Abstract
COVID-19 (Coronavirus disease 2019) is caused by SARS-CoV-2 (severe acute respiratory syndrome coronavirus-2), which can lead to pneumonia, cytokine storms, and lymphopenia. Patients with cancer are more susceptible to SARS-CoV-2 infection and severe COVID-19 due to immunosuppression. Recent studies have indicated that NRP1 (Neuropilin 1) may act as a novel mediator of SARS-CoV-2 entry into the host cell. As no systematic review has been performed investigating the characteristics of NRP1 in pan-carcinoma, we comprehensively analyzed NRP1 in patients with pan-cancer. Using a bioinformatics approach, we aimed to systematically examine NRP1 expression profiles in both pan-carcinoma and healthy tissues. We found that lung and genitourinary cancers have a relatively higher NRP-1 expression than other cancer patients, suggesting that these patients may be more susceptible to SARS-CoV-2. Our analysis further revealed that NRP1 expression was downregulated in Vero E6 cells, whole blood, lung organoids, testis tissue, and alveolospheres infected with SARS-CoV-2. Notably, NRP1 was associated with immune cell infiltration, immune checkpoint genes, and immune-related genes in most patients with cancer. These findings suggest that, in patients with specific types of cancer, especially lung and genitourinary, high expression of NRP1 contributes to greater susceptibility to SARS-CoV-2 infection and an increased risk of damage due to cytokine storms. Overall, NRP1 appears to play a critical role in regulating immunological properties and metabolism in many tumor types. Specific inhibitors of the NRP1 antigen (pegaptanib, EG00229, or MNRP1685A) combined with other anti-SARS-CoV-2 strategies may aid in treating patients with lung and genitourinary cancers following SARS-CoV-2 infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
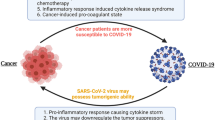
COVID-19 has spread globally, reaching over 600 million cases worldwide. Patients with tumors who receive chemotherapy or other treatments exhibit increased susceptibility to SARS-CoV-2 infection due to reduced immune function (Liang et al. 2020). In addition, increased levels of proinflammatory cytokines such as IL-6, TNF, and IL-33 result in hyperinflammation and a subsequent “cytokine storm” in patients with severe COVID-19 (Song et al. 2022). Further, immune dysregulation is believed to play an important role in the pathogenesis of COVID-19 (Nile et al. 2020).
Patients with obesity or specific types of cancer are at high risk for SARS-CoV-2 infection given high expression of ACE2 (Angiotensin Converting Enzyme 2) (Al Heialy et al. 2020). ACE2 has also been identified as a host factor for SARS-CoV-2 infection, facilitating cellular entry of the virus and enhancing infectivity (Cantuti-Castelvetri et al. 2020; Daly et al. 2020). NRP1, which is capable of binding to many ligands and various types of co-receptors, has been shown to affect cancer cell survival, migration, and attraction (Jubb et al. 2012; Dong et al. 2021). Once NRP1 binds to the CendR motif of the furin-cleaved SARS-CoV-2 S1 protein, SARS-CoV-2 infection and lentiviral particles pseudotyped with the S protein of SARS-CoV-2 are significantly upregulated. A recent study also reported that NRP1 is widely expressed in the olfactory epithelium and human brain, including olfactory-related regions, suggesting that NRP1 is involved in the development of anosmia in patients with COVID-19 (Davies et al. 2020).
The current strategy against SARS-CoV-2 consists of supportive care in combination with antiviral drugs such as paxlovid (Mahase 2021). However, with the increasing number of cases, there is still an urgent need to develop additional drugs to alleviate the symptoms of COVID-19 and decrease the risk of long-term damage. Notably, SARS-CoV-2 infections among healthy people depend on the immunopathology (Liu et al. 2021). A better understanding of the relative protease action of NRP1 and the effects of receptor binding will aid in elucidating the mechanism underlying viral infection and promote the development of novel antiviral therapies.
In the study, we systematically analyzed the basal expression levels of NRP1 genes in healthy human tissues and pan-cancer tissues and the correlations between NRP1 and infiltrating immune cell levels in patients with tumors. In addition to providing insight into the therapeutic significance of NRP1 in patients with cancer exhibiting SARS-CoV-2 infection, our results demonstrate how drugs targeting NRP1 can be used to prevent cytokine storms and complications of SARS-CoV-2 infection in patients with specific types of cancer.
