Abstract
Purpose
Women who are newly diagnosed with breast cancer may consider contralateral prophylactic mastectomy (CPM) to reduce their future risk of cancer in their unaffected breast. Pre-surgical BRCA1/2 genetic testing can provide valuable risk information to guide this choice. However, little is understood about why BRCA1/2 mutation noncarriers, who are generally not at substantially elevated risk of contralateral disease, select CPM.
Methods
We examined the uptake of CPM among breast cancer patients identified as BRCA1/2 mutation noncarriers (n = 92) as part of a larger prospective study of the impact of pre-surgical BRCA1/2 testing. Data obtained from self-report questionnaires and patient medical records were used to examine associations between theoretically relevant background and psychosocial factors and BRCA1/2 mutation noncarriers’ decisions to undergo CPM.
Results
Among BRCA1/2 mutation noncarriers, 25% (n = 23) elected to undergo CPM. Psychosocial factors including a self-reported physician recommendation for CPM, greater perceived contralateral breast cancer risk, and greater perceived benefits of CPM were all significantly associated with the uptake of CPM.
Conclusions
A sizeable minority of BRCA1/2 mutation noncarriers choose to undergo CPM after learning their mutation status through pre-surgical genetic testing. BRCA1/2 mutation noncarriers’ cognitive perceptions and social influences appear to be important in shaping their decisions regarding CPM. This work highlights the importance of several psychosocial factors in influencing patients’ surgical decisions. Future research is needed that examines the formation of BRCA1/2 mutation noncarriers’ beliefs regarding their disease and available treatment options, and that characterizes the physician-patient communication that occurs in this complex decision-making context.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In addition to complex treatment decisions, newly diagnosed breast cancer patients must make choices about managing their future cancer risk. One option they may consider is contralateral prophylactic mastectomy (CPM) to minimize the likelihood of developing cancer in their unaffected breast. This decision is somewhat time-sensitive because outcomes are optimized when a woman chooses to undergo CPM early in her treatment course, as she can then avoid risks associated with multiple surgeries and radiation that would compromise breast reconstruction options if she later chose to have a prophylactic mastectomy. The uptake of CPM has increased substantially, with estimates of uptake ranging from 11–18% in recent years [1–4].
Pre-surgical BRCA1/2 genetic testing can provide valuable risk information to guide patients’ decisions about CPM. This is because BRCA1/2 mutation carriers have an elevated risk of developing a new contralateral breast cancer (CBC) in their unaffected breast. Ten years after their index diagnosis, women who are carriers of pathogenic BRCA1/2 mutations have a 27–37% chance of developing CBC [5–7]. Conversely, BRCA1/2 mutation noncarriers face a much lower 10-year CBC risk of 5–10% [6, 8–10]. Following pre-surgical BRCA1/2 testing, mutation carriers are consistently more likely to opt for CPM than are patients with uninformative or negative genetic test results [11–15]. Yet, in spite of their lower levels of objective risk, some women identified as BRCA1/2 mutation noncarriers also choose to undergo CPM [11–17].
The psychosocial factors that may motivate BRCA1/2 mutation noncarriers to select CPM are not well understood. Past work suggests that demographic and medical factors, including younger age [13, 15], marital status [14], and family history of breast [11, 13] and ovarian cancer [15], are associated with BRCA1/2 mutation noncarriers’ use of CPM. Schwartz and colleagues [11] also observed that BRCA1/2 mutation noncarriers who reported that their physician had recommended genetic testing and had recommended CPM were more likely to undergo the surgery. Limited evidence suggests that psychological factors may also influence noncarriers’ decisions. In a retrospective survey, BRCA1/2 mutation noncarriers cited feeling at increased CBC risk, and the desire to reduce CBC risk, obtain peace of mind, and improve survival, as important reasons for choosing CPM [18]. Qualitative interviews conducted with breast cancer patients without BRCA1/2 mutations following completion of CPM also identified influential decision-making factors including patients’ subjective evaluation of the risks and benefits of the various treatment options, ability to maintain or improve breast appearance, and potential to avoid future cancer surveillance and worry [19]. The need exists, however, for studies that prospectively examine how such perceptions of the harms and benefits of CPM or emotional distress about breast cancer may be associated with subsequent CPM uptake among BRCA1/2 mutation noncarriers.
