Abstract
Pompe disease (PD) is caused by a deficiency of lysosomal acid α-glucosidase resulting from mutations in the GAA gene. The clinical spectrum ranges from a rapidly fatal multisystemic disorder (classic PD, onset < 1 year) to a milder adult onset myopathy. The aims of this study were to characterize the GAA mutations, to establish the disease epidemiology, and to identify potential genotype-phenotype correlations in French late-onset PD patients (onset ≥ 2 years) diagnosed since the 1970s. Data were collected from the two main laboratories involved in PD diagnosis and from the French Pompe registry. Two hundred forty-six patients (130 females and 116 males) were included, with a mean age at diagnosis of 43 years. Eighty-three different mutations were identified in the GAA gene, among which 28 were novel. These variants were spread all over the sequence and included 42 missense (one affecting start codon), 8 nonsense, 15 frameshift, 14 splice mutations, 3 small in-frame deletions, and one large deletion. The common c.-32-13T>G mutation was detected in 151/170 index cases. Other frequent mutations included the exon 18 deletion, the c.525del, and the missense mutations c.1927G>A (p.Gly643Arg) and c.655G>A (p.Gly219Arg). Patients carrying the c.-32-13T>G mutation had an older mean age at onset than patients non-exhibiting this mutation (36 versus 25 years). Patients with the same genotype had a highly variable age at onset. We estimated the frequency of late-onset PD in France around 1/69,927 newborns. In conclusion, we characterized the French cohort of late-onset PD patients through a nationwide study covering more than 40 years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
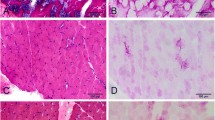
Pompe disease (PD), or glycogen storage disease type II (GSDII; MIM #232300), is an autosomal recessive disorder caused by a deficiency of the lysosomal enzyme acid α-glucosidase (GAA; EC 3.2.1.3), which catalyzes the hydrolysis of α-1,4 and α-1,6 links of glycogen. GAA deficiency leads to the accumulation of glycogen in lysosomes especially within skeletal, cardiac, and vascular smooth muscle cells. The clinical spectrum ranges from a rapidly fatal infantile-onset form to a slowly progressive adult form (Hirschhorn and Reuser 2001; van der Ploeg and Reuser 2008). The classic infantile-onset form presents in the first months of life with generalized hypotonia and muscle weakness, severe hypertrophic cardiomyopathy, failure to thrive, and respiratory insufficiency. Untreated patients usually die in the first year of life due to progressive cardiorespiratory failure (Kishnani et al. 2006). The late-onset (also called non-classic) form presents a more variable spectrum of clinical features, and onset of symptoms ranges from the first years of life to late adulthood (Chan et al. 2017). According to Güngör and Reuser (2013), the “childhood” Pompe disease includes patients with onset of symptoms ≤ 16 years without persisting and progressive cardiac hypertrophy, whereas the “adult” Pompe disease corresponds to patients with onset of symptoms > 16 years. The late-onset form is characterized by progressive proximal and axial muscle weakness leading to loss of motor function (Hagemans et al. 2006). Diaphragmatic weakness and respiratory insufficiency are frequent and prominent. The clinical phenotype usually correlates with mutation severity and subsequent residual enzymatic activity (Laforêt et al. 2000; Hirschhorn and Reuser 2001; Herzog et al. 2012).
The incidence of the disease varies from 1/14,000 to 1/600,000 depending on geographic origin, diagnostic criteria, and methods (Martiniuk et al. 1998; Leslie and Bailey 2007). The diagnosis of PD is established by evidencing a marked decrease of acid alpha-glucosidase activity either in lymphocytes/leucocytes, cultured fibroblasts, muscle biopsy, or dried blood spots, and it is confirmed by the determination of the causative mutations (Pompe Disease Diagnostic Working et al. 2008; Reuser et al. 2011). The GAA gene (HGNC: 4065) is located on 17q25. It contains 20 exons, and the start codon is at nucleotide 33 in exon 2 (Hoefsloot et al. 1990). The May 2016 edition of the Pompe Disease Mutation Database (http://www.pompecenter.nl) provides a list of 558 sequence variants spread along the entire gene, among which 374 are pathogenic. Many mutations are private, and only few mutations are common in specific populations, such as the c.-32-13T>G mutation in late-onset forms of PD in Caucasians.
