Abstract
Purpose
To assess tumor subtype distribution and the relative contribution of clinical and sociodemographic factors on breast cancer survival between Hispanic and non-Hispanic whites (NHWs).
Methods
We analyzed data from the California Cancer Registry, which included 29,626 Hispanic and 99,862 NHW female invasive breast cancer cases diagnosed from 2004 to 2014. Logistic regression was used to assess ethnic differences in tumor subtype, and Cox proportional hazard modeling to assess differences in breast cancer survival.
Results
Hispanics compared to NHWs had higher odds of having triple-negative (OR = 1.29; 95% CI 1.23–1.35) and HER2-overexpressing tumors (OR = 1.19; 95% CI 1.14–1.25 [HR−] and OR = 1.39; 95% CI 1.31–1.48 [HR+]). In adjusted models, Hispanic women had a higher risk of breast cancer mortality than NHW women (mortality rate ratio [MRR] = 1.24; 95% CI 1.19–1.28). Clinical factors accounted for most of the mortality difference (MRR = 1.05; 95% CI 1.01–1.09); however, neighborhood socioeconomic status (SES) and health insurance together accounted for all of the mortality difference (MRR = 1.01; 95% CI 0.97–1.05).
Conclusions
Addressing SES disparities, including increasing access to health care, may be critical to overcoming poorer breast cancer outcomes in Hispanics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Constituting 17% of the United States (U.S.) population, Hispanics are a large ethnic group that is estimated to double in size by 2050 [1]. Invasive breast cancer is the most commonly diagnosed malignancy and the leading cause of cancer death among Hispanic women in the U.S [2]. Relative to NHW women, Hispanics are more likely to be diagnosed with later stage breast cancers and larger tumors [2,3,4], factors that contribute to lower survival [5, 6]. There is also evidence that Hispanic women have higher proportions of the more aggressive tumor subtypes, including triple-negative and HER2-overexpressing tumors [3, 7,8,9,10]. Further, Hispanic patients are less likely to receive guideline concordant cancer treatment and experience poorer quality of life after diagnosis as compared to NHW women [7, 11]. Hispanics in general are of lower socioeconomic status (SES) and are less likely to have health insurance [12], factors that independently impact cancer survival. However, the contribution of clinical, molecular, and SES factors, alone or in combination, to differences in breast cancer mortality between Hispanics and NHWs is not completely understood, due to a lack of comprehensive studies in this area.
We used these data from the population-based California Cancer Registry (CCR) to assess differences in tumor subtype distribution between Hispanic and NHW breast cancer patients and to evaluate the relative contributions of tumor subtype, clinical factors, treatment, neighborhood SES (nSES), and health insurance on breast cancer survival differences in the two groups.
Methods
Study population
Breast cancer patients were identified through the CCR, part of the National Cancer Institute’s (NCI) SEER program, which requires the highest standards of data quality. Data on demographic factors, diagnosis and treatment information, and tumor characteristics are routinely ascertained. Vital status as of December 31, 2014 and the underlying cause of death are updated through linkages with administrative databases such as death certificates, hospital discharge data, Medicare, Department of Motor Vehicles, and Social Security Administration.
Patients included in this study were NHW and Hispanic female California residents, age 20 years and older, diagnosed from a non-autopsy/death certificate source with a first primary invasive breast cancer between 2004 and 2014. International Classification of Disease for Oncology, 3rd Edition (ICD-O-3) site codes C50.0–50.9, with the following ICD-O-3 coded histology subtypes of breast carcinoma or adenocarcinoma: 8000, 8001, 8010, 8020, 8022, 8050, 8140, 8201, 8211, 8230, 8255, 8260, 8401, 8453, 8480, 8481, 8500–8530, and 8575 was used to identify incident breast cancer cases (n = 159,883). Stage at diagnosis was defined based on American Joint Committee on Cancer (AJCC) collaborative staging system and stratified into three groups: stage I, stage II, and stage III/IV (no substantial difference in outcome was shown between stages III and IV). Cases with an unknown tumor subtype (n = 20,405), treatment (chemotherapy n = 2180, radiotherapy n = 26, surgery n = 91), marital status (n = 4745), or insurance status (n = 2948) were excluded from all analyses, resulting in a study sample size of 129,488.
