Abstract
Objectives
The secretome of mesenchymal stem cells (MSCs), also called MSC-conditioned media (MSC-CM), represents one of the promising strategies for cellular therapy and tissue repair and regeneration. MSC-CM contains growth factors and cytokines that control many cellular responses during development and regeneration. Traditional 2D cell culture (2DCC) has previously been used to generate MSC-CM while evidence has proved that the physiological and biological behaviors of cells in 2DCC are significantly different from those in 3D cell culture (3DCC). Therefore, the objective is to compare the content of MSC-CM generated from traditional 2DCC and 3DCC using a 3D scaffold.
Methods
Adipose tissue-derived MSCs (AT-MSCs) were isolated from four donors (N = 4) and characterized according to the criteria stipulated by the International Society for Cell Therapy (ISCT). MSCs at passage 3 were grown in traditional 2DCC until 70% confluence and MSC-CM were collected at 24, 48, and 94 h. On the other hand, MSCs at passage 3 were grown on a polystyrene scaffold for 10 days to generate a 3D model of MSCs, and then MSC-CM was collected at 24, 48, and 94 h. MSC-CM from both 2DCC and 3DCC were analyzed for protein content using ELISA. Haematoxylin eosin (HE) staining and immunofluorescence (IF) were used to characterize the 3DCC of MSCs.
Results
MSCs from 2DCC were fibroblast like cells, and flow cytometry showed they were positive for CD73 and CD105 while being negative for CD14, CD19, and HLA-DR. They were also able to differentiate into adipocytes, osteoblasts, and chondrocytes. HE and IF showed that MSCs formed 3D model structures on the polystyrene scaffold. MSC-CM collected from both 2DCC and 3DCC contained growth factors, e.g., platelet derived growth factor (PDGF-AB), transforming growth factor-1 (TGF-1), hepatocyte growth factor (HGF), stromal derived factor-1 (SDF-1), interleukin 1 (IL-1), and interleukin 6 (IL-6). Concentrations of biomolecules secreted by MSCs in 3DCC were significantly higher than in 2DCC.
Conclusion
It could be concluded that 3DCC of MSCs using a polystyrene scaffold is a novel approach to generate MSC secretome for therapeutic applications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mesenchymal stem cells (MSCs) were first discovered in 1968 by Alexander Friedenstein et al. (1968). They could be isolated from a variety of tissue sources from the adult human body (Hass et al. 2011). Bone marrow (BM), adipose tissue (AT), peripheral blood (PB), umbilical cord (UC), cord blood (CB), and placenta are primary sources of MSCs. AT-MSCs represent a promising tool for cellular therapy due to their ease of access, diversity, differentiation and proliferation capacity and immunomodulatory potentials in suppression of inflammatory responses (Shi et al. 2018). The potential of AT-MSCs in regenerative medicine and disorder treatment has been illustrated by their secretome which contain many biomolecules including growth factors, cytokines and extracellular vesicles that support cell migration, proliferation, differentiation, regeneration and development (Trzyna and Banaś-Ząbczyk 2021). Some 36 cytokines have been reported to be released by MSCs which act in concert to promote the regeneration and development (Hwang et al. 2009). For example, MSCs produce soluble factors play a vital role in development and regeneration and regulate cellular responses, such angiogenesis, tissue remodeling, haemostasis, inflammation, proliferation and migration. MSC secretome has also been reportedly utilized in many mechanisms of immunomodulation (Weiss and Dahlke 2019). In addition, MSCs exert antimicrobial activity via the secretion of the antimicrobial peptide LL‐37 thereby preventing wound infection (Al-Shaibani et al. 2016). In spite of the importance of MSC secretome, to date the vast majority approaches to collect their secretome have been achieved in traditional 2D cell culture when MSC are grown on a plastic surface. Although, these assays are advantageous as they are simple, quick, and inexpensive when compared to large-scale 2DCC using robotics or scale out approaches, they still have many disadvantages when compared to 3D culture (Edmondson et al. 2014). For instance, cells in 2D culture differ morphologically and physiologically from cells in 3D culture (Baharvand et al. 2006). Also, cells in 2D culture lack the criteria of being surrounded by cellular elements and extracellular matrix as in an in vivo environment, whereas 3D culture mimics this habitat and offers the cultured cells, to some extent, an environment mimicking in vivo conditions including the growth of cells floating in culture media (Bhadriraju and Chen 2002). Additionally, 2D culture does not enable adequate exposure of the cells to the tested drug or substance of interest resulting in false, non-predictive and misleading data (Birgersdotter et al. 2005). Therefore, there is an urgent need to collect MSC secretome in 3D cell culture environment to assess the differences in concentration of biomolecules compared to 2DCC for further uses in therapeutic applications. 