In France, a clinical network was set up among neuromuscular referral centers to facilitate diagnosis and follow-up of PD. Patient samples were sent to two main laboratories (Paris and Lyon) performing enzymatic and genetic analyses. Furthermore, a PD national registry has been created in 2004 and qualified in 2008, with the aim of prospectively gathering clinical, functional, and biological data of all French PD patients (Laforêt et al. 2013). Therefore, the aims of this study were as follows: (1) to characterize the GAA mutations present in late-onset French PD patients, (2) to establish the epidemiology of this clinical form in France, (3) to identify potential genotype-phenotype correlations.
Material and methods
Patients and databases
The study complies with national data protection requirements (Commission Nationale Informatique et Libertés, CNIL) and with the Code of Ethics of the World Medical Association (Declaration of Helsinki). The French Pompe registry has been qualified since 2008 by Comité National des Registres-Maladies Rares (CNR-MR) supported by Institut National de la Santé et de la Recherche Médicale (INSERM) and Institut de Veille Sanitaire (InVS).
Inclusion criteria were as follows: (1) confirmed diagnosis of PD, established with at least two different methods (either enzymatic test on lympho/leukocytes and confirmation on fibroblasts, or enzymatic test on lympho/leukocytes and confirmation by GAA gene sequencing, or enzymatic test on dried-blood spots and confirmation by GAA gene sequencing); (2) disease onset ≥ 2 years of age. Some patients had incomplete genetic (i.e., molecular analysis not performed, one unidentified allele, absence of informed consent) or clinical (age at onset, first symptoms) data. For the epidemiologic study, only patients diagnosed after January 1, 2001, were included (Fig. S1).
Genetic analyses
DNA amplification and sequencing
Genomic DNA was extracted from patient peripheral blood samples or cultured fibroblasts according to well-established procedures. PCR reactions were carried out to amplify the coding exons of the GAA gene and their corresponding intron-exon boundaries, using specific pairs of primers located in the flanking intronic regions. Each amplicon was purified and sequenced in both directions using the same primers. Sequencing was performed using the ABI PRISM Big Dye Terminator Kit (Applied Biosystems®) following standard recommendations. A specific PCR protocol was performed to detect the common deletion c.2481+102_2646+31del (delta exon 18) using primers located on both sides of the deletion.
Mutation analysis and in silico prediction of the identified variants
Sequence variations were compared with the reference sequence NM_000152.4. In silico prediction of the newly identified variants was performed using the Alamut® software (http://www.interactivebiosoftware.com). The severity of each mutation was classified as very severe, potentially less severe, less severe, and potentially mild according to the Pompe Disease Mutation Database ranking system (Kroos et al. 2008).
Epidemiology of Pompe disease
The French PD patients included in this study were collected using information from the following: (1) the neuromuscular disease referral centers and their large clinical network, (2) the two main diagnosis laboratories (Paris and Lyon), (3) the French Pompe registry. Incidence rate and proportion of newborns that will be affected by late-onset Pompe disease were estimated. The incidence rate describes how quickly a disease occurs in a population and is calculated by the ratio between the number of new late-onset PD diagnoses during specified time intervals (2001–2005, 2006–2010, 2011–2015, and for the whole period 2001–2015) and the average population during these time intervals. In order to estimate the proportion of newborns that will be affected by late-onset Pompe disease, we also assessed the number of diagnosed patients divided by the average number of newborns in their year of birth. The population data were extrapolated from Institut National de la Statistique et des Etudes Economiques (INSEE).
Clinical data
The clinical data regarding onset of the disease were obtained from the French Pompe registry or from clinical records. The onset of the disease was defined as the occurrence of muscular weakness (difficulty in running, climbing stairs, rising from floor, etc.) or signs of respiratory muscle weakness (orthopnea, respiratory insufficiency). HyperCKemia (2.5-fold the upper normal limit), muscle fatigue, and exercise intolerance were not considered as first symptoms.
Statistical analysis
Demographic descriptions are given in number and/or percentage (%) for qualitative variables, in mean and standard deviation (± SD) for quantitative variables (or in median in case of non-Gaussian distribution). Quantitative variables were compared using t test (two groups) or ANOVA with Bonferroni’s multiple comparison test (more than two groups) in the GraphPad Prism® software. The statistical significance was set at p < 0.05.
