Abstract
Breast cancer risk assessment can inform the use of screening and prevention modalities. We investigated the performance of the Breast Cancer Surveillance Consortium (BCSC) risk model in combination with a polygenic risk score (PRS) comprised of 83 single nucleotide polymorphisms identified from genome-wide association studies. We conducted a nested case–control study of 486 cases and 495 matched controls within a screening cohort. The PRS was calculated using a Bayesian approach. The contributions of the PRS and variables in the BCSC model to breast cancer risk were tested using conditional logistic regression. Discriminatory accuracy of the models was compared using the area under the receiver operating characteristic curve (AUROC). Increasing quartiles of the PRS were positively associated with breast cancer risk, with OR 2.54 (95 % CI 1.69–3.82) for breast cancer in the highest versus lowest quartile. In a multivariable model, the PRS, family history, and breast density remained strong risk factors. The AUROC of the PRS was 0.60 (95 % CI 0.57–0.64), and an Asian-specific PRS had AUROC 0.64 (95 % CI 0.53–0.74). A combined model including the BCSC risk factors and PRS had better discrimination than the BCSC model (AUROC 0.65 versus 0.62, p = 0.01). The BCSC-PRS model classified 18 % of cases as high-risk (5-year risk ≥3 %), compared with 7 % using the BCSC model. The PRS improved discrimination of the BCSC risk model and classified more cases as high-risk. Further consideration of the PRS’s role in decision-making around screening and prevention strategies is merited.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Breast cancer risk varies based on mammographic breast density, family history, reproductive history, hormone exposure, genetic variants, and other risk factors [1]. Risk prediction models are useful to identify high-risk women who may benefit from supplemental screening with MRI [2] or chemoprevention [1, 3]. Risk prediction models may also be useful to guide the age at which screening begins and the frequency of screening [4, 5]. Improving the predictive power of risk models is an important step toward targeted screening and prevention.
Risk prediction models [1, 6, 7] have incorporated family history, demographic, reproductive, and hormonal risk factors. We developed the Breast Cancer Surveillance Consortium (BCSC) risk model to include mammographic breast density, a strong risk factor for breast cancer, in addition to age, race/ethnicity, first-degree relative with breast cancer, and history of breast biopsy [8, 9]. The model has been validated in a multiethnic population and expanded to include history of benign breast disease [9].
Common genetic variants may also be useful in risk stratification. Genome-wide association studies (GWAS) have identified over 90 single nucleotide polymorphisms (SNPs) associated with breast cancer [10–20]. Although the individual effect sizes of each SNP are modest, together they account for 15–20 % of familial breast cancer risk [20].
Polygenic risk scores (PRS) combine the effects of multiple SNPs and enhance breast cancer risk models. The Breast Cancer Association Consortium demonstrated that a 77-SNP PRS was a strong predictor of breast cancer in women with and without a positive family history [21]. Vachon and colleagues reported that adding a 76-SNP PRS to the BCSC risk model improved prediction [22]. Likewise, a 77-SNP PRS improved the discrimination of the Gail and Tyrer-Cuzick models [23]. Studies combining PRS and breast cancer risk factors have focused on Caucasian populations. We sought to replicate these findings in an independent population including non-Caucasian women. We used 83 SNPs to construct our PRS given the expanding number of validated SNPs in populations of different ethnicities.
Materials and methods
Study population
We performed a nested case–control study within the California Pacific Medical Center (CPMC) Research Institute Cohort, which participates in the San Francisco Mammography Registry (SFMR). Participants were recruited from the Breast Health Center at CPMC, an imaging facility within the SFMR. All women presenting for mammography completed a questionnaire with demographic information and risk factor data. Questionnaire data were collected by the SFMR, as approved by the institutional review boards at CPMC and the University of California, San Francisco. From 2004 to 2011, women were also asked to provide blood samples for research and written informed consent to undergo genotyping. Samples were obtained from 19,276 women.
Cases (n = 1203) had a first diagnosis of invasive breast cancer between 1998 and 2013. Diagnosis of breast cancer was ascertained by linkage to the California Cancer Registry (CCR), with last linkage on October 31, 2013; women without breast cancer at this time were considered controls. We randomly selected 500 cases for genotyping. Since blood sample collection could have occurred before or after first diagnosis of breast cancer, incident and prevalent cases were included. We also genotyped 500 controls matched by age at study mammogram, race/ethnicity, and mammography machine.
Of the 1000 women genotyped, 19 were excluded from the analysis due to inability to retrieve the original mammography films for breast density measurement (n = 14), inability to calculate polygenic risk score due to failed genotyping (n = 4), and self-reported race for which BCSC risk could not be estimated (n = 1). Of the remaining 981 women, 495 were controls and 486 were cases.
Polygenic risk score
Genotyping was performed using an Illumina Oncoarray (Illumina, San Diego, CA, USA) at the Genomics Core of the University of Minnesota. For this analysis, we included SNPs reported as genome-wide significant (p < 5 × 10−8) in studies of invasive breast cancer in Caucasian, Asian, or Hispanic populations [10–12, 14–19, 24–26] which we identified by review of the GWAS catalog [27]. If a SNP was not on the array, we sought a proxy SNP in strong linkage disequilibrium (LD), r 2 > 0.9. If multiple SNPs at a single locus were reported, we selected the SNP most strongly associated at that locus and dropped SNPs in moderate to strong LD, r 2 > 0.5. We excluded SNPs associated with subtypes of breast cancer, but not breast cancer overall, and modifiers of BRCA1 and BRCA2 effect if they were not associated with breast cancer in non-BRCA1/2 carriers. The final list included 83 SNPs (Table S1).
We constructed two separate PRS, one with the allele frequencies and odds ratios (ORs) from Caucasian populations used in the main analysis, and another with allele frequencies and ORs from East Asian populations (Table S2) [15, 16, 18]. The Asian-specific PRS had 76 SNPs after the exclusion of SNPs that were non-polymorphic in Asian populations. For SNPs not validated in an Asian population, the Caucasian odds ratio and the published East Asian allele frequency from 1000 Genomes [28] were used.
We calculated the PRS as the composite likelihood ratio (LR) representing the individual effects of each SNP. For each locus with alleles A and a, the probability of genotypes given disease status can be given by the equations:
where p is the population frequency of the risk allele and γ is the per-allele relative risk of breast cancer (approximating the OR) [29]. The likelihood ratios for breast cancer can be given as \(\frac{{P({\text{AA | D + }}) }}{{P({\text{AA }}| {\text{D}} - )}}\), \(\frac{{P({\text{Aa }}| {\text{D}} + )}}{{P({\text{Aa }}| {\text{D}} - )}}\), and \(\frac{{P({\text{aa }}| {\text{D}} + )}}{{P({\text{aa }}| {\text{D}} - )}}\), respectively. Assuming all of the SNPs are inherited independently, and there are no interactions between them, the LR for each multi-SNP genotype, G i , is the product of the likelihood ratios for the genotype, g i , of each of the n SNPs.
Using a Bayesian approach, the 5-year risk of breast cancer for a person with LR Gi is
where K i is the 5-year risk probability projected by the BCSC model [29].
BCSC risk score
We used a fitted version of the BCSC model (fitted-BCSC) for multivariable analysis on the association of the PRS and other BCSC risk factors with breast cancer. Each variable was included as a separate regression term, including body mass index (BMI) given the confounding effect of BMI on the relationship between mammographic density and breast cancer risk [30]. We used version 2.0 of the BCSC model (BCSCv2) to generate absolute risk estimates [9]. Version 2.0 is the most current version of the BCSC model and allows calculation of 5- and 10-year risk, but does not calculate risk for women over the age of 74 [9]. Mammographic breast density was classified according to the Breast Imaging Reporting and Data System (BIRADS) scoring system [31]: almost entirely fatty (a), scattered areas of fibroglandular density (b), heterogeneously dense (c), and extremely dense (d). Category b was designated as the reference group.
Statistical analysis
We compared demographic data and risk factors between cases and controls using the Chi-squared test for categorical measures and the t test for continuous measures. All tests of statistical significance were two-sided, with α = 0.05. Univariate and multivariable conditional logistic regression models to predict breast cancer were constructed with the polygenic risk score, the fitted-BCSC model (fitted-BCSC), and the PRS combined with the fitted-BCSC model (fitted-BCSC-PRS model). The PRS was analyzed as a continuous variable and as quartiles based on its distribution in controls.
The area under the receiver operating characteristic curve (AUROC) was used to compare discrimination of the models. To account for the matched case–control design, the AUROC and confidence intervals were calculated using a stratified bootstrap algorithm (n = 1000 replications) with separate sampling from cases and controls. To evaluate for overfitting in the fitted-BCSC model, we performed split-sample validation. Two-thirds of the dataset (n = 654), with an equal number of cases and controls, was randomly sampled as the training set. The coefficients corresponding to the variables in the fitted-BCSC model were used for prediction in the validation set (n = 327). The AUROC of the fitted-BCSC model was compared between randomly generated discovery and validation sets across 1000 replications.
