Abstract
Purpose
Evidence suggests that premenopausal obesity decreases and postmenopausal obesity increases breast cancer risk. Because it is not well known whether this is subtype dependent, we studied the association between body mass index (BMI) and age at breast cancer diagnosis, or the probability of being diagnosed with a specific breast cancer phenotype, by menopausal status.
Methods
All patients with non-metastatic operable breast cancer from the University Hospital Leuven diagnosed between January 1, 2000 and December 31, 2013 were included (n = 7020) in this cross-sectional study. Linear models and logistic regression were used for statistical analysis. Allowing correction for age-related BMI-increase, we used the age-adjusted BMI score which equals the difference between a patient’s BMI score and the population-average BMI score corresponding to the patient’s age category.
Results
The quadratic relationship between the age-adjusted BMI and age at breast cancer diagnosis (p = 0.0207) interacted with menopausal status (p < 0.0001); increased age at breast cancer diagnosis was observed with above-average BMI scores in postmenopausal women, and with below-average BMI scores in premenopausal women. BMI was linearly related to the probabilities of Luminal B and HER2-like breast cancer phenotypes, but only in postmenopausal women. The relative changes in probabilities between both these subtypes mirrored each other.
Conclusion
BMI associates differently before and after menopause with age at breast cancer diagnosis and with the probability that breast cancer belongs to a certain phenotype. The opposite effect of increasing BMI on relative frequencies of Luminal B and HER2-like breast cancers suggests a common origin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is a multifactorial disease that globally remains the most frequently diagnosed malignancy and leading cause of cancer death in women. Obesity has been reported as a breast cancer risk factor and is becoming more prevalent worldwide [1, 2].
The relation between obesity and breast cancer risk is dual, and depends on menopausal status. An inverse association between obesity and breast cancer risk has been suggested in premenopausal women, while a reported positive association in postmenopausal women may account for 8% of postmenopausal breast cancers [3,4,5]. The explanation for this dual relationship remains unclear, although obesity-associated changes in progesterone levels may play a role [6].
If obesity exerts a key role in carcinogenesis, this dual relationship could be reflected in an earlier age at diagnosis in obese postmenopausal women and at a later age at diagnosis in obese premenopausal women. Interestingly, obesity-accelerated carcinogenesis was recently suggested in endometrial cancer by Nevadunsky and others, reporting an inverse association between age at diagnosis and BMI in postmenopausal patients [3, 7, 8]. This relationship for breast cancer is the topic of the current study.
Breast cancer heterogeneity may impact the dual relationship between obesity and breast cancer risk. A protective effect of obesity on premenopausal breast cancer risk might result from an increased likelihood of anovulatory cycles resulting in less estrogen receptor (ER)-positive breast cancers [9,10,11]. In postmenopausal women, obesity increases the risk for ER-positive breast cancer, but not in the absence of a positive progesterone receptor (PR) suggesting an important role for elevated circulating estrogens and an intact ER pathway reflected by the presence of PR [12, 13]. In a previous study, we already showed an inverse relationship between an activated ER pathway and human epidermal growth factor receptor 2 (HER2), only in postmenopausal breast cancer [14] and between obesity and HER2 status [15]. The dual association of obesity with breast cancer risk may thus be confounded by breast cancer subtype, but also by risk factors affecting breast cancer subtype, like age and parity. Indeed, a first full-term pregnancy may increase short-term breast cancer risk, but it protects in the longer term against ER-positive breast cancer [16, 17]. We therefore studied whether BMI is associated with the relative risk for a specific breast cancer subtype, and whether this relation is different by menopausal status and parity.
Methods
Patient selection
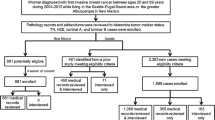
We retrieved all invasive operable breast cancer patients treated between January 1, 2000 and December 31, 2013 from our prospectively managed database (University Hospital Leuven, Belgium), excluding male (n = 62) and primary metastatic patients (n = 585) (advanced disease might interfere with BMI and increase age at diagnosis, also BMI was only available for 337/585 of these patients). A consort diagram is presented in Fig. 1 (online resource 1). BMI was assessed at surgery or at the start of neoadjuvant chemotherapy. Patients with unknown menopausal status (n = 170) were categorized as premenopausal if aged ≤ 50 years and as postmenopausal if aged > 50 years. Perimenopausal women (n = 233) were categorized as premenopausal. In case of bilateral breast cancer, both tumors were studied for analyses on tumor level. In case of multifocal breast cancer, only one focus was studied when all foci had similar phenotypes. Multifocal breast cancers were excluded when phenotypes differed between foci (n = 33).
