Abstract
Lynch et al., in an article in this issue, argue that an entire microbiome is rarely, if ever, the right target of analysis for causal explanations in microbiome research. They argue, using interventionist criteria of proportionality, specificity and stability, for restricting causal claims to the smallest subset of microbes—a causal core—that generate the effect of interest. A further question remains: what kind of interactions generate a consortium of microbes that can operate as causal agents in this manner? Here I introduce two possible kinds of such consortia: ‘trojan horses’ and ‘syntrophic’ individuals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The details of causal health claims emerging from human-associated microbiome research tend to be vague due to the limitations of current experimental techniques. When translated into health advice, nothing beyond broad proscriptions and recommendations with dubious efficacy for individual patients can be responsibly offered for most cases. In their penetrating analysis of the limitations of the causal explanations produced by microbiome research to date, Lynch et al. (2019) unmask a few of the culprits leading to this vagueness, as I have described it. I will focus on two such sources of vagueness.
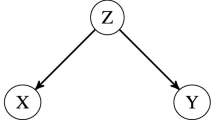
First, explanations that take whole human-associated microbiomes to be relevant causal agents invariably pull in too many background conditions that are not difference-makers. This leads to a loss of specificity regarding what actually was crucial for bringing about the effect under study. The inability to be specific reduces the ability to make accurate predictions across the wide variability in background conditions that come along with human–microbiome interactions in particular individuals.
Second, setting an explanatory target that is too general tends to produce explanations that are uninformative or ill-suited for making interventions. Trying to provide the causal explanation for such variable conditions as obesity or depression is like trying to provide the cause of wars. Generalizations about the cause of such complex and variable phenomena will need to be at such an abstract and high level that they will pass over the causal details that are important for intervening in or fully explaining any particular instance of that phenomena. The resulting explanations are too disproportionate and non-specific to account for the differences found at the scale of individuals.
Lynch et al. advocate for a more fine-grained approach using an interventionist framework of causation and related criteria of proportionality, specificity, and stability. Ideally, researchers should be moving away from whole-microbiome explanations and zeroing in on the particular mechanisms or taxa that are producing the effects of interest. If this approach is either not possible or not desirable, then which feature of a microbiome that is being taken as explanatory should be made clear. They offer up four such criteria: composition, function, outcome, or a ‘causal core’ group of microbes.
Their approach and the resulting prescriptions seem exactly right when it comes to searching for microbiome causal explanations. But given the nature of such a broad overview, a lot more can be said. For one, C. difficile might end up being a (relatively) easy case compared to the bulk of microbiome-related causal explanations. It follows many of the familiar rules for causal explanations in single-microbe studies. The disease is caused by a single organism and cured by inhibition or displacement. In this case by other microbes or an entire microbiome. The target effect variable, curing C. difficile, is clear and the pertinent causal chain is most likely direct interactions between microbes rather than causal chains mediated through the body, like in obesity or depression.
Cases like C. difficile might end up being rare in microbiome studies with their current exemplar status emerging because they were more easily experimentally accessible due to the outsize effects of one microbe. One significant difficulty in generating proportionate causal explanations in microbiome studies looks to be that the relevant causal variables will be at the level of a consortium of microbes, the ‘causal core’, and not at the level of single microbes. I predict that picking out and identifying those groups that form the relevant ‘causal cores’, along with the processes by which they are assembled and maintained, will be the primary challenge for human-microbiome health studies going into the future. I don’t take this to be a particularly unique claim, seeing similarities in recent microbiome research review articles such as Hall et al. (2018).
So what kind of thing is a ‘causal core’? More specifically, what might the interactions between the different microbes look like that generate enough cohesion to work as singular causal agent rather than just a set of independent causes jointly sufficient to bring about the effect. I will explore what I think are two plausible kinds of cases.
In the summer of 1924, Dr. Frank Schofield began investigating an equine disease epidemic—called ‘horse cholera’ by the local old-timers—that appeared to be confined to parts of just two counties in southern Ontario.Footnote 1 The disease would go through the horse populations every year, but only for the 2–3 weeks starting around mid-July. Horses with an acute form of the disease would usually die 7–10 days after onset. Schofield was convinced by the symptoms that the disease was due to a bacterial infection and began transmissibility experiments. Strangely, the horses did not appear to transmit the disease to each other. Healthy horses experimentally dosed with large amounts (one quart!) of diarrhea or given blood intravenously from acutely diseased horses developed only mild symptoms.
