Abstract
Objective
In order to identify specific mesenchymal stromal cell (MSC) populations with enhanced therapeutic efficacy, we evaluated the functional changes associated with the stable expression of CD200, which is associated with immune regulatory function and osteogenic differentiation, in human bone marrow-derived MSCs (CD200/MSCs).
Results
We detected significantly greater osteogenesis and chondrogenesis in CD200/MSCs than in mock-transfected MSCs. In addition, the immune regulatory function of MSCs in mixed lymphocyte reactions was enhanced by CD200 gene transfection. In CD200/MSCs, the secretion of inflammatory cytokines, i.e., IL-6 and IL-8, was reduced, and levels of the anti-inflammatory factors IL-10, FOXP3, and indoleamine 2,3-dioxygenase 1 were elevated. Finally, CD200 transfection increased the stemness of MSCs, as evidenced by greater colony numbers in colony-forming unit fibroblast assays and analyses of NANOG and OCT-4 expression.
Conclusions
These results suggest that CD200/MSCs have therapeutic applications, and further in-depth research should focus on the development of a clinically applicable cell-based therapeutic strategy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mesenchymal stromal cells (MSCs) have self-renewal capacity and the potential for multi-lineage differentiation into adipocytes, chondrocytes, and osteocytes (Salem et al. 2010). Based on their therapeutic potential for tissue repair, early studies focused on the use of MSCs in the field of regenerative medicine (Suh et al. 2017). As subsequent studies have shown that MSCs produce a number of immune-related molecules and possess immuno-modulatory and anti-inflammatory properties, many recent studies have focused on their use in the treatment of various immune disorders (Dazzi et al. 2012).
Despite their many advantages for clinical applications, such as easy preparation and low immunogenicity, MSCs are functionally heterogeneous and vary with respect to therapeutic efficacy at the level of individual cells. These limitations may be associated with a particular donor or source, culture conditions, epigenetic reprogramming, senescence, and cryopreservation (Kim et al. 2015). Several studies have examined methods to improve the therapeutic potential of MSCs. In one such study, key functional regulatory genes were overexpressed via gene transfection. MSC-mediated tissue repair was enhanced by the overexpression of hepatocyte growth factor in a rat model of radiation-induced liver damage (Zhang et al. 2014). In addition, researchers have forced the expression of specific genes related to immune regulation to improve the immunomodulatory function of MSCs in various models, e.g., IFN-γ in a mouse model of inflammatory colitis (Chen et al. 2015), IL-10 in a mouse model of acute graft-versus-host disease (Min et al. 2007), TGF-β in an autoimmune diabetes model (Daneshmandi et al. 2017), and IL-4 in a mouse autoimmune encephalomyelitis model (Payne et al. 2012). These studies have shown that MSCs can be specifically optimized to enhance their therapeutic efficacy for particular uses.
CD200, a membrane glycoprotein that belongs to the immunoglobulin superfamily, is a potential new marker of bone marrow-derived MSCs and may help discriminate MSCs from hematopoietic cells (Delorme et al. 2008). In addition to its role as a specific marker for native MSCs, CD200 has been studied owing to its immunomodulatory properties. CD200-positive MSCs, which interact with CD200R-positive cells, can initiate immunosuppressive signaling that leads to anti-inflammatory effects via the downregulation of several immune cell functions (Lee et al. 2006). Additionally, recent studies have shown that CD200-positive MSCs exhibit elevated osteogenic differentiation potential (Rostovskaya et al. 2012). Based on these collective observations, the selection of CD200-positive MSCs should be considered for therapeutic approaches. However, as the frequency of CD200-positive MSCs varies widely, with a mean of 37.7 ± 13% (range 23–63.4%) of total MSCs (Pontikoglou et al. 2016), an alternative strategy for modifying MSCs to stably and maximally express CD200 may be a more effective strategy than the selection of naturally occurring CD200-positive MSCs.
In this study, we transfected human bone marrow-derived MSCs to express CD200 and then assessed their multi-lineage differentiation potential and immunoregulatory functions. As the expression of CD200 decreases after the adipogenic and osteogenic induction of MSCs (Delorme et al. 2008), we also assessed changes in MSC stemness following the forced induction of CD200 expression.