Results
Patient population
PD diagnosis was established in 246 patients including 209 index cases and 37 relatives during the period 1972–2015. Sex ratio was 1:1 (130 females, 116 males). Consanguinity was reported in two families. Mean age at diagnosis was 43.1 ± 17.5 years. Sixteen patients were diagnosed at a presymptomatic stage (5 relatives and 11 index cases, the latest usually referred for hyperCKemia or aspecific symptoms such as fatigue or myalgia). Mean age at disease onset was 34.6 ± 20.1 years, ranging from 2 to 70 years. Of patients, 87.4% had an age at onset > 16 years (adult Pompe disease) and 12.6% an age at onset ≤ 16 years (childhood Pompe disease including 11% for the 4–16 years and 1.6% for the 2–3 years). The age at onset was not significantly different between males and females (mean age at disease onset 35.6 ± 20.4 versus 33.7 ± 19.9 years). First symptoms were usually muscular weakness and rarely respiratory problems. The mean diagnostic delay (years from disease onset to diagnosis) was 8.7 ± 9.3 years ranging from 0 to 46 years (Table S1).
GAA gene analysis
GAA gene sequencing was performed in 204 patients, and causative mutations were found in 185. In the 19 remaining patients, only one mutation was identified, usually due to the incomplete DNA analysis performed in the first years of the study. We identified 83 different pathogenic or probably pathogenic variants, spread all over the sequence except exons 16 and 20 (Fig. S2). They included 42 missense mutations (one affecting the start codon), 15 frameshift mutations leading to a premature stop codon, 14 splice mutations, 8 nonsense mutations, 3 small in-frame deletions and one large deletion. The distribution of mutations among patient alleles is shown in Table S2. Splice mutations (including the.c-32-13T>G) represented 53% of alleles, missense mutations 23%, deletions 9%, frameshift mutations 8%, nonsense mutations 5%, and other mutations or complex alleles 2%. Five patients including two siblings had complex alleles with two alterations in cis (Table S3).
The common c.-32-13T>G mutation was detected in 89% of index cases on at least one allele, and it was present on both alleles in 3 patients (allele frequency = 48.1%). Other recurrent mutations included the large deletion c.2481+102_2646+31del (7.5%), the missense mutations c.1927G>A (3.7%) and c.655G>A (2.7%), and the small deletion c.525del (2.4%). Other mutations had an allele frequency ≤ 2% (Table 1).
Among the 83 different variants identified, 28 (34%) were novel (Table 2). These included 13 mutations leading to a truncated mRNA and/or protein (9 frameshift mutations and 4 nonsense mutations), 3 splice mutations, 10 novel missense mutations, and 2 deletions of one amino acid. The novel variants were defined as probably disease-causing mutations using the Alamut® software.
Epidemiology of Pompe disease
The distribution of newly diagnosed PD patients per year is presented in Fig. 1. The number of diagnoses increased from 2.6/year (period before 2001) to 10.6/year (2001–2010) and 12.8/year (2011–2015). Considering the 2001–2015 period, we estimated the incidence of late-onset PD in France to 17.76 patients per 100,000,000 inhabitants per year. We could also estimate the proportion of newborns that will be affected by late-onset PD to 1.43/100,000 newborns or 1/69,927 newborns (Table S1).
Genotype-phenotype correlations
Clinical data and complete genotype identification were available for 149 patients. Patients with the c.-32-13T>G mutation (n = 131) presented a later onset compared to the 18 patients non-carrying the c.-32-13T>G mutation (mean age at onset 36.2 ± 13.9 years (ranging from 2 to 64) versus 24.7 ± 14.8 years (ranging from 3 to 51); p < 0.01) (Fig. 2a). Patients with the c.-32-13T>G mutation on one allele were grouped according to the severity of the second mutation. No correlation could be found with the age at onset, but all the patients presenting an early-onset had a very severe mutation on the second allele (Fig. 2b). Patients carrying identical GAA genotype (c.-32-13T>G on one allele and another recurrent mutation on the second allele) had a highly variable age at onset (Table 1, right column). In childhood PD patients (onset ≤ 16 years), the c.-32-13T>G mutation was less frequent (65%; 15/23 patients) than in adult PD patients (92%; 166/180; Chi-squared test, p < 0.001). Moreover, very severe mutations were detected in 14/23 childhood PD patients (Table 3). Concerning the five patients with three pathogenic or probably pathogenic variations in the GAA gene, their age at onset was heterogeneous, between 17 and 50 years (Table S3).
