Abstract
Polycystic ovary syndrome (PCOS) is a common multifaceted endocrine disorder among reproductive-aged women. Deranged luteinizing hormone levels and associated downstream signaling cascade mediated by its receptor luteinizing hormone chorionic gonadotropin receptor (LHCGR) are pivotal in the etiopathogenesis of PCOS. Genetic variations in the LHCGR have been associated with PCOS risk. However, the results are mixed and inconclusive. We evaluated the association of the LHCGR rs2293275 polymorphic variant with PCOS risk and its association with clinico-biochemical features of PCOS. 120 confirmed PCOS cases and an equal number of age-matched controls were subjected to clinical, biochemical, and hormonal investigations. Genotyping for rs2293275 was performed using polymerase chain reaction-restriction fragment length polymorphism. Logistic regression models were used to calculate odds ratios (ORs) at 95% confidence intervals (95% CIs). In the current study, PCOS cases reported a lower number of menstrual cycles per year than respective controls. A significantly higher BMI, Ferriman Galway score, levels of serum testosterone, insulin, TSH, FSH, and fasting glucose were observed in cases than in controls (p < 0.01). Compared to GG carriers, we observed a higher risk of developing PCOS in the subjects who harbored GA (OR 10.4, p < 0.0001) or AA (OR 7.73, p = 0.02) genotype. The risk persisted in the dominant model (GA + AA) as well (OR 10.29, p = 0.01). On stratification, a higher risk of developing PCOS was observed in variant genotype carriers who had a family history of either type two diabetes mellitus (OR 117; p < 0.0001) or hirsutism (OR 79; p < 0.0001). We also found significantly elevated levels of serum LH levels in the subject harboring GA and AA genotypes when compared to GG carriers. In the present study, we report a significant association of the LHCGR rs2293275 variant with the PCOS risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Worldwide, polycystic ovary syndrome (PCOS) is the most prevalent female endocrinopathy (Castillo-Higuera et al. 2021). This disorder starts early in life and significantly affects the reproductive phase of a woman’s life. It also has a lifelong impact on their metabolic health in the form of different comorbidities like type two diabetes mellitus (T2DM), cardiovascular diseases. (La Vignera et al. 2020). Phenotypically, PCOS is characterized by hyperandrogenism, polycystic ovarian morphology, oligo-anovulation, irregular menstrual cyclicity, infertility, alopecia, acne, hirsutism, and metabolic derangements including insulin resistance (IR), and hyperinsulinemia. Although these symptoms are non-uniform and follow a heterogeneous pattern but do impact the physical, psycho-sexual, emotional, and financial health of the women (Hiam, Moreno-Asso et al. 2019). The global prevalence of PCOS ranges between 5 and 10%, depending on the diagnostic criteria used (Castillo-Higuera et al. 2021). However, limited prevalence data from India suggests it to be a growing epidemic with 19–23% prevalence and is parallel to that of T2DM (Ganie and Kalra 2011).
The heterogenous aetio-pathophysiology of PCOS is a multifaceted and poorly understood orchestration of gene–gene and gene-environment interactions. Elevated androgen levels are central in the clinical phenotypes of PCOS patients. Furthermore, instigating endocrine abnormalities include an aberrant increase in gonadotropin-releasing hormone (GnRH), elevated luteinizing hormone (LH), sub-optimal levels of follicle-stimulating hormone (FSH), and subsequent hyperandrogenism leads to ovarian dysfunction and improper folliculogenesis. All of these hormonal derangements are implicated in the pathophysiology of PCOS. Normal ovarian function and follicular growth are a consequence of the complementary activities of FSH and LH. Any deviation of the ratio of LH to FSH from unity is an indication of abnormal ovarian function. The LH-mediated downstream cellular functions are transduced upon binding of LH to its receptor, the luteinizing hormone choriogonadotropin receptor (LHCGR). This G-protein coupled receptor LHGCR is expressed on the ovarian theca cells and regulates the action of both LH and choriogonadotropin in steroid biogenesis. The binding of these ligands to LHCGR induces a conformational shift, leading to its activation and subsequent signaling via the second messenger (cAMP). This signaling cascade is mediated by specific kinases to regulate the expression of genes involved in steroid biogenesis (Atoum et al. 2022). Therefore, any genetic variations altering the LHCGR protein structure or function would directly impact ovarian function and associated diseases including PCOS.