To evaluate the effect of the PRS on the reclassification of risk, we calculated two 5-year risk estimates: one using the BCSCv2 estimate, and another using the BCSCv2 estimate modified by the PRS (BCSCv2-PRS model). Given that the BCSCv2 model does not calculate risk estimates for women over age 74, this analysis was limited to the 471 cases and 460 controls under the age of 74. We calculated the percentages of controls and cases whose risk estimates fell within 5- and 10-year risk strata according to the BCSCv2 and BCSCv2-PRS models. Calibration of the fitted-BCSC-PRS model was assessed using the Hosmer–Lemeshow test [32].
Primary statistical analysis was performed using STATA 14.1 (StataCorp, College Station, TX, USA). The PRS was generated using a script in R (R Foundation, Vienna, Austria). The BCSCv2 absolute risk calculations were done using SAS Version 9.3 (SAS Institute, Cary, NC, USA).
Results
Demographics and exposures
Eighty percent of participants were of self-reported Caucasian/White race, while women of self-reported East Asian descent were the most prevalent non-Caucasian subgroup, comprising 11 % of overall participants (Table 1). Cases were more likely to have a positive family history of breast cancer, prior biopsy, and dense breasts (BIRADS c and d). Cases were also more likely to be at high or very high risk using the BCSCv2 5-year risk estimates. Three hundred three cases (62.3 %) had incident cancers, and the remaining 183 cases (37.7 %) had prevalent cancers.
An 83-SNP polygenic risk score was constructed based on SNPs with published genome-wide associations with breast cancer (Table S1). We expanded on a previously described 76-SNP PRS [22] by including SNPs validated in Asian or Hispanic populations [10, 11, 15], with additional SNPs curated from published catalogs [12, 13, 17, 27]. Our PRS had 71 SNPs in common with the previously described 76-SNP PRS [22]. Nine of the 83 SNPs were nominally associated with breast cancer (p < 0.05) (Table S1). The mean PRS was higher in cases than in controls, 1.20 (standard deviation 0.85) versus 0.97 (standard deviation 0.68).
Effect of polygenic risk score and other risk factors on breast cancer
There was a strong association between higher PRS and breast cancer, with the highest risk quartile having an OR of 2.54 (95 % CI 1.69–3.82) compared with the lowest risk quartile (Table 2). Family history (OR 1.89, 95 % CI 1.39–2.56), history of breast biopsy (OR 1.58, 95 % CI 1.16–2.15), and breast density (OR 1.51, 95 % CI 1.13–2.03 for BIRADS c and OR 1.95, 95 % CI 1.24–3.07 for BIRADS d) were also associated with breast cancer in univariate analyses. In a multivariable model including PRS and family history, there was minimal change in the associations between the PRS quartiles and family history on breast cancer risk. In the fitted-BCSC model, which includes all risk factors in the BCSC risk model in addition to BMI, the point estimates for the PRS were minimally changed.
The fitted-BCSC model accounts for the effect of BMI on breast density as a predictor. Since obesity is associated with higher breast cancer risk but lower breast density [33], we suspected that BMI was a negative confounder of the association between density and breast cancer. Adjusting for BMI increased the magnitude of the effect of breast density (Table S3). Adding the PRS to this model minimally attenuated the association between each density category and breast cancer. Given that BMI was a significant risk factor for breast cancer and changed the point estimates associated with each BIRADS category substantively (≥10 %), we used the fitted-BCSC model in our primary analysis.
Split-sample validation showed evidence of overfitting with the fitted-BCSC model, although the effect on the AUROC point estimate was minimal. The AUROC was 0.62 (95 % CI 0.59–0.66) in the discovery set and 0.61 (95 % CI 0.54–0.68) in the validation set.
Discrimination of models
Receiver operating characteristic curve analysis was used to compare the discrimination of three models (Fig. 1): the PRS alone, the fitted-BCSC model, and the polygenic risk score plus fitted-BCSC model (fitted-BCSC-PRS). The AUROC of the fitted-BCSC model was 0.62 (95 % CI 0.59–0.66), which was slightly higher than that of the PRS, which was 0.60 (95 % CI 0.57–0.64) (Table 3). The fitted-BCSC-PRS model had the highest discrimination, with an AUROC of 0.65 (95 % CI 0.61–0.68). Specifically, the difference between the AUROCs for the fitted-BCSC model with and without the PRS reached statistical significance (p = 0.01). When the analysis was restricted to incident cases only, the AUROCs were 0.01 higher for the PRS, fitted-BCSC, and fitted-BCSC-PRS models (Fig. S1).
A 76-SNP PRS constructed using East Asian-specific allele frequencies and ORs (Table S2) was tested in the Asian subset of our study. Using the Asian-specific PRS, the mean PRS was 0.96 (SD 0.43) in Asian controls and 1.24 (SD 0.60) in Asian cases. In Asians, the discrimination of the Asian PRS was higher than that of the overall PRS, with AUROC of 0.64 (95 % CI 0.53–0.74) versus AUROC 0.62 (95 % CI 0.52–0.73), Fig. 2a, b. In contrast, the AUROC associated with the general PRS was 0.59 (95 % CI 0.56–0.63) in Caucasians (Fig. 2c). When the Asian-specific PRS was combined with the fitted-BCSC model, the AUROC increased to 0.72 (95 % CI 0.62–0.82). In Caucasians, the fitted-BCSC-PRS model AUROC was 0.63 (95 % CI 0.59–0.67), Fig. S2.
The receiver operating characteristic curves and corresponding area under the curve (AUC) with 95 % confidence interval are shown for a the Asian-specific, 76-SNP polygenic risk score in East Asians, b the general, 83-SNP polygenic risk score in East Asians, and c the general, 83-SNP polygenic risk score in Caucasians
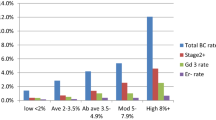
We investigated how risk prediction for cases and controls differed when the PRS was used to modify the BCSC model absolute risk estimate. Figure 3 shows the percentages of cases and controls classified within 5-year risk strata according to estimates generated using the BCSCv2 and BCSCv2-PRS models. The BCSCv2-PRS model classified 49 % of controls as having a 5-year risk ≤1 % (Fig. 3a), compared with 33 % of controls according to the BCSCv2 model (Fig. 3b). The 5-year risk threshold of ≤1 % is considered low-risk, given the 5-year risk of an average 50-year-old Caucasian woman is 1.3 % [34]. Additionally, the BCSCv2-PRS model classified more cases as extremely high risk (5-year risk ≥3 %, indicated by the dashed line in Fig. 3). The USPSTF currently recommends consideration of chemoprevention for women with a 5-year risk ≥3 %. The BCSCv2-PRS model classified 18 % of cases above this threshold, compared with 7 % according to the BCSCv2 model. A similar effect was seen when comparing 10-year risk estimates generated by the unmodified BCSCv2 model and the BCSCv2 model modified by the PRS (Fig. S3).
Calibration of the models was assessed using the Hosmer–Lemeshow test with the study population split into 10 subgroups of identical risk. There was no significant deviation from expectation of the fitted-BCSC-PRS model (Chi-squared = 975.7, p = 0.42), or the BCSCv2-PRS model (Chi-squared = 937.0, p = 0.41).
Discussion
An 83-SNP polygenic risk score was a strong risk factor for breast cancer whose effect was not diminished by adjustment for family history, prior breast biopsy, or breast density. Adding the PRS to the BCSC model improved discrimination, suggesting the PRS plays a role in risk stratification and exerts an effect distinct from clinical risk factors and breast density. The BCSCv2-PRS classified nearly three times as many cases into the high-risk (≥3 %) strata compared with the BCSCv2 model.
The results of our main analysis are mostly consistent with prior studies. The AUROC of our PRS alone, 0.60 (95 % CI 0.57–0.64), is similar to the c-statistic of 0.62 (95 % CI 0.62–0.63) using a 77-locus PRS in a study of over 30,000 cases and controls [21]. The only other study on a combined PRS-BCSC model reported improved discrimination when a 76-SNP PRS was added to the BCSC model [22]. Our study replicated these results from Vachon et al. using an 83-SNP PRS that included 71 SNPs from that study. There were slight differences in the AUROC for the BCSC-PRS model in our study (0.65, 95 % CI 0.61–0.68) compared with Vachon (0.69, 95 % CI 0.64–0.73) [22]. The reported AUC from the latter study was based on a multiple sampling approach in the validation cohort and did not account for BMI in the BCSC model.
The AUROC of 0.62 for the fitted-BCSC model was lower than previously reported values, which range from 0.65 to 0.66 [8, 9, 22]. Matching by age and race/ethnicity, two of the variables in the model, likely decreased its predictive power. Furthermore, prior studies incorporated solely incident cases while ours included both prevalent and incident cancers. When the analysis was restricted to incident cancers, the AUROC for the fitted-BCSC and fitted-BCSC-PRS models increased. On the other hand, overfitting may have led to overestimation of the AUROC of the fitted-BCSC and fitted-BCSC-PRS models. Our cross-validation analysis showed that the fitted-BCSC model had a higher AUROC in the discovery set, but the absolute difference was 0.01, justifying fitting a modified BCSC model to derive the predictive value of BMI-adjusted breast density.