a Age at disease onset in patients with the c.-32-13T>G mutation versus patients non-carrying the c.-32-13T>G mutation. Horizontal lines represent mean values (unpaired t test p = 0.0014). b Age at disease onset in patients carrying the c.-32-13T>G mutation on one allele grouped according to the second mutation severity. Horizontal lines represent mean values. No significant differences were observed between groups even if a trend toward earlier onset is observed in patients with severe mutations. The severity is given according to the ranking system used in the Pompe Disease Mutation Database (Kroos et al. 2008). VS very severe, PLS potentially less severe, LS less severe, PM potentially mild
Discussion
This study described molecular features and epidemiology of late-onset PD and investigated potential correlations between genotype and age at disease onset in the largest population ever reported. Homogeneity of the data and accuracy of the results were guaranteed by the French Pompe registry, which collected data on natural history and follow-up of all patients (whether treated with enzyme replacement therapy or not) in France. In this cohort, the common c.-32-13T>G mutation was present in 89% of index cases as described in the Caucasian population (Huie et al. 1994; Kroos et al. 1995; Montalvo et al. 2006; Herzog et al. 2012). This mutation leads to impaired splicing of exon 2. Since a low amount of normally spliced mRNA is produced, the GAA activity is not completely deficient, and patients usually develop a late-onset form of PD (Raben et al. 1996; Dardis et al. 2014). The carrier frequency of the c.-32-13T>G mutation was estimated at 1/154 in the general unaffected Dutch population (Ausems et al. 1999) and at 1/184 in the Genome Aggregation Database (gnomAD, Broad Institute; Lek et al. 2016). According to these estimates, Rairikar et al. (2017) calculated that 16 to 40% of all adult PD patients should theoretically have this mutation in homozygosity. However, few homozygous patients have been reported in the literature and they were 3 in our series, suggesting that homozygotes for the c.-32-13T>G mutation are usually asymptomatic or have a milder phenotype that could be underdiagnosed.
Two other common mutations were identified in our population: c.2481+102_2646+31del (delta exon 18) and c.525del. Their frequency was lower than in the Netherlands (Ausems et al. 2001) but comparable to non-Dutch populations (Hirschhorn and Huie 1999; Herzog et al. 2012). Two missense mutations, c.1927G>A (p.Gly643Arg) and c.655G>A (p.Gly219Arg), were more frequent in France than in other countries. Numerous other GAA mutations were found, confirming the high heterogeneity of mutations in PD. Among the 83 mutations identified, 55 (66%) were private. To note, France is an ethnically complex country as it has been settled by several European peoples and has several overseas territories spread all over the world. This genetic background could contribute to the high number of GAA variations. Interestingly, five patients had three mutations including at least one missense mutation (two of them were novel). It was not possible to clearly determine if the presence of two alterations in cis was necessary for the disease onset.
In our study, 28 mutations were novel. The nonsense and frameshift mutations (n = 13) created a premature termination codon (all located upstream of exon 20) leading to a truncated GAA mRNA with or without mRNA decay (absent or truncated protein). The splice mutations (n = 3) directly affected a donor or acceptor site, leading to aberrant splicing. The pathogenicity of the novel missense mutations and single amino-acid deletions (n = 12) was assessed using different criteria. In silico prediction studies argued in favor of their pathogenicity. They affected highly conserved residues among species and/or were in the nearby of the active site. Moreover, these gene alterations were absent from large population datasets of genetic variation (gnomAD), or at very low allele frequency (< 1/10.000).
The number of PD diagnoses increased in France over the last 40 years, reflecting the improvement of diagnostic techniques and greater awareness on PD clinical symptoms. As our data came from the two main French laboratories involved in PD diagnosis and the French Pompe registry, we could assume that this cohort of 246 patients represented almost the entire population of late-onset PD in France. Therefore, the frequency of late-onset PD was estimated around 1/69,927 newborns. This result was extrapolated from clinical data of adult patients, thus presenting signs or symptoms of the disease, and not from population-based studies. We think that this estimate is realistic, because it encompasses all the diagnosed patients in France during a long observational period (15 years). However, it has some obvious limitations: (1) it does not include potential asymptomatic or presymptomatic patients; (2) it does not consider immigration, old diagnoses, and deaths; (3) we used the average number of newborns as denominator to calculate the incidence of a late-onset disease. By comparison, other studies performed either with enzymatic newborn screening or genetic screening reported a frequency of 1/26,466 in Taiwan (Chien et al. 2011) and 1/57,000 in The Netherlands (Ausems et al. 1999), respectively. These epidemiologic studies also have limitations. For example, the genetic screening may overestimate the number of patients that will become symptomatic (as discussed above, the most frequent mutation in Caucasian patients, c.-32-13 T>G, is rarely seen in homozygous state in symptomatic patients, and it may be associated with a normal phenotype). Moreover, these studies were performed in more restricted populations and not in a large nationwide study covering a long observational period.