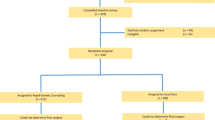
With the present study, we sought to extend past work by examining the CPM decision-making process among newly diagnosed breast cancer patients identified as BRCA1/2 mutation noncarriers through pre-surgical genetic testing. Specifically, we aimed to determine the frequency of CPM uptake, and to identify psychosocial factors contributing to this decision. We evaluated a conceptual model of CPM decision-making (Fig. 1), with the selection of psychosocial factors guided by past empirical work [11, 13, 14, 19–21] and the Preventive Health Model (that identifies various factors that can influence an individual’s decision about preventive behavior) [22, 23]. These factors can include background (e.g. sociodemographic characteristics and medical history), representational (e.g. cognitive perceptions and emotional responses), and social influences (e.g. interpersonal relationships and support). We hypothesized that background factors including family history of breast cancer and younger age (which are most relevant to absolute CBC risk [9]), marital status, and an invasive cancer diagnosis would be associated with CPM uptake. We further hypothesized that noncarriers’ cognitive and emotional representations of CPM would be relevant such that those who perceived greater CBC risk, experienced less decisional conflict, and reported greater breast cancer-related distress would be more likely to choose CPM. Given past qualitative work suggesting the importance of perceived treatment benefits and risks to this decision-making context [19], we also predicted that greater perceptions of benefits and lower perceptions of harms of CPM would be associated with uptake. Finally, we hypothesized that the social influence of a perceived physician recommendation for CPM would be associated with CPM uptake.
Conceptual model of decision-making about contralateral prophylactic mastectomy (CPM). This model describes psychosocial factors including background factors (e.g. sociodemographic characteristics and medical history), social influence factors (e.g. interpersonal relationships and support), and representational factors (e.g. cognitive perceptions and emotional responses) that may influence the decision to undergo CPM (adapted from [22, 23])
Methods
Participants and procedures
Data were collected as part of a larger prospective study of the impact of pre-surgical BRCA1/2 testing among newly diagnosed breast cancer patients. The Memorial Sloan Kettering Cancer Center Institutional Review Board approved the study protocol. Eligible participants included English-speaking women aged 18 or older with a diagnosis of invasive breast cancer or ductal carcinoma in situ (as a primary malignancy or as a second diagnosis if a CBC and the first cancer was not treated with mastectomy) who had not completed definitive surgical treatment and were deemed appropriate for genetic testing based on National Comprehensive Cancer Network criteria [24] (i.e. breast cancer diagnosed at age 45 or younger; bilateral breast cancer first diagnosed at age 50 or younger; breast cancer diagnosed at any age with a male relative with breast cancer; breast cancer diagnosed at age 50 or younger with either at least one relative with breast cancer diagnosed at age 50 or younger or at least one relative with ovarian cancer; or of Ashkenazi Jewish ethnicity with breast cancer diagnosed at age 60 or younger).
Participants were recruited at the time of their surgical consultation. All participants provided written informed consent and underwent a consultation with a genetic counselor trained in hereditary cancer risk assessment. Participants could then choose to provide a DNA sample for pre-surgical BRCA1/2 testing or defer genetic testing until a later time. All participants chose pre-surgical testing. Following genetic testing (Ashkenazi founder mutation testing or full sequencing with large rearrangement testing, as appropriate), participants returned for a genetic counseling session that included the disclosure of the results, and discussion of cancer risk management options and individualized screening recommendations. Prospective data for the present study were obtained from a written self-report questionnaire completed by participants after receiving their BRCA1/2 results and before their surgical treatment, and from review of participants’ medical records.
Measures
Perceived benefits of CPM were assessed with five investigator-designed items (e.g. “it might improve my chances of surviving breast cancer”). Participants rated their agreement with each item as a reason to have CPM on a five-point Likert scale (response options: 1 = “not at all a good reason for me” to 5 = “a very good reason for me”). Responses were summed to create a scale score ranging from 5 to 25, with higher values indicating greater perceived benefits of CPM (Cronbach’s α = 0.86).
Perceived harms of CPM were assessed with five investigator-designed items (e.g. “I would feel disfigured after surgery”). Participants rated their agreement with each item as a reason to not have CPM (response options: 1 = “not at all a good reason for me” to 5 = “a very good reason for me”). Item responses were summed; higher values indicate greater perceived harms of CPM (α = 0.91).
Perceived CBC risk was assessed with one item. Participants indicated how many of 100 women like them “will get breast cancer in their other breast in the next 10 years” (response options: “less than 5,” “between 5 and 10,” “between 10 and 15,” “between 15 and 20,” “between 20 and 25,” and “more than 25”). Responses were recorded to reflect perceived CBC risk consistent with that of a BRCA1/2 mutation noncarrier (0 = “10 or fewer women”) or higher (1 = “More than 10 women”).
