Abstract
The PI3K pathway is a key mechanism of trastuzumab resistance, but early attempts to indirectly target this pathway with mTOR inhibitors have had limited success. We present the results of a preclinical study of the selective alpha/delta isoform dominant PI3K inhibitor BAY 80-6946 tested alone and in combination with HER2-targeted therapies in HER2-positive cell lines, including models with acquired resistance to trastuzumab and/or lapatinib. A panel of HER2-positive breast cancer cells were profiled for their mutational status using Sequenom MassARRAY, PTEN status by Western blot, and anti-proliferative response to BAY 80-6946 alone and in combination with the HER2-targeted therapies trastuzumab, lapatinib and afatinib. Reverse phase protein array was used to determine the effect of BAY 80-6946 on expression and phosphorylation of 68 proteins including members of the PI3K and MAPK pathways. The Boyden chamber method was used to determine if BAY 80-6946 affected cellular invasion and migration. BAY 80-6946 has anti-proliferative and anti-invasive effects when used alone in our panel of cell lines (IC50s 3.9–29.4 nM). BAY 80-6946 inhibited PI3K signalling and was effective in cells regardless of their PI3K, P53 or PTEN status. The combination of HER2-targeted therapies and BAY 80-6946 inhibited growth more effectively than either therapy used alone (with clear synergism in many cases), and can restore sensitivity to trastuzumab and lapatinib in cells with acquired resistance to either trastuzumab and/or lapatinib. The addition of BAY 80-6946 to HER2-targeted therapy could represent an improved treatment strategy for patients with refractory metastatic HER2-positive breast cancer, and should be considered for clinical trial evaluation.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
HER2-positive breast cancer accounts for 15–20 % of all breast cancers and is associated with shorter time to progression and decreased overall survival [1]. Trastuzumab, a monoclonal antibody targeted to HER2, has significantly improved outcomes in both the adjuvant and metastatic settings [2], but resistance to trastuzumab remains a problem. Lapatinib, a small molecule tyrosine kinase inhibitor (TKI) against HER2 and EGFR, currently in use as a second-line therapy in patients who have progressed on trastuzumab therapy [3], is effective in some patients who acquire resistance to trastuzumab. However, the efficacy of lapatinib is also limited by the development of acquired resistance.
The phosphatidylinositol-3-kinase (PI3K) pathway, a major signalling mediator in cancer [4] is activated downstream of HER2. This pathway has been strongly implicated as a mediator of trastuzumab resistance in breast cancer [5, 6] and has recently been associated with lapatinib resistance [7, 8]. Preclinical data suggest that targeting a PI3K signalling node called mammalian target of rapamycin (mTOR), in combination with HER2-inhibition could overcome HER2-positive breast cancer resistance to HER2-targeted therapy [4]. However, the clinical efficacy of mTOR inhibitors in HER2-positive breast cancer has been disappointing [9], likely in part due to inhibition of mTOR activating a feedback loop which up regulates PI3K activity, thereby attenuating the anti-tumour efficacy of mTOR inhibitors [10].
We believe that directly targeting PI3K can overcome the limitation of feedback activation mediated by mTOR inhibition. BAY 80-6946 a novel, potent, highly selective PI3K inhibitor [11–14], able to induce apoptosis in vitro [11], was well tolerated in a Phase I clinical trial [15]. In the study presented here, we show that the novel PI3K inhibitor, BAY 80-6946, potently inhibited the growth of five HER2-positive cell lines and five HER2-positive lines with acquired trastuzumab/lapatinib resistance. We found that the combination of BAY 80-6946 and HER2-targeted therapies more effectively inhibited cell growth than either therapy used alone, with clear synergism in many cases, and that the addition of the PI3K inhibitor could restore sensitivity to HER2-targeted therapies in cells with acquired resistance to trastuzumab and lapatinib.
Materials and methods
Cell culture
Human HER2-positive breast cancer cell lines were obtained from the National Institute for Cellular Biotechnology (NICB), Dublin City University, and the Division of Haematology/Oncology, University of California, Los Angeles (UCLA). Resistant variants were developed by continuous growth in the relevant drug (SKBR3-T (NICB): 10 µg/ml trastuzumab; SKBR3-L (NICB): 250 nM lapatinib; SKBR3-TL (NICB): 5 µg trastuzumab and 150 nM lapatinib; HCC1954-L (NICB): 1,250 nM lapatinib; BT474-Res (UCLA): 100 ug/ml trastuzumab) for 6 months, with drug refreshed twice weekly. All cell lines were grown in RPMI-1640 media (Sigma) supplemented with 10 % FCS and 1 % Penicillin/Streptomycin (P/S) and maintained at 37 °C with 5 % CO2. Cell line identity was confirmed by DNA fingerprinting, which was performed by Source Biosciences™. Cell lines were Mycoplasma tested before and after the in vitro experiments. Trastuzumab (21 mg/ml) was obtained from St James University Hospital and prepared in bacteriostatic water. Lapatinib (10.8 mM) and Afatinib (20.6 mM) were purchased from Sequoia Chemicals and stock solutions prepared in dimethylsulfoxide (DMSO). BAY 80-6946 (10 mM) was obtained under MTA from Bayer Pharmaceuticals and prepared in DMSO and 5 % trifluoroacetic acid (TFA).
