeons guidelines for management of LCIS, namely that classic type found on core needle biopsy and concordant with imaging may be managed with imaging follow-up and counseling regarding reducing the risk of invasive cancer [30, 31]. With the above issues in mind, one should be able to identify appropriate patients in whom surgical excision of LN may be avoided. The majority of reports in the literature on LN are collections of patients undergoing surgical excision. Some studies however have described patients with observation and follow-up. Of these follow-up studies most did not include detailed information regarding subsequent imaging studies to determine if pathology arose in the precise location of the initial core biopsy yielding LN. Additional questions remain regarding optimal imaging protocols for patients electing to avoid surgical excision, and whether initiation of chemopreventive therapy should be factored into the decision algorithm.
References
Portschy PR, Marmor S, Nzara R, Virnig BA, Tuttle TM (2013) Trends in incidence and management of lobular carcinoma in situ: a population based analysis. Ann Surg Oncol 20(10):3240–3246
Fisher ER, Land SR, Fisher B, Mamounas E, Gilarski L, Wolmark N (2004) Pathologic findings from the National Surgical Adjuvant Breast and Bowel Project: twelve year observations concerning lobular carcinoma in situ. Cancer 100:238–244
McLaren BK, Schuyler PA, Sanders ME, Jensen RA, Simpson JF, Dupont WD, Page DL (2006) Excellent survival, cancer type, and Nottingham grade after atypical lobular hyperplasia on initial breast biopsy. Cancer 107(6):1227–1233
Page DL, Kidd TE Jr, Dupont WE, Simpson JF, Rogers LW (1991) Lobular neoplasia of the breast: higher risk for subsequent invasive cancer predicted by more extensive disease. Hum Pathol 22(12):1232–1239
Page DL, Dupont WD, Rogers LW, Rados MS (1985) Atypical hyperplastic lesions of the female breast. A long term followup study. Cancer 55(11):2698–2708
Foster MC, Helvie MA, Gregory NE, Rebner M, Nees AV, Paramagul C (2004) Lobular carcinoma in situ or atypical lobular hyperplasia at core needle biopsy: is excisional biopsy necessary? Radiology 231:813–819
Houssami N, Ciatto S, Bilous M, Vezzosi V, Bianchi S (2007) Borderline breast core needle histology: predictive values for malignancy in lesions of uncertain malignant potential (B3). Br J Cancer 96:1253–1257
Hwang H, Barke L, Mendelson EB, Susnik B (2008) Atypical lobular hyperplasia and classic lobular carcinoma in situ in core biopsy specimens: routine excision is not necessary. Mod Pathol 21:1208–1216
Ibrahim N, Bessissow A, Lalonde L, Mesurolle B, Trop I, Lisbona A, El-Khoury M (2012) Any difference between lobular carcinoma in situ and atypical lobular hyperplasia? AJR 198:288–291
Karabakhtsian RG, Johnson R, Sumkin J, Dabbs DJ (2007) The clinical significance of lobular neoplasia on breast core biopsy. Am J Surg Pathol 31:717–723
Brem RF, Lechner MC, Jackman RJ, Rapelyea JA, Evans WP, Philpotts LE, Hargreaves J, Wasden S (2008) Lobular neoplasia at percutaneous breast biopsy: variables associated with carcinoma at surgical excision. AJR 190:637–641
Lavoue V, Graesslin O, Classe JM, Fondrinier E, Angibeau H, Leveque J (2007) Management of lobular neoplasia diagnosed by core needle biopsy: study of 52 biopsies with follow up surgical excision. Breast 16:533–539
Londero V, Zuiani C, Linda A, Vianello E, Furlan A, Bazzocchi M (2008) Lobular neoplasia: core needle breast biopsy underestimation of malignancy in relation to radiologic and pathologic features. Breast 17:623–630
Mahoney MC, Robinson-Smith TM, Shaughnessy EA (2006) Lobular neoplasia at 11-guage vacuum-assisted stereotactic biopsy: correlation with surgical excisional biopsy and mammographic follow up. AJR 187:949–954