Registry data on race/ethnicity were enhanced with the North American Association for Central Cancer Registries Hispanic/Latino identification algorithm to improve identification of Hispanics based on Hispanic surnames and maiden names and birthplace [13]. Race/ethnicity was categorized into two mutually exclusive groups: non-Hispanic white and Hispanic (regardless of race). Data on age, year, marital status, and stage at diagnosis; histology; primary and secondary sources of payment to the reporting hospital (health insurance status); estrogen receptor (ER) status; progesterone receptor (PR) status; HER2 status; and first course of treatment (surgery, radiation, and chemotherapy) were also obtained from medical records. Registry birthplace information is missing for 43% of Hispanic patients in this analysis. Since birthplace is differentially missing between US- and foreign-born Hispanics, and by vital status [14], nativity was imputed for Hispanic patients with unknown birthplace using patients’ social security numbers (SSN). This validated imputation method assigns a foreign birthplace to Hispanic patients who received their SSNs after the age of 21 [15]. We included individual-level data on insurance status at diagnosis coded as private/military, Medicare only or Medicare plus private, public only, or uninsured. Addresses at diagnosis is used to assess residential nSES, which is based on census-block group level data on education, occupation, employment, household income, poverty, rent, and house values from the census 2000 summary file long form data (for cases diagnosed 2004–2005) and the 2007–2011 American Community Survey (ACS, which replaced the census long form, for cases diagnosed 2006 onward) [16, 17].
Our analyses involved categorizing tumors into the following tumor subtypes: HR+ (ER+ and/or PR+)/HER2−; HR+/HER2+; HR−/HER2+; and HR−/HER2− (triple-negative breast cancer, TNBC). Cases missing either HR status (n = 7338, 4.6%), HER2 status (n = 19,582, 12.2%), or both (6515, 4.1%) were excluded (total = 20,405, 12.8%). The study was approved by the institutional review boards at each institution; informed consent was waived as we analyzed de-identified data.
Statistical analysis
Logistic regression was used to estimate odds ratios (OR) and corresponding 95% confidence intervals (CI) for differences in the distributions of breast cancer molecular subtypes between NHWs and Hispanics. In these analyses, HR+/HER2− cancer cases were the referent tumor subtype and NHW were the referent race/ethnicity group. Analyses were stratified by age at diagnosis (<50 vs. 50+ years), stage (I, II, and III/IV), and nativity (Hispanic U.S.-born, Hispanic foreign-born). Two different models were evaluated, one that adjusted for age (continuous) and year of diagnosis (continuous), and another that adjusted for these two factors plus nSES. Cox proportional hazard regression was used to estimate breast cancer mortality rate ratios (MRRs) and corresponding 95% CI for differences in breast cancer mortality between NHW and Hispanic patients. Follow-up time for breast cancer mortality was computed as the number of days between the date of diagnosis and date of death from breast cancer through the end of the follow-up date (December 31, 2013), with censoring at the date of death for those who died from an underlying cause other than breast cancer. Analyses were stratified by age at diagnosis (<50 vs. 50+ years), stage (I/II vs. III/IV), and nativity. We constructed several models to assess the contribution of each set of the following variables to ethnic differences in breast cancer mortality: tumor subtype; tumor characteristics, clinical factors, and treatment; and nSES and health insurance. In model 1 (base model), we adjusted for age at diagnosis, calendar year, and marital status. We then assessed individual contribution of different set of variables beyond the base model as follows: model 2 includes model 1 plus tumor subtype. Model 3 included model 1 plus clinical variables (stage, grade, histology, tumor size, and lymph node status); these results showed that neither tumor size nor lymph node status contributed to the mortality differences beyond the other clinical variables, which resulted in dropping these variables from the model. Model 4 includes model 1 plus nSES and insurance status. We also considered inclusion of treatment variables but these had no effect on the MRRs. This resulted in a final model that included age at diagnosis, calendar year, marital status, tumor subtype, stage, grade, histology, nSES, and health insurance. All statistical analyses were performed using SAS version 9.3 (SAS Institute, Cary, NC).