The gene encoding LHCGR is located on Chromosome 2 (Gromoll et al. 1992; Ulloa-Aguirre et al. 2014) and is highly polymorphic with more than 300 single-nucleotide polymorphisms (SNPs) reported so far. Studies have persistently evaluated the association of these polymorphic variants with PCOS, and the results are mixed and inconclusive. The variation in these results has been attributed to ethnic variations and study designs. Kashmir valley, a north Indian state represents an ethnically distinct population with a conserved genetic pool where consanguineous marriages are common. The prevalence of PCOS has been reported to be as high as ~ 28.9% by NIH criteria and 34.3% by AE-PCOS criteria (Ganie et al. 2020). Given these observations, the Kashmiri population offers a unique setting for evaluating the genetic predisposition of PCOS. Therefore, we conducted a case–control study to evaluate the association of the LHCGR polymorphic variant (rs2293275) with the PCOS risk and its effect modification on the disease phenotypes.
Materials and Methods
Study Subjects, Their Clinical Assessment, and Anthropometric Assessment
We invited 137 women aged between 18 and 40 years for the current prospective case–control study visiting the PCOS clinic at the Department of Endocrinology, Sher-i-Kashmir Institute of Medical Sciences (SKIMS) Srinagar, Kashmir from January 2018 to January 2021. The subjects who agreed to participate underwent a complete clinical examination and anthropometric measurements like measurement of height, weight, waist-hip circumference ratio, and body mass index (BMI). The clinical history included information on the age of menarche, presence of acne, alopecia, and menstrual history. The assessment for hirsutism was done using a modified Ferriman-Gallwey score by counting nine specified body areas. A score of > 8 out of a total of 36 was taken as significant. The Rotterdam criteria were used for the diagnosis of PCOS which states that two out of three features need to be present to make the diagnosis of PCOS. These features include (1) Oligo- or anovulation (< eight menstrual cycles in the presenting year) (2) Clinical and/or biochemical signs of hyperandrogenism and (3) Polycystic ovaries (either 12 or more follicles measuring 2–9 mm in diameter, or an ovarian volume of > 10 mL or 12). However, women suffering from any endocrinological abnormality like congenital adrenal hyperplasia, Cushing’s syndrome, androgen-secreting neoplasms, androgenic/anabolic drug use/abuse, syndromes of severe IR, hyperprolactinemia, and thyroid dysfunction were excluded from the study. Of all the invited subjects, 11 did not agree to participate and six were ineligible. We also recruited an equal number of age-matched and apparently healthy subjects as controls (n = 120). The subjects were enrolled as controls only if they displayed no evidence of menstrual irregularity and clinical or biochemical hyperandrogenism from various medical camps organized across various colleges and universities in Kashmir valley. The study protocol was approved by the institutional ethics committee (IEC No.RP55/19), SKIMS. Written informed consent was collected from all the subjects.
Sample Collection
Five milliliters of peripheral blood were collected from all the participating subjects after 8–12 h of overnight fasting for analyzing various biochemical and hormonal parameters. Two milliliters of the collected blood were transferred into an EDTA vial and 3 ml were transferred into the clot-activated vial for the separation of serum. The blood and sera samples are stored at − 80 °C till further processing.
Biochemical and Hormonal Analysis
All the PCOS cases and controls were subjected to biochemical analysis for the following parameters: fasting blood glucose, oral glucose tolerance test (OGTT), triglycerides (TG), low-density lipoprotein (LDL) high-density lipoprotein (HDL), total cholesterol, uric acid, urea, creatinine, alkaline transferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), bilirubin, albumin and total protein. The biochemical estimations were carried out using a fully automatic biochemistry analyser (Response 910, Diasys) using standard commercially available kits following the manufacturer’s instructions. The immuno-chemical measurement of hormones including fasting insulin, FSH, LH, testosterone, prolactin, TSH, and T4 were analyzed by Electrochemiluminescence using Cobas e 411 (Roche diagnostics). The IR was evaluated in three different ways—Homeostasis model assessment of insulin resistance (HOMA-IR), quantitative insulin sensitivity check-index (QUICKI), and fasting glucose to fasting insulin ratio (FGIR). The HOMA index was calculated as [fasting serum insulin (μIU/mL) × fasting glucose (mg/dL)]/405. The QUICKI was calculated as 1/[log fasting insulin (μIU/mL)+log fasting glucose (mg/dL)]. High HOMA-IR, low QUICKI, and low FGIR scores denote insulin resistance (low insulin sensitivity). The BMI was calculated as body weight (kg) divided by body height squared (m2).