3DCC include three main platforms which are microcarriers, spheroids and 3D scaffolds. Microcarrier culture is used for cell expansion in vitro, while spheroids and 3D scaffolds are widely applied tissue engineering, cancer studies and cellular function (Mirbagheri et al. 2019). Previous studies by (Redondo-Castro et al. 2018; Miranda et al. 2019) generated MSC secretome using 3D spheroid culture. This type of culture is characterized by ability to obtain mature spheroid within few days with a high efficiency, performance, reproducibility and survival and homing capacities (Kouroupis and Correa 2021). However, spheroid culture has disadvantages such as shrinkage of the spheroid within time i.e., spheroid size at day 6 was significantly smaller than day 3 (Redondo-Castro et al. 2018) which mean cell survival might be limited to few days. Another disadvantage is using gelatin from animal materials which may interfere with the secretome of MSCs. Additionally, spheroid culture compacts the cells without extracellular matrix (ECM) in between cells which might affect their behavior (Bresciani et al. 2019). Moreover, spheroid shape change cell morphology and this is another issue that may affect MC behavior and impact their secretome (Tietze et al. 2019). Most scaffolds are biomaterials derived from animals which are characterized by a high level of diversity, as well as environmental and ethical considerations. Therefore, scaffolds were replaced with either natural polymers such as decellularized plant tissue, chitin/chitosan, and recombinant collagen or synthetic polymers such as polystyrene (Campuzano and Pelling, 2019). Decellularized plant tissue offers a diverse range of biochemical, topographical, and mechanical properties; chitin/chitosan-based scaffolds have shown synergistic bactericidal effects and improved cell–matrix interaction; recombinant collagen, unlike the other two, has the potential to closely resemble native tissue; and finally, polystyrene which can be processed more easily than natural polymers with high versatility properties (Hickey et al. 2018). The 3D culture used in this study utilized polystyrene 3D scaffold overcoming these problems since MSCs were able to form 3D tissue like structure with ECM in between cells that enable MSCs to grow without any stress that could alter their identity. This research studied a panel of growth factors and cytokines that play crucial roles in cellular responses during development, regeneration and immunological responses such as cell immobilization, migration, proliferation and differentiation. This panel of growth factors and cytokines included platelet derived growth factor (PDGF-AB), transforming growth factor-β1 (TGF-β1), hepatocyte growth factor (HGF), stromal derived factor-1 (SDF-1), interleukin 1 (IL-1) and interleukin 6 (IL-6) which play vital roles in majority of important biological processes such as development, regeneration, healing, immunological responses and other cellular responses such cell cycle, migration, proliferation and differentiation (Al-Shaibani et al. 2016).
Methods
Cell culture
All cell culture experiments were performed in class II cabinets to reduce the risk of infection and contamination. All cells and 3D models were incubated at standard culture conditions (SCC), which were provided by a humidified incubator adjusted to 37 °C, ≈ 20% O2 and 5% CO2. Unless otherwise stated, all culture conditions set out in this study for cell culture and cell experiments were SCC. Isolated MSCs were grown at SCC in DMEM-F10, which stands for Dulbecco's Modified Eagle Medium (Sigma/UK), and is composed of 500 ml of DMEM supplemented with 10% fetal calf serum (FCS) (Sigma/UK), 4% of 200 mM l-Glutamine, 1% of 100 IU/ml penicillin, and 100 µg/ml streptomycin (PS) (Sigma/UK). To split cells, old media was aspirated, and cells were rinsed with phosphate buffered saline (PBS), trypsinized with 0.25% trypsin 1X and incubated for 10 min. A quantity of 10 ml of DMEM-F10 was added to prepare the cell suspension and centrifuged at 1500 rpm for 5 min. The supernatant was discarded, and cells were counted, and a cell number of 0.3 × 106 was seeded per T175 flask (175 cm2). A quantity of 15–20 ml of fresh DMEM were added to the flask and incubated under SCC. Trypan blue stain was used to assess viability of cells. A volume of 10 μl trypan blue was mixed with 10 μl of cell suspension. A quantity of 10 μl of this mixture was transferred to a Neubauer chamber and covered with a cover slip prior to counting under the microscope (Sandell and Sakai 2008). Cell count and viability were estimated using Eqs. (1) and (2).