Materials and methods
Preparation and characterization of MSCs
Human MSCs (Catholic MASTER Cells, passage 2) were procured from the Catholic Institute of Cell Therapy (Seoul, Korea) and maintained in DMEM supplemented with 10% fetal bovine serum and 1% penicillin/streptomycin solution. Cells were maintained at 37 °C in a humidified atmosphere of in 5% CO2. Immunophenotypic analysis of CD73, CD90, CD14, CD34, CD45, CD105, and HLA-DR expression (antibodies from BD Biosciences, San Jose, CA, USA) was performed by flow cytometry in the expanded MSCs. The samples were analyzed using a BD™ LSR II Flow Cytometer (BD Biosciences), and data were analyzed using FlowJo (version 7.6.1). This study was approved by the Institutional Review Board of the Catholic University of Korea.
Construction of CD200 expression plasmids for transfection
The coding region of human CD200 from the CD200 Human cDNA ORF Clone (Origene, Rockville, MD, USA) was amplified by polymerase chain reaction (PCR) (Table 1) and cloned into the pEGFP-C1 expression vector (Takara Bio, Shiga, Japan). To increase the cloning efficiency, a sticky 5′ end and blunt 3′ end were created. The PCR primers used for cloning included enzyme sites at the 5′ and 3′ ends of the CD200 coding sequence. After PCR, the insert was prepared using EcoRI and BamHI (Takara Bio). The 3′ end was digested with EcoRI, and then T7 polymerase (Takara Bio) was used to blunt the end. The prepared vector and insert were ligated using the Takara Ligation Kit (Takara Bio) and transformed into cells to obtain the corresponding clones. PCR products were verified by DNA sequencing (Bioneer, Daejeon, Korea).
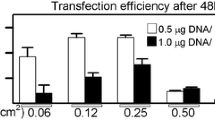
Electroporation and confirmation of transfection efficiency
Subconfluent MSCs were harvested, resuspended in a buffer provided by the manufacturer at a density of 3 × 105 cells/mL, and mixed with 0.5 μg of the constructed plasmids. Then, cells were electroporated with a Microporator (Thermo Fisher Scientific, Rockford, MD, USA) using the program recommended by the manufacturer: two pulses of 1400 V. MSCs were transfected with pEGFP-C1 without the interposed genes (mock/MSCs) or with CD200 (CD200/MSCs). Gene transfection efficiency was assessed using a fluorescence microscope and a BD™ LSR II flow cytometer 72 h after gene transfection. CD200 gene expression was assessed by real-time PCR using CD200 primers (Table 1).
Multi-lineage differentiation of MSCs
Chondrogenic, osteogenic, and adipogenic differentiation were induced as described previously (Kim et al. 2016; Xu et al. 2017). Cell differentiation status was then assessed by safranin-O, alkaline phosphatase (ALP) substrate, and Oil Red O staining, respectively. Real-time PCR and western blotting were performed to evaluate the mRNA and protein expression levels, respectively, of type II collagen, RUNX2, and PPAR-γ (Table 1). The blots were assayed using an enhanced chemiluminescence detection system (Amersham Biosciences, Piscataway, NJ, USA) (Xu et al. 2017).
Th0 differentiation conditions and T cell suppression assay
Peripheral blood mononuclear cells (PBMCs) were prepared from heparinized blood by Ficoll-Hypaque (GE Healthcare, Milwaukee, WI, USA) density-gradient centrifugation and cultured as described previously (Alvarez-Lara et al. 2004). CD4+ T cells were isolated from PBMCs from healthy individuals using a monoclonal anti-human CD4 antibody conjugated to MicroBeads (Miltenyi Biotech, Bergisch Gladbach, Germany). The purities of the T cell subsets were > 95%, as determined by flow cytometry (data not shown). For the T cell suppression assay, CD4+ T cells (2 × 105) were incubated with anti-CD3 (1 mg/mL) and anti-CD28 (1 mg/mL) (BD Biosciences), along with MSCs (2 × 103), mock/MSCs (2 × 103), or CD200/MSCs (2 × 103) for 48 h. CD4+ T cell proliferation was examined by adding [3H]-thymidine (1 mCi/well; GE Healthcare) to the cultures, followed by incubation for 8 h. [3H]-thymidine incorporation was measured using a liquid β-scintillation counter (Beckman Coulter, Brea, CA, USA).