DNA Isolation and Genotype Analysis
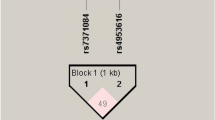
Genomic DNA was isolated from the peripheral blood of all the subjects using the standard phenol–chloroform/Isoamyl-alcohol method. The quality and quantity were determined by measuring A260/A280 in a Nano-drop (Jenway Genova) and by running the samples on 1% agarose gel. DNA was stored at − 20 °C until further processing. The targeted DNA fragment was amplified by PCR, using specific forward primer 5′-CCTCTTCTCTTTCAGACAGA-3′ and reverse primer 5′-CATGCAAATACTTACAGTGTTTTGGTA-3′ as per the published literature (Thathapudi et al. 2015). PCR was performed in three steps using Sure-thermocycler 8800 (Agilent Technologies). Briefly, the PCR conditions included an initial denaturation at 95 °C for 5 min, followed by 35 cycles of denaturation at 95 °C for 1 min, annealing at 58.5 °C for 30 s, extension at 72 °C for 45 s, and a final extension at 72 °C for 5 min. The 111 bp amplified PCR product was then digested with RsaI Restriction enzyme at 37 °C for 2 h and was electrophoresed on 3% agarose gel. The banding pattern demonstrated an undigested 111 bp in the case of GG (homozygous wild) genotype, 111/86/25 bp in the case of GA (heterozygous) genotype, and 86/25 bp in the case of AA (homozygous mutant) genotype.
Statistical Analysis
All the categorical variables were presented as numbers and percentages while the continuous variables were presented as mean ± standard deviation. The clinical, anthropometric, hormonal, and metabolic variables were compared between PCOS and controls by unpaired student t-test. We used logistic regression models to calculate odds ratios (ORs) as an estimate of risk at 95% confidence interval (CI). The p-value of the magnitude < 0.05 was considered statistically significant. All the statistical calculations were performed using STATA Software, version 16 (STATA Corp., College Station, TX, USA).
Power Calculations
Power calculations were carried out using the GAS power calculator (csg.sph.umich.edu/abecasis/gas_power_calculator). Using the dominant model, post hoc power analysis revealed that the study is significantly powered to detect any associations (power of the study:1-β = 87% at the significance level α = 0.01).
Results
Clinical, and Biochemical Profile of the Study Subjects
The anthropometric, clinical, and biochemical parameters of PCOS cases and controls are given in Table 1. The mean age (± SD) of case and controls was 22.72 ± 4.53 and 23.37 ± 3.03, respectively. The number of menstrual cycles/years was significantly lower in cases (7.51 ± 3.25) than in controls (11.95 ± 0.20), (p < 0.0001). Unlike controls, the BMI (24.58 ± 4.02 vs. 21.98 ± 3.72) and FG (12.04 ± 4.45 vs. 5.96 ± 0.99) score was significantly higher in cases. The hormone levels including testosterone, TSH (3.65 ± 2.01) vs. 3.02 ± 1.48), insulin (18.99 ± 15.20) vs. (6.26 ± 3.25), and LH to FSH ratio were higher in cases than controls (p < 0.001). The indices of glycaemic control including fasting blood glucose (mg/dL) and fasting insulin levels (μIU/mL) were considerably higher in cases compared to controls (87.47 ± 8.58 vs. 83.67 ± 9.23; P = 0.001 and 18.99 ± 15.20 vs. 6.26 ± 3.25; P < 0.0001). Likewise, Insulin resistance assessed by HOMA-IR, QUICKI, and FGIR was significantly higher in PCOS patients when compared to controls (P < 0.0001). Moreover, in PCOS cases, significantly higher levels of liver and renal function parameters, and lipid profile indicators were observed when compared to controls (P < 0.0001), Table 1.