Results
Compared to NHW breast cancer patients, Hispanics were more likely to be under age 50 at diagnosis (36 vs. 19.2%), to live in neighborhoods in the lower two nSES quintiles (52.7 vs. 21.1%), and to have Medicaid insurance (30.8 vs. 17.0%); they were also less likely to be diagnosed with stage I disease (39.8 vs. 51.1%), more likely to have positive lymph nodes (41.1 vs. 31.5%), and more likely to have stage III/IV disease (39.2 vs. 28.4%) (Table 1). Hispanic women were more likely to undergo mastectomy with or without radiation and were more frequently treated with chemotherapy than NHWs (53.2 vs. 38.5%).
After adjustment for age and nSES, Hispanic women had significantly higher odds of being diagnosed with tumors that were HR+/HER2+ (OR = 1.19; 95% CI 1.14–1.25), HR−/HER2+ (OR = 1.39; 95% CI 1.31–1.48), or triple negative (OR = 1.29; 95% CI 1.23–1.35), than HR+/HER2− as compared to NHWs (Table 2). Significant interactions according to age at diagnosis (P = 0.007) and stage (P < 0.0001) were observed but the differences in the ORs across the categories were modest. US-born Hispanic compared to NHW patients had significantly higher odds of being diagnosed with HR+/HER2− (OR = 1.10; 95% CI 1.04–1.16), HR−/HER2+ (OR = 1.24; 95% CI 1.15–1.34), and triple negative (OR = 1.31; 95% CI 1.24–1.38) than HR+/HER2− tumors. Similar associations were shown comparing foreign-born to NHW women, although the highest OR was observed comparing foreign-born patients with NHWs (OR = 1.54; 95% CI 1.43−1.66).
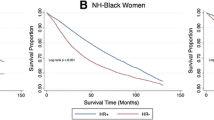
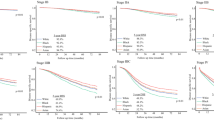
In the basic model that adjusted for age, calendar year, and marital status, breast cancer survival was significantly poorer for Hispanic patients compared to NHWs (MRR = 1.24; 95% CI 1.19−1.28); adjustment for tumor subtype did not materially reduce the difference (MRR = 1.18; 95% CI 1.14–1.22) (Table 3). The breast cancer mortality difference between Hispanic and NHW patients continued to be significant but was greatly attenuated when tumor characteristics (stage, grade, and histology) were included in the model (MRR = 1.05; 95% CI 1.01–1.09). However, when nSES and insurance were added to the basic model (without other covariates), no difference in mortality was observed (MRR = 1.01; 95% CI 0.97–1.05). The final model that included all variables shows a slight but significant lower mortality for Hispanic than NHW patients (MRR = 0.90; 95% CI 0.87–0.94). Additional inclusion of other characteristics, including tumor size, lymph node involvement, or treatment did not change the MRRs. Younger women had a higher risk of dying than older women (P-interaction < 0.001). In the basic model, stratification by age shows higher mortality differences for Hispanics vs. NHWs among younger (MRR = 1.42; 95% CI 1.32–1.53) than older women (MRR = 1.13; 95% CI 1.08–1.18). No substantial effect in the tumor subtype-stratified MRRs was seen. Inclusion of tumor characteristics in the age-stratified analysis did not entirely explain the differences, but nSES and insurance did. A significant interaction was shown according to stage (P < 0.001), but the difference in the MRRs was modest. Results stratified by nativity show that Hispanic U.S.-born (MRR = 1.22; 95% CI 1.16–1.28) and foreign-born (MRR = 1.29; 95% CI 1.23–1.35) women have significantly higher mortality than NHW patients in the basic model and the MRRs were attenuated with subsequent covariate adjustment.