Results
NRP1 Expression in Healthy Human Tissue
The NRP1 transcript was most highly expressed in the placenta, adipose tissue, muscle tissue, and lung tissue, while the NRP1 protein was most abundantly expressed in the respiratory system, especially in the nasopharynx and bronchus (Fig. 1a and b). Furthermore, we analyzed NRP1 expression using four public datasets (consensus, HPA, GTEx, and FANTOM5). NRP1 transcripts were found in high levels in the adipose, heart, and lung tissues (Fig. 1c–f). Intriguingly, the increased expression of NRP1 in human adipocytes is consistent with the current concept that patients with obesity are more susceptible to SARS-CoV-2 infection. Previous studies have shown that loss of taste (ageusia) and loss of smell (anosmia) are frequent neurological manifestations of COVID-19 (Passarelli et al. 2020). However, ACE2 is expressed at low levels in the olfactory epithelium and respiratory tract (Cantuti-Castelvetri et al. 2020). Our data showed that NRP1 was abundantly expressed in the nasopharynx and bronchial tissue, indicating that SARS-Cov-2 may mainly access NRP1 through the nasal olfactory mucosa, first reaching the olfactory bulb. Expression of the NRP1 protein was also detected at significantly high levels in the brain tissue (Fig. 1a and b). The ACE2 receptor also has relatively high expression in the brainstem (Lukiw et al. 2022), suggesting that ACE2 and NRP1 cooperate to mediate SARS-CoV-2 entry into the brain, leading to neurological manifestations of COVID-19. High levels of NRP1 gene expression were also observed in adipocytes, lung tissues, and kidney tissues (Fig. 1c–f). These results were also validated in the HCCDB dataset (Fig. 1g). These results indicate that NRP1 is widely distributed across tissues and abundantly expressed in adipocytes, the nasopharynx, the bronchus, the lung, and the kidney, which are susceptible to SARS-CoV-2 infection.
Expression of NRP1 in human tissues and organs. a mRNA and protein expression profiles of NRP1 in all tissues and organs in the tissue atlas database. b Detailed tissues or organs with NRP1 protein expression in the Tissue Atlas database. c–f NRP1 mRNA expression in various tissues analyzed from four databases (Consensus, HAP, GTEx, and Fantom5). g NRP1 mRNA expression in healthy human tissues analyzed from the HCCDB database. nTPM: normalized transcripts per million
NRP1 Expression in SARS-CoV-2-Infected Cell Lines/Organs
Seven publicly available transcriptomic datasets were reanalyzed to explore NRP1 expression in different SARS-CoV-2-infected cell lines/organs: GSE161881, GSE171110, GSE155518, GSE147507, GSE152060, GSE171430, and IPX0002393000. The mRNA abundance of NRP1 was significantly decreased in Vero E6 cells (Fig. 2a), whole blood (Fig. 2b), lung organoids (Fig. 2c and d), testis tissue (Fig. 2e), and alveolospheres (Fig. 2f) from patients infected with SARS-CoV-2 when compared with that observed in healthy controls. NRP1 expression in bronchial organoids also decreased with prolonged SARS-CoV-2 exposure (Fig. 2g). These data strongly suggest that NRP1 is critical in mediating SARS-CoV-2 infection in specific organs and cell lines.