Proliferation assays
For all resistant cell lines, drug was removed from the cells at least 7 days prior to starting assays, and no P/S was added to media during proliferation assays. 3 × 104 cells/well were seeded in 96-well plates, apart from BT474 and BT474-Res which were seeded at 5 × 104 cells/well. Plates are incubated overnight at 37 °C to allow cells to adhere. Drugs were added to the plates at specific concentrations and incubated at 37 °C. Following 5-day incubation, during which control cells attained 80–90 % confluence, all media was removed, and plates were washed once with PBS. Proliferation was measured using the acid phosphatase assay as previously described [16].
Invasion and migration assays
Invasion and migration assays were performed using the Boyden chamber method as previously described [16]. After 24 h, the plates were removed from the incubator. Matrigel and media were removed, the insert stained with crystal violet for 10 min, then rinsed three times in distilled water and left to dry at room temperature. Cells were counted at 200× magnification in 10 views from each well, with the average result taken to represent the number of invading/migrating cells in that well.
Protein extraction from cell lines
4.5 × 105 cells were seeded into 6-well plates and left to adhere overnight. Cells were treated with 1 nM BAY-806946 or an equivalent concentration of DMSO-TFA (vehicle control). Protein was extracted 6 and 24 h post treatment as indicated in Supplementary Materials and methods and stored at −80 °C.
Reverse phase protein array analysis
RPPA was carried out as previously described by us [5, 17]. The antibodies used are listed in Supplementary materials and methods. RPPA analysis was carried out using triplicate biological replicates.
DNA extraction and Sequenom MassArray analysis
DNA extraction was performed using an AllPrep™ DNA/RNA Mini Kit (Qiagen) as per manufacturer’s instructions. Mass spectrometry-based genotyping (Sequenom MassARRAY, Sequenom, San Diego, CA) was applied to detect a total of 547 single nucleotide mutations in 49 cancer-related genes, which are listed in Supplementary materials and methods. Reactions where >15 % of the resultant mass ran in the mutant site were scored as positive.
Statistical analysis
IC50 and combination index (CI) values @ effective dose 50 (ED50) were calculated using CalcuSyn software (BioSoft). A CI value of <0.9 is considered synergistic, 0.9–1.1 is considered additive and >1.1 is considered antagonistic. The Student’s t test was used to compare the effect of BAY 80-6946 on invasion and migration, and the effect of BAY 80-6946, lapatinib and the combination of both drug on protein expression and phosphorylation in our RPPA data. A Kruskal–Wallis non-parametric test was performed to compare trastuzumab alone, BAY 80-6946 alone and the combination. p < 0.05 was considered statistically significant.
Results
HER2-positive breast cancer cell lines respond to BAY 80-6946 regardless of their mutational status and response to lapatinib, afatinib or trastuzumab
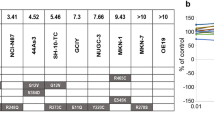
A panel of HER2-positive cell lines including matched models of acquired trastuzumab, lapatinib and combined trastuzumab and lapatinib resistance, was analysed by Sequenom MassArray for somatic mutations in 53 different genes (Table 1). Mutations in the PIK3CA gene were identified in BT474 (K111N), HCC1954 (H1047R) and MDAMB453 (H1047R) cells. The mutational status of PI3K, TP53 or the expression of PTEN did not change between parental cell lines and models of acquired resistance to trastuzumab and/or lapatinib (Table 1).
BAY 80-6946 achieves an IC50 in the panel of cell lines ranging from 3.9 ± 0.8 nM in BT474 to 29.4 ± 4.7 nM in MDAMB453 cells, and is effective in cell lines regardless of their PI3K or P53 mutational status (Table 1). Models of acquired resistance to trastuzumab have a higher IC50 to BAY 80-6946 than their matched parental cell lines (SKBR3 = 7.2 ± 0.8 nM; SKBR3-T = 26.2 ± 6.2 nM: BT474 = 3.9 ± 0.8 nM; BT474-Res = 6.25 ± 0.8 nM). Treatment with BAY 80-6946 (at a non-lethal dose) for 24 h significantly decreased invasion in two cell lines (BT474 p = 0.008; MDAMB453 p = 0.008) but had no effect on migration (Supplementary Fig. 1).
