Abstract
The risk of breast cancer is at least two-fold increased in young women with a family history of breast cancer. Pregnancy has a dual effect on breast cancer risk; a short-term increase followed by a long-term protection. We investigated if the risk of breast cancer during and within 10 years following pregnancy is affected by a family history of breast cancer. We followed a cohort of women aged 15–44 years between 1963 and 2009 identified in Swedish population-based registers. Family history was defined as having a mother or sister with breast cancer. We estimated incidence rate ratios of breast cancer during pregnancy and time intervals up to 10 years post-delivery, with a focus on pregnancy-associated breast cancer (PABC), defined as breast cancer during pregnancy or within 2 years post-delivery. In 3,452,506 women, there were 15,548 cases of breast cancer (1208 were PABC). Compared to nulliparous women, the risk of breast cancer was decreased during pregnancy, similar during first year and increased during second year post-delivery. The pattern was similar in women with or without family history of breast cancer. A peak in risk was observed 5–6 years following the first birth regardless of family history. After a second birth, this peak was only present in women with a family history. Our results indicate that women with a family history of breast cancer do not have a different breast cancer risk during and within 10 years following pregnancy compared to women without a family history.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The risk of breast cancer is at least two-fold increased in young women with a family history of breast cancer, with an even stronger influence on risk in young women where a first-degree relative was diagnosed with breast cancer at an early age (below 50 years) [1, 2]. Women with a genetic predisposition for breast cancer may be more likely to harbor pre-malignant cells at younger ages and could be particularly susceptible to physiological changes during childbearing, especially during a first pregnancy [3].
The risk of breast cancer varies substantially close to childbirth, with a decreased risk during pregnancy and an increased risk around 1 year post-delivery, possibly reflecting diagnostic delays or pregnancy-related growth promotion of pre-clinical malignancies [4]. Thus, it cannot be excluded that a family history of breast cancer may influence this risk pattern. We are only aware of one study that has included the pregnancy period in the assessment of breast cancer risk in women with a family history [5]. This study found evidence of a three-fold increased risk associated with family history both during childbearing and within 2 years following delivery, a time window commonly used to denote pregnancy-associated breast cancer (PABC).
The effects of a pregnancy on breast cancer risk are likely to persist beyond 2 years and several investigators have observed a transiently increased risk of breast cancer with a peak around 5–10 years following delivery [6–11]. It has been proposed that breast cancers occurring during pregnancy or lactation have different biological properties from those occurring 5–10 years post-delivery [12]. At least four studies have investigated the possible role of family history in relation to breast cancer risk more than 2 years after delivery [5, 13–15]. Although the overall findings from these studies indicate that family history does not alter the transient risk pattern following childbirth, there are subgroup findings of interest. In line with a suggested important role of the first pregnancy [3], Wohlfahrt et al. [13] found some, albeit weak, evidence that the transient risk increase was restricted to uniparous women with a family history of breast cancer. However, these studies have differed in methodological approach and two studies used broad 5-year intervals which precluded a detailed assessment of the risk pattern [13, 15].
We used information available in population-based Swedish registers to investigate if the effect of pregnancy on breast cancer risk is modified by a family history of breast cancer. We restricted the analysis to pre-menopausal women with a focus on PABC and breast cancer risk up to 10 years after childbirth.
Methods
In this population-based cohort study, we linked several Swedish national population registers using the personal identity number (PIN) assigned to all Swedish residents. Within the Swedish Multi-Generation Register (MGR), which links all persons born after 1932 and alive in 1961 to their parents, we established a cohort of women aged 15–44 years and residing in Sweden between 1963 and 2009. Data retrieved from the MGR provided information on dates of live childbirths for each woman, allowing assessment of risktime periods around a delivery. Information from the Swedish Cancer Register (SCR) was individually linked to each woman using the PIN. Since 1958, the SCR records all newly diagnosed tumors in Sweden, and includes date of diagnosis and tumor location based on the International Classification of Disease (ICD) versions 7 and later. In order to create a cohort free of cancer at start of follow-up, women with a cancer diagnosis prior to age 15 were excluded.