T cells (2 × 105) were then stimulated with anti-CD3 (1 mg/mL) and T cell-depleted, irradiated antigen-presenting cells in the presence or absence of MSCs (2 × 103), mock/MSCs (2 × 103), or CD200/MSCs (2 × 103). The purity of all T-cell subsets was > 95%, as determined by flow cytometry analysis (data not shown). Isolated effector cells were > 95% pure. For the T cell suppression assay, CD4+ effector T cells (1 × 105) were co-cultured with T-cell-depleted, irradiated antigen-presenting cells (1 × 105), anti-CD3 antibody (1 mg/mL), and MSCs (2 × 103), mock/MSCs (2 × 103), or CD200/MSCs (2 × 103) for 3 days. The proliferation of CD4+ T cells was examined by adding [3H]-thymidine (1 lCi/well; GE Healthcare) to the cultures, followed by incubation for 8 h. [3H]-thymidine incorporation was measured using a liquid β-scintillation counter (Beckman Coulter).
Enzyme-linked immunosorbent assay
Levels of IL-6 and IL-8 were measured in the culture supernatants of mock/MSCs and CD200/MSCs using sandwich enzyme-linked immunosorbent assays (ELISAs; R&D Systems, Minneapolis, MN, USA) according to the manufacturer’s instructions. Absorbance was measured at 405 nm using an ELISA microplate reader (Molecular Devices, Sunnyvale, CA, USA).
Stemness analysis
For colony-forming unit fibroblast (CFU-F) assays, MSCs were seeded in a culture plate at a density of 1 × 103 cells/plate in MethoCult™ (STEMCELL Technologies, Vancouver, Canada), which was changed every 2–3 days. After culture for 14 days under standard conditions, cells were fixed with ice-cold methanol and stained with 0.3% crystal violet. Visible colonies were then counted. Real-time PCR and western blotting were performed to evaluate the mRNA and protein expression levels of NANOG and OCT-4 (Table 1).
Statistical analyses
All quantitative data are expressed as group means and standard deviations. Statistical analyses were performed with the Mann–Whitney U-test using SPSS software (SPSS, Chicago, IL, USA; http://www.spss.com). P < 0.05 was considered statistically significant.
Results
Efficiency of CD200 gene transfection and changes in CD200 expression
We confirmed vector transfection using fluorescence microscopy 72 h after CD200 gene transfection (Fig. 1a). Although CD200/MSCs appeared more spread out, microscopy confirmed that there was no change in cell morphology (Fig. 1b). Transfection efficiency was 85% in mock/MSCs and 79% in CD200/MSCs (data not shown). After gene transfection, CD200 expression increased approximately 715-fold in CD200/MSCs compared to levels in FACS-sorted native CD200-positive MSCs (Fig. 1c).
Assessment of CD200 gene transfection efficiency. MSCs were transfected with the pEGFP-C1 and pEGFP-C1/CD200 vectors. Transfection efficiency was assessed by fluorescence microscopy (a). The morphology of transfected MSCs was observed using a microscope (b). Real-time PCR was used to confirm CD200 gene expression in CD200-sorted MSCs and CD200/MSCs (c)
Chondrogenic, osteogenic, and adipogenic differentiation of CD200/MSCs
We assessed the chondrogenic, osteogenic, and adipogenic differentiation of CD200/MSCs based on safranin-O, ALP substrate, and Oil Red O staining, respectively. CD200/MSCs were compared with mock/MSCs to verify differentiation capacity, and non-transfected MSCs were used to control for any potential effects of transfection. CD200/MSCs exhibited enhanced chondrogenic and osteogenic differentiation compared to those of mock/MSCs, whereas adipogenic differentiation was unaltered in CD200/MSCs (Fig. 2a). Each differentiation process is associated with the expression of a key regulator, i.e., type II collagen for chondrogenic differentiation, RUNX2 for osteogenic differentiation, and PPAR-γ for adipogenic differentiation. Type II collagen expression in CD200/MSCs was 5.2-fold higher and RUNX2 expression was 7.5-fold higher than the corresponding expression levels in mock/MSCs (Fig. 2b, P < 0.001). In contrast, the 1.2-fold increase in PPAR-γ expression was not statistically significant (Fig. 2b). The protein expression results were similar to the gene expression results (Fig. 2c). These results show that transfection of MSCs with CD200 increased chondrogenic and osteogenic, but not adipogenic, differentiation.