The mean age at diagnosis in our cohort (43 years) was higher compared to other published data (Hagemans et al. 2005; Winkel et al. 2005; Palmer et al. 2007; Remiche et al. 2014). The mean diagnostic delay in the last 20 years in France remained stable, around 9 years and was quite similar to other registries: 6 to 11 years (Winkel et al. 2005; Palmer et al. 2007; Kishnani et al. 2013; Remiche et al. 2014). This delay confirms that PD is a challenging diagnosis due to the high variability of symptoms and age at onset in late-onset PD, to the presence of atypical phenotypes and possible atypical histopathological features. Furthermore, late-onset PD is a very slow-evolving disease that can manifest with minimal signs in early adolescence before disease onset. Moreover, biases in the identification and annotation in medical records of the very first symptoms can be partially responsible for this long diagnostic delay. Clearly, this delay remains a big challenge in PD, since enzyme replacement therapy (ERT) is available and probably offers a better outcome when started earlier (Strothotte et al. 2010; van der Ploeg et al. 2010; Chien et al. 2011; Angelini et al. 2012). The detection of presymptomatic patients (7.8% of total diagnosis in the last 5 years in our study) could be facilitated in the future due to the increased knowledge on PD and development of miniaturized tests (dried blood spots) for the measurement of GAA activity. This will certainly improve the diagnostic work-up and clinical follow-up of patients (Echaniz-Laguna et al. 2015). Moreover, newborn screening (NBS) which is already performed in some countries (Taiwan, USA, Italy…) could also facilitate diagnosis and early treatment. However, some drawbacks need to be considered such as difficulties to predict phenotype and age at disease onset and false positives due to pseudodeficiency variants (Bodamer et al. 2017).
In our cohort, there was no straightforward relationship between genotype and age at disease onset. The c.-32-13T>G mutation was generally associated with onset in adulthood, but it could also be observed in late-onset PD patients presenting clinical onset in childhood (15 patients in our series with age at disease onset ranging from 2 to 16 years). Individuals with the same genotype presented first symptoms either in adulthood or childhood. This correlated with previous reports describing families with late-onset PD siblings and substantially variable phenotypes (Wens et al. 2013). This was probably due either to genetic factors (GAA polymorphisms, ACE, or ACTN3 variants) or environmental disease-modifying factors (De Filippi et al. 2014; Kroos et al. 2007; Kroos et al. 2012).
Conclusion
We reported molecular and epidemiologic data from the largest cohort of late-onset PD patients included in a nationwide study covering more than 40 years of this challenging diagnosis. We demonstrated high clinical and molecular variability in late-onset PD and estimated its frequency around 1/69,927 in France. PD diagnosis still remains difficult, as PD is a rare disease, with a heterogeneous and non-specific phenotype. An increased awareness of clinicians is needed to decrease the delay between onset and diagnosis.