In a subsequent step, we retrieved information on first emigration after age 15 from the Migration Register and date of death from the Cause of Death Register and the Total Population Register. Further, we obtained information on the highest achieved educational level from the Education Register.
Breast cancer and family history
Cases were defined as first occurrence of a malignant breast cancer during follow-up (ICD version 7: 170, patho-anatomical diagnosis (PAD) code: 096). By linking information in the MGR and the SCR, we were able to obtain information on family history of breast cancer in biological mothers and sisters to the women in the cohort. We defined family history as having a first-degree relative (mother or sister) with breast cancer at any age, and young familial onset as having a mother or a sister with breast cancer diagnosed before age 50 (old familial onset if both mother and sisters were diagnosed after age 50). Mean age at diagnosis was 60 years for mothers and 52 years for sisters.
Risktime and case-cohort design
Women were followed from entry to the cohort (at age 15 or in 1963) until first occurrence of breast cancer or censoring at date of diagnosis of another cancer, death, 45th birthday, first emigration, or at the end of follow-up in 2009, whichever came first. To simplify the analysis, only women who had four or fewer children were included (women with five or more children were censored 9 months prior to the fifth birth). More than 95 % of all breast cancers in the cohort occurred in women of parity less than 5. The final cohort for analysis comprised 3,452,506 women.
To enable fine adjustment for age, each woman’s follow-up time was split on attained age in 1-year intervals. Similarly, calendar time was split into intervals 1963–1969, 1970–1979, 1980–1989, 1990–1999, and 2000–2009. Furthermore, the risktime of parous women was split by parity into uniparous, biparous, triparous, and quadriparous timebands. These timebands were further split by time-since-pregnancy, including the pregnancy period (defined as nine months prior to delivery date of a liveborn child) and 1-year periods following delivery (first year post-delivery, second year post-delivery, up to 10th year post-delivery, and 10+ years post-delivery). Time-since-latest-pregnancy was coded as a time-varying exposure variable: a woman who had her second pregnancy 2 years after her first delivery changed status to “pregnant” 9 months prior to her second birth, so that time-since-latest-pregnancy represented the time from the start of the second pregnancy. Parity was coded as a time-varying exposure variable in a similar way, i.e., parity status was increased by 1 at 9 months prior to delivery of an additional child (the pregnancy period contributed to the assigned parity status).
For reasons of computational efficiency due to the massive amount of time splitting, we generated a case-cohort sample from the full cohort. We randomly selected a subcohort of 2 % of the women in the full cohort at start of follow-up, and also included all breast cancer cases occurring outside the subcohort. The total case-cohort sample included 83,800 women, of which 15,548 were cases (335 inside the subcohort, 15,213 outside the subcohort) and 68,252 were non-cases inside the subcohort. To account for the sampling in the statistical analysis, each woman’s risktime was weighted according to her case-cohort sampling probability using inverse probability weighting [16]. For non-cases, the weights were calculated as one over the sampling fraction of non-cases. For cases, the weights were set to 1, since all women with breast cancer were sampled. The weighted analysis yielded inference for the full cohort which gave rise to all the cases.
Statistical methods
We estimated incidence rate ratios (IRR) with 95 % confidence intervals (CI) using weighted Poisson regression models, including the case-cohort weights in the likelihood of the model, with robust standard errors [17]. The models were adjusted for attained age (by applying a restricted cubic spline), and for attained period and education (both in categories). Since 8.7 % of the women lacked information on education, the adjusted models are based on fewer observations than the overall numbers reported in Table 1.
First, we modeled the interaction between family history and time-since-latest-pregnancy, while adjusting for age, period, and education (Tables 2, 3). The IRRs by time-since-latest-pregnancy are presented separately for women with or without family history. In addition, we also present the ratio between the IRR (with family history) and the IRR (without family history) in each interval corresponding to the log of the interaction parameter for that interval (which is a Wald test of the interaction). Second, to adjust for parity, we assessed the effect of time-since-latest-pregnancy in women having an additional birth compared to those not having that additional birth, separately for women with or without family history. This approach has been proposed previously [9, 13] and compares the risk between women of a given parity to other women with similar reproductive history except for the latest childbirth, i.e., the excess risk associated with having an additional child. Hence, we assessed the effect of family history by time-since-first-pregnancy compared to nulliparous, by time-since-second-pregnancy compared to uniparous, and by time-since-third-pregnancy compared to biparous women (Table 4). The model also included adjustment for age at first birth, which because of collinearity with time-since-latest-pregnancy and attained age was estimable only in women with two or more children. The significance level was 5 % and all tests were two-sided.