Distribution of LHCGRrs2293275 Genotypes and Alleles
The genotypic and allele frequencies of rs2293275 LHCGRc.G935A (Ser312Asn) in PCOS cases and controls are presented in Table 2. The frequency of heterozygous (GA) and homozygous (AA) genotypes in cases was significantly higher in cases than in controls. The variant allele (A) was significantly overrepresented in cases than the respective controls (p < 0.0001). We observed a higher risk of developing PCOS in the subjects who harbored either GA (OR 10.4, p < 0.0001) or AA (OR 7.73, p = 0.02) genotype. The risk persisted in the dominant model (GA + AA) as well (OR 10.29, p = 0.01), (Table 2).
Risk Modification by the Variant Genotype of rs2293275 LHCGR in Presence of Other PCOS Modulators
Like earlier reports (Rashid et al. 2022), we also found a significant association between the family history of T2DM and hirsutism with the PCOS risk (Table 3). On further stratification of the participants, we observed a higher risk of developing PCOS in the subjects who harbored the variant genotype and had a family history of either T2DM (OR 117; p < 0.0001) or hirsutism (OR 79; p < 0.0001) when compared to the wildtype carriers who did not have any above-mentioned positive family histories. We observed a synergistic effect modification by the variant genotype of rs2293275 in the subjects whose BMI was ≥ 24 (OR 204; p < 0.0001), albeit with wider confidence intervals due to low numbers in the model.
To evaluate the correlation between serum LH levels and the genotype of LHCGR rs2293275, we categorized all the subjects based on their genotype. Compared to GG carriers, we observed a significant linear increase in the serum LH levels in the subjects that harbored GA genotypes. The LH levels were further increased in the AA carriers compared to both GA or GG carriers (Fig. 1). Besides, we found a strong risk of developing PCOS in the subjects who had LH levels ≥ 12.5 (mIU/mL) and harbored the variant genotype of the rs2293275 (Table 3). We also found a synergistic effect modification of the PCOS risk in the subjects carrying the variant genotype and presented either alopecia (OR 34.29; p < 0.0001), acne (OR 9.42; p < 0.0001) or acanthosis (OR 16.8; p < 0.0001) (Supplementary table S 1).
Discussion
The present case–control study evaluated the association of a polymorphic variant rs2293275 of LHCGR (p.S312N) with the PCOS risk and its correlation with the clinical and biochemical indices. We found a significant association of rs2293275 with the PCOS risk and linearly increased LH levels in the subjects harboring heterozygous (GA) and the mutant (AA) genotype when compared to the wild-type (GG) genotype carriers.
Our results demonstrated a significant difference in genotypic as well as allelic frequencies of rs2293275 between PCOS cases and controls, indicating that women with GA and AA genotypes are at higher risk for developing PCOS. The higher frequency of the A allele found in PCOS cases confered a > twofold increased risk of developing PCOS in our study. These findings are in agreement with the earlier studies from different ethnicities (Capalbo et al. 2012; Bassiouny et al. 2014; Ha et al. 2015; El-Shal et al. 2016). However, no significant association of this variant with the risk of PCOS was reported in Caucasian and Bahraini populations (Valkenburg et al. 2009; Almawi et al. 2015). On the contrary, Thathapudi et al. revealed that the GG (major allele), rather than AA, conferred a > threefold risk of developing PCOS in South Indian women (Thathapudi et al. 2015). However, a recent meta-analysis reported a ~ fourfold increased risk of developing PCOS for minor allele (AA) carriers (Zou et al. 2019). These conflicting results among the studies might be attributed to differences in sample size, non-uniform diagnostic criteria, ethnic background, and study design.
The LH is an associated member of the glycoprotein family that stimulates follicular development, steroid biogenesis, corpus luteum formation, and ovulation (Dufau 1998; Ascoli et al. 2002). The LH acts by binding with LHCGR, and subsequent signal transduction plays a vital role in the ovulation process (Dufau 1998; Qiao and Han 2019). LHCGR gene is one of the few candidate genes recognized as susceptibility loci and consistently associated with the risk of PCOS in diverse ethnicities.