Isolation and characterization of adipose tissue derived mesenchymal stem cells (AT-MSCs)
All protocols involving human participants were in accordance with the ethical standards of the Institutional Research Committee, with full local research ethics approval from the Council of the College of Biotechnology, Al-Nahrain University. A written informed consent was agreed and signed by each donor separately. Excess adipose (fat) tissue from 4 donors (N = 4) were obtained from liposuction procedures for abdominoplasty reduction. According to (Bernacki et al. 2008) a volume of 4–5 ml adipose tissue was added into 15-ml tubes with 4 ml of 0.075% type I collagenase solution. Minced tissue and lipoaspirate were drawn up and incubated together with agitation at 37 °C for 30 min. A volume of 4 ml of DMEM-F10 was then added to the aspirate to inhibit collagenase activity and centrifuged at 5000×g for 10 min to obtain a cellular pellet dense with MSCs, and the supernatant was discarded using a sterile pipette without disturbing the pellet. To lyse red blood cells, the pellet was resuspended in 2 ml of 160 mM of NH4Cl and incubated at room temperature (RT) for 10 min. The cell fraction was then transferred to new centrifuge tubes and spun at 1200 g for 10 min before being resuspended in DMEM-F10 and filtered through a Falcon® 100 m cell strainer. Cell suspension was seeded onto culture flasks containing an appropriate volume of DMEM-F10 medium and incubated at SCC with regular changes of medium (three times per week) until passage to the next passage upon reaching 80% confluence using the standard trypsinization method. All MSC samples at passage 3 were characterized by flow cytometry according to the International Society for Cell Therapy (ISCT) criteria (Dominici et al. 2006) using specific antibodies (BD Bioscience, UK) against CD14, CD19, and CD34 (FITC), CD73 (PE), CD90 (PerCPCy5.5), CD105 (APC), and HLA-DR (APC H7) and the cells were analysed using the BD FACSCanto™ II (BD Biosciences) using single parameter analysis since cells were treated with a total number of 0.04 × 106 events per sample using single antibody separately. Isotype-stained cells were also used separately. Flowing software v2.5.1 was used to gate cells depending on their stain. Briefly, the segregation step (Fig. 2A) included the exclusion of cell debris from the total analyzed cells. Live cells (DAPI negative) were used to segregate antibody-stained cells according to the specified wave length for each antibody which compared to its isotype for further overlapping plotting. MSC tri-lineage differentiation (adipocyte, osteoblast and chondrocyte) was confirmed using differentiation media (Miltenyi Biotec, Germany) i.e., adipocyte differentiation media (ADM) for 15 days, osteoblast differentiation media (ODM) for 21 days, and chondrocyte differentiation media (CDM) for 21 days, respectively, following standard protocols (Akiyama et al. 2012).
Construction and evaluation of 3D-MSC model (3D-MSC)
The basis of this model is the CytoBuilder scaffold developed by (Al-Shaibani 2020). This scaffold was made of polystyrene, which is widely used to synthesize plasticware for cell culture. The CytoBuilder scaffold was examined under a scanning electronic microscope and revealed grooves with diameters of 50–100 µm, which enable cells to spread through the scaffold. In addition, the thickness of the scaffold ranges from 500 to 700 µm. Both porosity and thickness are important parameters to establish a 3DCC. Before seeding cells, the CytoBuilder scaffold was activated with 70% ethanol for one minute, treated with DMEM-F10 for one minute, fixed in 6 well plates and incubated under SCC until required. To establish 3D MSC model, 2 × 106 cells were suspended in 100 µl DMEM-F10, seeded onto the CytoBuilder scaffold and incubated at SCC for 90 min. Then, 9 ml of DMEM-F10 was added to the well and covered the entire scaffold, and the culture was incubated at SCC for 10 days, with regular feeding of the 3D culture with DMEM-F10 every two days. Feeding the culture included withdrawal of old medium from the well using a micropipette and then 9 ml of fresh medium was gently added on the inside wall of the well without disturbing the cells on the CytoBuilder scaffold. MSC secretome (MSC-CM) was collected at 24, 48, and 96 h after creating the 3D culture. The 3D MSC model was then sectioned by a microtome adjusted to 4 µm, and the sections were kept in a water bath at 40 °C for 2–3 min. The slides were then heated in an oven at 60 °C overnight. The sections were deparaffinized and rehydrated with xylene, 100% ethanol, 95% ethanol, 70% ethanol, and deionized water then stained with haematoxylin for 7 min at room temperature. Sections were then rinsed with deionized water, and stained with eosin staining for 30 s, followed by 95% ethanol, 100% ethanol, and xylene to evaluate the formation of a 3D MSC model. MSC 3D models were also stained with Alcian blue (Merk/UK) overnight and washed with distilled water. Slides were then examined by a bright field microscope (Olympus/Japan) to detect the formation of ECM, mainly glycosaminoglycan.
Collection and analysis of MSC secretome (MSC-CM)
The MSC secretome (MSC-CM) from both cultures was collected in standard DMEM serum free supplemented with 4% of 200 mM l-Glutamine, 1% of 100 IU/ml penicillin, and 100 µg/ml streptomycin (PS) (Sigma/UK). In the case of 2D culture, when cells reached 80% confluence, it was considered day zero time point, old media was discarded, and a confluent monolayer of MSC culture was washed three times with PBS and fresh DMEM serum free was added to the culture. MSC-CM was collected from four samples (N = 4) seeded in 2DCC on day one, day two, and day four and is referred to as CM24-2D, CM48-2D, and CM96-2D. On the other hand, in 3D culture, MSCs formed a tissue like structure within 10 days, which is considered the day zero time point. On day zero, the old media was discarded and 3D MSC model was washed three times with PBS and fresh DMEM serum free was added to the culture. Following days, MSC-CM was collected from four samples (N = 4) of 3D MSC models at day one, two, and four and was referred to as CM-24-3D, CM48-3D and CM96-3D. The MSC-CM from 2DCC and 3D MSC model was collected and filtered using a 0.2 µm filter unit before being analyzed by ELISA for growth factors and cytokines such as platelet derived growth factor (PDGF-AB: Cat No. EHPDGFAB), transforming growth factor-β1 (TGF-β1: Cat No. BMS249-4TEN), hepatocyte growth factor (HGF: Cat No. KAC2211), stromal derived factor-1 (SDF-1: Cat No. EHCXCL12A), interleukin 1 (IL-1: Cat No. EH254RB) and interleukin 6 (IL-6: Cat No. BMS213-2). All kits were purchased from (Life Technologies Thermo Fisher Scientific/US) and assays were performed according to protocols stated by the manufacturer company.