Data preparations were done in SAS (version 9.3) and the statistical modeling in Stata (version 12.1). The study was approved by the Ethical Review Board at Karolinska Institutet, Sweden.
Results
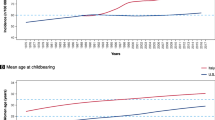
Among 3,452,506 women aged 15–44 years and residing in Sweden from 1963 to 2009, we identified 15,548 breast cancers in women with at most four children. As expected, the breast cancer incidence increased with age and calendar time (Table 1). Among women with breast cancer, the proportion with a family history of breast cancer was 14.5 %, and 4.8 % had a mother or sister with onset of disease below 50 years. Compared to women without a family history of breast cancer, women with a family history had a two-fold higher rate of breast cancer (adjusted IRR = 2.04, 95 % CI 1.92–2.16). If the woman had a relative with onset of breast cancer below 50 years, the rate was three times higher (IRR = 3.00, 95 % CI 2.70–3.34).
A total of 1208 women had PABC, while 5569 women were diagnosed with breast cancer between 2 and 10 years post-delivery. The proportion of PABC cases with a family history was 13.3 %, while 14.0 % of cases diagnosed between 2 and 10 years had a family history. Compared to nulliparous women, the rate of breast cancer was reduced during pregnancy following adjustment for age, period, and education. There was a modestly increased rate of breast cancer during the second year and 5–6 years following the most recent birth, compared to nulliparous women.
Risk during pregnancy and within 2 years post-delivery (PABC)
In women without a family history, the incidence rate of breast cancer was more than halved during pregnancy compared to nulliparous women (adjusted IRR = 0.36, 95 % CI 0.30–0.45) (Table 2). A similar pattern was observed in women with a family history (adjusted IRR = 0.39, 95 % CI 0.24–0.65; test of interaction: IRR ratio with vs without family history = 1.08; 95 % CI 0.63–1.85).
In women without a family history, there was some evidence of a lower incidence during the first year post-delivery compared to nulliparous women (IRR = 0.92, 95 % CI 0.82–1.03), while the rate was slightly increased during the second year after childbirth (IRR = 1.18, 95 % CI 1.07–1.30) (Table 2). In women with a family history, the pattern was similar (IRR = 0.78, 95 % CI 0.57–1.06 for the first year and IRR = 1.27; 0.99–1.62 for the second year, respectively). In each time window, there was no difference in IRR between women with or without family history (test of interaction: 0.85 (95 % CI 0.61–1.18) during the first year; 1.07 (0.82–1.40) during the second year).
Early age at onset of the relative’s breast cancer did not influence the incidence during pregnancy or the first year post-delivery differently compared to women without family history (Table 3). However, during the second year post-delivery, the increase in incidence compared to nulliparous was most pronounced among women with a familial onset below age 50 (IRR = 1.53; 95 % CI 1.02–2.28); the incidence was not increased in women with a familial onset above 50 years (IRR = 1.08, 95 % CI 0.78–1.49); and only modestly increased in women without family history (IRR = 1.18; 95 % CI 1.07–1.30).
Following stratification by parity, a reduced incidence rate during pregnancy was present after the first, second, and third pregnancy regardless of family history status (Table 4). An increased incidence rate within the second year post-delivery was present after first and second childbirth for women without a family history (IRR = 1.28, 95 % CI 1.07–1.53; IRR = 1.25, 95 % CI 1.09–1.43, respectively). For women with a family history, an increased incidence rate was only present after the second childbirth (IRR = 1.52, 95 % CI 1.08–2.12), although point estimates were slightly, but not statistically significantly, increased also after the first and third pregnancy. The IRRs for each time window were not statistically different when comparing women with versus without family history (test of interaction).