Decisional conflict was assessed with the 16-item Decisional Conflict Scale [25], which measures perceptions of uncertainty in choosing decision options; degree of feeling uninformed, unclear about personal values, and unsupported in decision-making; and perceptions of the effectiveness of decision-making regarding CPM (α = 0.96). Scores range from 0 to 100; higher values indicate greater decisional conflict.
Breast cancer-related distress was assessed with the 15-item Impact of Event Scale [26], which measures the presence of intrusive thoughts (α = 0.86; scores range from 0 to 35) and avoidance (α = 0.76; scores range from 0 to 40) regarding the participant’s breast cancer diagnosis.
Perceived physician recommendation for CPM was assessed with one item: “Has your doctor recommended that you have a prophylactic mastectomy?” (response options: yes/no).
Uptake of CPM at the time of each participant’s surgical treatment was abstracted from medical records (response options: yes/no).
Sociodemographic and medical factors abstracted from medical records included age, race, Ashkenazi Jewish ethnicity, marital status, family history of breast cancer, breast cancer diagnosis, hormone receptor status (ER, PR, and HER2/neu) of the diagnosed breast cancer, whether a mastectomy was required for treatment of the affected breast, whether neoadjuvant chemotherapy was used, number of previous breast biopsies, and breast density.
Data analysis
Data were analyzed using SPSS version 22.0. Descriptive statistics were computed for all variables. To describe participants’ perceptions of the benefits and harms of CPM, t-tests were used to compare responses on the individual items from each measure among those who did and did not choose CPM. Chi square significance tests and t-tests were used to examine bivariate associations between psychosocial, sociodemographic, and medical factors with the outcome of CPM uptake. Any variables significantly (p ≤ 0.05) associated with CPM uptake were then included as predictors in a multivariable logistic regression model. All statistical tests were two-tailed with α = 0.05.
Results
Sample characteristics
Data were available for 102 women who underwent pre-surgical BRCA1/2 testing; eight tested positive for a pathogenic BRCA1/2 mutation, two were found to have a variant of uncertain clinical significance, and 92 tested negative for a pathogenic BRCA1/2 mutation. None of these 92 women were tested for known familial mutations. These 92 “BRCA1/2 mutation noncarriers” comprise the present study sample (Table 1). Participant ages ranged from 29 to 59 (median = 43), and the majority were White/Caucasian (83.7; 4.3% of the participants were Black/African American, 4.3% were Asian, and 7.6% declined to answer). Almost two-thirds (62.2%) of the sample reported a family history of breast cancer, with participants reporting a median of one other affected family member (range: 0–5).
Uptake of CPM
Twenty-five percent of the BRCA1/2 mutation noncarriers (23/92) elected to undergo CPM following pre-surgical genetic testing. In comparison, 88% (7/8) of the patients identified as BRCA1/2 mutation carriers and 0% (0/2) of those with a variant of uncertain clinical significance in the larger study chose to undergo CPM.
Psychosocial correlates of the CPM decision
Among the sample of BRCA1/2 mutation noncarriers, 90.2% (83/92) provided responses to the self-report questionnaire including the psychosocial variables. Questionnaire nonresponders did not differ from responders in age, Ashkenazi Jewish ethnicity, cancer diagnosis, or CPM uptake; however, nonresponders were less likely to be married/partnered than responders (44.4 vs. 77.1%, p = 0.05).
We first examined BRCA1/2 mutation noncarriers’ cognitive perceptions of the benefits and harms of CPM (Fig. 2). Participants perceived the ability to reduce their chances of getting breast cancer again, improve their chances of surviving breast cancer, and decrease their worry about breast cancer as the greatest benefits of CPM. Participants who chose to undergo CPM endorsed each of the benefits more strongly than did those who chose to not have the surgery, with the greatest differences observed for the benefits of feeling good about the surgery and regretting not having the surgery. In general, participants did not strongly endorse any of the harms of CPM. No significant differences in the perceptions of harms were observed between those participants who did and did not choose CPM.