Expression of NRP1 in SARS-CoV-2-infected organs/cell lines. a mRNA level of NRP1 in Vero E6 cells with SARS-CoV-2 (n = 3) or mock infection (n = 3). b mRNA level of NRP1 in whole blood of COVID-19 patients (n = 44) and healthy donors (n = 10). c mRNA level of NRP1 in primary lung alveolar AT2 cells with SARS-CoV-2 (n = 3) or mock infection (n = 3). d mRNA level of NRP1 in lung tissue of patients with COVID-19 (n = 2) and healthy donors (n = 2). e mRNA level of NRP1 in testis tissue of patients with COVID-19 (n = 8) and healthy donors (n = 7). f mRNA level of NRP1 in alveolospheres with SARS-CoV-2 (n = 2) or mock infection (n = 2). g mRNA level of NRP1 in human bronchial epithelium organoids infected with SARS-Cov-2 for 72 h. Statistical significance was accepted at p < 0.05. Data were expressed as mean (standard deviation). *p < 0.05, ***p < 0.01, ***p < 0.001 (Student’s t-test)
Expression Landscape of NRP1 in Pan-Carcinoma
Patients with cancer are considered more prone to severe COVID-19 and have a poor prognosis (Li et al. 2020). Thus, we analyzed the profile of NRP1 expression on over 33 different tumor types of 10,000 cancer patients. In TCGA (The Cancer Genome Atlas) cohort, NRP1 transcript expression was increased in CHOL(Cholangiocarcinoma), ESCA (Esophageal carcinoma), GBM (Glioblastoma multiforme), HNSC (Head and Neck squamous cell carcinoma), KIRC (Kidney renal clear cell carcinoma), LIHC (Liver hepatocellular carcinoma), and STAD (Stomach adenocarcinoma) tissues when compared to adjacent normal tissues. In contrast, decreased NRP1 transcript expression was observed in BLCA (Bladder Urothelial Carcinoma), BRCA (Breast invasive carcinoma), CESC (Cervical squamous cell carcinoma and endocervical adenocarcinoma), COAD (Colon adenocarcinoma), KICH (Kidney Chromophobe), LUSC (Lung squamous cell carcinoma), READ (Rectum adenocarcinoma), and UCES (Uterine Corpus Endometrial Carcinoma) tissues (Fig. 3a, all p < 0.05). Consistent with these results, NRP1 protein was highly abundant in KIRC and GBM tissues and less abundant in BRCA, COAD, and UCES tissues (when compared with healthy tissue) (Fig. 3b, all p < 0.05). Moreover, NRP1 transcript expression was relatively increased in KIRC, LUAD (Lung Adenocarcinoma), and KIRP (Kidney Renal Papillary Cell Carcinoma) compared with other cancer types. Previous studies found that patients with lung and genitourinary cancers are the most susceptible to COVID-19 (Hu et al. 2021). These results indicated that lung and genitourinary cancers with a high level of NRP1 expression might be more susceptible to SARS-CoV-2.
Using the GEPIA2 database, we generated two survival curves to show the associations of NRP1 expression with OS (overall survival) and DFS (disease-free survival). Increased NRP1 expression was associated with a low overall survival rate in ACC (Adenoid Cystic Carcinoma) (HR = 3.9, p = 0.001), BLCA (HR = 1.3, p = 0.054), CESC (HR = 1.8, p = 0.016), GBM (HR = 1.5, p = 0.037), LGG (Low-Grade Glioma) (HR = 1.6, p = 0.009), LUSC (HR = 1.3, p = 0.041), MESO (Mesothelioma) (HR = 1.5, p = 0.085), STAD (HR = 1.8, p < 0.001), UCES (HR = 1.9, p = 0.070), and UVM (Uveal Melanoma) (HR = 4.3, p = 0.002) (Fig. 4). Conversely, high NRP1 expression predicted good overall survival in KIRC (HR = 0.59, p < 0.001). Moreover, increased expression of NRP1 correlated with poor DFS in ACC (HR = 3.9, p < 0.001), CESC (HR = 1.8, p = 0.040), ESCA (HR = 1.8, p = 0.020), GBM (HR = 1.6, p = 0.017), PAAD (HR = 1.6, p = 0.053), PRAD (Prostate Adenocarcinoma) (HR = 2.3, (p < 0.001), READ (HR = 2.7, p = 0.039), SARC (Sarcoma) (HR = 1.4, p = 0.051), and UVM (HR = 3.2, p = 0.014) (Fig. 5). In summary, these data suggest that the distribution of NRP1 in different tissues is related to poor prognoses in most patients with carcinoma.