One of the strengths of this study is the multiethnic makeup relative to prior investigations of the PRS. This allowed for exploration of the performance of a PRS tailored to East Asians, the largest non-Caucasian subgroup in this study. Nearly all SNPs discovered in Caucasians have been validated in Asians, with similar ORs [18]. The PRS using ORs from Caucasian populations applied to Asian populations should perform well, as we observed. When Asian-specific allele frequencies and ORs were used, the discrimination improved, although we are unable to exclude the effect of chance due to the relatively wide confidence interval for the AUROC in Asians. To our knowledge, our study is the first to investigate the performance of a race or ethnicity-specific PRS. Additional studies in larger populations should help refine the PRS in East Asians and other populations.
Our study supports previously reported observations about polygenic risk. First, the modest attenuation in the effects of PRS and family history in joint models suggests that a small fraction of family history is attributed to these SNPs. This is consistent with prior studies [21, 23, 35]. Second, the association between breast density and breast cancer was slightly attenuated after adjustment for the PRS. Breast density is 60–70 % heritable, and GWAS have identified seven loci associated with percent dense area [36]. Our PRS includes at least two SNPs associated with density, rs10995190 (ZNF365) and rs3817198 (LSP1) and SNPs from ESR1, a locus that is associated with density [36, 37]. Thus, our version of the PRS accounts for a small portion of the heritability of breast density, and inclusion of the PRS minimally affects the association between breast density and breast cancer.
We used a Bayesian approach to combine information on risk across SNPs [38]. Others have used an approach where the PRS is calculated as the sum of the product of the per-allele log-OR and the number of risk alleles for each SNP [21, 22] which can be rescaled so that it averages one [39]. Both approaches assume the independent effect of SNPs, a reasonable assumption based on an evaluation of 2-way interactions for breast cancer in Caucasian women [40]. Our Bayesian approach reflects the traditional method for combining information from diagnostic tests [41, 42]. In practice, we found that the Bayesian approach and the approach using ORs yield very similar results with these parameters.
Our results should be interpreted with caution since this was a single-center study with lower representation of black and Hispanic patients relative to the U.S. population. Women who perceived themselves as higher risk may have been more likely to consent to provide a blood sample, and it is possible that the baseline risk among study participants differs from that of the general population. Compared to previous descriptions of the BCSC cohort, controls were noted to have slightly higher breast density and were more likely to have a family history of breast cancer [43].
In addition, future analyses should evaluate the performance of race/ethnicity-specific PRS in non-Caucasian populations. The association between the PRS and various breast cancer phenotypes should be validated. Case–case studies have found that higher PRS is positively associated with good prognosis cancers [44, 45]. Our study was not adequately powered to explore subsets of breast cancer.
The USPSTF recommends the consideration of chemoprevention in women with 5-year risk ≥3 % [3]. The PRS reclassifies more women to this higher risk category when added to the BCSC model. One promising area of study involves using the PRS to identify women who would benefit from chemoprevention, since it is unknown whether a high PRS is predictive of benefit from tamoxifen. Although the PRS has been assessed in high-risk women enrolled in two large tamoxifen prevention trials [46], there are no comparative data on the PRS in women who received placebo, and the relative benefit of tamoxifen in women with high polygenic risk remains undetermined.
The PRS may also identify women who might benefit from intensive screening. The American Cancer Society recommends that women with >20–25 % lifetime risk consider screening with MRI [2]. Our study did not project lifetime risk since the BCSC model has only been calibrated for 5- and 10-year risk, though women in the top percentile based on PRS alone have >25 % lifetime risk and women in the top 5th percentile have >20 % risk [21]. Prospective studies are needed to determine whether more intensive screening for high-risk women based on PRS and other risk factors prevents breast cancer morbidity and mortality.
One approach that is currently being studied involves using the combined BCSC-PRS risk estimate to guide screening strategies depending on whether an individual’s 5-year risk exceeds certain thresholds. For instance, women aged 40–49 whose risk equals or exceeds that of an average 50-year-old may be recommended to begin screening immediately rather than defer to age 50. In those without known genetic mutations, polygenic risk may identify additional women whose genetic risk is comparable to that of moderate or high-penetrance mutation carriers. Adjunctive MRI screening may be considered for those at high polygenic risk, analogous to existing guidelines for mutation carriers [47]. A prospective trial on this approach is already underway [48].
In summary, the polygenic risk score is an independent predictor of breast cancer risk that may improve identification of high-risk women in both Caucasian and East Asians. The declining cost and increasing accessibility of genetic-based assays may make it possible to use the PRS with other models to risk-stratify women. The PRS deserves further study on its role in guiding both screening and prevention efforts, and the screening trial currently underway should address its utility, both alone and in combination with other risk factors, to impact clinical outcomes.
Abbreviations
- AUROC:
-
Area under the receiver operating characteristic curve
- BCSC:
-
Breast Cancer Surveillance Consortium
- BIRADS:
-
Breast Imaging Reporting and Data System
- BMI:
-
Body mass index
- CCR:
-
California Cancer Registry
- CPMC:
-
California Pacific Medical Center
- GWAS:
-
Genome-wide association study
- LR:
-
Likelihood ratio
- OR:
-
Odds ratio
- PRS:
-
Polygenic risk score
- SFMR:
-
San Francisco Mammography Registry
- SNPs:
-
Single nucleotide polymorphisms
References
Cummings SR, Tice JA, Bauer S, Browner WS, Cuzick J, Ziv E, Vogel V, Shepherd J, Vachon C, Smith-Bindman R, Kerlikowske K (2009) Prevention of breast cancer in postmenopausal women: approaches to estimating and reducing risk. J Natl Cancer Inst 101(6):384–398. doi:10.1093/jnci/djp018
Saslow D, Boetes C, Burke W, Harms S, Leach MO, Lehman CD, Morris E, Pisano E, Schnall M, Sener S, Smith RA, Warner E, Yaffe M, Andrews KS, Russell CA (2007) American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin 57(2):75–89