Tumor characteristics
For a detailed description of immunohistochemical and pathological assessments of tumor size, grade, nodal status, Nottingham Prognostic Index (NPI), NPI subgroups, ER, PR, and HER2, we refer to previous study [18]. Data on tumor size, nodal status, and NPI are based only on primary operable breast cancer patients. Five breast cancer phenotypes were defined according to the 2011 St. Gallen recommendations (Table 1, online resource 2) [18]. We applied the REcommendations for tumor MARKer prognostic studies (REMARK).
Statistical analysis
Chi-square and Kruskal–Wallis tests are used to compare categorical and ordinal or continuous variables between groups, respectively. Linear models are used to study the association between BMI and age at diagnosis. Age-adjusted BMI scores are used to account for the association between age and BMI in the population [5]. The adjusted BMI score equals the difference between a patient’s BMI score and the population-average BMI score corresponding to the patient’s age category. Population-average BMI scores were obtained from publicly available data from Belgian women in 2004 (n = 7975) and calculated for five-year age categories (age 30–34, 35–39,…) in order to have sufficient observations [19]. An adjusted BMI score of 5 thus indicates that a patient’s BMI is 5 points (kg/m2) above the population-average in her age category. Since women with higher BMI may have large tumors, analyses that study the relationship between adjusted BMI scores and age at diagnosis were corrected for tumor size.
Logistic regression models were used to study the association between BMI and binary outcomes (i.e., phenotypes). BMI was primarily studied as a continuous variable rather than as a categorical variable since biology does not take into account human arbitrary definitions. Categorical strata are, however, presented in patient demographic tables and were defined as follows: underweight (< 18), normal weight (18–24.9), overweight (25–29.9), obese (≥ 30) (kg/m2). Analyses were performed with correction for age at diagnosis since the relative frequencies of different breast cancer phenotypes vary by age.
All analyses were performed using SAS software, version 9.3 of the SAS System for Windows. Copyright © 2002 SAS Institute Inc. SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc., Cary, NC, U.S.A..
Results
We included 7020 patients with known age at diagnosis and BMI; 6304 or 89.8% were primary operable, and 716 or 10.2% received neoadjuvant therapy. Descriptive statistics for BMI, menopausal status, grade, receptor status, tumor size, nodal status, histology, and parity are presented in Table 2 (online resource 3). Table 3 (online resource 4) shows age at diagnosis by BMI categories.
Relation between BMI, adjusted BMI score, and age at diagnosis
We observed a quadratic relationship between BMI and age at breast cancer diagnosis in the overall study population (p < 0.0001) (Fig. 1a). This quadratic relationship remained significant (p = 0.0207) (Fig. 1b) using age-adjusted BMI scores, accounting for the association between age and BMI in the general population, and also after correction for tumor size (p = 0.0143). The quadratic relationship between age-adjusted BMI score and age at diagnosis interacted significantly with the menopausal status (p < 0.0001) (Fig. 1c). In brief and corrected for same-age in the general population, premenopausal patients with lower BMI had a higher age at diagnosis as compared to patients with a higher BMI and postmenopausal women with lower (respectively higher) BMI were diagnosed at an earlier (respectively elder) age. In addition, Fig. 1d shows that ER-positive subtypes were diagnosed at a later age compared to ER-negative subtypes, independently of BMI in premenopausal women. In postmenopausal women, ER status interacts significantly with age-adjusted BMI, suggesting a stronger positive association between age at diagnosis and age-adjusted BMI in ER-positive than in ER-negative breast cancers (p = 0.0308) (Fig. 1d). No other interactions were observed between menopausal status and histology or breast cancer subtypes (data not shown). The estimated changes in age at diagnosis per 5-unit change in BMI compared with the mean are presented in Table 1 for the overall population and for pre- and postmenopausal women separately. For instance, postmenopausal patients with a BMI score that is + 5 kg/m2 compared to the population mean BMI in their age category, were on average 1.09 years (95% CI 0.83–1.35) older at diagnosis; and, premenopausal patients with a BMI score that is − 5 kg/m2 compared to BMI of the general same-age population were experiencing diagnosis on average 0.82 years later (95% CI 0.20–1.44). Results remained identical when corrected for tumor size (data not shown).