Immunofluorescence staining of the 3D-MSC model (3D-MSC)
Paraffin embedded sections of the 3D-MSC model were sectioned by the microtome adjusted to 4 µm, and the sections were kept in a water bath at 40 °C for 2–3 min. The slides were then heated in an oven at 60 °C overnight. The sections were dehydrated by washing for 5 min in each of xylene, 100% ethanol, 95% ethanol, 70% ethanol, and distilled water. For antigen retrieval, slides were placed in previously heated 10 mM citrate buffer, pH 6.0, in a microwave for 1 min and then left to cool at room temperature for 30 min. They were then washed in 5 mM Tris buffered saline (TBS), pH 7.6 for 5 min. The slides were permeabilized with 0.2% Triton-X for 10 min at room temperature. All sections were blocked by 10% goat serum (Abcam) in PBS for 10 min at room temperature and washed with Tris base solution (TBS) four times to remove the goat serum. The sections were stained with 100 µl of CD73-PE and 100 µl of CD105-APC separately and incubated at 4 °C for 30 min. Control slides were not stained but incubated with blocking solution instead. Sections were then washed four times with TBS for 2 min, stained with DAPI (1:1000), covered with DPX, left in the dark at room temperature overnight, and visualized the next day using a fluorescent microscope (Leica, Germany).
Statistical analysis
The data from the research was analysed by using means ± standard error of the mean (SEM) and a Two-way RM ANOVA test to determine significant differences between samples when P values were less than 0.05. Multiple comparisons were required to find differences between pairs of means with appropriate adjustment for multiple testing in every single condition during different time points in each separate experiment. Tukey's multiple comparisons test was used to detect variations, which were considered significant when the P value was less than 0.05. All types of analyses were achieved by GraphPad Prism software version 6.0.
Results
Characteristics of MSCs
The isolated MSCs were able to adhere to the plastic surface after 24 h of isolation and after 4 h in the next passages. Morphologically, they are longitudinal fibroblast-like cells with some processes as shown in (Fig. 1A). Additionally, the isolated MSCs showed the ability to differentiate in vitro into three lineages; adipogenic, osteogenic, and chondrogenic lineages when grown in specified differentiation media as shown in (Fig. 1 B, C, and D), respectively.
Morphology and differentiation potential of MSCs. A MSCs in passage 3 at 80% confluence. B MSC differentiation potential to develop lipid vacuoles after 18 days in ADM stained with oil red dye. C They were also able to differentiate into osteoblasts after three weeks of treatment with ODM because they formed calcium crystals that stained black after incubation with Von Kosa stain. D Moreover, they differentiated into chondrocytes when grown in CDM for 21 days and formed proteoglycan stained in bright blue. Magnification = 10×, scale bar = 50 µm
Under standard conditions for MSCs, the isolated MSCs (N = 4) expressed the stem cell markers CD73 (96.8 ± 1.7%), and CD105 (97.4 ± 1.4%). These samples minimally expressed CD14, CD19, and CD45 (1.0 ± 0.7%) and human leucocyte antigen (HLA-DR) (1.2 ± 0.8%) (Fig. 2B). In another word, more than 98% of MSCs were negative for the expression of CD14 (which is expressed by monocytes, macrophages, and endothelial progenitor cells), CD19 (a B-lymphocyte antigen), CD34 (a marker expressed by primitive haematopoietic stem cells), CD45 (a marker of all haematopoietic cells) and HLA-DR (Fig. 2C). The ISCT stated that these CD markers are expressed at certain ratios, i.e., CD73 and CD105 are expressed in 98% of the cell population; while CD14, CD19, CD45 and HLA-DR should be expressed in less than 2% of the cell population. In another word, cells that express CD73 and CD105 less than 98%, or CD14, CD19, CD45, and HLA-DR more than 2%, cannot be considered as stem cells and cannot be used for further investigations. These results confirm the identity of the isolated cells as MSCs as per the ISCT criteria as reported by (Dominic et al. 2006).