Moyer VA (2013) Medications to decrease the risk for breast cancer in women: recommendations from the U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 159(10):698–708. doi:10.7326/0003-4819-159-10-201311190-00717
Schousboe JT, Kerlikowske K, Loh A, Cummings SR (2011) Personalizing mammography by breast density and other risk factors for breast cancer: analysis of health benefits and cost-effectiveness. Ann Intern Med 155(1):10–20. doi:10.7326/0003-4819-155-1-201107050-00003
Shieh Y, Eklund M, Sawaya GF, Black WC, Kramer BS, Esserman LJ (2016) Population-based screening for cancer: hope and hype. Nat Rev Clin Oncol. doi:10.1038/nrclinonc.2016.50
Gail MH, Brinton LA, Byar DP, Corle DK, Green SB, Schairer C, Mulvihill JJ (1989) Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst 81(24):1879–1886
Tyrer J, Duffy SW, Cuzick J (2004) A breast cancer prediction model incorporating familial and personal risk factors. Stat Med 23(7):1111–1130. doi:10.1002/sim.1668
Tice JA, Cummings SR, Smith-Bindman R, Ichikawa L, Barlow WE, Kerlikowske K (2008) Using clinical factors and mammographic breast density to estimate breast cancer risk: development and validation of a new predictive model. Ann Intern Med 148(5):337–347
Tice JA, Miglioretti DL, Li CS, Vachon CM, Gard CC, Kerlikowske K (2015) Breast density and benign breast disease: risk assessment to identify women at high risk of breast cancer. J Clin Oncol 33(28):3137–3147. doi:10.1200/jco.2015.60.8869
Cai Q, Zhang B, Sung H, Low SK, Kweon SS, Lu W, Shi J, Long J, Wen W, Choi JY, Noh DY, Shen CY, Matsuo K, Teo SH, Kim MK, Khoo US, Iwasaki M, Hartman M, Takahashi A, Ashikawa K, Matsuda K, Shin MH, Park MH, Zheng Y, Xiang YB, Ji BT, Park SK, Wu PE, Hsiung CN, Ito H, Kasuga Y, Kang P, Mariapun S, Ahn SH, Kang HS, Chan KY, Man EP, Iwata H, Tsugane S, Miao H, Liao J, Nakamura Y, Kubo M, Delahanty RJ, Zhang Y, Li B, Li C, Gao YT, Shu XO, Kang D, Zheng W (2014) Genome-wide association analysis in East Asians identifies breast cancer susceptibility loci at 1q32.1, 5q14.3 and 15q26.1. Nat Genet 46(8):886–890. doi:10.1038/ng.3041
Fejerman L, Ahmadiyeh N, Hu D, Huntsman S, Beckman KB, Caswell JL, Tsung K, John EM, Torres-Mejia G, Carvajal-Carmona L, Echeverry MM, Tuazon AM, Ramirez C, Gignoux CR, Eng C, Gonzalez-Burchard E, Henderson B, Le Marchand L, Kooperberg C, Hou L, Agalliu I, Kraft P, Lindstrom S, Perez-Stable EJ, Haiman CA, Ziv E (2014) Genome-wide association study of breast cancer in Latinas identifies novel protective variants on 6q25. Nat Commun 5:5260. doi:10.1038/ncomms6260
Ahsan H, Halpern J, Kibriya MG, Pierce BL, Tong L, Gamazon E, McGuire V, Felberg A, Shi J, Jasmine F, Roy S, Brutus R, Argos M, Melkonian S, Chang-Claude J, Andrulis I, Hopper JL, John EM, Malone K, Ursin G, Gammon MD, Thomas DC, Seminara D, Casey G, Knight JA, Southey MC, Giles GG, Santella RM, Lee E, Conti D, Duggan D, Gallinger S, Haile R, Jenkins M, Lindor NM, Newcomb P, Michailidou K, Apicella C, Park DJ, Peto J, Fletcher O, dos Santos Silva I, Lathrop M, Hunter DJ, Chanock SJ, Meindl A, Schmutzler RK, Muller-Myhsok B, Lochmann M, Beckmann L, Hein R, Makalic E, Schmidt DF, Bui QM, Stone J, Flesch-Janys D, Dahmen N, Nevanlinna H, Aittomaki K, Blomqvist C, Hall P, Czene K, Irwanto A, Liu J, Rahman N, Turnbull C, Dunning AM, Pharoah P, Waisfisz Q, Meijers-Heijboer H, Uitterlinden AG, Rivadeneira F, Nicolae D, Easton DF, Cox NJ, Whittemore AS (2014) A genome-wide association study of early-onset breast cancer identifies PFKM as a novel breast cancer gene and supports a common genetic spectrum for breast cancer at any age. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol 23(4):658–669. doi:10.1158/1055-9965.epi-13-0340
Fletcher O, Johnson N, Orr N, Hosking FJ, Gibson LJ, Walker K, Zelenika D, Gut I, Heath S, Palles C, Coupland B, Broderick P, Schoemaker M, Jones M, Williamson J, Chilcott-Burns S, Tomczyk K, Simpson G, Jacobs KB, Chanock SJ, Hunter DJ, Tomlinson IP, Swerdlow A, Ashworth A, Ross G, dos Santos Silva I, Lathrop M, Houlston RS, Peto J (2011) Novel breast cancer susceptibility locus at 9q31.2: results of a genome-wide association study. J Natl Cancer Inst 103(5):425–435
Garcia-Closas M, Couch FJ, Lindstrom S, Michailidou K, Schmidt MK, Brook MN, Orr N, Rhie SK, Riboli E, Feigelson HS, Le Marchand L, Buring JE, Eccles D, Miron P, Fasching PA, Brauch H, Chang-Claude J, Carpenter J, Godwin AK, Nevanlinna H, Giles GG, Cox A, Hopper JL, Bolla MK, Wang Q, Dennis J, Dicks E, Howat WJ, Schoof N, Bojesen SE, Lambrechts D, Broeks A, Andrulis IL, Guenel P, Burwinkel B, Sawyer EJ, Hollestelle A, Fletcher O, Winqvist R, Brenner H, Mannermaa A, Hamann U, Meindl A, Lindblom A, Zheng W, Devillee P, Goldberg MS, Lubinski J, Kristensen V, Swerdlow A, Anton-Culver H, Dork T, Muir K, Matsuo K, Wu AH, Radice P, Teo SH, Shu XO, Blot W, Kang D, Hartman M, Sangrajrang S, Shen CY, Southey MC, Park DJ, Hammet F, Stone J, Veer LJ, Rutgers EJ, Lophatananon A, Stewart-Brown S, Siriwanarangsan P, Peto J, Schrauder MG, Ekici AB, Beckmann MW, Dos Santos Silva I, Johnson N, Warren H, Tomlinson I, Kerin MJ, Miller N, Marme F, Schneeweiss A, Sohn C, Truong T, Laurent-Puig P, Kerbrat P, Nordestgaard BG, Nielsen SF, Flyger H, Milne RL, Perez JI, Menendez P, Muller H, Arndt V, Stegmaier C, Lichtner P, Lochmann M, Justenhoven C, Ko YD, Muranen TA, Aittomaki K, Blomqvist C, Greco D, Heikkinen T, Ito H, Iwata H, Yatabe Y, Antonenkova NN, Margolin S, Kataja V, Kosma VM, Hartikainen JM, Balleine R, Tseng CC, Berg DV, Stram DO, Neven P, Dieudonne AS, Leunen K, Rudolph A, Nickels S, Flesch-Janys D, Peterlongo P, Peissel B, Bernard L, Olson JE, Wang X, Stevens K, Severi G, Baglietto L, McLean C, Coetzee GA, Feng Y, Henderson BE, Schumacher F, Bogdanova NV, Labreche F, Dumont M, Yip CH, Taib NA, Cheng CY, Shrubsole M, Long J, Pylkas K, Jukkola-Vuorinen A, Kauppila S, Knight JA, Glendon G, Mulligan AM, Tollenaar RA, Seynaeve CM, Kriege M, Hooning MJ, van den Ouweland AM, van Deurzen CH, Lu W, Gao YT, Cai H, Balasubramanian SP, Cross SS, Reed MW, Signorello L, Cai Q, Shah M, Miao H, Chan CW, Chia KS, Jakubowska A, Jaworska K, Durda K, Hsiung CN, Wu PE, Yu JC, Ashworth A, Jones M, Tessier DC, Gonzalez-Neira A, Pita G, Alonso MR, Vincent D, Bacot F, Ambrosone CB, Bandera EV, John EM, Chen GK, Hu JJ, Rodriguez-Gil JL, Bernstein L, Press MF, Ziegler RG, Millikan RM, Deming-Halverson SL, Nyante S, Ingles SA, Waisfisz Q, Tsimiklis H, Makalic E, Schmidt D, Bui M, Gibson L, Muller-Myhsok B, Schmutzler RK, Hein R, Dahmen N, Beckmann L, Aaltonen K, Czene K, Irwanto A, Liu J, Turnbull C, Rahman N, Meijers-Heijboer H, Uitterlinden AG, Rivadeneira F, Olswold C, Slager S, Pilarski R, Ademuyiwa F, Konstantopoulou I, Martin NG, Montgomery GW, Slamon DJ, Rauh C, Lux MP, Jud SM, Bruning T, Weaver J, Sharma P, Pathak H, Tapper W, Gerty S, Durcan L, Trichopoulos D, Tumino R, Peeters PH, Kaaks R, Campa D, Canzian F, Weiderpass E, Johansson M, Khaw KT, Travis R, Clavel-Chapelon F, Kolonel LN, Chen C, Beck A, Hankinson SE, Berg CD, Hoover RN, Lissowska J, Figueroa JD, Chasman DI, Gaudet MM, Diver WR, Willett WC, Hunter DJ, Simard J, Benitez J, Dunning AM, Sherman ME, Chenevix-Trench G, Chanock SJ, Hall P, Pharoah PD, Vachon C, Easton DF, Haiman CA, Kraft P (2013) Genome-wide association studies identify four ER negative-specific breast cancer risk loci. Nat Genet 45(4):392–398, 398e391–392. doi:10.1038/ng.2561