We studied the effect of lapatinib and afatinib (dual EGFR/HER2 inhibitors) in our panel of cell lines. Lapatinib IC50s range from 33.3 ± 9.5 nM in BT474 cells up to greater than 500 nM in cells with acquired lapatinib resistance. The cell lines with acquired lapatinib resistance SKBR3-L, -TL and HCC1954-L did not achieve an IC50 at greater than 500 nM lapatinib whilst MDAMB453 cells did not achieve an IC50 at greater than 2 µM lapatinib. Afatinib IC50s range from 3.8 ± 2.4 nM in SKBR3-T cells to greater than 1 µM in MDAMB453 cells. Interestingly, the SKBR3-L and SKBR3-TL cells have a greater IC50 to afatinib than that seen in SKBR3 cells; however the same affect is not observed in the HCC1954-L cell line relative to HCC1954 cells. Cells have varying sensitivity to trastuzumab when used alone, achieving between 43.6 ± 4.1 % growth inhibition in BT474 cells to no growth inhibition (e.g. in HCC1954 cells).
The effect of BAY 80-6946 on cell signalling in a panel of HER2-positive cell lines
The expression of PI3K-P110-alpha was not significantly affected by BAY 80-6946 treatment in any cell line tested including those models of acquired resistance to either trastuzumab and/or lapatinib. AKT phosphorylation (S473) was significantly reduced in 3/5 cell lines tested (SKBR3, BT474 and MDAMB453); however it remained unchanged in HCC1569 and increased in HCC1954 cells (Table 2, Supplementary Fig. 2). In SKBR3 and BT474 cells which had diminished AKT activation (S473) in response to BAY 80-6946 treatment, a corresponding decrease in phosphorylation of mTOR (S2481) was observed. In the models of acquired resistance, AKT phosphorylation (S473) was reduced in SKBR3-L, -T, -TL but not in HCC1954-L and BT474-RES cells whose AKT phosphorylation remained unchanged.
We found in all models tested that treating cells with 1 nM BAY 80-6946 did not result in increases in PARP cleavage or in cleavage of caspase-7, -8 or -9 (results not shown), indicating that BAY 80-6946 does not induce apoptosis in our cells at the concentration tested.
We found that HER2 (Y1248) was significantly increased in HCC1954 cells (p = 0.003) and was increased in BT474 cells treated for 6 h with BAY 80-6946 (p = 0.06). HER3 expression or activation (Y1289) was not altered after BAY 80-6946 treatment in parental HER-2 positive cells. We also saw a significant increase in MAPK activation (T202/Y204) in HCC1954 (p = 0.006), BT474 (p = 0.03) and MDAMB453 (p = 0.04) cells after treatment with BAY 80-6946.
Interestingly in models of acquired lapatinib resistance, treatment with BAY 80-6946 significantly reduced HER3 phosphorylation (Y1289) (SKBR3-L (p = 0.03) and HCC1954-L (p = 0.03)), whilst a similar effect was seen in BT474-Res cells (p = 0.04) but not in the SKBR3-TL cells or SKBR3-T cells. MAPK activation (T202/Y204) was also significantly increased in SKBR3-T (p = 0.05) cells after treatment with BAY 80-6946.
Combinations of lapatinib and BAY 80-6946 are synergistic in HER2-positive breast cancer cell lines including those with acquired lapatinib resistance
Combinations of lapatinib and BAY 80-6946 enhance growth inhibition relative to testing either drug alone in all cell lines tested (Fig. 1). Lapatinib has a synergistic response in the majority of HER2-positive breast cancer cell lines when tested in combination with BAY 80-6946. (BT474-RES CI @ ED50 = 0.32 ± 0.12 ranging to SKBR3-L CI @ ED50 = 0.85 ± 0.23) (Table 4). Despite lapatinib resistant models SKBR3-L, HCC1954-L and SKBR3-TL having limited sensitivity to lapatinib, the combination of lapatinib and BAY 80-6946 is still synergistic with clear restoration of sensitivity to lapatinib in these cell lines. This trend is also observed in the trastuzumab resistant cell lines BT474-Res and SKBR3-T, whereby the combination of lapatinib plus BAY 80-6946 remains highly synergistic (Table 3).
Efficacy of lapatinib (◊), BAY 80-6946 (□) and a combination of lapatinib and BAY 80-6946 (△) in a panel of HER2-positive cell lines, including those with acquired resistance to either trastuzumab (-T or -Res), lapatinib (-L) or the combination of trastuzumab and lapatinib (-TL). Error bars are representative of standard deviations across triplicate experiments. The ratio of lapatinib: BAY 80-6946 in this assay is fixed at 5:1
MAPK signalling activation by BAY 80-6946 is inhibited by co-treatment with BAY 80-6946 and lapatinib
After 6 h treatment with BAY 80-6946, MAPK (T202/Y204) phosphorylation was significantly increased in three of the five parental cell lines. We, therefore, performed a 30 min RPPA experiment in the SKBR3 and HCC1954 models and in the matched models of acquired lapatinib resistance to analyse the effect of lapatinib and BAY 80-6946 alone and in combination on MAPK and MEK signalling (Table 4, Supplementary Fig. 3).