MSC phenotypic assay. A Representative scattering figures show a gating strategy which summarizes the path for segregating specific cell populations from the entire mixed population. All cells are a mixture of live and dead cells. Dead cells were excluded, and only live cells were used to extract the specific cell population. Cells were characterized for their phenotypic characteristics when comparing antibody-stained cells against isotype-stained cells. B Overlapping of antibody and isotype-stained cells which show positive and negative phenotypic markers expressed by AT-MSCs grown in DMEM-F10 at passage three. AT-MSCs showed compatibility of antibodies (blue line ) expressed by MSCs and their isotypes (red line). C MSC marker expression percentage: Over 95% of MSCs grown expressed CD73 and CD105, which were stained with PE and APC, respectively. 98% and over of these cells were negative for the expression of CD14, CD19, and CD45, which were stained with FITC. Also, over 98% of MSCs were negative for expression of HLA-DR antibody, which was stained with APC H7
Evaluation of 3D-MSC model (3D-MSC)
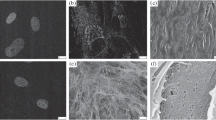
All models generated in this study (N = 4) were prepared by seeding AT-MSCs on the CytoBuilder scaffold for 10 days. As shown in (Fig. 3A), hematoxylin–eosin staining revealed that MSCs distributed within the scaffold and formed a tissue-like structure in which cells are distributed in a 3D environment that mimics an in vivo niche. Additionally, MSCs were able to adapt to the 3D scaffold and started to secrete extracellular matrix (ECM) represented by glycosaminoglycan (GAG) after 10 days of seeding MSCs on the scaffold, as shown in (Fig. 3B). To clarify the difference between the empty scaffold and the 3D-MSC model, (Fig. 3C) shows an empty scaffold stained with HE, which reveals negative staining of the empty scaffold because it has no cells that pick up the HE satins.
Formation of 3D-MSC model. A Hematoxylin–eosin (HE) staining shows 3D culture of MSCs at day 10 after seeding the MSCs over the CytoBuilder scaffold, revealing the formation of a cellular layer of MSCs that mimics an in vivo niche. After 1 week of seeding the cells, they spread and deeply penetrated the scaffold, forming a tissue-like structure. B MSCs secrete ECM in 3D culture. After 1 week of seeding, the cells represented by GAG were stained with Alcian blue, which is indicated by black arrows. C An empty CytoBuilder scaffold stained with HE shows a net of threads that are negative for HE staining. Scale bar = 100 µm
To assess the cytotoxic effect of the scaffold on the identity and viability of stem cells in the scaffold, expression of key biomarkers by MSCs (CD73 and CD105) was evaluated. As demonstrated in (Fig. 4 A and B), MSCs stained with CD73-PE antibody and CD105-APC antibody, respectively, invaded the scaffold and deeply distributed within 10 days of seeding the cells. Hence, the use of these phenotypic markers was to confirm that the MSCs retained their phenotypic characteristics and had not been affected by the scaffold, and that the DAPI stain was used as an indicator that cells penetrated the scaffold from the top to the bottom, and hence this is an indication there were no short-term cytotoxic effects as cells were able to migrate through the scaffold. These data suggest viability and mobility of MSCs in an environment mimic in vivo.
Immunofluorescence micrographs of 3D-MSC model. Micrographs show the growth and penetration of MSCs through the CytoBuilder scaffold after 10 days of seeding the cells and reveal that MSCs stained with CD73-PE antibody, stained in green (A), and CD105-APC antibody stained in green (B). MSCs spread and deeply penetrated the CytoBuilder scaffold within 10 days. Blue = DAPI stain (1:1000) in (1% BSA). Scale bar = 50 µm
Analysis of MSC secretome (MSC-CM)
MSCs secreted detectable levels of some growth factors and cytokines at different concentrations in both the 2DCC and 3D-MSC model, such as PDGF-AB, TGF-β1, HGF, SDF-1, IL-1, and IL-6. Multiple comparisons were investigated between MSC secretome using Tukey's multiple comparisons test. The first one compared concentrations of growth factors and cytokines collected from 2DCC at different time points. MSC-CM contained different concentrations of growth factors and cytokines collected from their culture at 24 h, with consistent secretion of these growth factors within this time frame until 48 h. Interestingly, there was a decrease in growth factor concentrations at time point 96 h. Two-way ANOVA revealed significant differences in concentrations of all studied growth factors and cytokines at time points of 24 h and 96 h. As shown in (Fig. 5A), PDGF-AB had significant depletion from 89.5 ± 14 ng/ml to 22.5 ± 3 ng/ml (P = 0.02), TGF-β1 concentration decreased from 106 ± 7 ng/ml to 30 ± 2 ng/ml (P = 0.03), HGF concentration dropped from 1397 ± 49 ng/ml to 278 ± 18 ng/ml (P = 0.0001), SDF-1 level decreased from 184 ± 4 ng/ml to 107 ± 7 ng/ml (P = 0.02), IL-1 concentration depleted from 170 ± 11 ng/ml to 82 ± 5 ng/ml (P = 0.01) and finally, IL-6 level decreased from 299 ± 26 ng/ml to 99 ± 16 ng/ml (P = 0.0001). The second compared between concentrations of growth factors and cytokines collected from 3DCC at different time points. MSC-CM collected from 3DCC contained consistent levels of the tested growth factors and cytokines within time change. Two-way ANOVA revealed no significant differences (P > 0.05) in concentrations of all studied growth factors and cytokines at time points 24, 48 and 96 h as shown in (Fig. 5B). The third comparison investigated differences between concentrations of the studied growth factors and cytokines collected from 2 and 3DCC at the same time points. Two-way ANOVA showed significant variations between concentrations of MSC secretome collected from both 2DCC and 3DCC. As shown in (Table 1A) and (Fig. 5C), at time point 24 h concentrations of target growth factors and cytokines collected from 3DCC were significantly higher than those collected from 2DCC. Additionally, at time point 48 h, concentrations of the studied growth factors and cytokines collected from 3DCC were also significantly higher than those collected from 2DCC as shown in (Table 1B) and (Fig. 5D). Moreover, concentrations of target growth factors and cytokines collected from 3DCC were significantly higher than those collected from 2DCC as shown in (Table 1C) and (Fig. 5E).