Perceived benefits and harms of contralateral prophylactic mastectomy (CPM) among newly diagnosed breast cancer patients identified as BRCA1/2 mutation noncarriers through pre-surgical genetic testing (n = 83). Error bars correspond to the standard error of the mean. Asterisks indicate significant differences in perceived benefits of CPM between those who did and did not choose CPM (p ≤ 0.005)
Next, we examined the extent to which the hypothesized psychosocial factors were associated with BRCA1/2 mutation noncarriers’ surgical decisions. Bivariate (Table 1) and multivariable (Table 2) analyses confirmed several of the hypothesized associations. The social factor of perceiving that one’s physician had recommended CPM was significantly associated with the decision to undergo CPM. Furthermore, the cognitive representation factors of perceiving greater CBC risk and perceiving greater benefits of CPM were both significantly associated with CPM uptake. However, the cognitive representation factors of perceived harms of CPM and decisional conflict, and the emotional representation factor of breast cancer-related distress were not significantly associated with noncarriers’ surgical decisions (all ps > 0.05). In addition, although the medical factor of breast density was associated with CPM uptake in the bivariate analysis (p = 0.04), it did not remain significant in multivariable analysis (p = 0.26) and was thus excluded from the final model. Similarly, none of the other sociodemographic and medical factors were significantly associated with noncarriers’ surgical decisions (all ps > 0.05).
Discussion
The present study examined CPM uptake among newly diagnosed breast cancer patients identified as BRCA1/2 mutation noncarriers through pre-surgical genetic testing. Although BRCA1/2 mutation noncarriers generally do not face substantially elevated CBC risk, we observed that 25% of these patients chose to undergo CPM. This figure is substantially lower than that observed among BRCA1/2 mutation carriers in our larger study (88%), and is consistent with a few other studies of CPM in noncarriers following pre-surgical BRCA1/2 testing [11, 12, 15, 17]. However, this level of uptake is somewhat higher than estimates in the general population of women with breast cancer, which suggest that approximately 11–18% of patients ultimately choose CPM [1–4]. This difference may be attributable in part to the fact that study participants were generally younger (ages 29–59) than is typically observed in a population ascertainment.
In an attempt to explain why BRCA1/2 mutation noncarriers chose to undergo CPM, we also examined how psychosocial factors consistent with the Preventive Health Model [22, 23] contributed to patients’ decision-making. Contrary to our predictions, the examined background sociodemographic and medical factors (which included age and family history, factors most relevant to absolute CBC risk [9]) and emotional factor of breast cancer-related distress were not associated with CPM uptake. Rather, several cognitive representations and social influence factors were most relevant. Results demonstrate that BRCA1/2 mutation noncarriers perceive various benefits of CPM, and these perceptions influence choice of this cancer risk management strategy. Conversely, noncarriers appear to give less weight to the potential harms of CPM, as these beliefs do not contribute to their decision. This observation is noteworthy because CPM is associated with serious physical risks including increased surgical site and post-operative complications as compared to unilateral mastectomy [27–29], and is also associated with psychological complaints regarding physical appearance, sexuality, and feelings of femininity among a minority of patients [18, 30, 31]. Why study participants appear to be less concerned about harms of CPM is unclear, although one study noted that physicians are more likely to discuss reasons for having CPM as opposed to reasons for not having CPM with breast cancer patients who are BRCA1/2 mutation noncarriers [18]. Such findings suggest that patients may benefit from interventions such as decision aids or physician-directed prompts in the electronic medical record that encourage the discussion and deliberation of both the advantages and disadvantages of CPM to promote informed treatment decisions.
As hypothesized, patients’ cognitive perceptions of personal CBC risk also contributed to the decision to undergo CPM. Theoretical and empirical work supports the role of heightened disease risk perceptions in influencing adoption of health protective behaviors [32–35]. However, breast cancer patients can overestimate their likelihood of developing CBC [18, 36]; indeed, in the present study, 59% of participants overestimated their 10 year CBC risk. Evidence is mixed regarding the efficacy of existing educational interventions, including genetic counseling, for improving patients’ subjective understanding of their cancer risk [37, 38]. Newly diagnosed breast cancer patients, in particular, face numerous communication challenges that may interfere with their ability to process or accurately recall this risk information (e.g. exposure to a large amount of complex medical information, the need to make important decisions in a short time period, receipt of conflicting messages from various healthcare providers). Thus, these individuals may benefit from research to develop and test targeted, novel educational and risk communication approaches that promote accurate disease risk perceptions, and consequently, more informed treatment and risk management decision-making.