NRP1 Expression at the Single Cell Level
Patients with severe SARS-CoV-2 infection most often develop a “cytokine storm” response that leads to a more severe form of acute respiratory distress syndrome (Hu et al. 2021). In PMBC (peripheral blood mononuclear cells) from healthy people, pDC (plasmacytoid dendritic cells) exhibited the highest levels of NRP1 expression, and classical monocytes also expressed appreciable levels of NRP1 (Fig. 6a–c). Single-cell transcriptomic studies demonstrated similar results for classical monocytes and pDC in the whole blood of patients with COVID-19 (Fig. 6d). However, at the cellular level, NRP1 expression seems to exhibit tissue specificity in different organs. Single-cell RNA-seq analysis of tissues from patients with COVID-19 revealed that NRP1 was highly expressed in fibroblast cells in lung tissue (Fig. 6e–g) and macrophages in heart tissue (Fig. 6h–j). pDCs are the primary producers of IFN-α in PMBC(peripheral blood mononuclear cell) in response to SARS-CoV-2, which makes macrophages more responsive to environmental stimuli and triggers the production of multiple cytokines in the lungs (Laurent et al. 2022). High expression of NRP1 in PBMC may contribute to this process.
Expression of NRP1 in various cell types from multiple datasets. a–c HPA, Monaco, and Schmiedel datasets for NRP1 expression in human PBMC. d Single-cell RNA-Seq data for NRP1 expression in PBMCs from patients with COVID-19. Each black dot represents the expression of NRP1 across different cell types (total of 125,000 cells). e–g Single-cell RNA-Seq data for NRP1 expression in the lungs of 16 SARS-CoV-2-infected autopsy donors (total 106,792 cells). h–j Single-cell RNA-Seq data for NRP1 expression in the hearts of 18 SARS-CoV-2-infected autopsy donors (total of 40,880 cells)
Correlation Between NRP1 Expression and Immune Infiltration in the Tumor Microenvironment in Pan-Cancer
TIICs (Tumor-infiltrating immune cells) in the TME (tumor microenvironment) are closely associated with malignant tumor initiation, progression, invasion, and metastasis. Therefore, using the TIMER2 dataset, we first analyzed the correlation between NRP1 expression and TIIC levels across 33 cancer types. Expression of NRP1 was positively associated with the infiltration of CD8+ T cells, CD4+ T cells, macrophages, monocytes, dendritic cells, mast cells, neutrophils, and cancer-associated fibroblasts in patients with pan-carcinoma (Fig. 7). We performed gene co-expression analyses to assess the relationship of NRP1 expression with the expression of chemokines and chemokine receptor proteins. Almost all the analyzed genes were co-expressed with NRP1, and the majority were positively correlated with NRP1 in most tumors (Figure S1).
Correlation Between NRP1 Expression and Immune Infiltration in the Tumor Microenvironment in Lung Cancer
Low expression of NRP1 predicted good OS in patients with LUSC (Fig. 4). Thus, we investigated the relationship between NRP1 expression and immune storms in patients with lung cancer, including LUSC and LUAD. NRP1 expression was significantly and positively correlated with infiltrating levels of CD8 cells, CD4 cells, macrophages, monocytes, DCs, mast cells, and Tregs in patients with LUSC (Fig. 8a). A similar association was also observed in patients with LUAD (Fig. 9a). These findings strongly suggest that NRP1 plays a specific role in the recruitment of TIIC in the context of lung cancers.
Fibroblasts may make immune cells more prone to viruses by transinfecting the immune cells (Shu et al. 2021). Similar to HIV, COVID-19 may hijack fibroblasts to cause viremia. In single-cell analysis, we found that NRP1 was highly expressed in fibroblast cells in the lung tissue of patients with COVID-19 (Fig. 6e–g). Its expression positively correlates with CAFs (cancer-associated fibroblasts) in lung cancer (Figs. 8a and 9a). Our results indicated that high levels of NRP1 in fibroblasts make it a potential therapeutic target in COVID-19 patients with lung cancer.
We further assessed correlations between various immune markers and NRP1 expression levels in the context of lung cancer. NRP1 exhibited significant correlations with CD163, CLEC10A, MRC1, and MS4A4A expression (Fig. 8c) but not with IL1A, NOS2, or IRF5 (Fig. 8b) in patients with LUSC. In LUAD, IL1A, NOS2, and IRF5, there was a slightly positive correlation with NRP1 (Fig. 9b), while CD163, MRC1, and MS4A4A had a robust correlation (Fig. 9c). These results suggest that M2 macrophage markers showed strong correlations with NRP1 expression, while M1 macrophage markers showed weak correlations.