Risk after 2 and before 10 years post-delivery
In women without a family history, the breast cancer risk was modestly and transiently increased with a peak in incidence rate 5–6 years following delivery compared to nulliparous (IRR = 1.09, 95 % CI 1.01–1.18) (Table 2). A similar transient increase in risk was observed in women with a family history (IRR = 1.11, 95 % CI 0.91–1.35 at 5–6 years post-delivery). Age at onset of familial breast cancer did not affect the shape or size of the transient risk within 10 years post-delivery (Table 3).
Stratifying by parity, the transient risk beyond 2 years post-delivery was most pronounced following the first birth with around 40 % increased incidence at 5–6 years after delivery (IRR = 1.44, 95 % CI 1.25–1.66 without family history; IRR = 1.43 (1.00–2.05) with family history) (Table 4). In women with a family history, the risk was also increased at 5–6 years following the second birth (IRR = 1.36, 95 % CI 1.07–1.72), but no transient risk increase was detected after the third birth. For women without a family history, the transient risk was much less pronounced and not significant after the second or third birth (with the possible exception of an increase at 3–4 years post-delivery following third birth). The IRRs in each time window were not significantly different in women with or without family history (test of interaction).
In a sensitivity analysis, the analysis was restricted to women at risk after 1990 or later (including 56 % of the breast cancer cases) and yielded results similar to those for the full period.
Discussion
Taken together our findings indicate that a family history of breast cancer neither modifies the risk of PABC, nor the pattern of risk up to 10 years post-delivery. The risk of breast cancer was much lower than expected during pregnancy, a finding that was consistent over family history and parity status. Further, while no increased risk of breast cancer during the first year post-delivery was observed, there was evidence of an increased risk of breast cancer during the second year post-delivery. This finding was also consistent when assessed by family history, with the possible exception of a stronger effect during the second year post-delivery in women with a family history of early age onset breast cancer.
Beyond 2 years post-delivery there was a peak in the risk around 5–6 years, which was most pronounced following the first birth with a more than 40 % increase in breast cancer incidence both in women with or without a family history. The transient risk increase was less pronounced after the second and not detectable after the third birth in women without a family history, while there was some evidence of a transient risk after the second birth in women with a family history, but not following a third birth.
This is the first study that has examined breast cancer risk by family history in narrow time windows around delivery, separating the pregnancy period from the first and second years post-delivery. In contrast to our finding of similar risk pattern for women with and without family history around delivery, Hou et al. [5] found some evidence of a risk-modifying influence of family history in women diagnosed during pregnancy and within 2 years following delivery. Hou et al. also reported a higher proportion of BRCA1/BRCA2 carriers (25 %) among women with PABC, compared to women diagnosed more than 5 years post-delivery (11.5 %). The parameterization used by Hou et al. precluded detailed assessment of the shape of the transient risk increase following pregnancy.
There are several possible explanations for our finding of a lower incidence of breast cancer during pregnancy and the rebound observed shortly after delivery [4]. These include factors related to detection, such as patient’s and doctor’s delay, and a lower diagnostic intensity during childbearing. Other possible contributing factors are true lower (during pregnancy) or higher (post-delivery) risks, due to physiological changes associated with childbearing. Such changes include exposure to increased levels of pregnancy hormones, immunological changes, and alterations in the tissue microenvironment of the breast following post-lactation involution that may promote the growth of pre-clinical malignant cells [18]. A lower incidence during pregnancy may also reflect under-ascertainment of cases during pregnancy due to spontaneous or induced abortions.
Our finding that family history does not modify the transient risk between 2 and 10 years post-delivery (including among uniparous women) is not in line with findings by Wohlfahrt et al. who observed a weak transient risk within 5 years post-delivery restricted to uniparous women with a family history [13]. While Wohlfahrt et al. found no increased risk following the second or higher order births, we found a possible increase after the second birth in women with family history. Albrektsen et al. reported an increased transient risk among women with a family history, but the comparison group was nulliparous women without family history [14]. Hence, the time-since-birth effect reported was a mix of time-since-birth and family history, and is likely to be primarily driven by family history which is the stronger effect of the two.