Multi-lineage differentiation of MSCs after CD200 gene transfection. Cells were stained with safranin-O, ALP substrate, and Oil Red O to assess chondrogenic, osteogenic, and adipogenic differentiation, respectively (a). Real-time PCR (b) and western blotting (c) were used to analyze the expression of type II collagen, RUNX2, and PPAR-γ to assess chondrogenic, osteogenic, and adipogenic differentiation, respectively. *P < 0.05, **P < 0.01 versus MSCs, #P < 0.05, ##P < 0.01 versus mock/MSCs
Protective effect of CD200/MSCs against T cell- or inflammatory cytokine-induced inflammation
We observed significantly higher transcript levels of IL10 (2.1-fold), FOXP3 (2.7-fold), and indoleamine 2,3-dioxygenase (IDO, 2.1-fold) in CD200/MSCs compared to levels in MSCs (Fig. 3a). CD200/MSCs suppressed the proliferation of Th0 cells to a greater extent than MSCs or mock/MSCs in mixed lymphocyte reactions (Fig. 3b). Levels of IL-6 and IL-8 measured after 48 h of incubation were significantly lower in CD200/MSCs than in MSCs or mock/MSCs (Fig. 3c). These results suggest that CD200 overexpression enhanced the immunomodulatory function of MSCs, as shown by their effective suppression of Th0 cell activation and inflammatory cytokine production.
Effects of CD200 gene transfection on MSC-mediated immune regulation. Expression levels of IL10, FOXP3, and IDO were determined by real-time PCR (a). The suppressive effect of MSCs transfected with CD200 on effector Th0 cell proliferation was assessed (b). Levels of IL-6 and IL-8 produced by MSCs, mock/MSCs, and CD200/MSCs were measured by ELISA 48 h after transfection (c). *P < 0.05, **P < 0.01 versus MSCs, #P < 0.05, ##P < 0.01 versus mock/MSCs
Enhancement of MSC stemness by CD200 transfection
Next, we assessed whether these increases in differentiation ability and the immunomodulatory functions of MSCs induced by CD200 transfection were associated with changes in MSC stemness. According to the results of a CFU-F assay, CFU counts were at least twofold higher in CD200/MSCs (74.6 ± 4.2) than in mock/MSCs (30.3 ± 3.2) or MSCs (24.3 ± 2.1) (Fig. 4a, P < 0.01). We did not observe differences between the control MSCs and mock/MSCs. To determine whether this increase in stemness was related to changes in the expression levels of NANOG and OCT-4, we performed real-time PCR and western blotting. NANOG and OCT4 transcript levels were 5.1 times (P < 0.001) and 3.9 times (P < 0.05) higher, respectively, in CD200/MSCs than in mock/MSCs (Fig. 4b). Similar changes were also observed at the protein level (Fig. 4c). These results suggest that CD200 is not only a marker of MSCs but also a key regulator of MSC stemness.
Discussion
The expression of CD200 in MSCs is heterogeneous (Pontikoglou et al. 2016); accordingly, we developed a system to promote the high, stable expression of CD200. We observed marked improvements in the chondrogenic and osteogenic differentiation of CD200/MSCs but found no significant difference in adipogenic ability. Our osteogenic differentiation results are similar to those reported by Lee et al., who found that CD200 enhances calvarial osteoblast formation (Lee et al. 2006), and the results of other studies showing that CD200 mediates improvements in osteogenesis. In addition, CD200 is a predictive marker for low adipogenic capacity in adipose- or bone marrow-derived MSCs (Rostovskaya et al. 2012). With regard to chondrogenesis, we found a positive correlation between CD200 transfection and Type II collagen expression; such a relationship was not observed by Pontikoglou et al. (2016), though these authors did not perform chondrogenic differentiation assays. Additional in-depth studies are necessary to reveal the relationship between CD200 expression and chondrogenic differentiation.