In lung cancer, we also observed significant positive correlations of NRP1 with inflammatory cytokine and chemokine marker genes, including CCL2, IL6, IL10, IL33, CXCL10, and CXCL12 (Figs. 8d and 9d). Moreover, NRP1 expression was positively correlated with levels of immune checkpoint molecules, including BTLA, HAVCR2, CD274, CTLA4, LAG3, PDCD1LG2, PDCD1, and TIGIT (Figs. 8e and 9e). These results indicate that NRP1 expression is specifically correlated with TIICs, which may eventually lead to a cytokine storm in patients with lung cancer following infection with SARS-CoV-2.
Correlation Between NRP1 Expression and Immune Infiltration in the Tumor Microenvironment in Genitourinary Cancers
We investigated the relationship between NRP1 expression and immune storms in patients with genitourinary cancers, including KIRP and KIRC. NRP1 expression was significantly and positively correlated with infiltrating levels of CD8 cells, CD4 cells, macrophages, monocytes, DCs, mast cells, Tregs, and CAFs in patients with KIRP (Figure S2a). A similar association was also observed in patients with KIRC (Figure S3a). High levels of NRP1 gene expression were also observed (Fig. 3a). These findings strongly suggest that NRP1 plays a specific role in the recruitment of TIIC in the context of genitourinary cancers.
We further assessed correlations between various immune markers and NRP1 expression levels in the context of genitourinary cancers, including KIRP and KIRC. IL1A, NOS2, and IRF5 were positively correlated with NRP1 (Figure S2b and Figure S3b), while CD163, MRC1, and MS4A4A had a robust correlation (Figs. S2c and S3c). These results suggest that M2 macrophage markers showed strong correlations with NRP1 expression, while M1 macrophage markers showed weak correlations in genitourinary cancers. In genitourinary cancers, we also observed significant positive correlations of NRP1 with inflammatory cytokine and chemokine marker genes including IL6, IL10, IL33, CXCL10, and CXCL12 (Figs. S2d and S3d). These results indicate that NRP1 expression is specifically correlated with TIICs, which may eventually lead to a cytokine storm in patients with genitourinary cancer following infection with SARS-CoV-2.
Discussion
The COVID-19 pandemic continues to impact multiple countries worldwide, and more effective treatment is needed (Song et al. 2022). The poor prognosis among individuals with obesity and patients with cancer infected with SARS-CoV-2 is due to the high expression of ACE2 (Liang et al. 2020; Al Heialy et al. 2020), which may be the primary receptor targeted by SARS-CoV-2. NRP1, a cofactor of SARS-CoV-2, significantly potentiates SARS-CoV-2 infectivity by facilitating entry of SARS-CoV-2 into the cell in the presence of ACE2 (Cantuti-Castelvetri et al. 2020). Understanding the host factors of SARS-CoV-2 may provide new insights into the molecular mechanisms underlying the pathogenesis of COVID-19 and aid in identifying new therapeutic targets (Li et al. 2022; Shu et al. 2021).
Our results indicated that the NRP1 protein was highly expressed in the nasopharynx and bronchus. Anosmia is a known symptom of COVID-19. NRP1 is mainly found in the cell layer of the nasal cavity in tissue samples collected from deceased patients. These results suggest that NRP1 promotes SARS-CoV-2 transport into the brain to a certain degree.
A previous study reported vertical transmission of COVID-19 in a 1-day-old neonate (Farmer 2021). Furthermore, SARS‐CoV‐2 present in the placenta has been shown to induce placental vasculopathy and vertical transmission, especially in pregnant women who may have been exposed to COVID-19 in early pregnancy (Hsu et al. 2021). Although no co-transcription of ACE2 and TMPRSS2 has been observed in the placenta according to single-cell and RNA sequencing data, the possibility of SARS-CoV-2 transmission via the placenta at any stage of pregnancy cannot be excluded based on some studies (Pique-Regi et al. 2020). NRP1 transcripts were expressed at high levels in the placenta in the current study, supporting this notion. NRP1 transcripts were also highly expressed in adipose tissue, heart tissue, and the lung, suggesting that these organs are highly susceptible to invasion by the SARS-CoV-2 virus. Immune cells are always negative for ACE2 (Hamming et al. 2004). The high expression of NRP1 in pDC and monocytes may explain the development of lymphocytopenia in patients with COVID-19 (Zhang et al. 2021). In addition, elevated levels of NRP1 may be a critical factor leading to severe clinical symptoms of COVID-19 in patients with obesity.