Even stranger was “that the disease always appears a few days after the May flies appear, and is at its worst by the time the May flies disappear”. Mayflies would descend like locusts, “piled up inches deep under electric lights”, so thick in the pastures that it was “impossible to walk without treading on them”. But the locally popular “May fly theory” of the disease also had a few problems. First, there are mayflies in many other places in Ontario where the disease is unknown, and the disease would linger for a bit even after the mayflies died. Furthermore, mayflies don’t bite horses, and the horses appeared only to accidently eat a few while out at pasture. And finally, experimentally feeding horses dead adult mayflies and molts collected from the pastures failed to produce the disease. The 1924 epidemic came to an end and Schofield’s transmissibility experiments came to a stop for a want of diseased materials. He left without any definitive answers.
Fifty years later in 1979, a news reporter coined the term “Potomac horse fever” to describe a recurring disease outbreak that happened every July in a narrow strip of land running along a 6-mile stretch of the Potomac River in Maryland. Later electron microscopy and molecular genetics work through the 80s and 90s finally allowed researchers to identify a culprit: Neorickettsia risticii, an obligate intracellular bacterium of trematodes and mammals. The bacterium makes its living inside the cells of digenetic trematodes, a class of parasitic flatworms. Trematodes, in turn, parasitize many different organisms over the course of their complicated life cycles. The first hosts of these particular trematodes are freshwater snails. The trematodes reproduce and metamorphosize inside the snail before leaving and infecting aquatic insects like mayflies, where they metamorphosize again. When the insects are eaten by bats, they migrate to the intestine and develop into adults. The adults lay eggs inside the bats’ intestinal cavity, and when the feces makes its way to freshwater the eggs hatch and infect snails to start the cycle anew. But in those few weeks where the mayflies are so thick that they coat the pastures, horses accidently ingest dying mayflies here and there. When that happens, the bacterium leaves the trematode cells and migrates into the horse’s intestinal epithelial and immune cells. The intestinal tissues appear to transform and no longer adequately reabsorb water and salt, causing diarrhea and lethargy, and 10–15 days later, death. Researchers were able to experimentally transmit the disease from horse to horse by isolating the bacterium from white blood cells that had been fractioned off and cultured, and then inoculating a susceptible pony. They also were able to do it by simply feeding horses snail secretions or living mature aquatic insects containing living trematodes. The trematodes are a living Trojan Horse that N. risticii requires to be able to sneak in and successfully invade a horse host. In this war the Trojan horses are worms, and the horses are not Trojan.
“Horse cholera” struck the Ontario area again between the years 1995 through 2010. Nearly 90 years after Schofield’s failed transmission studies, researchers were able to determine that “horse cholera” and “Potomac horse fever” are likely one and the same.
So what then is the cause of Potomac horse fever? In tightly controlled and artificial lab conditions, researchers can get direct transmission of the disease through the isolation, culturing, and subsequent inoculation of N. risticii. This indicates, by traditional experimental standards, that the proportional cause is at the level of the bacteria. But this is not how the disease is transmitted in natural environments, and that makes a difference for explaining the cause of Potomac Horse fever. If the explanatory target is discovering which particular organism causes the disease, then there is no such one organism.
I offer that the appropriately identified cause of Potomac horse fever is the nested trematode-bacteria consortium. Potomac horse fever is caused by a two-organism ‘causal core’: N. risticii and the Trojan worm it sneaks in on. One organism being present without the other won’t bring about the effect. But expanding further to include the trematode’s host is going too broad. Which of the many possible hosts the horse ingests doesn’t appear to make a difference in whether or not the disease develops. What is crucial is that the horse ingests an infected trematode sometime during the trematode’s lifecycle. The variation in trematode hosts over that time makes them a part of the causal background. The trematode-bacterium consortium is both a specific explanation for N. risticii infection and a proportional explanation for Potomac horse fever in natural settings. If the explanatory target is broadened to the cause of Potomac horse fever epidemics, then it is reasonable to say the proportionate cause is the further nested mayfly-trematode-bacterium consortium.
Trojan horse cases are one kind of multi-organism consortia that might satisfy the proportionality requirement of causal explanations. Similar cases involving no multi-cellular organisms are also to be found, and may not be that uncommon (Valdivia and Heitman 2007). The common sexually transmitted infection trichomoniasis is caused by the parasitic protozoan Trichomonas vaginalis. Its virulence may actually be dependent on the parasite itself being further infected by specific T. vaginalis viruses (Fichorova et al. 2012; Graves et al. 2019).