In this cohort, as with other analyses involving cancer registry data [18, 19], Hispanic patients were more likely than NHW patients to be lost to follow-up (5.9% among Hispanics and 1.2% in NHWs), defined here as date of last follow-up greater than 2 years before the study follow-up date. We conducted sensitivity analysis to assess the potential impact of differential follow-up on the observed MRRs comparing Hispanic to NHW patients, by assuming that (1) all Hispanics lost to follow-up (considered here as date of last follow-up more than 2 years prior to study cut-off date) were deceased, or (2) all Hispanics with distant stage disease lost to follow-up were deceased. These results suggest that if there were differential loss to follow-up, such that we are not capturing some deaths among Hispanics, the actual MRRs comparing Hispanics to NHWs would be higher than those reported here. For example, if we assumed that all Hispanics lost to follow-up were deceased, the multivariable-adjusted MRR for Hispanic vs. NHW is 1.15 (95% CI 1.11–1.19), which is higher than that observed with no assumptions.
Discussion
Results of this large population-based study show that, in California, breast cancers among Hispanic women are more likely than those among NHWs to be triple negative or overexpress HER2, relative to HR+/HER2−. This pattern was observed regardless of age or stage at diagnosis, and independent of nSES. Associations were slightly higher among foreign-born than US-born Hispanic women, especially for patients with HER2+/HR− tumors. We also show that Hispanic patients are more likely to die of breast cancer compared to NHWs, with the difference largely attributable to the combined effect of nSES and health insurance, suggesting that these socioeconomic factors likely serve as fundamental causes of the survival disparity.
Our results are consistent with published reports showing that breast tumors in Hispanic women are more likely to be triple negative and HER2+ than HR+/HER2− as compared to tumors in NHW patients [3, 9, 10, 20]. Our findings extend prior work to show that these ethnic differences hold true across categories of age at diagnosis and stage; even among younger women and those with early-stage tumors, these tumor subtype distribution differences are evident. A novel finding relates to the differences in tumor subtype distributions according to nativity in Hispanic patients, where the data suggest that the odds of being diagnosed with the more aggressive tumor subtypes was higher in foreign-born women, especially for HR−/HER2+ tumors, which is consistent with an earlier report by Banegas et al. [18]. Reasons for higher prevalence of TNBC in Hispanics vs. NHWs could be due to differences in reproductive profile, such as higher parity in Hispanic vs. NHW women, which we have reported previously [21]. However, differences in HER2 overexpressing tumors are less clear given that the etiology of this rare tumor subtype is largely unknown [22].
Reports on breast cancer survival between Hispanics and NHWs are inconsistent. Earlier population-based studies showed that Hispanic breast cancer patients had a significantly higher risk of breast cancer mortality compared to NHWs [5, 6]. Using SEER data, our group previously reported that risks of mortality were elevated relative to NHW women across each of the four Hispanic subgroups for which country of origin was available, but the risk among Puerto Rican women was significant after multivariate adjustment [9], which is consistent with additional reports published by our group [10, 18]. Lastly, a report from the National Comprehensive Cancer Network (NCCN) breast cancer outcomes database [23], a non-population-based study, found that Hispanic compared to NHW patients did not have a higher risk of dying of breast cancer after age adjustment, contrary to our results; the multivariable-adjusted MRR was 0.74 (95% CI 0.58–0.95).
Lacking in the literature, however, is an understanding of the contributing factors accounting for the survival differences reported between Hispanic and NHW breast cancer patients. Differences in modeling approaches and inclusion of different and a more comprehensive set of covariates in estimating risk of mortality could explain the variation in published reports from ours. Results of our sequential modeling indicate that, although Hispanics are more likely to be diagnosed with aggressive tumor subtypes, this does not explain their higher mortality. Among younger and US-born women, differences in tumor characteristics (stage, grade, and histology) do not fully account for the survival differences between Hispanics and NHWs. However, when nSES and health insurance were included in the model (without clinical or tumor characteristics), the survival difference between Hispanics and NHWs disappeared. These findings are noteworthy given that Hispanics, compared to NHWs, have lower educational attainment [24] and a lower median income, are more likely to live in poverty [25], and are less likely to have private insurance [12]. Consistent with other national reports [26], these data suggest that addressing SES factors, including health insurance and other cost-related barriers to cancer care, are important components for reducing or eliminating disparities in cancer outcome in Hispanic breast cancer patients. This is an important consideration given that the percentage of uninsured individuals in the U.S. has declined from 16.0% in 2010 to 9.1% in 2015 as a result of the Affordable Care Act (ACA) [27]. In California, the percentage of uninsured individuals has dropped by almost half since the implementation of the ACA (from 16% in 2013 to 9% in 2016) [28], although Hispanics continue to lag behind. As President Obama pointed out in a recent publication [27], despite the ACA’s progress, too many Americans continue to have challenges accessing health care and additional work is needed to reform rather than repeal the current health care system. Reversals of the gains made in reducing the population of uninsured Americans could have substantial deleterious effects on breast cancer survival.