Higher NRP1 expression was associated with a poor prognosis in most cancer types, suggesting a role in tumor progression. The extent of immune cell infiltration affects the prognosis of cancer patients, and researchers have increasingly emphasized the role of NRP1 in the immune response (Chuckran et al. 2020). Indeed, NRP1 has an essential function in memory T cells (Liu et al. 2020); however, its role in other T cell populations and immune cells remains to be determined. Our analysis indicated that NRP1 expression was positively correlated with diverse types of immune infiltration in various cancer types, including CD8+ T cells, CD4+ T cells, macrophages, monocytes, DCs, mast cells, monocytes, and CAFs. Interestingly, NRP1 was also highly expressed in lung fibroblasts. The risk of severe events due to COVID-19 infection is increased in patients with lung cancer compared to those observed in individuals without cancer (Liang et al. 2020). In this study, high NRP1 expression was positively associated with OS among patients with LUSC.
The correlation between NRP1 expression and immune cell marker genes indicates a critical role of NRP1 in regulating tumor immunology in patients with lung cancer and genitourinary cancers. Gene markers of M1 macrophages, such as IL1A, IRF5, and NOS2, exhibited a weak correlation with the expression of NRP1. In contrast, markers for M2 macrophages exhibited medium and robust correlations, suggesting a potential regulatory role of NRP1 in the polarization of tumor-associated macrophages. In addition, NRP1 has the potential to induce Treg and T-cell exhaustion. Together, these results highlight the potential of NRP1 to intensify the “cytokine storm” observed in patients with lung cancer and genitourinary cancers following SARS-CoV-2 infection.
The current results demonstrate that NRP1 is abundantly expressed in various tissues, including the nasopharynx, bronchus, placenta, adipose tissue, heart, and lungs. The immune response triggered by increased expression of NRP1 may contribute to severe symptoms following infection with SARS CoV-2. Since NRP1 is a host factor for SARS-CoV-2 infection and facilitates SARS-CoV-2 entry into the cell and infectivity, NRP1 inhibitors may provide therapeutic benefits for patients with specific types of cancer, such as lung cancers and genitourinary cancers, who have been infected with SARS-CoV-2.
Methods
Gene Expression Analysis
The expression data for NRP1 mRNA and protein in various tissues were obtained from the Human Protein Atlas (https://www.protein atlas.org). The expression profiles of NRP1 mRNA in 33 cancer types were obtained from the TIMER2 database (http://timer.cistrome.org/). Single-cell RNA-seq analysis was performed using the UCSC browser portal (http://www.cells.ucsc.edu/) and the Single Cell portal (https://singlecell.broadinstitute.org/single_cell) to examine NRP1 expression in different cell types. The data on NRP1 expression in PBMCs from patients with COVID-19 was obtained from Can Liu et al. study (Liu et al. 2021). The data of NRP1 expression in the lungs of 16 SARS-CoV-2-infected autopsy donors and hearts of 18 SARS-CoV-2-infected autopsy donors was obtained from Delorey et al. study (Delorey et al. 2021).
To examine NRP1 expression in cells or organs with SARS-CoV-2 infection, we analyzed seven transcriptomic datasets (GSE161881, GSE171110, GSE155518, GSE147507, GSE152060, GSE171430, and IPX0002393000) derived from the Gene Expression Omnibus database and iProX database. In the GSE161881 dataset, Vero E6 cells were infected with SARS-CoV-2 (multiplicity of infection = 2) eight hours post-infection. The GE171110 dataset was used to obtain whole blood gene expression profiles from 44 patients with COVID-19 and ten healthy donors. Primary lung alveolar AT2 cells were either mock infected or infected with SARS-CoV-2 in the GSE147507 dataset. The GSE147507 dataset contains lung tissue gene expression profiles from two patients with COVID-19 and two healthy donors. RNA expression in the testis was assessed based on data from eight patients with COVID-19 and seven healthy donors downloaded from the IPX0002393000 dataset. For the GSE152060 dataset, bronchial organoids were infected with SARS-Cov-2 for 72 h and compared to the uninfected mock control. The GSE171430 set contained mRNA profiles of alveolospheres with SARS-CoV-2 or mock infection two days post-infection.