Menon S, Porter G, Evans AJ, Ellis I, Elston CW, Hodi Z, Lee A (2008) The significance of lobular neoplasia on needle core biopsy of the breast. Virchows Arch 452:473–479
Middleton LP, Sneige N, Coyne R, Shen Y, Dong W, Dempsey P, Bevers TB (2014) Most lobular carcinoma in situ and atypical lobular hyperplasia diagnosed on core needle biopsy can be managed clinically with radiologic follow up in a multidisciplinary setting. Cancer Med 3(3):492–499
Mulheron B, Gray RJ, Pockaj BA, Apsey H (2009) Is excisional biopsy indicated for patients with lobular neoplasia diagnosed on percutaneous core needle biopsy of the breast? Am J Surg 198:792–797
Murray MP, Luedtke C, Liberman L, Nehhozina T, Akram M, Brogi E (2013) Classic lobular carcinoma in situ and atypical lobular hyperplasia at percutaneous breast core biopsy: outcomes of prospective excision. Cancer 119:1073–1079
Nagi CS, O’Donnell JE, Bleiweiss IJ, Jaffer SM (2008) Lobular neoplasia on core needle biopsy does not require excision. Cancer 112:2152–2158
Niell B, Specht M, Gerade B, Rafferty E (2012) Is excisional biopsy required after a breast core biopsy yields lobular neoplasia? AJR 199:929–935
Purdie CA, McLean D, Stormonth E, Macaskill EJ, McCullough JB, Edwards SL, Brown DC, Jordan LB (2010) Management of in situ lobular neoplasia detected on needle core biopsy of breast. J Clin Pathol 63:987–993
Atkins KA, Cohen MA, Nicholson B, Rao S (2013) Atypical lobular hyperplasia and lobular carcinoma in situ at core breast biopsy: use of careful radiologic-pathologic correlation to recommend excision or observation. Radiology 269(2):340–347
Rendi MH, Dintzis SM, Lehman CD, Calhoun KE, Allison KH (2012) Lobular in-situ neoplasia on breast core needle biopsy: imaging indication and pathologic extent can identify which patients require excisional biopsy. Ann Surg Oncol 19:914–921
Shah-Kahn MG, Geiger X, Reynolds C, Jakub J, DePeri ER, Glazebrook K (2012) Long term follow up of lobular neoplasia (atypical lobular hyperplasia/lobular carcinoma in situ) diagnosed on core needle biopsy. Ann Surg Oncol 19:3131–3138
Lewis JL, Lee DY, Tartter PI (2012) The significance of lobular carcinoma in situ and atypical lobular hyperplasia of the breast. Ann Surg Oncol 19:4124–4128
Sohn VY, Arthurs ZM, Kim FS, Brown TA (2008) Lobular neoplasia: is surgical excision warranted? Am Surg 74(2):172–177
Middleton LP, Palacios DM, Bryant BR et al (2000) Pleomorphic lobular carcinoma: morphology, immunohistochemistry, and molecular analysis. Am J Surg Pathol 24:1650–1656
Brem R, Lechner M, Jackman R, Rapelyea J, Evans W et al (2008) Lobular neoplasia at percutaneous breast biopsy: variables associated with carcinoma at surgical excision. AJR 190:637–641
Susnik B, Day D, Krueger J, Abeln E, Bowman T et al (2016) Surgical outcome of lobular neoplasia diagnosed in core biopsy: prospective study of 316 cases. Clin Breast Cancer 16(6):507–513
National Comprehensive Cancer Network NCCN Guidelines for Breast Cancer, V 3.2017, (2017) p. 9. www.nccn.org/professionals/physician_gls/default.aspx
American Society of Breast Surgeons Consensus Guideline on Concordance Assessment of Image-Guided Breast Biopsies and Management of Borderline or High-Risk Lesions, p. 3
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The research reported in this manuscript complies with the current laws of the United States. The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Schmidt, H., Arditi, B., Wooster, M. et al. Observation versus excision of lobular neoplasia on core needle biopsy of the breast. Breast Cancer Res Treat 168, 649–654 (2018). https://doi.org/10.1007/s10549-017-4629-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-017-4629-2