The social influence factor of perceived physician recommendation for CPM was also associated with patients’ surgical choices. Physicians are a primary source of information and advice for breast cancer patients facing treatment decisions [18, 39]. Furthermore, patient-reported physician recommendations for CPM have been previously associated with CPM uptake in a prospective study of newly diagnosed BRCA1/2 mutation noncarriers [11] and a retrospective study of breast cancer patients who had the surgery [21]. In the present study, perceived physician recommendation for CPM was the strongest predictor of the CPM decision; however, this finding should be interpreted cautiously as only a small proportion of participants (16%) reported that their physician made this recommendation. These participants were treated by different physicians (six different medical oncologists and surgeons among the 13 participants reporting a physician recommendation). Yet, we lack any information about the actual clinical communication that occurred between participants and their physicians—for instance, it is not clear to what extent physicians may have strongly recommended CPM, or simply mentioned it as an available option. Future observational research incorporating qualitative and quantitative methods is needed to examine the content of physician-patient communication regarding CPM and other breast cancer treatment options and to understand what aspects of this communication may shape patients’ perceptions of their physicians’ opinions and preferences.
This study represents one of the first attempts to prospectively evaluate how theoretically informed psychosocial factors influence BRCA1/2 mutation noncarriers’ decision-making about CPM. However, this study has several limitations. Data were collected from a small sample of primarily younger, Caucasian patients at a single cancer center. Study participants may also have been more willing to consider CPM than patients who decline pre-surgical genetic testing (although it is routine surgical practice at our center to refer all high-risk patients for genetic testing and participants were offered the option of deferring genetic testing until after their treatment but none chose to do so); such potential selection bias may have influenced the study results. Thus, the generalizability of these findings to more diverse patients and treatment settings requires further study. Furthermore, the small sample size likely contributed to the wide confidence intervals observed for the associations between perceived CBC risk and perceived physician recommendation with CPM uptake. Future studies utilizing larger, more diverse samples would provide more precise estimates and greater insight into the role of these psychosocial factors in patients’ decision-making. Established, well-validated measures were used to assess several of the psychosocial factors. However, novel measures and single-item measures were also used, and the reliability and validity of such items are unknown. In addition, the measures of perceived benefits and harms of CPM may not have assessed the full range of issues that patients and their physicians consider in this decision-making context. Relevant medical factors including the hormone receptor status of the cancer, necessity of mastectomy and neoadjuvant chemotherapy for treatment of the affected breast, and participants’ history of breast biopsies and breast density were included in the analyses; however, additional clinical data that may contribute to contralateral disease risk (e.g. history of benign disease in the contralateral breast) and therefore inform decision-making were not available. Finally, no data were available regarding the outcomes of this decision (e.g. surgical complications, regret, satisfaction), although such longitudinal data would provide valuable insight into the CPM decision-making process among BRCA1/2 mutation noncarriers.
In spite of these limitations, these results can guide future research. We observed that social influences, namely physician recommendations, shape BRCA1/2 mutation noncarriers’ decisions about CPM. However, it remains possible that other individuals, such as a patient’s spouse/partner, family members, and close friends, also influence this decision [21]. These individuals could provide direct feedback about the appropriateness of CPM, or indirectly influence a patient’s decision by shaping her cognitive representations, including her perceptions of future disease risk [40, 41]. Research should investigate the development of BRCA1/2 mutation noncarriers’ beliefs about their CBC risk and the benefits and harms of CPM, with a particular emphasis on the interpersonal communication that occurs in this decision-making context. Studies could utilize observational methods (e.g. recordings of discussions between patients and physicians) and collect data from multiple individuals (e.g. patients and spouses/partners) to examine how others’ perspectives can inform and interact with women’s past experiences, emotions, and beliefs to influence their cancer risk management decisions.
Conclusions
Study results demonstrate that a sizable minority of recently diagnosed breast cancer patients who learn that they are BRCA1/2 mutation noncarriers through pre-surgical genetic testing will nonetheless elect to undergo CPM. These patients’ CPM decisions are influenced by psychosocial factors including their cognitive perceptions about the benefits of CPM and their CBC risk. In addition, patients’ physicians can exert a powerful social influence on their decision-making about CPM. Future research is needed that examines the formation of patients’ beliefs regarding their disease and available treatment options and that characterizes the communication between patients and physicians regarding these issues. Such work could inform the development of educational, risk communication, and decision-making interventions to assist newly diagnosed breast cancer patients with making informed cancer risk management decisions.