Data on the association between nativity and breast tumor subtype or survival in Hispanics are sparse. Keegan et al. reported that while foreign-born Hispanic women were more likely than US-born to be diagnosed with later stage disease, they had lower stage-adjusted mortality, even after accounting for differential loss to follow-up [29]. Using a CCR dataset with shorter follow-up than ours, Banegas et al. reported that both U.S.- and foreign-born Hispanic women with TNBC had a higher risk of dying than those with HR+/HER2− breast cancer [18]. Our findings including a more contemporary sample of 29,626 Hispanic breast cancer patients in the CCR show a higher risk of breast cancer deaths for both US-born and foreign-born Hispanics than NHWs; however, these differences disappeared after accounting for clinical, treatment, nSES, and insurance factors. Of note, the survival difference between foreign-born Hispanics relative to NHWs disappeared after adjusting for clinical or socioeconomic factors, whereas the difference between US-born Hispanics and NHWs disappeared in the full multivariate model.
Although our study has many strengths, including the large population-based resource, there are limitations that must be considered. Cancer registry-recorded race, ethnicity, and birthplace may be subject to misclassification; although, because this information is usually based on self-report [30], it is generally accurate for most racial/ethnic groups [15, 31,32,33]. Because registry birthplace data are incomplete in a biased manner, we used a validated approach to impute nativity. We lacked information on potentially important confounders such as comorbidities, specific treatment modalities, and adherence to treatment. Tumor subtype information was missing for approximately 15% of participants, potentially introducing bias, although the direction of this is uncertain. As has been previously reported [19], survival data derived from population-based cancer registries are based on censoring that is non-random across racial/ethnic groups. For Hispanics, this bias results in overt inflation of survival estimates, which results in erroneously projecting a survival advantage for Hispanics when compared to NHWs. Problematic death linkages for Hispanics also contribute to missing deaths, which further overestimates survival. Thus, our observed MRRs are likely under-estimated. We were not able to examine specific Hispanic ethnicity because the Hispanic origin variable is not specified for 58.9% of patients. It is likely that the majority of Hispanic patients in our sample are of Mexican descent, given that 83% of the California Hispanic population is of Mexican origin [34]. Lastly, because this study was based on data from California, results are not generalizable to Hispanic women in other regions of the U.S. and are probably mostly relevant to those of Mexican descent, the largest Hispanic group in the U.S.
Conclusion
A large, aging, and growing proportion of Hispanics will continue to increase the breast cancer burden in the U.S. This ethnic group has a disproportionate burden of uninsured and low SES individuals, the two factors that explain the survival differences between NHWs and Hispanics in our study. Our results support the importance of sustained efforts to increase access to medical care, especially screening and early detection, thereby addressing inequities related to SES factors, including decreasing the proportion of uninsured Hispanic individuals in the U.S.
Change history
04 September 2017
An erratum to this article has been published.