Treatment with BAY 80-6946 for 30 min increased MAPK (T202/Y204) and MEK (S217/221) phosphorylation in SKBR3 and SKBR3-L cells, whilst there was an increase in MAPK (T202/Y204) signalling in HCC1954 and HCC1954-L cells. BAY 80-6946 alone decreased MEK (S217/221) phosphorylation in HCC1954 cells. Treatment with lapatinib reduced MAPK (T202/Y204) phosphorylation relative to treatment with BAY 80-6946 in all cell lines tested; however it only reduced MEK (S217/221) phosphorylation in the SKBR3-L and HCC1954-L cell lines. Finally, treatment with the combination of BAY 80-6946 and lapatinib inhibited the increase in MAPK (T202/Y204) phosphorylation by BAY 80-6946 but did not reduce further the phosphorylation of either MAPK (T202/Y204) or MEK (S217/221) relative to treatment with lapatinib alone in all cell lines tested.
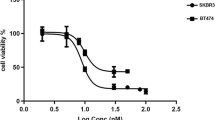
Combinations of afatinib and BAY 80-6946 are synergistic in HER2-positive cell lines
The combination of afatinib and BAY 80-6946 enhances growth inhibition relative to testing either drug alone (Fig. 2). Afatinib and BAY 80-6946 have an additive response in SKBR3 cells (CI @ ED50 = 0.91 ± 0.13) and a synergistic response in the remaining cell lines, (SKBR3-TL CI @ ED50 = 0.48 ± 0.02 to HCC1569 CI @ ED50 = 0.58 ± 0.13) (Fig. 2, Table 3). Indeed, the combination is far more synergistic in BT474-Res, SKBR3-T, SKBR3-L and SKBR3-TL than in BT474 and SKBR3 parental cells, respectively. Interestingly, afatinib/BAY 80-6946 synergism is thus enhanced in cell line models of acquired resistance to trastuzumab and/or lapatinib.
Efficacy of afatinib (◊), BAY 80-6946 (□) and a combination of afatinib and BAY 80-6946 (△) in a panel of HER2-positive cell lines, including those with acquired resistance to either trastuzumab (-T or -Res), lapatinib (-L) or the combination of trastuzumab and lapatinib (-TL). Error bars are representative of standard deviations across triplicate experiments. The ratio of lapatinib: BAY 80-6946 in this assay is fixed at 1:1
Combinations of trastuzumab and BAY 80-6946 improve response to either drug tested alone in HER2-positive breast cancer cells including those with acquired trastuzumab resistance
The combination of trastuzumab and BAY 80-6946 resulted in significantly improved growth inhibition compared to either therapy alone in three of the four parental cell lines tested (BT474, HCC1954 and SKBR3) (Fig. 3). Combinations of BAY 80-6946 and trastuzumab significantly enhanced growth inhibition in models of acquired trastuzumab and/or lapatinib resistance (BT474-Res, SKBR3-L, -T, -TL (p < 0.05)) but not in HCC1954-L cells.
The efficacy of combining trastuzumab (T) at 10 μg/ml and BAY 80-6946 (B) at varying concentrations in a panel of HER2-positive cell lines including matched models of acquired trastuzumab and/or lapatinib resistance. Standard Deviations are representative of independent triplicate experiments. Asterisk indicates a p value < 0.05 as calculated by Kruskal–Wallis non-parametric test
PI3K inhibition does not sensitise de novo resistant HER2-positive breast cancer cell lines to HER2 inhibitors
Although our data shows the benefit of combining BAY 80-6946 with HER2-targeted therapies in cells which are either sensitive to or have acquired resistance to HER2-inhibitors, combinations of BAY 80-6946 and lapatinib or afatinib do not demonstrate an increase in proliferation inhibition in MDAMB453 cells which have de novo lapatinib resistance (Supplementary Fig. 4). However, despite their resistance to HER2 inhibitors, these cells are still sensitive to BAY 80-6946 (Table 1) and no increased proliferation is observed when tested with the combination of lapatinib and BAY 80-6946.
Discussion
Resistance to trastuzumab remains a significant clinical problem, with up to 30 % of patients not responding to it in the metastatic setting [2]. Strong evidence has implicated the PI3K pathway in trastuzumab and lapatinib resistance [5, 6, 18], although data supporting the involvement of PI3K signalling in lapatinib resistance are somewhat conflicting [8, 19]. Preclinical testing of mTOR inhibitors led to anticipation that resistance to HER2 targeted therapies could be overcome, but their clinical benefit has been somewhat disappointing [9], reflected in the results of the Phase 3 BOLERO-3 clinical trial [20]. We, therefore, hypothesised that targeting PI3K directly would represent a more optimal strategy, and that combined PI3K- and HER2-inhibition may represent an improved treatment strategy for HER2-positive breast cancer.
BAY 80-6946 is a novel, potent PI3K inhibitor with in vitro and in vivo efficacy [11–14] which was well tolerated in a phase I clinical trial [15] and we found it to have anti-proliferative effects in HER2-positive breast cancer cell lines regardless of their PI3K mutational status. We also found that BAY 80-6946 inhibited invasion but had no effect on migration. The PI3K pathway, like HER2, has previously been shown to up regulate invasion [21, 22], a crucial step in metastasis [23]. Therefore, it is encouraging to note that in addition to inhibiting proliferation, BAY 80-6946 also inhibited invasion in HER2-positive cell lines. This may also suggest a potential role for BAY 80-6946 in the adjuvant treatment of breast cancer as well as in the metastatic setting.