Based on a similar Swedish dataset, Hemminki et al. found no apparent effect of family history on the pattern of short-term risk following delivery [15]. However, the authors made comparisons between women of same parity and used broad 5 years post-delivery intervals limiting the possibility to examine time-since-pregnancy in detail.
Strengths of the present study included the use of one of the largest databases to date where the effect of family history on breast cancer risk around pregnancy can be investigated. The population-based setting using information from nationwide registers provided high quality data on reproductive history and family history, and a virtually complete follow-up.
Unlike earlier studies, we included the pregnancy window in the analysis since risks during pregnancy may be driven by mechanisms different than those further away from delivery. Similar to Wohlfahrt et al. [13], we compared women with the same parity and age at first birth with or without an additional childbirth. This approach is likely to better capture the effect of time-since-pregnancy than a comparison to nulliparous women which rather reflects the combined effect of time-since-pregnancy and parity [14]. Also, a comparison between women of same parity would make the comparison group too similar and precludes assessment of any risk increase attributable to an additional pregnancy [15]. In contrast to previous studies, we assessed the pregnancy window separately and thus excluded it from being counted as risktime in a previous pregnancy, which could alter estimates when comparing different parities. Also, a comparison of women with and without an additional birth, allowed for adjustment of possible carry-over effects between subsequent pregnancies.
Several limitations of the present study need to be acknowledged. Firstly, despite the large dataset at hand, the lack of power in some of the analyses hampered the possibilities to draw firm conclusions. Only about 8 % of all pre-menopausal breast cancers occurred during pregnancy or within 2 years following delivery. Corroborating earlier estimates, the proportion of breast cancer cases with a family history was 14.5 % in our cohort [1, 19]. Since no data were available on induced abortions, miscarriages, or stillbirths, only pregnancies resulting in a live birth were included in the analyses. While we were able to identify first-degree relatives using register information, we cannot exclude that some breast cancers in relatives were not captured since information in the SCR was restricted to cases identified from the start of the SCR (1958). However, adjustment for period and age should minimize cohort and period effects. A sensitivity analysis showed that the overall results were similar to those in women diagnosed after 1990.
No information was available as to whether a breast cancer case was detected by screening or not. While invitational mammography screening was broadly introduced in Sweden in the 1990s, it was not until recently all Swedish regions included women from 40 years of age in outreach screening programmes [20, 21]. Also, the data at hand did not include information on TNM stage at presentation, or BRCA1/BRCA2 status.
In conclusion, our results indicate that the risk of breast cancer during and within 10 years following pregnancy appears to be unrelated to family history of breast cancer, i.e., genetic factors or shared familial factors. Hence, this study does not support the hypothesis that a recent pregnancy increases the risk of breast cancer to a higher extent in women with family history of breast cancer.