Abnormal LH signaling is believed to play a crucial role in augmenting ovarian androgen production in PCOS cases leading to anovulation (Balen 1993; Norman et al. 2007). Zhihua et al. showed that mutation in LHCGR causes abnormal LHCGR glycosylation, decreased LHCGR protein level, effects on subcellular localization, and reduced cellular ATP consumption. These observations indicated defective signal transduction that could lead to abnormal ovulation (Zhang et al. 2020). Reports have shown that enhanced expression or overactivation of LHCGR might contribute to the development of PCOS (Kanamarlapudi et al. 2016). In addition to the two-cell—two-gonadotrophin theory, LH modulates mRNA levels of multiple genes in the granulose cells through the LHCGR receptor, which can aid in the growth of follicles (Sasson et al. 2004; Lindeberg et al. 2007). The secretion of androgen hormones by ovarian theca cells promoted by LH may result in follicular maturation arrest. Consequently, the variation in the levels of LH may potentially influence the reproductive process including menstruation and fertility, thereby orchestrating the PCOS risk (Laven et al. 2002).
The LHCGR variant rs2293275 (p.S312N) lies in juxtaposition with the glycosylation signals of the LHCGR protein. Any variations in this vicinity might affect the trafficking and stability of the LHCGR, thereby increasing the risk of PCOS (Thathapudi et al. 2015). An earlier study reported that inactivating gene variants of the LHCGR cause gonadal resistance to LH thereby increasing the LH levels and subsequent anovulation (Segaloff 2009). Moreover, a recent study showed a strong association of LHCGR rs2293275 polymorphism with high LH levels and LH/FSH ratio in women with PCOS. The study suggested that high serum LH levels in PCOS subjects are important for PCOS diagnosis and may be useful as a molecular marker for the early detection of PCOS cases (Atoum et al. 2022). Given the important pivotal role of LH in androgen metabolism and ovulation, it can be a plausible explanation for the enhanced PCOS risk in the women that harbored the variant genotype of LHCGR in our study. However, further mechanistic studies are warranted to elucidate LHCGR (rs2293275) mediated PCOS etiology. On stratification analysis, similar to earlier reports, we found a significantly increased serum LH level in subjects with PCOS who harbored variant genotypes when compared to healthy controls (Piersma et al. 2006; El-Shal et al. 2016).
Maternal family history of PCOS is considered a risk factor in daughters (Rashid et al. 2022). PCOS is thought to be a heritable disorder based on familial case clustering (Rosenfield and Ehrmann 2016). The pervasiveness of PCOS or its clinical manifestations among first-degree relatives suggests that genetic and familial factors play a role in the disorder (Bruni, Capozzi et al. 2021). We found an enhanced risk in the subjects who had a family history of T2DM or hirsutism and harbored the variant genotype of rs2293275. These observations also suggest the heritability associated with the rs2293275 in PCOS women. Although in absence of a direct correlation, positive family history of T2DM has been previously associated with the development of PCOS (Kulshreshtha et al. 2013; Yilmaz et al. 2018). Vrbikova et al. reported that defective early beta cell function was characteristic of patients with PCOS who had a positive family history of T2DM (Vrbikova et al. 2009). They also reported a significant difference in glucose and lipid metabolism between PCOS patients with and without a family history of T2DM (Wang et al. 2021). A literature survey suggests that T2DM appears to be an important factor in predicting the risks of metabolic abnormalities in women with PCOS (Ehrmann et al. 2005; Vrbíková et al. 2008; Lerchbaum et al. 2014). However, further replicative and mechanistic studies are required to validate and unveil the underlying role.
Compared to healthy controls, we found an enhanced PCOS risk in subjects that harbored variant genotypes of rs2293275 and had either alopecia, acne, or Acanthosis nigricans. With 58–82% of hyperandrogenic women having PCOS, the androgen excess is considered to be the hallmark feature of PCOS (Pinola et al. 2017). Elevated LH levels or increased testosterone production from polycystic ovaries may cause hyperandrogenaemia (Ashraf et al. 2019). Elevated insulin levels may also trigger increased testosterone levels in women and thus modulate the risk of PCOS (Nestler et al. 1998). Consequently, the resulting androgen excess (hyperandrogenism) acts as the main promoting factor inducing anovulation and follicular arrest (Qiao and Feng 2011).