References
Angelini C, Semplicini C, Ravaglia S et al (2012) Observational clinical study in juvenile-adult glycogenosis type 2 patients undergoing enzyme replacement therapy for up to 4 years. J Neurol 259:952–958
Ausems MG, Verbiest J, Hermans MP et al (1999) Frequency of glycogen storage disease type II in The Netherlands: implications for diagnosis and genetic counselling. Eur J Hum Genet 7:713–716
Ausems MG, ten Berg K, Sandkuijl LA et al (2001) Dutch patients with glycogen storage disease type II show common ancestry for the 525delT and del exon 18 mutations. J Med Genet 38:527–529
Bodamer OA, Scott CR, Giugliani R, Pompe Disease Newborn Screening Working Group (2017) Newborn screening for Pompe disease. Pediatrics 140:S4–S13
Chan J, Desai AK, Kazi ZB, Corey K, Austin S, Hobson-Webb LD, Case LE, Jones HN, Kishnani PS (2017) The emerging phenotype of late-onset Pompe disease: a systematic literature review. Mol Genet Metab 120:163–172
Chien YH, Lee NC, Huang HJ, Thurberg BL, Tsai FJ, Hwu WL (2011) Later-onset Pompe disease: early detection and early treatment initiation enabled by newborn screening. J Pediatr 158:1023–1027
Dardis A, Zanin I, Zampieri S et al (2014) Functional characterization of the common c.-32-13T>G mutation of GAA gene: identification of potential therapeutic agents. Nucleic Acids Res 42:1291–1302
De Filippi P, Saeidi K, Ravaglia S et al (2014) Genotype-phenotype correlation in Pompe disease, a step forward. Orphanet J Rare Dis 9:102
Echaniz-Laguna A, Carlier RY, Laloui K et al (2015) Should patients with asymptomatic Pompe disease be treated? A nationwide study in France. Muscle Nerve 51:884–889
Güngör D, Reuser AJ (2013) How to describe the clinical spectrum in Pompe disease? Am J Med Genet A 161A:399–400
Hagemans ML, Winkel LP, Van Doorn PA et al (2005) Clinical manifestation and natural course of late-onset Pompe’s disease in 54 Dutch patients. Brain 128:671–677
Hagemans ML, Hop WJ, Van Doorn PA, Reuser AJ, van der Ploeg AT (2006) Course of disability and respiratory function in untreated late-onset Pompe disease. Neurology 66:581–583
Herzog A, Hartung R, Reuser AJ et al (2012) A cross-sectional single-centre study on the spectrum of Pompe disease, German patients: molecular analysis of the GAA gene, manifestation and genotype-phenotype correlations. Orphanet J Rare Dis 7:35
Hirschhorn R, Huie ML (1999) Frequency of mutations for glycogen storage disease type II in different populations: the delta525T and deltaexon 18 mutations are not generally “common” in white populations. J Med Genet 36:85–86
Hirschhorn R, Reuser AJ (2001) Glycogen storage disease type II: acid alpha-glucosidase (acid maltase) deficiency. In: Scriver C, Baudet A, Sly et al (eds) The metabolic and molecular bases of inherited diseases. McGraw-Hill, New York, pp 3389–3420
Hoefsloot LH, Hoogeveen-Westerveld M, Reuser AJ, Oostra BA (1990) Characterization of the human lysosomal alpha-glucosidase gene. Biochem J 272:493–497
Huie ML, Chen AS, Tsujino S et al (1994) Aberrant splicing in adult onset glycogen storage disease type II (GSDII): molecular identification of an IVS1 (-13T>G) mutation in a majority of patients and a novel IVS10 (+1GT>CT) mutation. Hum Mol Genet 3:2231–2236
Kishnani PS, Hwu WL, Mandel H et al (2006) A retrospective, multinational, multicenter study on the natural history of infantile-onset Pompe disease. J Pediatr 148:671–676
Kishnani PS, Amartino HM, Lindberg C et al (2013) Timing of diagnosis of patients with Pompe disease: data from the Pompe registry. Am J Med Genet A 161A:2431–2443
Kroos MA, Van der Kraan M, Van Diggelen OP et al (1995) Glycogen storage disease type II: frequency of three common mutant alleles and their associated clinical phenotypes studied in 121 patients. J Med Genet 32:836–837