Long J, Cai Q, Sung H, Shi J, Zhang B, Choi JY, Wen W, Delahanty RJ, Lu W, Gao YT, Shen H, Park SK, Chen K, Shen CY, Ren Z, Haiman CA, Matsuo K, Kim MK, Khoo US, Iwasaki M, Zheng Y, Xiang YB, Gu K, Rothman N, Wang W, Hu Z, Liu Y, Yoo KY, Noh DY, Han BG, Lee MH, Zheng H, Zhang L, Wu PE, Shieh YL, Chan SY, Wang S, Xie X, Kim SW, Henderson BE, Le Marchand L, Ito H, Kasuga Y, Ahn SH, Kang HS, Chan KY, Iwata H, Tsugane S, Li C, Shu XO, Kang DH, Zheng W (2012) Genome-wide association study in east Asians identifies novel susceptibility loci for breast cancer. PLoS Genet 8(2):e1002532. doi:10.1371/journal.pgen.1002532
Low SK, Takahashi A, Ashikawa K, Inazawa J, Miki Y, Kubo M, Nakamura Y, Katagiri T (2013) Genome-wide association study of breast cancer in the Japanese population. PLoS One 8(10):e76463. doi:10.1371/journal.pone.0076463
Siddiq A, Couch FJ, Chen GK, Lindstrom S, Eccles D, Millikan RC, Michailidou K, Stram DO, Beckmann L, Rhie SK, Ambrosone CB, Aittomaki K, Amiano P, Apicella C, Baglietto L, Bandera EV, Beckmann MW, Berg CD, Bernstein L, Blomqvist C, Brauch H, Brinton L, Bui QM, Buring JE, Buys SS, Campa D, Carpenter JE, Chasman DI, Chang-Claude J, Chen C, Clavel-Chapelon F, Cox A, Cross SS, Czene K, Deming SL, Diasio RB, Diver WR, Dunning AM, Durcan L, Ekici AB, Fasching PA, Feigelson HS, Fejerman L, Figueroa JD, Fletcher O, Flesch-Janys D, Gaudet MM, Gerty SM, Rodriguez-Gil JL, Giles GG, van Gils CH, Godwin AK, Graham N, Greco D, Hall P, Hankinson SE, Hartmann A, Hein R, Heinz J, Hoover RN, Hopper JL, Hu JJ, Huntsman S, Ingles SA, Irwanto A, Isaacs C, Jacobs KB, John EM, Justenhoven C, Kaaks R, Kolonel LN, Coetzee GA, Lathrop M, Le Marchand L, Lee AM, Lee IM, Lesnick T, Lichtner P, Liu J, Lund E, Makalic E, Martin NG, McLean CA, Meijers-Heijboer H, Meindl A, Miron P, Monroe KR, Montgomery GW, Muller-Myhsok B, Nickels S, Nyante SJ, Olswold C, Overvad K, Palli D, Park DJ, Palmer JR, Pathak H, Peto J, Pharoah P, Rahman N, Rivadeneira F, Schmidt DF, Schmutzler RK, Slager S, Southey MC, Stevens KN, Sinn HP, Press MF, Ross E, Riboli E, Ridker PM, Schumacher FR, Severi G, Dos Santos Silva I, Stone J, Sund M, Tapper WJ, Thun MJ, Travis RC, Turnbull C, Uitterlinden AG, Waisfisz Q, Wang X, Wang Z, Weaver J, Schulz-Wendtland R, Wilkens LR, Van Den Berg D, Zheng W, Ziegler RG, Ziv E, Nevanlinna H, Easton DF, Hunter DJ, Henderson BE, Chanock SJ, Garcia-Closas M, Kraft P, Haiman CA, Vachon CM (2012) A meta-analysis of genome-wide association studies of breast cancer identifies two novel susceptibility loci at 6q14 and 20q11. Hum Mol Genet 21(24):5373–5384. doi:10.1093/hmg/dds381
Zheng W, Zhang B, Cai Q, Sung H, Michailidou K, Shi J, Choi JY, Long J, Dennis J, Humphreys MK, Wang Q, Lu W, Gao YT, Li C, Cai H, Park SK, Yoo KY, Noh DY, Han W, Dunning AM, Benitez J, Vincent D, Bacot F, Tessier D, Kim SW, Lee MH, Lee JW, Lee JY, Xiang YB, Zheng Y, Wang W, Ji BT, Matsuo K, Ito H, Iwata H, Tanaka H, Wu AH, Tseng CC, Van Den Berg D, Stram DO, Teo SH, Yip CH, Kang IN, Wong TY, Shen CY, Yu JC, Huang CS, Hou MF, Hartman M, Miao H, Lee SC, Putti TC, Muir K, Lophatananon A, Stewart-Brown S, Siriwanarangsan P, Sangrajrang S, Shen H, Chen K, Wu PE, Ren Z, Haiman CA, Sueta A, Kim MK, Khoo US, Iwasaki M, Pharoah PD, Wen W, Hall P, Shu XO, Easton DF, Kang D (2013) Common genetic determinants of breast-cancer risk in East Asian women: a collaborative study of 23 637 breast cancer cases and 25 579 controls. Hum Mol Genet 22(12):2539–2550. doi:10.1093/hmg/ddt089
Michailidou K, Hall P, Gonzalez-Neira A, Ghoussaini M, Dennis J, Milne RL, Schmidt MK, Chang-Claude J, Bojesen SE, Bolla MK, Wang Q, Dicks E, Lee A, Turnbull C, Rahman N, Fletcher O, Peto J, Gibson L, Dos Santos Silva I, Nevanlinna H, Muranen TA, Aittomaki K, Blomqvist C, Czene K, Irwanto A, Liu J, Waisfisz Q, Meijers-Heijboer H, Adank M, van der Luijt RB, Hein R, Dahmen N, Beckman L, Meindl A, Schmutzler RK, Muller-Myhsok B, Lichtner P, Hopper JL, Southey MC, Makalic E, Schmidt DF, Uitterlinden AG, Hofman A, Hunter DJ, Chanock SJ, Vincent D, Bacot F, Tessier DC, Canisius S, Wessels LF, Haiman CA, Shah M, Luben R, Brown J, Luccarini C, Schoof N, Humphreys K, Li J, Nordestgaard BG, Nielsen SF, Flyger H, Couch FJ, Wang X, Vachon C, Stevens KN, Lambrechts D, Moisse M, Paridaens R, Christiaens MR, Rudolph A, Nickels S, Flesch-Janys D, Johnson N, Aitken Z, Aaltonen K, Heikkinen T, Broeks A, Veer LJ, van der Schoot CE, Guenel P, Truong T, Laurent-Puig P, Menegaux F, Marme F, Schneeweiss A, Sohn C, Burwinkel B, Zamora MP, Perez JI, Pita G, Alonso MR, Cox A, Brock IW, Cross SS, Reed MW, Sawyer EJ, Tomlinson I, Kerin MJ, Miller N, Henderson BE, Schumacher F, Le Marchand L, Andrulis IL, Knight JA, Glendon G, Mulligan AM, Lindblom A, Margolin S, Hooning MJ, Hollestelle A, van den Ouweland AM, Jager A, Bui QM, Stone J, Dite GS, Apicella C, Tsimiklis H, Giles GG, Severi G, Baglietto L, Fasching PA, Haeberle L, Ekici AB, Beckmann MW, Brenner H, Muller H, Arndt V, Stegmaier C, Swerdlow A, Ashworth A, Orr N, Jones M, Figueroa J, Lissowska J, Brinton L, Goldberg MS, Labreche F, Dumont M, Winqvist R, Pylkas K, Jukkola-Vuorinen A, Grip M, Brauch H, Hamann U, Bruning T, Radice P, Peterlongo P, Manoukian S, Bonanni B, Devilee P, Tollenaar RA, Seynaeve C, van Asperen CJ, Jakubowska A, Lubinski J, Jaworska K, Durda K, Mannermaa A, Kataja V, Kosma VM, Hartikainen JM, Bogdanova NV, Antonenkova NN, Dork T, Kristensen VN, Anton-Culver H, Slager S, Toland AE, Edge S, Fostira F, Kang D, Yoo KY, Noh DY, Matsuo K, Ito H, Iwata H, Sueta A, Wu AH, Tseng CC, Van Den Berg D, Stram DO, Shu XO, Lu W, Gao YT, Cai H, Teo SH, Yip CH, Phuah SY, Cornes BK, Hartman M, Miao H, Lim WY, Sng JH, Muir K, Lophatananon A, Stewart-Brown S, Siriwanarangsan P, Shen CY, Hsiung CN, Wu PE, Ding SL, Sangrajrang S, Gaborieau V, Brennan P, McKay J, Blot WJ, Signorello LB, Cai Q, Zheng W, Deming-Halverson S, Shrubsole M, Long J, Simard J, Garcia-Closas M, Pharoah PD, Chenevix-Trench G, Dunning AM, Benitez J, Easton DF (2013) Large-scale genotyping identifies 41 new loci associated with breast cancer risk. Nat Genet 45(4):353–361, 361e351–352. doi:10.1038/ng.2563