CD200 plays a crucial role in controlling autoimmunity, inflammation, and adaptive immune responses. The binding of CD200 to CD200 receptors suppresses mast cell degranulation by inhibiting MAPK signaling pathways (Zhang et al. 2004), and the production of IL-13, TNF-α, IFN-α, and IL-17 is also reduced by CD200–CD200R engagement (Cherwinski et al. 2005). The addition of a CD200-Fc fusion protein to mixed leukocyte reactions decreases the production of IL-β and increases that of IL-10. Furthermore, MSCs with high CD200 expression inhibit TNF-α and have immunosuppressive properties under clinical conditions (Pietilä et al. 2012). Thus, our experimental results using CD200-transfected MSCs confirm the critical role of CD200 in MSC-mediated immune regulation and suggest the need for further in vivo validation of CD200/MSCs as a potential immunosuppressive cell therapy.
As multi-lineage differentiation capacity is associated with stemness and as stemness is elevated in CD200-positive MSCs (Delorme et al. 2008), we investigated whether the enhanced differentiation capacity and immune regulatory effects of CD200/MSCs were related to stemness. We observed enhanced stemness in CD200/MSCs, consistent with a previous report indicating a relationship between CD200 expression and stemness in follicular stem cells (Mohanty et al. 2013). These results highlight the role of stemness in CD200-mediated improvements in the selective differentiation of and immune regulation by CD200/MSCs. However, the present study is limited by its focus on functional analyses; future studies should explore the mechanisms linking stemness and CD200 expression.
This is the first study to confirm the effects of CD200 overexpression on MSC immunomodulation and differentiation, with the objective of maximizing the therapeutic potential of CD200-positive MSCs. Our results suggest that the improvement in MSC function following CD200 transfection may be associated with the acquisition of stemness, though further research is necessary to firmly establish this link. Our findings also suggest the potential application of CD200/MSCs as a therapeutic tool, and thus further research geared toward clinical applications is warranted.
References
Alvarez-Lara MA, Carracedo J, Ramírez R, Martín-Malo A, Rodríguez M, Madueño JA, Aljama P (2004) The imbalance in the ratio of Th1 and Th2 helper lymphocytes in uraemia is mediated by an increased apoptosis of Th1 subset. Nephrol Dial Transplant 19(12):3084–3090
Chen Y, Song Y, Miao H, Xu Y, Lv M, Wang T, Hou Y (2015) Gene delivery with IFN-gamma-expression plasmids enhances the therapeutic effects of MSCs on DSS-induced mouse colitis. Inflamm Res 64(9):671–681
Cherwinski HM, Murphy CA, Joyce BL, Bigler ME, Song YS, Zurawski SM, Moshrefi MM, Gorman DM, Miller KL, Zhang S, Sedgwick JD, Phillips JH (2005) The CD200 receptor is a novel and potent regulator of murine and human mast cell function. J Immunol 174(3):1348–1356
Daneshmandi S, Karimi MH, Pourfathollah AA (2017) TGF-beta engineered mesenchymal stem cells (TGF-β/MSCs) for treatment of Type 1 diabetes (T1D) mice model. Int Immunopharmacol 44:191–196
Dazzi F, Lopes L, Weng L (2012) Mesenchymal stromal cells: a key player in ‘innate tolerance’? Immunology 137(3):206–213
Delorme B, Ringe J, Gallay N, Le Vern Y, Kerboeuf D, Jorgensen C, Rosset P, Sensebé L, Layrolle P, Häupl T, Charbord P (2008) Specific plasma membrane protein phenotype of culture-amplified and native human bone marrow mesenchymal stem cells. Blood 111(5):2631–2635
Kim N, Cho SG (2015) New strategies for overcoming limitations of mesenchymal stem cell-based immune modulation. Int J Stem Cells 8(1):54–68