References
Jagsi R, Jiang J, Momoh AO, Alderman A, Giordano SH, Buchholz TA, Kronowitz SJ, Smith BD (2014) Trends and variation in use of breast reconstruction in patients with breast cancer undergoing mastectomy in the United States. J Clin Oncol 32(9):919–926. doi:10.1200/jco.2013.52.2284
Kurian AW, Lichtensztajn DY, Keegan TH, Nelson DO, Clarke CA, Gomez SL (2014) Use of and mortality after bilateral mastectomy compared with other surgical treatments for breast cancer in California, 1998–2011. JAMA 312(9):902–914. doi:10.1001/jama.2014.10707
Tuttle TM, Habermann EB, Grund EH, Morris TJ, Virnig BA (2007) Increasing use of contralateral prophylactic mastectomy for breast cancer patients: a trend toward more aggressive surgical treatment. J Clin Oncol 25(33):5203–5209. doi:10.1200/jco.2007.12.3141
Kummerow KL, Du L, Penson DF, Shyr Y, Hooks MA (2015) Nationwide trends in mastectomy for early-stage breast cancer. JAMA Surg 150(1):9–16. doi:10.1001/jamasurg.2014.2895
Robson M, Svahn T, McCormick B, Borgen P, Hudis CA, Norton L, Offit K (2005) Appropriateness of breast-conserving treatment of breast carcinoma in women with germline mutations in BRCA1 or BRCA2: a clinic-based series. Cancer 103(1):44–51. doi:10.1002/cncr.20728
Robson ME, Chappuis PO, Satagopan J, Wong N, Boyd J, Goffin JR, Hudis C, Roberge D, Norton L, Begin LR, Offit K, Foulkes WD (2004) A combined analysis of outcome following breast cancer: differences in survival based on BRCA1/BRCA2 mutation status and administration of adjuvant treatment. Breast Cancer Res 6(1):R8–r17. doi:10.1186/bcr658
Metcalfe K, Lynch HT, Ghadirian P, Tung N, Olivotto I, Warner E, Olopade OI, Eisen A, Weber B, McLennan J, Sun P, Foulkes WD, Narod SA (2004) Contralateral breast cancer in BRCA1 and BRCA2 mutation carriers. J Clin Oncol 22(12):2328–2335. doi:10.1200/jco.2004.04.033
Rhiem K, Engel C, Graeser M, Zachariae S, Kast K, Kiechle M, Ditsch N, Janni W, Mundhenke C, Golatta M, Varga D, Preisler-Adams S, Heinrich T, Bick U, Gadzicki D, Briest S, Meindl A, Schmutzler RK (2012) The risk of contralateral breast cancer in patients from BRCA1/2 negative high risk families as compared to patients from BRCA1 or BRCA2 positive families: a retrospective cohort study. Breast Cancer Res 14(6):R156. doi:10.1186/bcr3369
Reiner AS, John EM, Brooks JD, Lynch CF, Bernstein L, Mellemkjaer L, Malone KE, Knight JA, Capanu M, Teraoka SN, Concannon P, Liang X, Figueiredo JC, Smith SA, Stovall M, Pike MC, Haile RW, Thomas DC, Begg CB, Bernstein JL (2013) Risk of asynchronous contralateral breast cancer in noncarriers of BRCA1 and BRCA2 mutations with a family history of breast cancer: a report from the women’s environmental cancer and radiation epidemiology study. J Clin Oncol 31(4):433–439. doi:10.1200/jco.2012.43.2013
Malone KE, Begg CB, Haile RW, Borg A, Concannon P, Tellhed L, Xue S, Teraoka S, Bernstein L, Capanu M, Reiner AS, Riedel ER, Thomas DC, Mellemkjaer L, Lynch CF, Boice JD Jr, Anton-Culver H, Bernstein JL (2010) Population-based study of the risk of second primary contralateral breast cancer associated with carrying a mutation in BRCA1 or BRCA2. J Clin Oncol 28(14):2404–2410. doi:10.1200/jco.2009.24.2495
Schwartz MD, Lerman C, Brogan B, Peshkin BN, Halbert CH, DeMarco T, Lawrence W, Main D, Finch C, Magnant C, Pennanen M, Tsangaris T, Willey S, Isaacs C (2004) Impact of BRCA1/BRCA2 counseling and testing on newly diagnosed breast cancer patients. J Clin Oncol 22(10):1823–1829. doi:10.1200/jco.2004.04.086
Lokich E, Stuckey A, Raker C, Wilbur JS, Laprise J, Gass J (2014) Preoperative genetic testing affects surgical decision making in breast cancer patients. Gynecol Oncol 134(2):326–330. doi:10.1016/j.ygyno.2014.05.028