Michailidou K, Beesley J, Lindstrom S, Canisius S, Dennis J, Lush MJ, Maranian MJ, Bolla MK, Wang Q, Shah M, Perkins BJ, Czene K, Eriksson M, Darabi H, Brand JS, Bojesen SE, Nordestgaard BG, Flyger H, Nielsen SF, Rahman N, Turnbull C, Fletcher O, Peto J, Gibson L, dos-Santos-Silva I, Chang-Claude J, Flesch-Janys D, Rudolph A, Eilber U, Behrens S, Nevanlinna H, Muranen TA, Aittomaki K, Blomqvist C, Khan S, Aaltonen K, Ahsan H, Kibriya MG, Whittemore AS, John EM, Malone KE, Gammon MD, Santella RM, Ursin G, Makalic E, Schmidt DF, Casey G, Hunter DJ, Gapstur SM, Gaudet MM, Diver WR, Haiman CA, Schumacher F, Henderson BE, Le Marchand L, Berg CD, Chanock SJ, Figueroa J, Hoover RN, Lambrechts D, Neven P, Wildiers H, van Limbergen E, Schmidt MK, Broeks A, Verhoef S, Cornelissen S, Couch FJ, Olson JE, Hallberg E, Vachon C, Waisfisz Q, Meijers-Heijboer H, Adank MA, van der Luijt RB, Li J, Liu J, Humphreys K, Kang D, Choi JY, Park SK, Yoo KY, Matsuo K, Ito H, Iwata H, Tajima K, Guenel P, Truong T, Mulot C, Sanchez M, Burwinkel B, Marme F, Surowy H, Sohn C, Wu AH, Tseng CC, Van Den Berg D, Stram DO, Gonzalez-Neira A, Benitez J, Zamora MP, Perez JI, Shu XO, Lu W, Gao YT, Cai H, Cox A, Cross SS, Reed MW, Andrulis IL, Knight JA, Glendon G, Mulligan AM, Sawyer EJ, Tomlinson I, Kerin MJ, Miller N, Lindblom A, Margolin S, Teo SH, Yip CH, Taib NA, Tan GH, Hooning MJ, Hollestelle A, Martens JW, Collee JM, Blot W, Signorello LB, Cai Q, Hopper JL, Southey MC, Tsimiklis H, Apicella C, Shen CY, Hsiung CN, Wu PE, Hou MF, Kristensen VN, Nord S, Alnaes GI, Giles GG, Milne RL, McLean C, Canzian F, Trichopoulos D, Peeters P, Lund E, Sund M, Khaw KT, Gunter MJ, Palli D, Mortensen LM, Dossus L, Huerta JM, Meindl A, Schmutzler RK, Sutter C, Yang R, Muir K, Lophatananon A, Stewart-Brown S, Siriwanarangsan P, Hartman M, Miao H, Chia KS, Chan CW, Fasching PA, Hein A, Beckmann MW, Haeberle L, Brenner H, Dieffenbach AK, Arndt V, Stegmaier C, Ashworth A, Orr N, Schoemaker MJ, Swerdlow AJ, Brinton L, Garcia-Closas M, Zheng W, Halverson SL, Shrubsole M, Long J, Goldberg MS, Labreche F, Dumont M, Winqvist R, Pylkas K, Jukkola-Vuorinen A, Grip M, Brauch H, Hamann U, Bruning T, Radice P, Peterlongo P, Manoukian S, Bernard L, Bogdanova NV, Dork T, Mannermaa A, Kataja V, Kosma VM, Hartikainen JM, Devilee P, Tollenaar RA, Seynaeve C, Van Asperen CJ, Jakubowska A, Lubinski J, Jaworska K, Huzarski T, Sangrajrang S, Gaborieau V, Brennan P, McKay J, Slager S, Toland AE, Ambrosone CB, Yannoukakos D, Kabisch M, Torres D, Neuhausen SL, Anton-Culver H, Luccarini C, Baynes C, Ahmed S, Healey CS, Tessier DC, Vincent D, Bacot F, Pita G, Alonso MR, Alvarez N, Herrero D, Simard J, Pharoah PP, Kraft P, Dunning AM, Chenevix-Trench G, Hall P, Easton DF (2015) Genome-wide association analysis of more than 120,000 individuals identifies 15 new susceptibility loci for breast cancer. Nat Genet 47(4):373–380. doi:10.1038/ng.3242
Mavaddat N, Pharoah PDP, Michailidou K, Tyrer J, Brook MN, Bolla MK, Wang Q, Dennis J, Dunning AM, Shah M, Luben R, Brown J, Bojesen SE, Nordestgaard BG, Nielsen SF, Flyger H, Czene K, Darabi H, Eriksson M, Peto J, dos-Santos-Silva I, Dudbridge F, Johnson N, Schmidt MK, Broeks A, Verhoef S, Rutgers EJ, Swerdlow A, Ashworth A, Orr N, Schoemaker MJ, Figueroa J, Chanock SJ, Brinton L, Lissowska J, Couch FJ, Olson JE, Vachon C, Pankratz VS, Lambrechts D, Wildiers H, Van Ongeval C, van Limbergen E, Kristensen V, Grenaker Alnæs G, Nord S, Borresen-Dale A-L, Nevanlinna H, Muranen TA, Aittomäki K, Blomqvist C, Chang-Claude J, Rudolph A, Seibold P, Flesch-Janys D, Fasching PA, Haeberle L, Ekici AB, Beckmann MW, Burwinkel B, Marme F, Schneeweiss A, Sohn C, Trentham-Dietz A, Newcomb P, Titus L, Egan KM, Hunter DJ, Lindstrom S, Tamimi RM, Kraft P, Rahman N, Turnbull C, Renwick A, Seal S, Li J, Liu J, Humphreys K, Benitez J, Pilar Zamora M, Arias Perez JI, Menéndez P, Jakubowska A, Lubinski J, Jaworska-Bieniek K, Durda K, Bogdanova NV, Antonenkova NN, Dörk T, Anton-Culver H, Neuhausen SL, Ziogas A, Bernstein L, Devilee P, Tollenaar RAEM, Seynaeve C, van Asperen CJ, Cox A, Cross SS, Reed MWR, Khusnutdinova E, Bermisheva M, Prokofyeva D, Takhirova Z, Meindl A, Schmutzler RK, Sutter C, Yang R, Schürmann P, Bremer M, Christiansen H, Park-Simon T-W, Hillemanns P, Guénel P, Truong T, Menegaux F, Sanchez M, Radice P, Peterlongo P, Manoukian S, Pensotti V, Hopper JL, Tsimiklis H, Apicella C, Southey MC, Brauch H, Brüning T, Ko Y-D, Sigurdson AJ, Doody MM, Hamann U, Torres D, Ulmer H-U, Försti A, Sawyer EJ, Tomlinson I, Kerin MJ, Miller N, Andrulis IL, Knight JA, Glendon G, Marie Mulligan A, Chenevix-Trench G, Balleine R, Giles GG, Milne RL, McLean C, Lindblom A, Margolin S, Haiman CA, Henderson BE, Schumacher F, Le Marchand L, Eilber U, Wang-Gohrke S, Hooning MJ, Hollestelle A, van den Ouweland AMW, Koppert LB, Carpenter J, Clarke C, Scott R, Mannermaa A, Kataja V, Kosma V-M, Hartikainen JM, Brenner H, Arndt V, Stegmaier C, Karina Dieffenbach A, Winqvist R, Pylkäs K, Jukkola-Vuorinen A, Grip M, Offit K, Vijai J, Robson M, Rau-Murthy R, Dwek M, Swann R, Annie Perkins K, Goldberg MS, Labrèche F, Dumont M, Eccles DM, Tapper WJ, Rafiq S, John EM, Whittemore AS, Slager S, Yannoukakos D, Toland AE, Yao S, Zheng W, Halverson SL, González-Neira A, Pita G, Rosario Alonso M, Álvarez N, Herrero D, Tessier DC, Vincent D, Bacot F, Luccarini C, Baynes C, Ahmed S, Maranian M, Healey CS, Simard J, Hall P, Easton DF, Garcia-Closas M (2015) Prediction of breast cancer risk based on profiling with common genetic variants. J Natl Cancer Inst 107(5). doi:10.1093/jnci/djv036
Vachon CM, Pankratz VS, Scott CG, Haeberle L, Ziv E, Jensen MR, Brandt KR, Whaley DH, Olson JE, Heusinger K, Hack CC, Jud SM, Beckmann MW, Schulz-Wendtland R, Tice JA, Norman AD, Cunningham JM, Purrington KS, Easton DF, Sellers TA, Kerlikowske K, Fasching PA, Couch FJ (2015) The contributions of breast density and common genetic variation to breast cancer risk. J Natl Cancer Inst 107(5). doi:10.1093/jnci/dju397
Dite GS, MacInnis RJ, Bickerstaffe A, Dowty JG, Allman R, Apicella C, Milne RL, Tsimiklis H, Phillips KA, Giles GG, Terry MB, Southey MC, Hopper JL (2016) Breast cancer risk prediction using clinical models and 77 independent risk-associated SNPS for women aged under 50 years: Australian Breast Cancer Family Registry. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol 25(2):359–365. doi:10.1158/1055-9965.epi-15-0838
Purrington KS, Slager S, Eccles D, Yannoukakos D, Fasching PA, Miron P, Carpenter J, Chang-Claude J, Martin NG, Montgomery GW, Kristensen V, Anton-Culver H, Goodfellow P, Tapper WJ, Rafiq S, Gerty SM, Durcan L, Konstantopoulou I, Fostira F, Vratimos A, Apostolou P, Konstanta I, Kotoula V, Lakis S, Dimopoulos MA, Skarlos D, Pectasides D, Fountzilas G, Beckmann MW, Hein A, Ruebner M, Ekici AB, Hartmann A, Schulz-Wendtland R, Renner SP, Janni W, Rack B, Scholz C, Neugebauer J, Andergassen U, Lux MP, Haeberle L, Clarke C, Pathmanathan N, Rudolph A, Flesch-Janys D, Nickels S, Olson JE, Ingle JN, Olswold C, Slettedahl S, Eckel-Passow JE, Anderson SK, Visscher DW, Cafourek VL, Sicotte H, Prodduturi N, Weiderpass E, Bernstein L, Ziogas A, Ivanovich J, Giles GG, Baglietto L, Southey M, Kosma VM, Fischer HP, Reed MW, Cross SS, Deming-Halverson S, Shrubsole M, Cai Q, Shu XO, Daly M, Weaver J, Ross E, Klemp J, Sharma P, Torres D, Rudiger T, Wolfing H, Ulmer HU, Forsti A, Khoury T, Kumar S, Pilarski R, Shapiro CL, Greco D, Heikkila P, Aittomaki K, Blomqvist C, Irwanto A, Liu J, Pankratz VS, Wang X, Severi G, Mannermaa A, Easton D, Hall P, Brauch H, Cox A, Zheng W, Godwin AK, Hamann U, Ambrosone C, Toland AE, Nevanlinna H, Vachon CM, Couch FJ (2014) Genome-wide association study identifies 25 known breast cancer susceptibility loci as risk factors for triple-negative breast cancer. Carcinogenesis 35(5):1012–1019. doi:10.1093/carcin/bgt404