References
Colby SL, Ortman JM (2014) Projections of the size and composition of the U.S. population: 2014 to 2060. In: Current population reports. U.S. Census Bureau, Washington DC
Siegel RL, Fedewa SA, Miller KD, Goding-Sauer A, Pinheiro PS, Martinez-Tyson D, Jemal A (2015) Cancer statistics for Hispanics/Latinos, 2015. CA Cancer J Clin 65(6):457–480
Martinez ME, Nielson CM, Nagle R, Lopez AM, Kim C, Thompson P (2007) Breast cancer among Hispanic and non-Hispanic white women in Arizona. J Health Care Poor Underserved 18(4 Suppl):130–145
Iqbal J, Ginsburg O, Rochon PA, Sun P, Narod SA (2015) Differences in breast cancer stage at diagnosis and cancer-specific survival by race and ethnicity in the United States. JAMA 313(2):165–173
Clegg LX, Li FP, Hankey BF, Chu K, Edwards BK (2002) Cancer survival among US whites and minorities: a SEER (Surveillance, Epidemiology, and End Results) program population-based study. Arch Intern Med 162(17):1985–1993
Elledge RM, Clark GM, Chamness GC, Osborne CK (1994) Tumor biologic factors and breast cancer prognosis among white, Hispanic, and black women in the United States. J Natl Cancer Inst 86(9):705–712
Chen L, Li CI (2015) Racial disparities in breast cancer diagnosis and treatment by hormone receptor and HER2 status. Cancer Epidemiol Biomark Prev 24(11):1666–1672
Howlader N, Altekruse SF, Li CI, Chen VW, Clarke CA, Ries LA, Cronin KA (2014) US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. J Natl Cancer Inst 106(5):1–8
Ooi SL, Martinez ME, Li CI (2011) Disparities in breast cancer characteristics and outcomes by race/ethnicity. Breast Cancer Res Treat 127(3):729–738
Banegas MP, Li CI (2012) Breast cancer characteristics and outcomes among Hispanic Black and Hispanic White women. Breast Cancer Res Treat 134(3):1297–1304
Freedman RA, Virgo KS, He Y, Pavluck AL, Winer EP, Ward EM, Keating NL (2011) The association of race/ethnicity, insurance status, and socioeconomic factors with breast cancer care. Cancer 117(1):180–189
Cohen RA, Martinez ME (2015) Health Insurance Coverage: early release of estimates from the National Health Interview Survey, January–March 2015. In: National Center for Health Statistics
NAACCR guideline for enhancing Hispanic/Latino identification: Revised NAACCR Hispanic/Latino identification algorithm [NHIA v2.2.1]. In: Group NRaEW. Springfield, IL: North American Association of Central Cancer Registries; 2001
Gomez SL, Glaser SL (2005) Quality of cancer registry birthplace data for Hispanics living in the United States. Cancer Causes Control 16(6):713–723
Keegan TH, John EM, Fish KM, Alfaro-Velcamp T, Clarke CA, Gomez SL (2010) Breast cancer incidence patterns among California Hispanic women: differences by nativity and residence in an enclave. Cancer Epidemiol Biomark Prev 19(5):1208–1218
Yang J, Schupp C, Harrati A, Clarke C, Keegan T, Gomez S (2014) Developing an area-based socioeconomic measure from American Community Survey data. Cancer Prevention Institute of California, Fremont
Yost K, Perkins C, Cohen R, Morris C, Wright W (2001) Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control 12(8):703–711
Banegas MP, Tao L, Altekruse S, Anderson WF, John EM, Clarke CA, Gomez SL (2014) Heterogeneity of breast cancer subtypes and survival among Hispanic women with invasive breast cancer in California. Breast Cancer Res Treat 144(3):625–634
Pinheiro PS, Morris CR, Liu L, Bungum TJ, Altekruse SF (2014) The impact of follow-up type and missed deaths on population-based cancer survival studies for Hispanics and Asians. J Natl Cancer Inst Monogr 2014(49):210–217
Miller BA, Hankey BF, Thomas TL (2002) Impact of sociodemographic factors, hormone receptor status, and tumor grade on ethnic differences in tumor stage and size for breast cancer in US women. Am J Epidemiol 155(6):534–545
Martinez ME, Wertheim BC, Natarajan L, Schwab R, Bondy M, Daneri-Navarro A, Meza-Montenegro MM, Gutierrez-Millan LE, Brewster A, Komenaka IK et al (2013) Reproductive factors, heterogeneity, and breast tumor subtypes in women of Mexican descent. Cancer Epidemiol Biomark Prev 22(10):1853–1861
Anderson KN, Schwab RB, Martinez ME (2014) Reproductive risk factors and breast cancer subtypes: a review of the literature. Breast Cancer Res Treat 144(1):1–10