Kroos MA, Pomponio RJ, Hagemans ML et al (2007) Broad spectrum of Pompe disease in patients with the same c.-32-13T>G haplotype. Neurology 68:110–115
Kroos M, Pomponio RJ, van Vliet L et al (2008) Update of the Pompe disease mutation database with 107 sequence variants and a format for severity rating. Hum Mutat 29:E13–E26
Kroos M, Hoogeveen-Westerveld M, van der Ploeg A, Reuser AJ (2012) The genotype-phenotype correlation in Pompe disease. Am J Med Genet C Semin Med Genet 160C:59–68
Laforet P, Nicolino M, Eymard PB et al (2000) Juvenile and adult-onset acid maltase deficiency in France: genotype-phenotype correlation. Neurology 55:1122–1128
Laforêt P, Laloui K, Granger B et al (2013) The French Pompe registry. Baseline characteristics of a cohort of 126 patients with adult Pompe disease. Rev Neurol 169:595–602
Lek M, Karczewski KJ, Minikel EV et al (2016) Analysis of protein-coding genetic variation in 60,706 humans. Nature 536:285–291
Leslie N, Bailey L (2007) Pompe disease. In: Adam MP, Ardinger HH, Pagon RA et al (eds) GeneReviews®.Seattle (WA). University of Washington, Seattle, pp 1993–2018
Martiniuk F, Chen A, Mack A et al (1998) Carrier frequency for glycogen storage disease type II in New York and estimates of affected individuals born with the disease. Am J Med Genet 79:69–72
Montalvo AL, Bembi B, Donnarumma M et al (2006) Mutation profile of the GAA gene in 40 Italian patients with late onset glycogen storage disease type II. Hum Mutat 27:999–1006
Palmer RE, Amartino HM, Niizawa G, Blanco M, Pomponio RJ, Chamoles NA (2007) Pompe disease (glycogen storage disease type II) in Argentineans: clinical manifestations and identification of 9 novel mutations. Neuromuscul Disord 17:16–22
Pompe Disease Diagnostic Working Group, Winchester B, Bali D et al (2008) Methods for a prompt and reliable laboratory diagnosis of Pompe disease: report from an international consensus meeting. Mol Genet Metab 93:275–281
Raben N, Nichols RC, Martiniuk F, Plotz PH (1996) A model of mRNA splicing in adult lysosomal storage disease (glycogenosis type II). Hum Mol Genet 5:995–1000
Rairikar MV, Case LE, Bailey LA et al (2017) Insight into the phenotype of infants with Pompe disease identified by newborn screening with the common c.-32-13T>G “late-onset” GAA variant. Mol Genet Metab 122:99–107
Remiche G, Ronchi D, Magri F et al (2014) Extended phenotype description and new molecular findings in late onset glycogen storage disease type II: a northern Italy population study and review of the literature. J Neurol 261:83–97
Reuser AJ, Verheijen FW, Bali D et al (2011) The use of dried blood spot samples in the diagnosis of lysosomal storage disorders - current status and perspectives. Mol Genet Metab 104:144–148
Strothotte S, Strigl-Pill N, Grunert B et al (2010) Enzyme replacement therapy with alglucosidase alfa in 44 patients with late-onset glycogen storage disease type 2: 12-month results of an observational clinical trial. J Neurol 257:91–97
van der Ploeg AT, Reuser AJ (2008) Pompe’s disease. Lancet 372:1342–1353
van der Ploeg AT, Clemens PR, Corzo D et al (2010) A randomized study of alglucosidase alfa in late-onset Pompe’s disease. N Engl J Med 362:1396–1406
Wens SC, van Gelder CM, Kruijshaar ME et al (2013) Phenotypical variation within 22 families with Pompe disease. Orphanet J Rare Dis 8:182
Winkel LP, Hagemans ML, van Doorn PA et al (2005) The natural course of non–classic Pompe’s disease; a review of 225 published cases. J Neurol 252:875–884
Acknowledgements
We are thankful to Armelle Guenegou-Arnoux for her help with statistical analyses.
We thank Genzyme-Sanofi and INSERM for the financial sponsorship of the French Pompe Registry.