Couch FJ, Wang X, McGuffog L, Lee A, Olswold C, Kuchenbaecker KB, Soucy P, Fredericksen Z, Barrowdale D, Dennis J, Gaudet MM, Dicks E, Kosel M, Healey S, Sinilnikova OM, Lee A, Bacot F, Vincent D, Hogervorst FB, Peock S, Stoppa-Lyonnet D, Jakubowska A, Radice P, Schmutzler RK, Domchek SM, Piedmonte M, Singer CF, Friedman E, Thomassen M, Hansen TV, Neuhausen SL, Szabo CI, Blanco I, Greene MH, Karlan BY, Garber J, Phelan CM, Weitzel JN, Montagna M, Olah E, Andrulis IL, Godwin AK, Yannoukakos D, Goldgar DE, Caldes T, Nevanlinna H, Osorio A, Terry MB, Daly MB, van Rensburg EJ, Hamann U, Ramus SJ, Toland AE, Caligo MA, Olopade OI, Tung N, Claes K, Beattie MS, Southey MC, Imyanitov EN, Tischkowitz M, Janavicius R, John EM, Kwong A, Diez O, Balmana J, Barkardottir RB, Arun BK, Rennert G, Teo SH, Ganz PA, Campbell I, van der Hout AH, van Deurzen CH, Seynaeve C, Gomez Garcia EB, van Leeuwen FE, Meijers-Heijboer HE, Gille JJ, Ausems MG, Blok MJ, Ligtenberg MJ, Rookus MA, Devilee P, Verhoef S, van Os TA, Wijnen JT, Frost D, Ellis S, Fineberg E, Platte R, Evans DG, Izatt L, Eeles RA, Adlard J, Eccles DM, Cook J, Brewer C, Douglas F, Hodgson S, Morrison PJ, Side LE, Donaldson A, Houghton C, Rogers MT, Dorkins H, Eason J, Gregory H, McCann E, Murray A, Calender A, Hardouin A, Berthet P, Delnatte C, Nogues C, Lasset C, Houdayer C, Leroux D, Rouleau E, Prieur F, Damiola F, Sobol H, Coupier I, Venat-Bouvet L, Castera L, Gauthier-Villars M, Leone M, Pujol P, Mazoyer S, Bignon YJ, Zlowocka-Perlowska E, Gronwald J, Lubinski J, Durda K, Jaworska K, Huzarski T, Spurdle AB, Viel A, Peissel B, Bonanni B, Melloni G, Ottini L, Papi L, Varesco L, Tibiletti MG, Peterlongo P, Volorio S, Manoukian S, Pensotti V, Arnold N, Engel C, Deissler H, Gadzicki D, Gehrig A, Kast K, Rhiem K, Meindl A, Niederacher D, Ditsch N, Plendl H, Preisler-Adams S, Engert S, Sutter C, Varon-Mateeva R, Wappenschmidt B, Weber BH, Arver B, Stenmark-Askmalm M, Loman N, Rosenquist R, Einbeigi Z, Nathanson KL, Rebbeck TR, Blank SV, Cohn DE, Rodriguez GC, Small L, Friedlander M, Bae-Jump VL, Fink-Retter A, Rappaport C, Gschwantler-Kaulich D, Pfeiler G, Tea MK, Lindor NM, Kaufman B, Shimon Paluch S, Laitman Y, Skytte AB, Gerdes AM, Pedersen IS, Moeller ST, Kruse TA, Jensen UB, Vijai J, Sarrel K, Robson M, Kauff N, Mulligan AM, Glendon G, Ozcelik H, Ejlertsen B, Nielsen FC, Jonson L, Andersen MK, Ding YC, Steele L, Foretova L, Teule A, Lazaro C, Brunet J, Pujana MA, Mai PL, Loud JT, Walsh C, Lester J, Orsulic S, Narod SA, Herzog J, Sand SR, Tognazzo S, Agata S, Vaszko T, Weaver J, Stavropoulou AV, Buys SS, Romero A, de la Hoya M, Aittomaki K, Muranen TA, Duran M, Chung WK, Lasa A, Dorfling CM, Miron A, Benitez J, Senter L, Huo D, Chan SB, Sokolenko AP, Chiquette J, Tihomirova L, Friebel TM, Agnarsson BA, Lu KH, Lejbkowicz F, James PA, Hall P, Dunning AM, Tessier D, Cunningham J, Slager SL, Wang C, Hart S, Stevens K, Simard J, Pastinen T, Pankratz VS, Offit K, Easton DF, Chenevix-Trench G, Antoniou AC (2013) Genome-wide association study in BRCA1 mutation carriers identifies novel loci associated with breast and ovarian cancer risk. PLoS Genet 9(3):e1003212. doi:10.1371/journal.pgen.1003212
Turnbull C, Ahmed S, Morrison J, Pernet D, Renwick A, Maranian M, Seal S, Ghoussaini M, Hines S, Healey CS, Hughes D, Warren-Perry M, Tapper W, Eccles D, Evans DG, Hooning M, Schutte M, van den Ouweland A, Houlston R, Ross G, Langford C, Pharoah PD, Stratton MR, Dunning AM, Rahman N, Easton DF (2010) Genome-wide association study identifies five new breast cancer susceptibility loci. Nat Genet 42(6):504–507. doi:10.1038/ng.586
Burdett T, Hall P, Hasting E, Hindorff L, Junkins A, Klemm A, MacArthur J, Manolio T, Morales J, Parkinson H, Welter D (2015) The NHGRI-EBI catalog of published genome-wide association studies. https://www.ebi.ac.uk/gwas/home
Flicek P, Amode MR, Barrell D, Beal K, Billis K, Brent S, Carvalho-Silva D, Clapham P, Coates G, Fitzgerald S, Gil L, Girón CG, Gordon L, Hourlier T, Hunt S, Johnson N, Juettemann T, Kähäri AK, Keenan S, Kulesha E, Martin FJ, Maurel T, McLaren WM, Murphy DN, Nag R, Overduin B, Pignatelli M, Pritchard B, Pritchard E, Riat HS, Ruffier M, Sheppard D, Taylor K, Thormann A, Trevanion SJ, Vullo A, Wilder SP, Wilson M, Zadissa A, Aken BL, Birney E, Cunningham F, Harrow J, Herrero J, Hubbard TJP, Kinsella R, Muffato M, Parker A, Spudich G, Yates A, Zerbino DR, Searle SMJ (2014) Ensembl 2014. Nucleic Acids Res 42(D1):D749–D755. doi:10.1093/nar/gkt1196
Lu Q, Elston RC (2008) Using the optimal receiver operating characteristic curve to design a predictive genetic test, exemplified with type 2 diabetes. Am J Hum Genet 82(3):641–651. doi:10.1016/j.ajhg.2007.12.025
Boyd NF, Guo H, Martin LJ, Sun L, Stone J, Fishell E, Jong RA, Hislop G, Chiarelli A, Minkin S (2007) Mammographic density and the risk and detection of breast cancer. N Engl J Med 356(3):227–236
Sickles EA, C.J. DO, L.W. B (2013) Mammography. In: ACR BI-RADS® Atlas, Breast Imaging Reporting and Data System. American College of Radiology, Reston, VA
Hosmer DW, Lemeshow SA, Sturdivant RX (2013) Applied logistic regression, 3rd edn. Wiley, Hoboken
Boyd NF, Martin LJ, Sun L, Guo H, Chiarelli A, Hislop G, Yaffe M, Minkin S (2006) Body size, mammographic density, and breast cancer risk. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol 15(11):2086–2092. doi:10.1158/1055-9965.epi-06-0345
National Cancer Institute (2015) Surveillance, epidemiology, and end results (SEER) program populations (1969–2013). http://www.seer.cancer.gov/popdata
Sawyer S, Mitchell G, McKinley J, Chenevix-Trench G, Beesley J, Chen XQ, Bowtell D, Trainer AH, Harris M, Lindeman GJ, James PA (2012) A role for common genomic variants in the assessment of familial breast cancer. J Clin Oncol 30(35):4330–4336. doi:10.1200/JCO.2012.41.7469
Lindstrom S, Thompson DJ, Paterson AD, Li J, Gierach GL, Scott C, Stone J, Douglas JA, dos-Santos-Silva I, Fernandez-Navarro P, Verghase J, Smith P, Brown J, Luben R, Wareham NJ, Loos RJ, Heit JA, Pankratz VS, Norman A, Goode EL, Cunningham JM, deAndrade M, Vierkant RA, Czene K, Fasching PA, Baglietto L, Southey MC, Giles GG, Shah KP, Chan HP, Helvie MA, Beck AH, Knoblauch NW, Hazra A, Hunter DJ, Kraft P, Pollan M, Figueroa JD, Couch FJ, Hopper JL, Hall P, Easton DF, Boyd NF, Vachon CM, Tamimi RM (2014) Genome-wide association study identifies multiple loci associated with both mammographic density and breast cancer risk. Nat Commun 5:5303. doi:10.1038/ncomms6303