In our cell line panel, we tested BAY 80-6946 at 1 nM to observe pure signalling effects, without the signalling interference associated with cell death. BAY 80-6946 did not effectively inhibit AKT phosphorylation in all our cell lines at the concentration tested. However, previous reports have indicated that AKT phosphorylation is effectively inhibited in other models of cancer at higher concentrations (200 µmol/L) [13]. We believe that the reduction of PI3K signalling observed in some, but not all cell lines may thus in part reflect the dose of BAY 80-6946 used in our RPPA signalling experiment (1 nM). In addition, we have previously observed that pharmacokinetics including cellular uptake of kinase inhibitor drugs vary across cell lines [24] and also that PI3K promotes oncogenic activity through both AKT-dependent and AKT-independent mechanisms [25]. However, an elucidation of the exact reason(s) for the reduction of PI3K signalling in some but not all cell lines by BAY 80-6946 is beyond the scope of our article.
In what is arguably the most important observation of this study, we found that combining BAY 80-6946 with the HER2-targeted therapies trastuzumab, lapatinib and afatinib resulted in significantly greater proliferation inhibition relative to testing either drug alone in our panel of cells including those with acquired resistance to trastuzumab and/or lapatinib. To evaluate BAY 80-6946’s potential to restore the efficacy of the HER-targeted therapies in cells with acquired resistance, we compared the IC50’s of lapatinib and afatinib used in combination with BAY 80-6946 against the IC50 of lapatinib and afatinib alone. In all cases, the IC50 of the HER-targeted therapy was less in combination with BAY 80-6946 than as a single agent. In SKBR3-L and HCC1954-L cells, lapatinib when used with BAY 80-6946 achieved an IC50 that was similar or less than the IC50 of lapatinib used alone in the corresponding parental cell line, indicating that the addition of BAY 80-6946 does restore sensitivity to lapatinib. Importantly, combinations of BAY 80-6946 with lapatinib and afatinib were synergistic in all cell lines with acquired resistance to lapatinib and/or trastuzumab, indicating a potential clinical benefit to using combinations of the PI3K inhibitor BAY 80-6946 with HER-targeted agents in patients whose cancers have developed resistance to these HER2-targeted agents.
Although PI3K inhibition has previously been shown by some to activate HER3 [26], possibly attenuating the antitumor effect of some PI3K inhibitors [27], we found that BAY 80-6946 did not activate HER3 phosphorylation in any cell line tested. We did, however, find that when used alone, BAY 80-6946 activated HER2 phosphorylation. PI3K inhibition has also previously been shown to enhance HER signalling resulting in compensatory MAPK signalling in HER2-positive breast cancer [28]. Because we observed increases in MAPK signalling, in some cases associated with increases in HER2 phosphorylation, after treatment with BAY 80-6946, we hypothesised that combining BAY 80-6946 with lapatinib would overcome this MAPK activation. We found that combining BAY 80-6946 with lapatinib inhibited MAPK (T202/Y204) phosphorylation by BAY 80-6946 and instead resulted in a reduction of MAPK signalling in all cell lines tested (with a parallel reduction in MEK signalling in some models of acquired lapatinib resistance). This finding may underlie, at least in part, the synergy between BAY 80-6946 and HER2 inhibitors, and further supports the argument that PI3K inhibition should be used in combination with HER2-inhibitors.
In summary, BAY 80-6946 is effective as monotherapy in HER2-positive breast cancer cells including models of acquired resistance to trastuzumab and/or lapatinib. Combinations of BAY 80-6946 with HER2-targeted therapies offer greater benefit than testing drugs alone and can restore sensitivity to HER2-inhibitors in cells with acquired resistance to trastuzumab and lapatinib. BAY 80-6946 also inhibits the invasion of HER2-positive breast cancer cells. Taken together, our data argue that the addition of the PI3K inhibitor BAY 80-6946 to HER2-targeted therapy should be considered for clinical trial evaluation in patients with HER2-positive breast cancer whose disease has become refractory to HER2-targeted therapies such as trastuzumab or lapatinib.