Analysis of MSC-CM content by ELISA. Concentrations of growth factors and cytokines secreted by AT-MSCs in both 2DCC and 3DCC at different time points (24, 48, and 96 h). A Concentrations of growth factors and cytokines collected from 2DCC at different time points show a significant decrease in concentrations of all target growth factors and cytokines at 96 h compared to 24 h. A Concentrations of growth factors and cytokines collected from 3DCC at different time points show no significant differences in concentrations of all target growth factors and cytokines at the different time points (24, 48, and 96 h). (C, D and E) Statistical comparisons show that concentrations of growth factors and cytokines collected from 3DCC are significantly higher than their counterparts collected from 2DCC at 24, 48, and 96 h, respectively. The data is represented as a mean of the concentration of a given growth factor and cytokine. N = 4, error bars = standard error of the mean (SEM)
Discussion
Over the last two decades, intensive attention has been paid and numerous studies have concentrated on using the secretome of stem cells as a strategy for cellular therapy, including wound healing, tissue repair, and immunomodulation. Previous studies compared secretome of MSCs in 2DCC against 3D spheroid culture (Bartosh et al. 2010; Ylöstalo et al. 2012; Redondo-Castro et al. 2018; Miranda et al. 2019; Kouroupis and Correa 2021). Whereas, to date there is no study has used 3D scaffold to collect MSC secretome and compare it with 2DCC; therefore, this study aimed to compare between secretome of MSCs collected from 2DCC and 3D MSC model using polystyrene scaffold. The biological behavior of cells in vivo is significantly different form their behavior in vitro and this difference is mainly attributed to 3D microenvironment in the living organism (Edmondson et al. 2014). It has been reported that MSC secretome is improved when they grow on extracellular matrix (ECM) scaffold and enhance tissue regeneration (Qiu et al. 2018). ECM play a pivotal role for successful growth of cells in vivo and enable the cells to communicate with other cells whereas in 2DCC cells lack the appropriate ECM and subsequently fail to exert their natural behavior as in vivo and further affect their secretome. Therefore, 3D scaffold could be used as an alternative or replacement to ECM to represent a space that provide mechanical support for cells to grow, adhere, proliferate and enable the cells to establish the proper spatial spreading for further cell–cell or cell-ECM communication (Lv et al. 2017). Therefore, the consistent secretions of growth factors and cytokines collected from 3DCC culture could be attributed to the 3D architecture which is later supported by secretion of ECM represented glycosaminoglycan secreted by MSCs. Additionally, ECM secreted by MSCs act as a bridge between cells that communicate them together keeping MSCs to stay at place and work without immobilization keeping energy and increasing their performance (Qiu et al. 2018). However, choosing the appropriate scaffold represent the most influential factors that impact cell behavior and biology. In this study the CytoBuilder polystyrene scaffold developed by (Al-Shaibani 2020) was used to grow MSCs and collect their secretome. MSCs grew well, penetrated the scaffold and formed a 3D tissue like structure. Additionally, expression of key MSC markers (CD73 and CD105) suggest that MSCs in the 3D culture retained their identity without changes in their stemness and characteristics which is an important feature should be taken into account when seeding MSCs in 3D culture and collect their secretome; whereas other studies achieved by Redondo-Castro et al. (2018) and Bresciani et al. (2019) who used 3D spheroid culture. MSC secreted growth factors and cytokines with concentrations significantly higher and more sustainable than those secreted in 2DCC at the same time points indicating the suitability of the selected type of scaffold for collecting MSC secretome. An interpretation for these results is the fact that the tissue architecture of 3DCC is more complex than 2DCC and cell–cell or cell-ECM communication present in the 3DCC (Desrochers et al.2014). Another interpretation is that cells in 3DCC culture grow as aggregates which sustain more nutrient and oxygen level thereby increase the performance of cells (Friedrich et al. 2009). Additionally, primary cells isolated from donors and further grown on 3D scaffold sustain their multicellular architecture of their parental tissue which led to the appropriate cell–cell and cell-ECM communication and cell proliferation rate is significantly higher in 3DCC than 2DCC which mean cell density of 3DCC will be higher than 2DCC and the outcome of secretome is significantly higher (Kapałczyńska et al. 2018). Furthermore, 3DCC is characterized by similar attributes of in vivo such as cellular topology, stimuli reception, signalling molecules, gene expression and metabolism (Marushima et al. 2011). Despite the fact that 3DCC is preferable over 2DCC, not all 3DCC types produce the same results. For the following reasons, 3D scaffold is preferred over 3D spheroid culture: Spheroid culture shrinks over time, as indicated by the fact that spheroid size at day 6 was much smaller than at day 3 (Redondo-Castro et al. 2018), suggesting that cell survival may be limited to a few days. Another issue is the use of animal-derived gelatin, which may interfere with the MSC secretome. Furthermore, eliminating the extracellular matrix (ECM) between cells in spheroid culture compacts cells, which may alter their activity (Bresciani et al. 2019). In addition, the spheroid form changes cell morphology, which is another element that could affect MSC activity and secretome. In summary, 3DCC represented by growing cells on scaffold is potentially a novel strategy and robust approach to collect MSC secretome for further cellular therapies leading us towards achieving main goals of tissue engineering and regenerative medicine. Additionally, the 3D model is able to remain in culture for prolonged period, which would allow repetitive and reproducible collection of cells secretome. However, more investigations are required to be achieved in this regard such as comparing different type of scaffolds for collecting secretome from MSCs and other stem cells, study the molecular similarities and variations between MSCs and other stem cells in 2DCC and 3DCC, investigate comprehensive panel of growth factors and cytokines collected from MSCs and other stem cells in both 2DCC and 3DCC, investigate the biological effect of 3DCC and scaffolds on proliferation and differentiation of MSCs and other stem cells.