Kim HJ, Kwon YR, Bae YJ, Kim YJ (2016) Enhancement of human mesenchymal stem cell differentiation by combination treatment with 5-azacytidine and trichostatin A. Biotechnol Lett 38(1):167–174
Lee L, Liu J, Manuel J, Gorczynski RM (2006) A role for the immunomodulatory molecules CD200 and CD200R in regulating bone formation. Immunol Lett 105(2):150–158
Min CK, Kim BG, Park G, Cho B, Oh IH (2007) IL-10-transduced bone marrow mesenchymal stem cells can attenuate the severity of acute graft-versus-host disease after experimental allogeneic stem cell transplantation. Bone Marrow Transplant 39(10):637–645
Mohanty S, Kumar A, Dhawan J, Sharma VK, Gupta S (2013) Depletion of CD200+ Hair Follicle Stem Cells in Human Prematurely Gray Hair Follicles. J Cutan Aesthet Surg 6(2):90–92
Payne NL, Dantanarayana A, Sun G, Moussa L, Caine S, McDonald C, Herszfeld D, Bernard CC, Siatskas C (2012) Early intervention with gene-modified mesenchymal stem cells overexpressing interleukin-4 enhances anti-inflammatory responses and functional recovery in experimental autoimmune demyelination. Cell Adhes Migr 6(3):179–189
Pietilä M, Lehtonen S, Tuovinen E, Lähteenmäki K, Laitinen S, Leskelä HV, Nätynki A, Pesälä J, Nordström K, Lehenkari P (2012) CD200 positive human mesenchymal stem cells suppress TNF-alpha secretion from CD200 receptor positive macrophage-like cells. PLoS ONE 7(2):e31671
Pontikoglou C, Langonné A, Ba MA, Varin A, Rosset P, Charbord P, Sensébé L, Deschaseaux F (2016) CD200 expression in human cultured bone marrow mesenchymal stem cells is induced by pro-osteogenic and pro-inflammatory cues. J Cell Mol Med 20(4):655–665
Rostovskaya M, Anastassiadis K (2012) Differential expression of surface markers in mouse bone marrow mesenchymal stromal cell subpopulations with distinct lineage commitment. PLoS ONE 7(12):e51221
Salem HK, Thiemermann C (2010) Mesenchymal stromal cells: current understanding and clinical status. Stem Cells 28(3):585–596
Suh N, Subramanyam D, Lee M-Y (2017) Molecular signatures of secretomes from mesenchymal stem cells: therapeutic benefits. Mol Cell Toxicol 13(2):133–141
Xu L, Liu Y, Sun Y, Wang B, Xiong Y, Lin W, Wei Q, Wang H, He W, Wang B, Li G (2017) Tissue source determines the differentiation potentials of mesenchymal stem cells: a comparative study of human mesenchymal stem cells from bone marrow and adipose tissue. Stem Cell Res Ther 8(1):275
Xue L, Zenlong W, Zhalun L, Chen Q, Peng Z, Haiwen C, Ziming W (2017) RBPJ contributes to acquire docetaxel resistance in prostate cancer cells. Mol Cell Toxicol 13(3):279–285
Zhang S, Cherwinski H, Sedgwick JD, Phillips JH (2004) Molecular mechanisms of CD200 inhibition of mast cell activation. J Immunol 173(11):6786–6793
Zhang J, Zhou S, Zhou Y, Feng F, Wang Q, Zhu X, Ai H, Huang X, Zhang X (2014) Hepatocyte growth factor gene-modified adipose-derived mesenchymal stem cells ameliorate radiation induced liver damage in a rat model. PLoS ONE 9(12):e114670
Acknowledgements
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Science, ICT & Future Planning (Grant Nos. 2015R1A2A2A04002756 and 2018R1A2B2006820). It was also supported by the Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Education (Grant Nos. 2010-0008762, 2014R1A1A3054664).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Kim, H.J., Kim, KW., Kwon, YR. et al. Forced expression of CD200 improves the differentiation capability and immunoregulatory functions of mesenchymal stromal cells. Biotechnol Lett 40, 1425–1433 (2018). https://doi.org/10.1007/s10529-018-2561-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10529-018-2561-0