References
Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL (1987) Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 235(4785):177–182
Piccart-Gebhart MJ, Procter M, Leyland-Jones B, Goldhirsch A, Untch M, Smith I, Gianni L, Baselga J, Bell R, Jackisch C, Cameron D, Dowsett M, Barrios CH, Steger G, Huang CS, Andersson M, Inbar M, Lichinitser M, Lang I, Nitz U, Iwata H, Thomssen C, Lohrisch C, Suter TM, Ruschoff J, Suto T, Greatorex V, Ward C, Straehle C, McFadden E, Dolci MS, Gelber RD, Herceptin Adjuvant Trial Study T (2005) Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. N Engl J Med 353(16):1659–1672. doi:10.1056/NEJMoa052306
Scaltriti M, Chandarlapaty S, Prudkin L, Aura C, Jimenez J, Angelini PD, Sanchez G, Guzman M, Parra JL, Ellis C, Gagnon R, Koehler M, Gomez H, Geyer C, Cameron D, Arribas J, Rosen N, Baselga J (2010) Clinical benefit of lapatinib-based therapy in patients with human epidermal growth factor receptor 2-positive breast tumors coexpressing the truncated p95HER2 receptor. Clin Cancer Res 16(9):2688–2695. doi:10.1158/1078-0432.CCR-09-3407
Hennessy BT, Smith DL, Ram PT, Lu Y, Mills GB (2005) Exploiting the PI3K/AKT pathway for cancer drug discovery. Nat Rev Drug Discov 4(12):988–1004. doi:10.1038/nrd1902
Stemke-Hale K, Gonzalez-Angulo AM, Lluch A, Neve RM, Kuo WL, Davies M, Carey M, Hu Z, Guan Y, Sahin A, Symmans WF, Pusztai L, Nolden LK, Horlings H, Berns K, Hung MC, van de Vijver MJ, Valero V, Gray JW, Bernards R, Mills GB, Hennessy BT (2008) An integrative genomic and proteomic analysis of PIK3CA, PTEN, and AKT mutations in breast cancer. Cancer Res 68(15):6084–6091. doi:10.1158/0008-5472.CAN-07-6854
Berns K, Horlings HM, Hennessy BT, Madiredjo M, Hijmans EM, Beelen K, Linn SC, Gonzalez-Angulo AM, Stemke-Hale K, Hauptmann M, Beijersbergen RL, Mills GB, van de Vijver MJ, Bernards R (2007) A functional genetic approach identifies the PI3K pathway as a major determinant of trastuzumab resistance in breast cancer. Cancer Cell 12(4):395–402. doi:10.1016/j.ccr.2007.08.030
Gallardo A, Lerma E, Escuin D, Tibau A, Munoz J, Ojeda B, Barnadas A, Adrover E, Sanchez-Tejada L, Giner D, Ortiz-Martinez F, Peiro G (2012) Increased signalling of EGFR and IGF1R, and deregulation of PTEN/PI3K/Akt pathway are related with trastuzumab resistance in HER2 breast carcinomas. Br J Cancer 106(8):1367–1373. doi:10.1038/bjc.2012.85
Gayle SS, Arnold SL, O’Regan RM, Nahta R (2012) Pharmacologic inhibition of mTOR improves lapatinib sensitivity in HER2-overexpressing breast cancer cells with primary trastuzumab resistance. Anticancer Agents Med Chem 12(2):151–162
Chan S, Scheulen ME, Johnston S, Mross K, Cardoso F, Dittrich C, Eiermann W, Hess D, Morant R, Semiglazov V, Borner M, Salzberg M, Ostapenko V, Illiger HJ, Behringer D, Bardy-Bouxin N, Boni J, Kong S, Cincotta M, Moore L (2005) Phase II study of temsirolimus (CCI-779), a novel inhibitor of mTOR, in heavily pretreated patients with locally advanced or metastatic breast cancer. J Clin Oncol 23(23):5314–5322. doi:10.1200/JCO.2005.66.130
Sun SY, Rosenberg LM, Wang X, Zhou Z, Yue P, Fu H, Khuri FR (2005) Activation of Akt and eIF4E survival pathways by rapamycin-mediated mammalian target of rapamycin inhibition. Cancer Res 65(16):7052–7058. doi:10.1158/0008-5472.CAN-05-0917
Liu NRB, Schneider C, Bull C, Hoffmann J, Kaekoenen S, Hentemann M, Scott W, Mumberg D, Ziegelbauer K (2010) BAY 80-6946, a highly selective and potent pan-class I PI3K inhibitor, induces tumor apoptosis in vitro and tumor regression in vivo in a subset of tumor models. Paper presented at the American Association for Cancer Research, Washington DC
Liu NHA, Bull C, Schatz C, Wiehr S, Pichler BJ, Hauff P, Mumberg D, Jenkins S, Schwarz T, Ziegelbauer K (2010) BAY 80-6946, a highly potent and efficacious PI3K class I inhibitor, induces complete tumor regression or tumor stasis in tumor xenograft models with PIK3CA mutant or PTEN deletion. Paper presented at the American Association for Cancer Research, Washington DC