Wang F, Amara D, Peled AW, Sbitany H, Foster RD, Ewing CA, Alvarado M, Esserman LJ (2015) Negative genetic testing does not deter contralateral prophylactic mastectomy in younger patients with greater family histories of breast cancer. Ann Surg Oncol 22(10):3338–3345. doi:10.1245/s10434-015-4745-3
Howard-McNatt M, Schroll RW, Hurt GJ, Levine EA (2011) Contralateral prophylactic mastectomy in breast cancer patients who test negative for BRCA mutations. Am J Surg 202(3):298–302. doi:10.1016/j.amjsurg.2011.04.001
Elsayegh N, Kuerer HM, Lin H, Gutierrez Barrera AM, Jackson M, Muse KI, Litton JK, Albarracin C, Afrough A, Hortobagyi GN, Arun BK (2014) Predictors that influence contralateral prophylactic mastectomy election among women with ductal carcinoma in situ who were evaluated for BRCA genetic testing. Ann Surg Oncol 21(11):3466–3472. doi:10.1245/s10434-014-3747-x
Rosenberg SM, Ruddy KJ, Tamimi RM, Gelber S, Schapira L, Come S, Borges VF, Larsen B, Garber JE, Partridge AH (2016) BRCA1 and BRCA2 mutation testing in young women with breast cancer. JAMA oncol. doi:10.1001/jamaoncol.2015.5941
Elsayegh N, Profato J, Barrera AMG, Lin H, Kuerer HM, Ardic C, Litton JK, Tripathy D, Arun BK (2015) Predictors that influence election of contralateral prophylactic mastectomy among women with ductal carcinoma in situ who are BRCA-negative. J Cancer 6(7):610–615. doi:10.7150/jca.11710
Rosenberg SM, Tracy MS, Meyer ME, Sepucha K, Gelber S, Hirshfield-Bartek J, Troyan S, Morrow M, Schapira L, Come SE, Winer EP, Partridge AH (2013) Perceptions, knowledge, and satisfaction with contralateral prophylactic mastectomy among young women with breast cancer: a cross-sectional survey. Ann Intern Med 159(6):373–381. doi:10.7326/0003-4819-159-6-201309170-00003
Rendle KA, Halley MC, May SG, Frosch DL (2015) Redefining risk and benefit: understanding the decision to undergo contralateral prophylactic mastectomy. Qual Health Res 25(9):1251–1259. doi:10.1177/1049732314557085
Beesley H, Holcombe C, Brown SL, Salmon P (2013) Risk, worry and cosmesis in decision-making for contralateral risk-reducing mastectomy: analysis of 60 consecutive cases in a specialist breast unit. Breast 22(2):179–184. doi:10.1016/j.breast.2012.06.005
Soran A, Ibrahim A, Kanbour M, McGuire K, Balci FL, Polat AK, Thomas C, Bonaventura M, Ahrendt G, Johnson R (2015) Decision making and factors influencing long-term satisfaction with prophylactic mastectomy in women with breast cancer. Am J Clin Oncol 38(2):179–183. doi:10.1097/COC.0b013e318292f8a7
Myers RE (2005) Decision counseling in cancer prevention and control. Health Psychol 24(4 Suppl):S71–s77. doi:10.1037/0278-6133.24.4.s71
Myers RE, Ross E, Jepson C, Wolf T, Balshem A, Millner L, Leventhal H (1994) Modeling adherence to colorectal cancer screening. Prev Med 23(2):142–151. doi:10.1006/pmed.1994.1020
Daly MB, Axilbund JE, Buys S, Crawford B, Farrell CD, Friedman S, Garber JE, Goorha S, Gruber SB, Hampel H, Kaklamani V, Kohlmann W, Kurian A, Litton J, Marcom PK, Nussbaum R, Offit K, Pal T, Pasche B, Pilarski R, Reiser G, Shannon KM, Smith JR, Swisher E, Weitzel JN (2010) Genetic/familial high-risk assessment: breast and ovarian. J Natl Compr Canc Netw 8(5):562–594
O’Connor AM (1995) Validation of a Decisional Conflict Scale. Med Decis Making 15(1):25–30. doi:10.1177/0272989x9501500105
Horowitz M, Wilner N, Alvarez W (1979) Impact of Event Scale: a measure of subjective stress. Psychosom Med 41:209–218
Silva AK, Lapin B, Yao KA, Song DH, Sisco M (2015) The effect of contralateral prophylactic mastectomy on perioperative complications in women undergoing immediate breast reconstruction: a NSQIP analysis. Ann Surg Oncol 22(11):3474–3480. doi:10.1245/s10434-015-4628-7
Miller ME, Czechura T, Martz B, Hall ME, Pesce C, Jaskowiak N, Winchester DJ, Yao K (2013) Operative risks associated with contralateral prophylactic mastectomy: a single institution experience. Ann Surg Oncol 20(13):4113–4120. doi:10.1245/s10434-013-3108-1