Analysis of the Relationships Between NRP1 and Prognosis
The GEPIA2 dataset (http://gepia2.cancer-pku.cn/#index) (Tang et al. 2019) was used to obtain the overall survival (OS) and disease-free survival (DFS) data for NRP1 in all cancer types. The survival analysis for each cancer type was conducted using the Kaplan–Meier method and log-rank test.
Relationship Between NRP1 Expression and Immunity
The TIMER2 database (http://timer.cistrome.org/) was used to determine correlations between immune cell abundance and NRP1 expression in various cancers. NRP1 was used for the x-axis, and related marker genes were represented on the y-axis. The gene expression level was displayed as log2 TPM.
Statistical Analysis
Spearman’s rank correlation coefficients were examined. The strength of correlations was determined based on the absolute value, as follows: 0.00–0.19, “very weak”; 0.20–0.39, “weak”; 0.40–0.59, “medium”; 0.60–0.79, “strong”; 0.80–1.0, “very strong”. A p-value ≤ 0.05 was considered significant.
References
Al Heialy S et al (2020) Regulation of angiotensin- converting enzyme 2 in obesity: implications for COVID-19. Front Physiol. https://doi.org/10.3389/fphys.2020.555039
Cantuti-Castelvetri L et al (2020) Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity. Science 370:856–860. https://doi.org/10.1126/science.abd2985
Chuckran CA, Liu C, Bruno TC, Workman CJ, Vignali DAA (2020) Neuropilin-1: a checkpoint target with unique implications for cancer immunology and immunotherapy. J Immunother Cancer 8:e000967. https://doi.org/10.1136/jitc-2020-000967
Daly JL et al (2020) Neuropilin-1 is a host factor for SARS-CoV-2 infection. Science 370:861–865. https://doi.org/10.1126/science.abd3072
Davies JM et al (2020) Neuropilin-1 as a new potential SARS-CoV-2 infection mediator implicated in the neurologic features and central nervous system involvement of COVID-19. Mol Med Rep 22:4221–4226
Delorey TM et al (2021) COVID-19 tissue atlases reveal SARS-CoV-2 pathology and cellular targets. Nature 595:107–113. https://doi.org/10.1038/s41586-021-03570-8
Dong Y et al (2021) Role of NRP1 in bladder cancer pathogenesis and progression. Front Oncol. https://doi.org/10.3389/fonc.2021.685980
Farmer ML (2021) A Neonate with vertical transmission of COVID-19 and acute respiratory failure: a case report. Adv Neonatal Care. https://doi.org/10.1097/ANC.0000000000000954
Hamming I et al (2004) Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol 203:631–637. https://doi.org/10.1002/path.1570
Hsu AL et al (2021) Placental SARS-CoV-2 in a pregnant woman with mild COVID-19 disease. J Med Virol 93:1038–1044. https://doi.org/10.1002/jmv.26386
Hu B, Huang S, Yin L (2021) The cytokine storm and COVID-19. J Med Virol 93:250–256. https://doi.org/10.1002/jmv.26232
Jubb AM et al (2012) Neuropilin-1 expression in cancer and development. J Pathol 226:50–60. https://doi.org/10.1002/path.2989
Laurent P et al (2022) Sensing of SARS-CoV-2 by pDCs and their subsequent production of IFN-I contribute to macrophage-induced cytokine storm during COVID-19. Sci Immunol 7:eadd4906. https://doi.org/10.1126/sciimmunol.add4906
Li X, Geng M, Peng Y, Meng L, Lu S (2020) Molecular immune pathogenesis and diagnosis of COVID-19. J Pharm Anal 10:102–108. https://doi.org/10.1016/j.jpha.2020.03.001
Li J et al (2022) Comprehensive profiling analysis of CD209 in malignancies reveals the therapeutic implication for tumor patients infected with SARS-CoV-2. Front Genet 13:883234. https://doi.org/10.3389/fgene.2022.883234
Liang W et al (2020) Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol 21:335–337. https://doi.org/10.1016/s1470-2045(20)30096-6