Liu N, Rowley BR, Bull CO, Schneider C, Haegebarth A, Schatz CA, Fracasso PR, Wilkie DP, Hentemann M, Wilhelm SM, Scott WJ, Mumberg D, Ziegelbauer K (2013) BAY 80-6946 is a highly selective intravenous PI3K inhibitor with potent p110alpha and p110delta activities in tumor cell lines and xenograft models. Mol Cancer Ther 12(11):2319–2330. doi:10.1158/1535-7163.MCT-12-0993-T
Glauer J, Pletz N, Schon M, Schneider P, Liu N, Ziegelbauer K, Emmert S, Wulf GG, Schon MP (2013) A novel selective small-molecule PI3K inhibitor is effective against human multiple myeloma in vitro and in vivo. Blood Cancer J 3:e141. doi:10.1038/bcj.2013.37
Lotze MTAL, Ramanathan RK, Tolcher AW, Beeram M, Papadopoulos KP, Rasco DW, Weiss GJ, Mountz JM, Toledo FGS, Alvarez RJ, Oborski MJ, Rajagopalan P, Jeffers M, Roth D, Duboxy RL, Patnaik A (2012) Phase I study of intravenous PI3K inhibitor BAY 80-6946: activity in patients with advanced solid tumors and non-Hodgkin’s lymphoma treated in MTD expansion cohorts. Paper presented at the American Society of Clinical Oncology, Chicago, Illinois
Eustace AJ, Crown J, Clynes M, O’Donovan N (2008) Preclinical evaluation of dasatinib, a potent Src kinase inhibitor, in melanoma cell lines. J Transl Med 6:53. doi:10.1186/1479-5876-6-53
Hennessy BT, Lu Y, Gonzalez-Angulo AM, Carey MS, Myhre S, Ju Z, Davies MA, Liu W, Coombes K, Meric-Bernstam F, Bedrosian I, McGahren M, Agarwal R, Zhang F, Overgaard J, Alsner J, Neve RM, Kuo WL, Gray JW, Borresen-Dale AL, Mills GB (2010) A technical assessment of the utility of reverse phase protein arrays for the study of the functional proteome in non-microdissected human breast cancers. Clin Proteomics 6(4):129–151. doi:10.1007/s12014-010-9055-y
Saal LH, Holm K, Maurer M, Memeo L, Su T, Wang X, Yu JS, Malmstrom PO, Mansukhani M, Enoksson J, Hibshoosh H, Borg A, Parsons R (2005) PIK3CA mutations correlate with hormone receptors, node metastasis, and ERBB2, and are mutually exclusive with PTEN loss in human breast carcinoma. Cancer Res 65(7):2554–2559. doi:10.1158/0008-5472-CAN-04-3913
O’Brien NA, Browne BC, Chow L, Wang Y, Ginther C, Arboleda J, Duffy MJ, Crown J, O’Donovan N, Slamon DJ (2010) Activated phosphoinositide 3-kinase/AKT signaling confers resistance to trastuzumab but not lapatinib. Mol Cancer Ther 9(6):1489–1502. doi:10.1158/1535-7163.MCT-09-1171
O’Regan R, Ozguroglu M, Andre F, Toi M, Jerusalem G, Wilks S, Isaacs C, Xu B, Masuda N, Arena F, Yardley D, Yap Y, Mukhopadhyay P, Douma S, El-Hashimy M, Taran T, Sahmoud T, Lebwohl D, Gianni L (2013) Phase III, randomized, double-blind, placebo-controlled multicenter trial of daily everolimus plus weekly trastuzumab and vinorelbine in trastuzumab-resistant, advanced breast cancer (BOLERO-3). J Clin Oncol 31(suppl; abstr 505)
Chen JSWQ, Fu XH, Huang XH, Chen X, Cao L, Chen L, Tan H, Li W, Bi J, Zhang L (2008) Involvement of PI3K/PTEN/AKT/mTOR pathway in invasion and metastasis in hepatocellular carcinoma: association with MMP-9. Hepatol Res 39(2):177–186
Asrani K, Keri RA, Galisteo R, Brown SA, Morgan SJ, Ghosh A, Tran NL, Winkles JA (2013) The HER2- and heregulin beta1 (HRG)-inducible TNFR superfamily member Fn14 promotes HRG-driven breast cancer cell migration, invasion, and MMP9 expression. Mol Cancer Res 11(4):393–404. doi:10.1158/1541-7786.MCR-12-0542
Seyfried TN, Huysentruyt LC (2013) On the origin of cancer metastasis. Crit Rev Oncog 18(1–2):43–73
Hennessy BT, Lu Y, Poradosu E, Yu Q, Yu S, Hall H, Carey MS, Ravoori M, Gonzalez-Angulo AM, Birch R, Henderson IC, Kundra V, Mills GB (2007) Pharmacodynamic markers of perifosine efficacy. Clin Cancer Res 13(24):7421–7431. doi:10.1158/1078-0432.CCR-07-0760
Vasudevan KM, Barbie DA, Davies MA, Rabinovsky R, McNear CJ, Kim JJ, Hennessy BT, Tseng H, Pochanard P, Kim SY, Dunn IF, Schinzel AC, Sandy P, Hoersch S, Sheng Q, Gupta PB, Boehm JS, Reiling JH, Silver S, Lu Y, Stemke-Hale K, Dutta B, Joy C, Sahin AA, Gonzalez-Angulo AM, Lluch A, Rameh LE, Jacks T, Root DE, Lander ES, Mills GB, Hahn WC, Sellers WR, Garraway LA (2009) AKT-independent signaling downstream of oncogenic PIK3CA mutations in human cancer. Cancer Cell 16(1):21–32. doi:10.1016/j.ccr.2009.04.012