References
Collaborative Group on Hormonal Factors in Breast C (2001) Familial breast cancer: collaborative reanalysis of individual data from 52 epidemiological studies including 58,209 women with breast cancer and 101,986 women without the disease. Lancet 358(9291):1389–1399. doi:10.1016/S0140-6736(01)06524-2
Pharoah PD, Day NE, Duffy S, Easton DF, Ponder BA (1997) Family history and the risk of breast cancer: a systematic review and meta-analysis. Int J Cancer 71(5):800–809
Colditz GA, Rosner BA, Speizer FE (1996) Risk factors for breast cancer according to family history of breast cancer. For the Nurses’ Health Study Research Group. J Natl Cancer Inst 88(6):365–371
Andersson TM, Johansson AL, Fredriksson I, Lambe M (2015) Cancer during pregnancy and the postpartum period: a population-based study. Cancer. doi:10.1002/cncr.29325
Hou N, Ogundiran T, Ojengbede O, Morhason-Bello I, Zheng Y, Fackenthal J, Adebamowo C, Anetor I, Akinleye S, Olopade OI, Huo D (2013) Risk factors for pregnancy-associated breast cancer: a report from the Nigerian Breast Cancer Study. Ann Epidemiol 23(9):551–557. doi:10.1016/j.annepidem.2013.06.008
Bruzzi P, Negri E, La Vecchia C, Decarli A, Palli D, Parazzini F, Del Turco MR (1988) Short term increase in risk of breast cancer after full term pregnancy. BMJ 297(6656):1096–1098
Lambe M, Hsieh C, Trichopoulos D, Ekbom A, Pavia M, Adami HO (1994) Transient increase in the risk of breast cancer after giving birth. N Engl J Med 331(1):5–9. doi:10.1056/NEJM199407073310102
Leon DA, Carpenter LM, Broeders MJ, Gunnarskog J, Murphy MF (1995) Breast cancer in Swedish women before age 50: evidence of a dual effect of completed pregnancy. Cancer Causes Control 6(4):283–291
Wohlfahrt J, Andersen PK, Mouridsen HT, Melbye M (2001) Risk of late-stage breast cancer after a childbirth. Am J Epidemiol 153(11):1079–1084
Liu Q, Wuu J, Lambe M, Hsieh SF, Ekbom A, Hsieh CC (2002) Transient increase in breast cancer risk after giving birth: postpartum period with the highest risk (Sweden). Cancer Causes Control 13(4):299–305
Albrektsen G, Heuch I, Hansen S, Kvale G (2005) Breast cancer risk by age at birth, time since birth and time intervals between births: exploring interaction effects. Br J Cancer 92(1):167–175. doi:10.1038/sj.bjc.6602302
Borges VF, Schedin PJ (2012) Pregnancy-associated breast cancer: an entity needing refinement of the definition. Cancer 118(13):3226–3228. doi:10.1002/cncr.26643
Wohlfahrt J, Olsen JH, Melby M (2002) Breast cancer risk after childbirth in young women with family history (Denmark). Cancer Causes Control 13(2):169–174
Albrektsen G, Heuch I, Thoresen S, Kvale G (2006) Family history of breast cancer and short-term effects of childbirths on breast cancer risk. Int J Cancer 119(6):1468–1474. doi:10.1002/ijc.22003
Hemminki K, Forsti A, Sundquist J, Ji J (2008) Risk of familial breast cancer is not increased after pregnancy. Breast Cancer Res Treat 108(3):417–420. doi:10.1007/s10549-007-9611-y
Klein JP, van Houwelingen HC, Ibrahim JG, Scheike TH (2013) Handbook of survival analysis. Chapman and Hall/CRC Press, Boca Raton
Moger TA, Pawitan Y, Borgan O (2008) Case-cohort methods for survival data on families from routine registers. Stat Med 27(7):1062–1074. doi:10.1002/sim.3004
Schedin P (2006) Pregnancy-associated breast cancer and metastasis. Nat Rev Cancer 6(4):281–291
Schwab FD, Burki N, Huang DJ, Heinzelmann-Schwarz V, Schmid SM, Vetter M, Schotzau A, Guth U (2014) Impact of breast cancer family history on tumor detection and tumor size in women newly-diagnosed with invasive breast cancer. Fam Cancer 13(1):99–107. doi:10.1007/s10689-013-9682-3
Hellquist BN, Duffy SW, Nystrom L, Jonsson H (2012) Overdiagnosis in the population-based service screening programme with mammography for women aged 40–49 years in Sweden. J Med Screen 19(1):14–19. doi:10.1258/jms.2012.011104
Socialstyrelsen, Sweden. Mammography screening guidelines. http://www.socialstyrelsen.se/riktlinjer/nationellascreeningprogram/brostcancer-screeningmedmammog/. Accessed 11 March 2015
Acknowledgments
This work was supported by a grant from Susan G. Komen for the Cure (Grant number KG 100116).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the Ethical Review Board at Karolinska Institutet, Sweden. For this type of study formal consent is not required.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Johansson, A.L.V., Andersson, T.ML., Hsieh, CC. et al. Family history and risk of pregnancy-associated breast cancer (PABC). Breast Cancer Res Treat 151, 209–217 (2015). https://doi.org/10.1007/s10549-015-3369-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-015-3369-4