The case for the second potential kind of causal core regards what I will call ‘syntrophic individuals’.Footnote 2 ‘Syntrophy’ means cross-feeding, and refers more specifically to the relationship between two or more partner species where each species requires or lives off of the products of the other species. Syntrophy is primarily used in the context of bacterial interactions and has been thought of as an example of obligately mutualistic metabolisms, or in extreme cases, one metabolism spread between two organisms. We use the idea of ‘syntrophic individuals’ to pick out these cross-feeding obligately mutualistic consortia. One reason to call these special consortia individuals is because they interact causally with the environment at the level of the consortium. That is, they can influence the environment or are acted upon by the environment as a single entity.
There may be different kinds of processes that generate syntrophic individuals. One way is via Black Queen scenarios. The Black Queen hypothesis explains the evolution of obligate cross-feeding dependencies in microbes through adaptive gene loss (Morris 2012, 2015). Another way may be through “It’s the Song Not the Singer” (ITSNTS) scenarios (Doolittle and Booth 2016). ITSNTS hypothesizes about highly constrained microbial interaction patterns—described in terms of biochemical functions—that recur again and again due to the historical existence of those patterns generating the environmental conditions that ensure their reassembly. The microbial interaction networks propagate the very environmental conditions necessary for future instantiations of the network. A possible subset of ITSNTS networks that are locally constrained and persist via direct cross-feeding interactions would count as syntrophic individuals.
What I take to be important here is the possibility of recurring multi-organismal systems. If the persistence and self-maintenance happens at the level of the consortium and not at the level of the individual organismal parts, then the consortium may be a relevant level of individuality. The plausible mechanisms for generating syntrophic individuals are fragile enough that it seems unlikely that large numbers of different kinds of organisms could come together and be maintained in such a way (Skillings 2016). A system as complex as the human gut microbiome being such an individual seems implausible.
Returning to the trojan horse case of Potomac horse fever, it is the bacterium that is the proximate cause of changes in the gut that underlie the disease. The trematode plays no part in the disease mechanism. But it is a necessary part of the infection and transmission mechanism. Likewise, I expect there would be cases where only one member of a syntrophic individual is the proximate cause for the effect under investigation—say by the ongoing production of a particular metabolite or toxin. But if the survival and perpetuation of that microbe requires that it be part of a syntrophic individual in non-artificial conditions, then the disease or health state requires the entire consortium. It is that ‘causal core’ of organisms that is the proportionate cause of the state to be explained, and not the individual microbe.
Notes
The historical details used in this example come from Baird and Arroyo (2013).
This coining and account of individuals has been developed in conjunction with my coauthor and collaborator Leonardo Bich from the University of the Basque Country.
References
Baird JD, Arroyo LG (2013) Historical aspects of Potomac horse fever in Ontario (1924–2010). Can Vet J 54:565–572
Doolittle WF, Booth A (2016) It’s the song, not the singer: an exploration of holobiosis and evolutionary theory. Biol Philos 32:5–24
Fichorova RN et al (2012) Endobiont viruses sensed by the human host: beyond conventional antiparasitic therapy. PLoS ONE 7(11):e48418. https://doi.org/10.1371/journal.pone.0048418
Graves KJ et al (2019) Trichomonas vaginalis virus: a review of the literature. Int J STD AIDS 30:496–504
Hall EK et al (2018) Understanding how microbiomes influence the systems they inhabit. Nat Microbiol 3:977–982
Lynch KE, Parke EC, O’Malley MA (2019) How causal are microbiomes? A comparison with the Helicobacter pylori explanation of ulcers. Biol Philos. https://doi.org/10.1007/s10539-019-9702-2
Morris JJ et al (2012) The Black Queen Hypothesis: evolution of dependencies through adaptive gene loss. MBio. Published online May 2, 2012. http://dx.doi.org/10.1128/mBio.00036-12
Morris JJ (2015) Black Queen evolution: the role of leakiness in structuring microbial communities. Trends Genet 31(8):475–482
Skillings DJ (2016) Holobionts and the ecology of organisms: multi-species communities or integrated individuals? Biol Philos 31:875
Valdivia RH, Heitman J (2007) Endosymbiosis: the evil within. Curr Biol 17(11):R408–R410
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This comment refers to the article available at https://doi.org/10.1007/s10539-019-9702-2.
Rights and permissions
About this article
Cite this article
Skillings, D. Trojan Horses and Black Queens: ‘causal core’ explanations in microbiome research. Biol Philos 34, 60 (2019). https://doi.org/10.1007/s10539-019-9718-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10539-019-9718-7