French Pompe Registry Study Group:
A. Béhin2, B. Eymard2, S. Leonard-Louis2, T. Stojkovic2, G. Bassez2, P. G. Carlier4, K. Laloui4, G. Ollivier4, A. Canal4, J. Y. Hogrel4, H. Prigent19,20, C. Desnuelle9,10, J. Pouget11, M. Piraud21, A. L. Bedat-Millet22, F. Boyer23, Y. Castaing24, F. Chapon25, P. Cintas26, I. Durieu27, A. Lacour28, L. Feasson28, A. Furby28, D. Germain29, K. Benistan29, H. Journel30, V. Tiffreau31, C. Tard31, J. Deibener-Kaminsky32, A. Magot33, Y. Péréon33, M. C. Minot-Myhié34, A. Nadaj-Pakleza35, C. Nathier35, N. Pellegrini36, P. Petiot37, J. Praline38, D. Vincent39, D. Renard40, R. Y. Carlier41, F. Bouibede42, R. Juntas-Morales43, E. Krim44, E. Lagrange45, L. Magy46, M. Michaud47
20Service Physiologie et Explorations-Fonctionnelles, INSERM CIC 1429, AP-HP, Hôpital Raymond Poincaré, Garches, France
21Centre de biologie et pathologie Est, hospices civils de Lyon, Bron, France
22Centre de compétence de pathologie neuromusculaire, CHU Charles Nicolle, Rouen, France
23Service de médecine physique et de réadaptation, CHU de Reims, France
24Service de réanimation, CHU de Bordeaux, Bordeaux, France
25Centre de compétence des maladies neuromusculaires, CHU de Caen, France
26Centre SLA et maladies neuromusculaires, CHU de Toulouse-Rangueil, Toulouse, France
27Service de médecine interne, centre hospitalier Lyon Sud, Pierre-Bénit, France
28Centre de référence des maladies neuromusculaires rares Rhône-Alpes, Hôpital Nord, CHU de Saint-Etienne, France
29Service de génétique médicale, Hôpital Raymond-Poincaré, Garches, France
30Génétique médicale, centre hospitalier Bretagne-Atlantique, Vannes, France
31CHRU de Lille, centre de référence des maladies neuromusculaires de Lille, Lille, France
32Centre de référence des maladies héréditaires du métabolisme de Nancy, hôpitaux de
33Centre de référence des maladies neuromusculaires Nantes-Angers, Hôtel Dieu, Nantes, France
34Service neurologie, CHU de Rennes, Rennes, France
35Centre de référence des maladies neuromusculaires Nantes/Angers, Service de neurologie, CHU d’Angers, Angers, France
36Service de soins de suite et de réadaptation neurologie, GHI du Vexin, Aincourt, France
37Centre de référence maladies neuromusculaires de la région Rhône-Alpes, hôpital de la Croix-Rousse, Lyon, France
38Centre de compétence des maladies neuromusculaires, CHRU de Tours, Tours, France
39Service de neurologie, groupe hospitalier La Rochelle - Ré - Aunis, La Rochelle, France
40Department of Neurology, Nîmes University Hospital, 4 Rue du Pr Debré, 30029, Nîmes, France
41Department of Medical Imaging, Hôpitaux universitaires Paris Ile-de-France Ouest, Hôpital Raymond Poincaré, Garches, France
42Service de Médecine Interne, Hôpital Porte Madeleine, Orléans, France
43Clinique du motoneurone et pathologies neuromusculaires, CHRU de Montpellier, Montpellier, France
44Service de neurologie, Hôpital F. Mitterrand, 4 bd Hauterive, 64046 Pau, France
45Pôle psychiatrie, neurologie et rééducation neurologique, clinique de neurologie, CHU de Grenoble, 38000 Grenoble, France
46Department of Neurology, Reference Center for Rare Peripheral Neuropathies, University Hospital of Limoges
47Department of Neurology, Central’s Hospital, Nancy 54000, France
Funding
Funding for the set up and maintenance of the French Pompe registry has been provided by Association Française contre les Myopathies (AFM), Association Francophone des Glycogénoses (AFG), Institut National de la Santé et de la Recherche Médicale (INSERM), Institut de Veille Sanitaire (InVS) and Sanofi Genzyme Corporation.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Pr Pascal Laforêt received grants and honorarium from Genzyme-Sanofi, and is a member of the board of International Pompe Registry.
C. Semplicini, P. Letard, M. De Antonio, N. Taouagh, B. Perniconi, F. Bouhour, A. Echaniz-Laguna, D. Orlikowski, S. Sacconi, E. Salort-Campana, G. Sole, F. Zagnoli, D. Hamroun, R. Froissart, and C. Caillaud declare that they have no conflict of interest.
Animal rights
This study does not use animals.
Additional information
Communicating Editor: Manuel Schiff
Electronic supplementary material
Figure S1
Description of the PD patient cohorts studied. (PNG 315 kb)
Figure S2
Mutation spectrum in late-onset PD patients diagnosed in France. Newly described mutations are in bold. Missense mutations and in-frame small deletions are shown below and other mutations above the GAA gene. Gray squares indicate exons. (PNG 6677 kb)
Table S1
(DOC 35 kb)
Table S2
(DOC 21 kb)
Table S3
(DOC 24 kb)
Rights and permissions
About this article
Cite this article
Semplicini, C., Letard, P., De Antonio, M. et al. Late-onset Pompe disease in France: molecular features and epidemiology from a nationwide study. J Inherit Metab Dis 41, 937–946 (2018). https://doi.org/10.1007/s10545-018-0243-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10545-018-0243-7