Garrett JT, Olivares MG, Rinehart C, Granja-Ingram ND, Sanchez V, Chakrabarty A, Dave B, Cook RS, Pao W, McKinely E, Manning HC, Chang J, Arteaga CL (2011) Transcriptional and posttranslational up-regulation of HER3 (ErbB3) compensates for inhibition of the HER2 tyrosine kinase. Proc Natl Acad Sci USA 108(12):5021–5026. doi:10.1073/pnas.1016140108
Chakrabarty A, Sanchez V, Kuba MG, Rinehart C, Arteaga CL (2012) Feedback upregulation of HER3 (ErbB3) expression and activity attenuates antitumor effect of PI3K inhibitors. Proc Natl Acad Sci USA 109(8):2718–2723. doi:10.1073/pnas.1018001108
Serra V, Scaltriti M, Prudkin L, Eichhorn PJ, Ibrahim YH, Chandarlapaty S, Markman B, Rodriguez O, Guzman M, Rodriguez S, Gili M, Russillo M, Parra JL, Singh S, Arribas J, Rosen N, Baselga J (2011) PI3K inhibition results in enhanced HER signaling and acquired ERK dependency in HER2-overexpressing breast cancer. Oncogene 30(22):2547–2557. doi:10.1038/onc.2010.626
Acknowledgments
We thank Dr. Scott Wilhelm and Bayer Pharmaceuticals for providing us with BAY 80-6946. We also thank Dr. Norma O’Donovan, Dublin City University, for her gift of SKBR3-T, SKBR3-L, SKBR3-TL and HCC1954-L, and Dr. Neil O’Brien, University of California Los Angeles, for BT474-PAR and BT474-Res. We also thank St James University Hospital pharmacy for providing us with trastuzumab.
Conflict of interest
The authors state that they have no conflicts of interest in relation to this article or the funding bodies.
Financial information
This work was supported by Irish Cancer Society Research (CRS11ELS), Health Research Board (HRA/POR2012/054), BREAST-PREDICT, NECRET, the North Eastern Cancer Research and Education Trust and the Royal Irish Academy Mobility Grant 2013.
Author information
Authors and Affiliations
Corresponding author
Additional information
B. T. Hennessy and A. J. Eustace, joint senior authors have contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10549_2014_3239_MOESM1_ESM.docx
Supplementary Fig. 1: Effect of 5nM BAY 80-6946 on (a) invasion and (b) migration in MDAMB453 and BT474 cells over a 24 h period. Error bars represent standard deviations of triplicate experiments. ‘*’ represents p < 0.05 as calculated by Student’s t-test. Supplementary material 1 (DOCX 56 kb)
10549_2014_3239_MOESM2_ESM.docx
Supplementary Fig. 2: Percentage changes in protein expression or phosphorylation as calculated from RPPA analysis following treatment of cells with 1nM BAY 80-6946 for 6 h relative to untreated controls in A) panel of HER2 positive BC cells, B) SKBR3 parental and resistant models C) HCC1954 and BT474 parental and resistant models. Standard deviations are calculated using propagation of error from triplicate independent biological experiments. Supplementary material 2 (DOCX 126 kb)
10549_2014_3239_MOESM3_ESM.docx
Supplementary Fig. 3: Percentage changes in protein expression or phosphorylation as calculated from RPPA analysis following treatment of cells with ‘●‘1nM BAY 80-6946, ‘▲‘lapatinib or ‘□‘a combination of lapatinib and BAY 80-6946 for 30 min relative to untreated controls SKBR3 and HCC1954 parental and lapatinib resistant cells. Standard deviations are calculated using propagation of error from triplicate independent biological experiments. Supplementary material 3 (DOCX 110 kb)
10549_2014_3239_MOESM4_ESM.docx
Supplementary Fig. 4: Efficacy of lapatinib or afatinib (-◊-), BAY 80-6946 (-□-) and a combination of lapatinib or afatinib with BAY 80-6946 (–∆–) in MDAMB453 cell lines which have de novo resistance to HER2-inhibitors. Error bars are representative of standard deviations across triplicate experiments. The ratio of lapatinib: BAY 80-6946 in this assay is fixed at 1:1. Supplementary material 4 (DOCX 50 kb)
Rights and permissions
About this article
Cite this article
Elster, N., Cremona, M., Morgan, C. et al. A preclinical evaluation of the PI3K alpha/delta dominant inhibitor BAY 80-6946 in HER2-positive breast cancer models with acquired resistance to the HER2-targeted therapies trastuzumab and lapatinib. Breast Cancer Res Treat 149, 373–383 (2015). https://doi.org/10.1007/s10549-014-3239-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-014-3239-5