Warner ET, Tamimi RM, Hughes ME, Ottesen RA, Wong YN, Edge SB, Theriault RL, Blayney DW, Niland JC, Winer EP et al (2015) Racial and ethnic differences in breast cancer survival: mediating effect of tumor characteristics and sociodemographic and treatment factors. J Clin Oncol 33(20):2254–2261
Ryan CL, Bauman K (2016) Educational attainment in the United States: 2015. In: Current population reports (P20-578), U.S. Census Bureau, Washington DC
Proctor BD, Semega JL, Kollar MA (2016) Income and poverty in the United States: 2015. In: Current population reports P60-256(RV), U.S. Census Bureau, Washington DC
Ward E, Halpern M, Schrag N, Cokkinides V, DeSantis C, Bandi P, Siegel R, Stewart A, Jemal A (2008) Association of insurance with cancer care utilization and outcomes. CA Cancer J Clin 58(1):9–31
Obama B (2016) United States health care reform: progress to date and next steps. JAMA 316(5):525–532
California’s uninsured: as coverage grows, millions go without. http://www.chcf.org/publications/2016/12/californias-uninsured
Keegan TH, Quach T, Shema S, Glaser SL, Gomez SL (2010) The influence of nativity and neighborhoods on breast cancer stage at diagnosis and survival among California Hispanic women. BMC cancer 10:603
Gomez SL, Le GM, West DW, Satariano WA, O’Connor L (2003) Hospital policy and practice regarding the collection of data on race, ethnicity, and birthplace. Am J Public Health 93(10):1685–1688
Gomez SL, Quach T, Horn-Ross PL, Pham JT, Cockburn M, Chang ET, Keegan TH, Glaser SL, Clarke CA (2010) Hidden breast cancer disparities in Asian women: disaggregating incidence rates by ethnicity and migrant status. Am J Public Health 100(Suppl 1):S125–S131
Clegg LX, Reichman ME, Hankey BF, Miller BA, Lin YD, Johnson NJ, Schwartz SM, Bernstein L, Chen VW, Goodman MT et al (2007) Quality of race, Hispanic ethnicity, and immigrant status in population-based cancer registry data: implications for health disparity studies. Cancer Causes Control 18(2):177–187
Gomez SL, Glaser SL (2004) Quality of birthplace information obtained from death certificates for Hispanics, Asians, and Pacific Islanders. Ethn Dis 14(2):292–295
Demographic profile of Hispanics in California, 2014. http://www.pewhispanic.org/states/state/ca/
Acknowledgements
We would like to thank Valesca Largaespada for her contribution in the manuscript preparation.
Funding
This work was supported by the Specialized Cancer Center Support Grant to the University of California San Diego Moores Cancer Center (CA023100-29), by the SDSU/UCSD Comprehensive Cancer Center Partnership (CA132379), by and the Stanford Cancer Institute. The collection of cancer incidence data used in this study was supported by the California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety code section 103885; the National Cancer Institute’s Surveillance, Epidemiology and End Results Program under contract HHSN261201000140C awarded to the Cancer Prevention Institute of California, contract HHSN261201000035C awarded to the University of Southern California, and contract HHSN261201000034C awarded to the Public Health Institute; and the Centers for Disease Control and Prevention’s National Program of Cancer Registries, under agreement U58DP003862-01 awarded to the California Department of Public Health. The ideas and opinions expressed herein are those of the author(s) and endorsement by the State of California, Department of Public Health the National Cancer Institute, and the Centers for Disease Control and Prevention or their Contractors and Subcontractors is neither intended nor should be inferred.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
An erratum to this article is available at https://doi.org/10.1007/s10549-017-4455-6.
Rights and permissions
About this article
Cite this article
Martínez, M.E., Gomez, S.L., Tao, L. et al. Contribution of clinical and socioeconomic factors to differences in breast cancer subtype and mortality between Hispanic and non-Hispanic white women. Breast Cancer Res Treat 166, 185–193 (2017). https://doi.org/10.1007/s10549-017-4389-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-017-4389-z