Obesity is a common finding in PCOS that worsens its phenotypes and is considered one of the most crucial pathophysiological features in PCOS. It also aggravates menstrual irregularity and increases serum total testosterone levels (Xita and Tsatsoulis 2006; Baldani et al. 2013). These elevated androgen levels in turn can affect follicle growth, metabolic process, and insulin levels, thereby enhancing the PCOS risk in obese women. Furthermore, a recent study showed that increased testosterone level promotes visceral fat accumulation and IR by inhibiting lipolysis and promoting lipogenesis (Rosenfield and Ehrmann 2016). Dysregulated lipid metabolism and IR are in turn associated with suppressed ovulation and high LH levels (Roth et al. 2014). In the current study, we found a synergistic effect on the PCOS risk in the subjects carrying the LHCGR variant genotype (GA+AA) and having BMI greater than ≥ 24; albeit with wider CIs due to low numbers in the model. Our findings are consistent with previous studies that highlight the contribution of BMI and LHCGR polymorphism to PCOS phenotypes (Thathapudi et al. 2015; Atoum et al. 2022). While the current study was statistically powered to detect any associations, however, the low number in the subsequent stratification analysis might be a concern of the present study.
Conclusion
The present study indicated the potential influence of LHCGR (rs2293275) polymorphism on the development and clinical course of PCOS. More replicative studies are warranted to substantiate our findings.
Data Availability
Data will be available to anyone on a reasonable request to the corresponding author.
References
Almawi WY, Hubail B, Arekat DZ, Al-Farsi SM, Al-Kindi SK, Arekat MR, Mahmood N, Madan S (2015) Leutinizing hormone/choriogonadotropin receptor and follicle stimulating hormone receptor gene variants in polycystic ovary syndrome. J Assist Reprod Genet 32(4):607–614
Ascoli M, Fanelli F, Segaloff DL (2002) The lutropin/choriogonadotropin receptor, a 2002 perspective. Endocr Rev 23(2):141–174
Ashraf S, Nabi M, Rasool SA, Rashid F, Amin S (2019) Hyperandrogenism in polycystic ovarian syndrome and role of CYP gene variants: a review. Egypt J Med Hum Gen 20(1):25
Atoum MF, Alajlouni MM, Alzoughool F (2022) A case-control study of the luteinizing hormone level in luteinizing hormone receptor gene (rs2293275) polymorphism in polycystic ovarian syndrome females. Public Health Genom 25(3–4):89–97
Aversa A, La Vignera S, Rago R, Gambineri A, Nappi RE, Calogero AE, Ferlin A (2020) Fundamental concepts and novel aspects of polycystic ovarian syndrome: expert consensus resolutions. Front Endocrinol. https://doi.org/10.3389/fendo.2020.00516
Baldani DP, Skrgatić L, Goldstajn MS, Vrcić H, Canić T, Strelec M (2013) Clinical, hormonal and metabolic characteristics of polycystic ovary syndrome among obese and nonobese women in the Croatian population. Coll Antropol 37(2):465–470
Balen AH (1993) Hypersecretion of luteinizing hormone and the polycystic ovary syndrome. Hum Reprod 8(suppl_2):123–128
Bassiouny YA, Rabie WA, Hassan AA, Darwish RK (2014) Association of the luteinizing hormone/choriogonadotropin receptor gene polymorphism with polycystic ovary syndrome. Gynecol Endocrinol 30(6):428–430
Bruni, V., A. Capozzi and S. Lello (2021). "The Role of Genetics, Epigenetics and Lifestyle in Polycystic Ovary Syndrome Development: the State of the Art." Reprod Sci.