Brand JS, Li J, Humphreys K, Karlsson R, Eriksson M, Ivansson E, Hall P, Czene K (2015) Identification of two novel mammographic density loci at 6Q25.1. Breast Cancer Res 17:75. doi:10.1186/s13058-015-0591-2
Padhukasahasram B, Halperin E, Wessel J, Thomas DJ, Silver E, Trumbower H, Cargill M, Stephan DA (2010) Presymptomatic risk assessment for chronic non-communicable diseases. PLoS One 5(12). doi:10.1371/journal.pone.0014338
Mealiffe ME, Stokowski RP, Rhees BK, Prentice RL, Pettinger M, Hinds DA (2010) Assessment of clinical validity of a breast cancer risk model combining genetic and clinical information. J Natl Cancer Inst 102(21):1618–1627. doi:10.1093/jnci/djq388
Milne RL, Herranz J, Michailidou K, Dennis J, Tyrer JP, Zamora MP, Arias-Perez JI, Gonzalez-Neira A, Pita G, Alonso MR, Wang Q, Bolla MK, Czene K, Eriksson M, Humphreys K, Darabi H, Li J, Anton-Culver H, Neuhausen SL, Ziogas A, Clarke CA, Hopper JL, Dite GS, Apicella C, Southey MC, Chenevix-Trench G, Swerdlow A, Ashworth A, Orr N, Schoemaker M, Jakubowska A, Lubinski J, Jaworska-Bieniek K, Durda K, Andrulis IL, Knight JA, Glendon G, Mulligan AM, Bojesen SE, Nordestgaard BG, Flyger H, Nevanlinna H, Muranen TA, Aittomaki K, Blomqvist C, Chang-Claude J, Rudolph A, Seibold P, Flesch-Janys D, Wang X, Olson JE, Vachon C, Purrington K, Winqvist R, Pylkas K, Jukkola-Vuorinen A, Grip M, Dunning AM, Shah M, Guenel P, Truong T, Sanchez M, Mulot C, Brenner H, Dieffenbach AK, Arndt V, Stegmaier C, Lindblom A, Margolin S, Hooning MJ, Hollestelle A, Collee JM, Jager A, Cox A, Brock IW, Reed MW, Devilee P, Tollenaar RA, Seynaeve C, Haiman CA, Henderson BE, Schumacher F, Le Marchand L, Simard J, Dumont M, Soucy P, Dork T, Bogdanova NV, Hamann U, Forsti A, Rudiger T, Ulmer HU, Fasching PA, Haberle L, Ekici AB, Beckmann MW, Fletcher O, Johnson N, dos Santos Silva I, Peto J, Radice P, Peterlongo P, Peissel B, Mariani P, Giles GG, Severi G, Baglietto L, Sawyer E, Tomlinson I, Kerin M, Miller N, Marme F, Burwinkel B, Mannermaa A, Kataja V, Kosma VM, Hartikainen JM, Lambrechts D, Yesilyurt BT, Floris G, Leunen K, Alnaes GG, Kristensen V, Borresen-Dale AL, Garcia-Closas M, Chanock SJ, Lissowska J, Figueroa JD, Schmidt MK, Broeks A, Verhoef S, Rutgers EJ, Brauch H, Bruning T, Ko YD, Couch FJ, Toland AE, Yannoukakos D, Pharoah PD, Hall P, Benitez J, Malats N, Easton DF (2014) A large-scale assessment of two-way SNP interactions in breast cancer susceptibility using 46,450 cases and 42,461 controls from the breast cancer association consortium. Hum Mol Genet 23(7):1934–1946. doi:10.1093/hmg/ddt581
Grimes DA, Schulz KF (2005) Refining clinical diagnosis with likelihood ratios. Lancet (London, England) 365(9469):1500–1505. doi:10.1016/s0140-6736(05)66422-7
Gill CJ, Sabin L, Schmid CH (2005) Why clinicians are natural bayesians. BMJ 330(7499):1080–1083. doi:10.1136/bmj.330.7499.1080
Kerlikowske K, Zhu W, Tosteson AN, Sprague BL, Tice JA, Lehman CD, Miglioretti DL (2015) Identifying women with dense breasts at high risk for interval cancer: a cohort study. Ann Intern Med 162:673–681. doi:10.7326/m14-1465
Holm J, Li J, Darabi H, Eklund M, Eriksson M, Humphreys K, Hall P, Czene K (2016) Associations of breast cancer risk prediction tools with tumor characteristics and metastasis. J Clin Oncol Off J Am Soc Clin Oncol 34(3):251–258. doi:10.1200/jco.2015.63.0624
Li J, Holm J, Bergh J, Eriksson M, Darabi H, Lindstrom LS, Tornberg S, Hall P, Czene K (2015) Breast cancer genetic risk profile is differentially associated with interval and screen-detected breast cancers. Ann Oncol 26(3):517–522. doi:10.1093/annonc/mdu565
Vachon CM, Schaid DJ, Ingle JN, Wickerham DL, Kubo M, Mushiroda T, Goetz MP, Carlson EE, Paik S, Wolmark N, Nakamura Y, Wang L, Weinshilboum R, Couch FJ (2015) A polygenic risk score for breast cancer in women receiving tamoxifen or raloxifene on NSABP P-1 and P-2. Breast Cancer Res Treat 149(2):517–523. doi:10.1007/s10549-014-3175-4
Daly MB, Pilarski R, Axilbund JE, Berry M, Buys SS, Crawford B, Farmer M, Friedman S, Garber JE, Khan S, Klein C, Kohlmann W, Kurian A, Litton JK, Madlensky L, Marcom PK, Merajver SD, Offit K, Pal T, Rana H, Reiser G, Robson ME, Shannon KM, Swisher E, Voian NC, Weitzel JN, Whelan A, Wick MJ, Wiesner GL, Dwyer M, Kumar R, Darlow S (2016) Genetic/familial high-risk assessment: breast and ovarian, version 2.2015. J Natl Compr Cancer Netw JNCCN 14(2):153–162
Wisdom: About the Study [online], https://wisdom.secure.force.com/portal/WsdSiteStudy (2015)
Acknowledgments
We are grateful to Sarah D. Sawyer, PhD for her assistance with the polygenic risk score. The collection of cancer data was supported in part by the California Cancer Registry. For a full description, please see: http://breastscreening.cancer.gov/work/acknowledgement.html. We thank the participating women, mammography facilities, and radiologists for the data they have provided for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
K. Kerlikowske received support for the Breast Cancer Surveillance Consortium from the National Cancer Institute, grant P01 CA154292. E. Ziv received support from the National Cancer Institute under grant K24 CA169004. S.R. Cummings received support for the collection of blood specimens from the DaCosta Fund for the Prevention of Breast Cancer, the Clinical Research in Clinical Care (CRCLE) funds provided by the California Pacific Medical Center, and by a grant from the Eli Lilly Foundation. Y. Shieh was supported by a National Research Service Award through the National Institutes of Health T32 HP19025. Data collection for this work was supported by the National Cancer Institute-funded Breast Cancer Surveillance Consortium (HHSN261201100031C). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
Conflict of interest
Dr. Jessica Leung receives consultation fees from Hologic, Inc. related to the development of contrast-enhanced mammography.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Specifically, each registry in the Breast Cancer Surveillance Consortium and the Statistical Coordinating Center (SCC) have received institutional review board approval for either active or passive consenting processes or a waiver of consent to enroll participants, link data, and perform analytic studies. All procedures are Health Insurance Portability and Accountability Act (HIPAA) compliant and all registries and the SCC have received a Federal Certificate of Confidentiality and other protection for the identities of women, physicians, and facilities who are subjects of this research.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Drs. Kerlikowske and Ziv are co-senior authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shieh, Y., Hu, D., Ma, L. et al. Breast cancer risk prediction using a clinical risk model and polygenic risk score. Breast Cancer Res Treat 159, 513–525 (2016). https://doi.org/10.1007/s10549-016-3953-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-016-3953-2