Quadratic relationship between BMI (a) or adjusted BMI score (b) and age at breast cancer diagnosis. A significant interaction was found with menopausal status (c) and ER status (d) but not with HER2 status (e) or breast cancer phenotype (f) or histology (data not shown). (TNBC triple-negative breast cancer)
Relation between BMI, parity, and probability of being diagnosed with a certain breast cancer phenotype
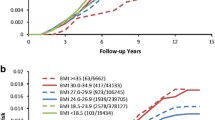
We further explored the impact of BMI on the probability of being diagnosed with certain breast cancer subtypes. We observed a linear relationship between BMI and the probability of being diagnosed with Luminal B breast cancer (p = 0.0375) (Table 2, Fig. 2a). No such relationship could be demonstrated for other breast cancer subtypes, unless menopausal status was taken into account. Indeed, menopausal status significantly interacted with BMI in explaining the probability of being diagnosed with Luminal B and HER2-like breast cancer. BMI was associated with the probabilities of these subtypes only in postmenopausal women, and the relative changes in probabilities between both subtypes are mirroring each other (Table 2, Fig. 2b). An interaction effect between BMI and parity could not be demonstrated, except for a trend in Luminal HER2-like breast cancer (p = 0.0627) (Table 2). Although for Luminal B the interaction between BMI and menopause looks stronger in nulliparous than in multiparous women, the three-way interaction tests between BMI, parity, and menopausal status remained nonsignificant (Table 2), perhaps due to low numbers in the nulliparous group.
Probability of being diagnosed with a breast cancer phenotype by BMI (a). Analyses were repeated for Luminal B and HER2-like subtypes, patients were stratified by menopausal status (b). Breast cancer phenotypes are studied as binary variables (e.g., Luminal A versus non-Luminal A). (TNBC triple-negative breast cancer)
Discussion
To our knowledge, this is the first study where a potential relation between BMI and age at breast cancer diagnosis has been explored in a case-only cohort. We found a quadratic relation between BMI and age at breast cancer diagnosis. However, since elder women are more likely obese [5], a correction was introduced by means of country-specific age-adjusted BMI scores, and since obese women are more likely to have larger tumors at the time of diagnosis, a correction for tumor size was applied. After correction for these potential confounders, the quadratic relationship between BMI and age at breast cancer diagnosis remained identical.
In addition, a significant interaction effect with menopausal status was found, as was hypothesized based on the dual relationship between obesity and breast cancer risk from the literature. Lower than average body mass was associated with increased age at diagnosis in premenopausal women, but with younger age at diagnosis in postmenopausal women. On the contrary, higher than average body mass was not associated with age at diagnosis in premenopausal women, but was associated with older age at diagnosis in postmenopausal women. The direction of this effect in postmenopausal women was opposite to the one anticipated from the Nevadunsky study in endometrial cancer. They indeed found that a higher BMI was associated with younger age at diagnosis in postmenopausal endometrial cancer, suggestive for an accelerated carcinogenesis [7]. A first potential explanation for our results could be a delayed diagnosis due to a more difficult clinical/radiological assessment or due to the fact that obese patients are less likely to undergo mammographic screening [20]. We attempted to control for this through correction for tumor size, since delayed diagnosis may result in larger tumors, although this might be insufficient. Correction for detection mode could be of value, but was not possible since organized screening mammography is only available above age 50 years in Belgium.
An alternative explanation could be the hypothesis that obesity induces different (slower growing) breast cancer subtypes than those arising in normal weight postmenopausal women. In order to elucidate this hypothesis, we examined the impact of BMI on the probability of being diagnosed with a certain breast cancer phenotype, correcting for age at diagnosis, since the probability of the different breast cancer phenotypes varies by age. Although our case-only cohort study design does not allow calculating absolute risks, it allows studying heterogeneity of effect of a given risk factor across different breast cancer phenotypes [21]. We found that obesity is associated with the probability of being diagnosed with Luminal B and HER2-like breast cancer. These results were only significant in postmenopausal women. While a higher BMI was associated with an increased probability of being diagnosed with Luminal B breast cancer, an inverse and mirroring relationship was seen for HER2-like breast cancer. This has not been described in previous studies [22]. Adding to the strength of this observation, we have previously reported both inverse associations between BMI and HER2 receptor status and between ER/PR and HER2 status in postmenopausal women [14, 15]. Taken together, current and previous studies could represent clinical evidence of a common progenitor cancer cell for Luminal B and HER2-like breast cancers. Luminal progenitors have been proposed to be the cell type most commonly associated with the initiation of breast cancer, even in BRCA1-related basal-like breast cancers [23]. We hypothesize that a luminal progenitor may not be able to become clinically apparent in an otherwise low (postmenopausal) estrogen environment, except in the case of an obesity-stimulated ER pathway. Bidirectional crosstalk between ER and HER2 pathways has been well documented, and an obesity-activated ER pathway will therefore suppress HER2, resulting in the Luminal B phenotype [24]. Vice versa, the luminal progenitor in normal-weight postmenopausal women will need to activate another growth pathway, for example, the HER2 pathway, before it can become clinically apparent. Since the ER pathway is not stimulated, this results in a HER2-like phenotype. This obesity-induced heterogeneity in breast cancer phenotype might also explain the obesity-induced increase in age at breast cancer diagnosis as hypothesized earlier in this article.