Capalbo A, Sagnella F, Apa R, Fulghesu AM, Lanzone A, Morciano A, Farcomeni A, Gangale MF, Moro F, Martinez D, Ciardulli A, Palla C, Uras ML, Spettu F, Cappai A, Carcassi C, Neri G, Tiziano FD (2012) The 312N variant of the luteinizing hormone/choriogonadotropin receptor gene (LHCGR) confers up to 2·7-fold increased risk of polycystic ovary syndrome in a Sardinian population. Clin Endocrinol (oxf) 77(1):113–119
Castillo-Higuera T, Alarcón-Granados MC, Marin-Suarez J, Moreno-Ortiz H, Esteban-Pérez CI, Ferrebuz-Cardozo AJ, Forero-Castro M, Camargo-Vill Alba G (2021) A comprehensive overview of common polymorphic variants in genes related to polycystic ovary syndrome. Reprod Sci 28(9):2399–2412
Dufau ML (1998) The luteinizing hormone receptor. Annu Rev Physiol 60:461–496
Ehrmann DA, Kasza K, Azziz R, Legro RS, Ghazzi MN (2005) Effects of race and family history of type 2 diabetes on metabolic status of women with polycystic ovary syndrome. J Clin Endocrinol Metab 90(1):66–71
El-Shal AS, Zidan HE, Rashad NM, Abdelaziz AM, Harira MM (2016) Association between genes encoding components of the Leutinizing hormone/Luteinizing hormone-choriogonadotrophin receptor pathway and polycystic ovary syndrome in Egyptian women. IUBMB Life 68(1):23–36
Ganie MA, Kalra S (2011) Polycystic ovary syndrome – A metabolic malady, the mother of all lifestyle disorders in women – Can Indian health budget tackle it in future? Indian J Endocrinol Metab 15:239–241
Ganie MA, Rashid A, Sahu D, Nisar S, Wani IA, Khan J (2020) Prevalence of polycystic ovary syndrome (PCOS) among reproductive age women from Kashmir valley: a cross-sectional study. Int J Gynecol Obstet 149(2):231–236
Gromoll J, Gudermann T, Nieschlag E (1992) Molecular cloning of a truncated isoform of the human follicle stimulating hormone receptor. Biochem Biophys Res Commun 188(3):1077–1083
Ha L, Shi Y, Zhao J, Li T, Chen ZJ (2015) Association study between polycystic ovarian syndrome and the susceptibility genes polymorphisms in Hui Chinese women. PLoS ONE 10(5):e0126505
Hiam D, Moreno-Asso A, Teede HJ, Laven JSE, Stepto NK, Moran LJ, Gibson-Helm M (2019) The genetics of polycystic ovary syndrome: an overview of candidate gene systematic reviews and genome-wide association studies. J Clin Med 8(10):1606
Kanamarlapudi V, Gordon UD, López Bernal A (2016) Luteinizing hormone/chorionic gonadotrophin receptor overexpressed in granulosa cells from polycystic ovary syndrome ovaries is functionally active. Reprod Biomed Online 32(6):635–641
Kulshreshtha B, Singh S, Arora A (2013) Family background of Diabetes Mellitus, obesity and hypertension affects the phenotype and first symptom of patients with PCOS. Gynecol Endocrinol 29(12):1040–1044
Laven JS, Imani B, Eijkemans MJ, Fauser BC (2002) New approach to polycystic ovary syndrome and other forms of anovulatory infertility. Obstet Gynecol Surv 57(11):755–767
Lerchbaum E, Schwetz V, Giuliani A, Obermayer-Pietsch B (2014) Influence of a positive family history of both type 2 diabetes and PCOS on metabolic and endocrine parameters in a large cohort of PCOS women. Eur J Endocrinol 170(5):727–739
Lindeberg M, Carlström K, Ritvos O, Hovatta O (2007) Gonadotrophin stimulation of non-luteinized granulosa cells increases steroid production and the expression of enzymes involved in estrogen and progesterone synthesis. Hum Reprod 22(2):401–406
Nestler JE, Jakubowicz DJ, Falcon de Vargas A, Brik C, Quintero N, Medina F (1998) Insulin stimulates testosterone biosynthesis by human thecal cells from women with polycystic ovary syndrome by activating its own receptor and using inositolglycan mediators as the signal transduction system1. J Clin Endocrinol Metab 83(6):2001–2005
Norman RJ, Dewailly D, Legro RS, Hickey TE (2007) Polycystic ovary syndrome. Lancet (london, England) 370(9588):685–697