Liu C et al (2020) Neuropilin-1 is a T cell memory checkpoint limiting long-term antitumor immunity. Nat Immunol 21:1010–1021. https://doi.org/10.1038/s41590-020-0733-2
Liu C et al (2021) Time-resolved systems immunology reveals a late juncture linked to fatal COVID-19. Cell. https://doi.org/10.1016/j.cell.2021.02.018
Liu X et al (2021) Impaired AGO2/miR-185-3p/NRP1 axis promotes colorectal cancer metastasis. Cell Death Dis 12:390. https://doi.org/10.1038/s41419-021-03672-1
Lukiw WJ, Pogue A, Hill JM (2022) SARS-CoV-2 Infectivity and neurological targets in the brain. Cell Mol Neurobiol 42:217–224. https://doi.org/10.1007/s10571-020-00947-7
Mahase E (2021) Covid-19: Pfizer’s paxlovid is 89% effective in patients at risk of serious illness, company reports. BMJ 375:n2713. https://doi.org/10.1136/bmj.n2713
Nile SH et al (2020) COVID-19: pathogenesis, cytokine storm and therapeutic potential of interferons. Cytokine Growth Factor Rev 53:66–70. https://doi.org/10.1016/j.cytogfr.2020.05.002
Passarelli PC, Lopez MA, Mastandrea Bonaviri GN, Garcia-Godoy F, D’Addona A (2020) Taste and smell as chemosensory dysfunctions in COVID-19 infection. Am J Dent 33:135–137
Pique-Regi R et al (2020) Does the human placenta express the canonical cell entry mediators for SARS-CoV-2. Elife 9:e58716. https://doi.org/10.7554/eLife.58716
Shu L et al (2021) Landscape profiling analysis of DPP4 in malignancies: therapeutic implication for tumor patients with coronavirus disease 2019. Front Oncol 11:624899. https://doi.org/10.3389/fonc.2021.624899
Song C et al (2022) SARS-CoV-2: the monster causes COVID-19. Front Cell Infect Microbiol. https://doi.org/10.3389/fcimb.2022.835750
Tang Z, Kang B, Li C, Chen T, Zhang Z (2019) GEPIA2: an enhanced web server for large-scale expression profiling and interactive analysis. Nucleic Acids Res 47:W556–W560. https://doi.org/10.1093/nar/gkz430
Zhang Z et al (2021) SARS-CoV-2 spike protein dictates syncytium-mediated lymphocyte elimination. Cell Death Differ 28:2765–2777. https://doi.org/10.1038/s41418-021-00782-3
Acknowledgements
We thank Jianming Zeng (University of Macau) and all members of his bioinformatics team, Biotrainee, for generously sharing their experience. We thank all authors who contributed valuable data and made them public.
Funding
Y.L. is supported, in part, by the Sun Yat-sen University Start-up Funding, grant 201603, Y.W. is supported by the National Natural Science Foundation of China (Grant No. 82100184), the Natural Science Foundation of Guangdong (Grant No. 2022A1515012521), and the Beijing Xisike Clinical Oncology Research Foundation (Grant No. Y-Young20220281).
Author information
Authors and Affiliations
Contributions
SC and LZ performed the research, collected and analyzed the data, wrote the manuscript. YS and KX collected data. YL and YW conceptualized the study and reviewed and edited the manuscript. All authors gave their final approval of the version submitted for publication.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical Approval
No local ethical approval, official statement, or informed consent was necessary since the clinical data were obtained from publicly available databases.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, S., Zhang, L., Song, Y. et al. A Comprehensive Analysis of NRP1 in Malignancies Provide Therapeutic Implication for Treating Cancer Patients Infected with SARS-CoV-2. Biochem Genet 62, 2399–2417 (2024). https://doi.org/10.1007/s10528-023-10518-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10528-023-10518-2