In the view of these results, we believe that obesity carries a mitogenic rather than a mutagenic or carcinogenic function, similar to the association between hormone substitution therapy (HST) and breast cancer risk [25]. This hypothesis may be supported by (a) the absence of an obesity-associated breast cancer risk in HST users [26] (b) the fact that an obesity-associated breast cancer risk exists in larger tumors only [27], (c) the proposed mitogenic rather than mutagenic ability of insulin which may be a mediator of obesity [28] and (d) the lack of a prognostic effect of obesity in postmenopausal women with ER-positive breast cancer [29].
To our knowledge, our report represents the largest case-only series examining the relationship between obesity and breast cancer phenotypes. Case–control studies should now further investigate this relationship, since other currently available data are conflicting and/or originate from small series [26, 30,31,32,33]. Potential confounders such as smoking, dietary factors, HST and detailed reproductive variables were not available in our study and should be incorporated in future studies, if possible. For example, a low BMI may act as a proxy for heavier smoking [3], and nulliparity and obesity may have synergistic effects on breast cancer risk [17]. Our study did include data on parity. Although the interaction between BMI and menopause appears visually stronger for Luminal B breast cancer in nulliparous, this was not statistically confirmed. This could be explained by the fact that these associations may be significant in elderly women only [17].
References
DeSantis CE, Lin CC, Mariotto AB et al (2014) Cancer treatment and survivorship statistics, 2014. CA Cancer J Clin 64:252–271
WHO (2011) World Health Statistics 2011. World Health Organization, Geneva
Bhaskaran K, Douglas I, Forbes H et al (2014) Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5 24 million UK adults. Lancet 384(9945):755–765
Yang XR, Chang-Claude J, Goode EL et al (2011) Associations of breast cancer risk factors with tumor subtypes: a pooled analysis from the Breast Cancer Association Consortium studies. J Natl Cancer Inst 103(3):250–263
James WP, Jackson-Leach R, Ni Mhurchu C et al. WHO report Comparative Quantification of Health Risks, Chapter 8 Overweight and obesity (high body mass index), 497–596
Dowsett M, Folkerd E (2015) Reduced progesterone levels explain the reduced risk of breast cancer in obese premenopausal women: a new hypothesis. Breast Cancer Res Treat 149(1):1–4
Nevadunsky NS, Van Arsdale A, Strickler HD et al (2014) Obesity and age at diagnosis of endometrial cancer. Obstet Gynecol 124(2 Pt 1):300–306
Kounelis S, Kapranos N, Kouri E et al. Immunohistochemical profile of endometrial adenocarcinoma: a study of 61 cases and review of the literature. Mod Pathol 13(4): 379–88 (2000); Int J Cancer 135(11): 2678–86 (2014)
Peacock SL, White E, Daling JR et al (1999) Relation between obesity and breast cancer in young women. Am J Epidemiol 149(4):339–346
Tehard B, Clavel-Chapelon F (2006) Several anthropometric measurements and breast cancer risk: results of the E3 N cohort study. Int J Obes 30(1):156–163
Millikan RC, Newman B, Tse CK et al (2008) Epidemiology of basal-like breast cancer. Breast Cancer Res Treat 109(1):123–139
Suzuki R, Orsini N, Saji S et al (2009) Body weight and incidence of breast cancer defined by estrogen and progesterone receptor status—a meta-analysis. Int J Cancer 124(3):698–712
Horwitz KB, Koseki Y, McGuire WL (1978) Estrogen control of progesterone receptor in human breast cancer: role of estradiol and antiestrogen. Endocrinology 103(5):1742–1751
Huang HJ, Neven P, Drijkoningen M et al (2005) Association between HER-2/neu and the progesterone receptor in oestrogen-dependent breast cancer is age-related. Breast Cancer Res Treat 91(1):81–87
Van Mieghem T, Leunen K, Pochet N et al (2007) Body mass index and HER-2 overexpression in breast cancer patients over 50 years of age. Breast Cancer Res Treat 106(1):127–133