Conclusion
This is the first study to evaluate variations in the MSC secretome generated from 2DCC and 3DCC. The developed 3D-MSC model secretes higher concentrations of growth factors and cytokines than those collected from traditional 2DCC, suggesting a novel approach could be used as a strategy for collecting MSC secretome for further therapeutic application.
References
Akiyama K, You Y-O, Yamaza T et al (2012) Characterization of bone marrow derived mesenchymal stem cells in suspension. Stem Cell Res Ther 3(5):40. https://doi.org/10.1186/scrt131
Al-Shaibani MBH, Dickinson A, Nong-Wang X et al (2016) Effect of conditioned media from mesenchymal stem cells (MSC-CM) on wound healing using a prototype of a fully humanised 3D skin model. Cytotherapy 19(5):e23–e24. https://doi.org/10.1016/j.jcyt.2017.03.062
Al-Shaibani MBH (2020) Manufacturing of a Novel scaffold to culture human and animal cells in 3 dimensional microenvironment. paper presented at the international Eurasian conference on biotechnology and biochemistry (BioTechBioChem), Ankara, Turkey. https://www.biotechbiochem.org
Baharvand H, Hashemi SM, Kazemi Ashtiani S, Farrokhi A (2006) Differentiation of human embryonic stem cells into hepatocytes in 2D and 3D culture systems in vitro. Int J Dev Biol 50(7):645–652. https://doi.org/10.1387/ijdb.052072hb
Bartosh TJ, Ylostalo JH, Mohammadipoor A et al (2010) Aggregation of human mesenchymal stromal cells (MSCs) into 3D spheroids enhances their antiinflammatory properties. Proc Natl Acad Sci USA 107(31):13724–13729. https://doi.org/10.1073/pnas.1008117107
Bernacki SH, Wall ME, Loboa EG (2008) Isolation of human mesenchymal stem cells from bone and adipose tissue. Methods Cell Biol 86:257–278. https://doi.org/10.1016/S0091-679X(08)00011-3
Bhadriraju K, Chen CS (2002) Engineering cellular microenvironments to improve cell-based drug testing. Drug Discov Today 7(11):612–620. https://doi.org/10.1016/S1359-6446(02)02273-0
Birgersdotter A, Sandberg R, Ernberg I (2005) Gene expression perturbation in vitro: a growing case for three-dimensional (3D) culture systems. Semin Cancer Biol 15(5):405–412. https://doi.org/10.1016/j.semcancer.2005.06.009
Bresciani G, Hofland LJ, Dogan F et al (2019) Evaluation of spheroid 3D culture methods to study a pancreatic neuroendocrine neoplasm cell line. Front Endocrinol. https://doi.org/10.3389/fendo.2019.00682
Campuzano S, Pelling AE (2019) Scaffolds for 3D cell culture and cellular agriculture applications derived from non-animal sources. Front Sustain Food Syst. https://doi.org/10.3389/fsufs.2019.00038
Desrochers TM, Palma E, Kaplan DL (2014) Tissue-engineered kidney disease models. Adv Drug Deliv Rev 69–70:67–80. https://doi.org/10.1016/j.addr.2013.12.002
Dominic M, Le-Blanc K, Mueller I et al (2006) Minimal criteria for defining multipotent mesenchymal stromal cells. Int Soc Cell Therapy Position Statement Cytotherapy 8(4):315–317. https://doi.org/10.1080/14653240600855905
Edmondson R, Broglie JJ, Adcock AF, Yang L (2014) Three-dimensional cell culture systems and their applications in drug discovery and cell-based biosensors. Assay Drug Dev Technol 12(4):207–218. https://doi.org/10.1089/adt.2014.573
Friedenstein AJ, Petrakova KV, Kurolesova AI, Frolova GP (1968) Heterotopic of bone marrow. Anal Precursor Cells Osteogenic Hematopoietic Tissues Transpl 6(2):230–247
Friedrich J, Seidel C, Ebner R, Kunz-Schughart LA (2009) Spheroid-based drug screen: considerations and practical approach. Nat Protoc 4(3):309–324. https://doi.org/10.1038/nprot.2008.226
Hass R, Kasper C, Bohm S, Jacobs R (2011) Different populations and sources of human mesenchymal stem cells (MSC): A comparison of adult and neonatal tissue-derived MSC. Cell Commun Signal 9:12. https://doi.org/10.1186/1478-811X-9-12