Osman F, Saleh F, Jackson TD, Corrigan MA, Cil T (2013) Increased postoperative complications in bilateral mastectomy patients compared to unilateral mastectomy: an analysis of the NSQIP database. Ann Surg Oncol 20(10):3212–3217. doi:10.1245/s10434-013-3116-1
Frost MH, Hoskin TL, Hartmann LC, Degnim AC, Johnson JL, Boughey JC (2011) Contralateral prophylactic mastectomy: long-term consistency of satisfaction and adverse effects and the significance of informed decision-making, quality of life, and personality traits. Ann Surg Oncol 18(11):3110–3116. doi:10.1245/s10434-011-1917-7
Frost MH, Slezak JM, Tran NV, Williams CI, Johnson JL, Woods JE, Petty PM, Donohue JH, Grant CS, Sloan JA, Sellers TA, Hartmann LC (2005) Satisfaction after contralateral prophylactic mastectomy: the significance of mastectomy type, reconstructive complications, and body appearance. J Clin Oncol 23(31):7849–7856. doi:10.1200/jco.2005.09.233
Orom H, Kiviniemi MT, Shavers VL, Ross L, Underwood Iii W (2013) Perceived risk for breast cancer and its relationship to mammography in Blacks, Hispanics, and Whites. J Behav Med 36(5):466–476. doi:10.1007/s10865-012-9443-z
Katapodi MC, Lee KA, Facione NC, Dodd MJ (2004) Predictors of perceived breast cancer risk and the relation between perceived risk and breast cancer screening: a meta-analytic review. Prev Med 38(4):388–402. doi:10.1016/j.ypmed.2003.11.012
Dillard AJ, Couper MP, Zikmund-Fisher BJ (2010) Perceived risk of cancer and patient reports of participation in decisions about screening: the decisions study. Med Decis Making 30(5 suppl):96S–105S. doi:10.1177/0272989x10377660
Weinstein ND (1993) Testing four competing theories of health-protective behavior. Health Psychol 12(4):324–333
Abbott A, Rueth N, Pappas-Varco S, Kuntz K, Kerr E, Tuttle T (2011) Perceptions of contralateral breast cancer: an overestimation of risk. Ann Surg Oncol 18(11):3129–3136. doi:10.1245/s10434-011-1914-x
Smerecnik CMR, Mesters I, Verweij E, De Vries NK, De Vries H (2009) A systematic review of the impact of genetic counseling on risk perception accuracy. J Genet Couns 18(3):217–228. doi:10.1007/s10897-008-9210-z
Dieng M, Watts CG, Kasparian NA, Morton RL, Mann GJ, Cust AE (2014) Improving subjective perception of personal cancer risk: systematic review and meta-analysis of educational interventions for people with cancer or at high risk of cancer. Psychooncology 23(6):613–625. doi:10.1002/pon.3476
O’Leary KA, Estabrooks CA, Olson K, Cumming C (2007) Information acquisition for women facing surgical treatment for breast cancer: influencing factors and selected outcomes. Patient Educ Couns 69(1–3):5–19. doi:10.1016/j.pec.2007.08.002
Hamilton JG, Lobel M (2015) Psychosocial factors associated with risk perceptions for chronic diseases in younger and middle-aged women. Women Health 55(8):921–942. doi:10.1080/03630242.2015.1061094
Montgomery GH, Erblich J, DiLorenzo T, Bovbjerg DH (2003) Family and friends with disease: their impact on perceived risk. Prev Med 37(3):242–249. doi:10.1016/S0091-7435(03)00120-8
Acknowledgements
This study was supported by award C026591 (PI: Mark E. Robson, MD) from the New York State Department of Health, NCI P30 CA008748, Robert and Kate Niehaus Center for Inherited Cancer Genomics, and the Breast Cancer Research Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
This research complies with the current laws of the country in which it was performed (United States). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Hamilton, J.G., Genoff, M.C., Salerno, M. et al. Psychosocial factors associated with the uptake of contralateral prophylactic mastectomy among BRCA1/2 mutation noncarriers with newly diagnosed breast cancer. Breast Cancer Res Treat 162, 297–306 (2017). https://doi.org/10.1007/s10549-017-4123-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-017-4123-x