Pathak DR (2002) Dual effect of first full term pregnancy on breast cancer risk: empirical evidence and postulated underlying biology. Cancer Causes Control 13:295–298
Opdahl S, Alsaker MDK, Janszky I, Romundstad PR, Vatten LJ (2011) Joint effects of nulliparity and other breast cancer risk factors. Br J Cancer 105:731–736
Brouckaert O, Laenen A, Vanderhaegen J et al (2012) Applying the 2011 St Gallen panel of prognostic markers on a large single hospital cohort of consecutively treated primary operable breast cancers. Ann Oncol 23(10):2578–2584
Drieskens S, Charafeddine R, Demarest S, Gisle L, Tafforeau J, Van der Heyden J Health Interview Survey, Belgium, 1997–2001–2004–2008–2013: Health Interview Survey Interactive Analysis. Brussels: WIV-ISP. https://hisia.wiv-isp.be/
Maruthur NM, Bolen S, Brancati FL (2009) Clark JM Obesity and mammography: a systematic review and meta-analysis. J Gen Intern Med 24(5):665–677. https://doi.org/10.1007/s11606-009-0939-3
Martinez ME, Cruz GI, Brewster AM, Bondy ML, Thompson PA (2010) What can we learn about disease etiology from case-case analyses? Lessons from breast cancer. Cancer Epidemiol Biomark Prev 19:2710–2714
Biglia N, Peano E, Sgandurra P et al (2013) Body mass index (BMI) and breast cancer: impact on tumor histopathologic features, cancer subtypes and recurrence rate in pre and postmenopausal women. Gynecol Endocrinol 29(3):263–267
Molyneux G, Geyer FC, Magnay FA et al (2010) BRCA1 basal-like breast cancers originate from luminal epithelial progenitors and not from basal stem cells. Cell Stem Cell 7(3):403–417
Prat Aleix, Baselga José (2008) The role of hormonal therapy in the management of hormonal-receptor-positive breast cancer with co-expression of HER2. Nat Clin Pract Oncol 5(9):531–542
Countercurrents Series, Narod SA (2012) Disappearing breast cancers. Curr Oncol 19(2):59–60
Phipps AI, Malone KE, Porter PL, Daling JR, Li CI (2008) Body size and risk of luminal, HER2-overexpressing, and triple-negative breast cancer in postmenopausal women. Cancer Epidemiol Biomarkers Prev 17(8):2078–2086
Garcia-Closas M, Brinton LA, Lissowska J et al (2006) Established breast cancer risk factors by clinically important tumour characteristics. Br J Cancer 95(1):123–129
Vineis P, Schatzkin A, Potter JD (2010) Models of carcinogenesis: an overview. Carcinogenesis 31:1703–1709
Pan Hongchao, Gray Richard G, on behalf of the Early Breast Cancer Trialists’ Collaborative Group (2014) Effect of obesity in premenopausal ER + early breast cancer: EBCTCG data on 80,000 patients in 70 trials. J Clin Oncol 32:503
Petekkaya I, Sahin U, Gezgen G et al (2013) Association of breast cancer subtypes and body mass index. Tumori 99(2):129–133
Miyagawa Y, Miyake T, Yanai A et al. (2013) Association of body mass index with risk of luminal A but not luminal B estrogen receptor-positive and HER2-negative breast cancer for postmenopausal Japanese women. Breast Cancer
Song Q, Huang R, Li J, Fan J et al (2013) The diverse distribution of risk factors between breast cancer subtypes of ER, PR and HER2: a 10-year retrospective multi-center study in China. PLoS ONE 8(8):e72175
Yanai A, Miyagawa Y, Murase K et al (2014) Influence of body mass index on clinicopathological factors including estrogen receptor, progesterone receptor, and Ki67 expression levels in breast cancers. Int J Clin Oncol 19(3):467–472
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
None declared (for all authors).
Ethical approval
We declare that the experiments comply with the current laws in Belgium.
Informed consent
Informed consent was obtained for patients included in this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Brouckaert, O., Van Asten, K., Laenen, A. et al. Body mass index, age at breast cancer diagnosis, and breast cancer subtype: a cross-sectional study. Breast Cancer Res Treat 168, 189–196 (2018). https://doi.org/10.1007/s10549-017-4579-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-017-4579-8