Hickey RJ, Modulevsky DJ, Cuerrier CM, Pelling AE (2018) Customizing the shape and microenvironment biochemistry of biocompatible macroscopic plant-derived cellulose scaffolds. ACS Biomater Sci Eng. https://doi.org/10.1021/acsbiomaterials.8b00178
Hwang JH, Shim SS, Seok OS et al (2009) Comparison of cytokine expression in mesenchymal stem cells from human placenta, cord blood, and bone marrow. J Korean Med Sci 24(4):547–554. https://doi.org/10.3346/jkms.2009.24.4.547
Kapałczyńska M, Kolenda T, Przybyła W et al (2018) 2D and 3D cell cultures: a comparison of different types of cancer cell cultures. Arch Med Sci 14(4):910–919. https://doi.org/10.5114/aoms.2016.63743
Kouroupis D, Correa D (2021) Increased mesenchymal stem cell functionalization in three-dimensional manufacturing settings for enhanced therapeutic applications. Front Bioeng Biotechnol. https://doi.org/10.3389/fbioe.2021.621748
Lv D, Hu Z, Lu L et al (2017) Three-dimensional cell culture: A powerful tool in tumor research and drug discovery (Review). Oncol Lett 14(6):6999–7010. https://doi.org/10.3892/ol.2017.7134
Marushima H, Shibata S, Asakura T et al (2011) Three-dimensional culture promotes reconstitution of the tumor-specific hypoxic microenvironment under TGFβ stimulation. Int J Oncol 39(5):1327–1336. https://doi.org/10.3892/ijo.2011.1142
Miranda JP, Camões SP, Gaspar MM et al (2019) The secretome derived from 3D-cultured umbilical cord tissue MSCs counteracts manifestations typifying rheumatoid arthritis. Front Immunol. https://doi.org/10.3389/fimmu.2019.00018
Mirbagheri M, Adibnia V, Hughes BR et al (2019) Advanced cell culture platforms: a growing quest for emulating natural tissues. Mater Horiz 6(1):45–71. https://doi.org/10.1039/C8MH00803E
Qiu X, Liu S, Zhang H et al (2018) Mesenchymal stem cells and extracellular matrix scaffold promote muscle regeneration by synergistically regulating macrophage polarization toward the M2 phenotype. Stem Cell Res Ther 9(1):88. https://doi.org/10.1186/s13287-018-0821-5
Redondo-Castro E, Cunningham CJ, Miller J et al (2018) Generation of human mesenchymal stem cell 3D spheroids using low-binding plates. Bio-Protoc 8(16):2968. https://doi.org/10.21769/BioProtoc.2968
Sandell L, SakaiD (2008) Mammalian cell culture. In: Current protocols essential laboratory techniques. Wiley
Shi Y, Wang Y, Li Q et al (2018) Immunoregulatory mechanisms of mesenchymal stem and stromal cells in inflammatory diseases. Nat Rev Nephrol 14(8):493–507. https://doi.org/10.1038/s41581-018-0023-5
Tietze S, Kräter M, Jacobi A, Taubenberger A et al (2019) Spheroid culture of mesenchymal stromal cells results in morphorheological properties appropriate for improved microcirculation. Adv Sci 6(8):1802104. https://doi.org/10.1002/advs.201802104
Trzyna A, Banaś-Ząbczyk A (2021) Adipose-derived stem cells secretome and its potential application in “stem cell-free therapy.” Biomolecules 11(6):878. https://doi.org/10.3390/biom11060878
Weiss ARR, Dahlke MH (2019) Immunomodulation by mesenchymal stem cells (MSCs): mechanisms of action of living, apoptotic, and dead MSCs. Front Immunol 10:1191. https://doi.org/10.3389/fimmu.2019.01191
Ylöstalo JH, Bartosh TJ, Coble K, Prockop DJ (2012) Human mesenchymal stem/stromal cells cultured as spheroids are self-activated to produce prostaglandin E2 that directs stimulated macrophages into an anti-inflammatory phenotype. Stem Cells 30(10):2283–2296. https://doi.org/10.1002/stem.1191
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Al-Shaibani, M.B.H. Three-dimensional cell culture (3DCC) improves secretion of signaling molecules of mesenchymal stem cells (MSCs). Biotechnol Lett 44, 143–155 (2022). https://doi.org/10.1007/s10529-021-03216-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10529-021-03216-9