Piersma D, Berns EM, Verhoef-Post M, Uitterlinden AG, Braakman I, Pols HA, Themmen AP (2006) A common polymorphism renders the luteinizing hormone receptor protein more active by improving signal peptide function and predicts adverse outcome in breast cancer patients. J Clin Endocrinol Metab 91(4):1470–1476
Pinola P, Puukka K, Piltonen TT, Puurunen J, Vanky E, Sundström-Poromaa I, Stener-Victorin E, Lindén Hirschberg A, Ravn P, Skovsager Andersen M, Glintborg D, Mellembakken JR, Ruokonen A, Tapanainen JS, Morin-Papunen LC (2017) Normo- and hyperandrogenic women with polycystic ovary syndrome exhibit an adverse metabolic profile through life. Fertil Steril 107(3):788-795.e782
Qiao J, Feng HL (2011) Extra- and intra-ovarian factors in polycystic ovary syndrome: impact on oocyte maturation and embryo developmental competence. Hum Reprod Update 17(1):17–33
Qiao J, Han B (2019) Diseases caused by mutations in luteinizing hormone/chorionic gonadotropin receptor. Prog Mol Biol Transl Sci 161:69–89
Rashid R, Shah IA, Asrar MM, Godha M, Ganai BA, Ganie MA (2022) Family history of menstrual irregularity or diabetes mellitus enhances the susceptibility to polycystic ovary syndrome among subjects harboring rs7903146 genetic variant of TCF7L2. J Diabetes Metab Disord 21(1):769–776
Rosenfield RL, Ehrmann DA (2016) The Pathogenesis of polycystic ovary syndrome (PCOS): the hypothesis of PCOS as functional ovarian hyperandrogenism revisited. Endocr Rev 37(5):467–520
Roth LW, Allshouse AA, Bradshaw-Pierce EL, Lesh J, Chosich J, Kohrt W, Bradford AP, Polotsky AJ, Santoro N (2014) Luteal phase dynamics of follicle-stimulating and luteinizing hormones in obese and normal weight women. Clin Endocrinol (oxf) 81(3):418–425
Sasson R, Rimon E, Dantes A, Cohen T, Shinder V, Land-Bracha A, Amsterdam A (2004) Gonadotrophin-induced gene regulation in human granulosa cells obtained from IVF patients. Modulation of steroidogenic genes, cytoskeletal genes and genes coding for apoptotic signalling and protein kinases. MHR Basic Sci Repro Med 10(5):299–311
Segaloff DL (2009) Diseases associated with mutations of the human lutropin receptor. Prog Mol Biol Transl Sci 89:97–114
Thathapudi S, Kodati V, Erukkambattu J, Addepally U, Qurratulain H (2015) Association of luteinizing hormone chorionic gonadotropin receptor gene polymorphism (rs2293275) with polycystic ovarian syndrome. Genet Test Mol Biomarkers 19(3):128–132
Ulloa-Aguirre A, Reiter E, Bousfield G, Dias JA, Huhtaniemi I (2014) Constitutive activity in gonadotropin receptors. Adv Pharmacol 70:37–80
Valkenburg O, Uitterlinden AG, Piersma D, Hofman A, Themmen AP, de Jong FH, Fauser BC, Laven JS (2009) Genetic polymorphisms of GnRH and gonadotrophic hormone receptors affect the phenotype of polycystic ovary syndrome. Hum Reprod 24(8):2014–2022
Vrbíková J, Grimmichová T, Dvořáková K, Hill M, Stanická S, Vondra K (2008) Family history of diabetes mellitus determines insulin sensitivity and beta cell function in polycystic ovary syndrome. Physiol Res 57(4):547–553
Wang Y, Gao H, Di W, Gu Z (2021) Endocrinological and metabolic characteristics in patients who are non-obese and have polycystic ovary syndrome and different types of a family history of type 2 diabetes mellitus. J Int Med Res 49(5):3000605211016672
Vrbikova J, Bendlova B, Vankova M, Dvorakova K, Grimmichova T, Vondra K, Pacini G (2009) Beta cell function and insulin sensitivity in women with polycystic ovary syndrome: influence of the family history of type 2 diabetes mellitus. Gynecol Endocrinol 25(9):597–602
Xita N, Tsatsoulis A (2006) Review: fetal programming of polycystic ovary syndrome by androgen excess: evidence from experimental, clinical, and genetic association studies. J Clin Endocrinol Metab 91(5):1660–1666
Yilmaz B, Vellanki P, Ata B, Yildiz BO (2018) Diabetes mellitus and insulin resistance in mothers, fathers, sisters, and brothers of women with polycystic ovary syndrome: a systematic review and meta-analysis. Fertil Steril 110(3):523-533.e514
Zhang Z, Wu L, Diao F, Chen B, Fu J, Mao X, Yan Z, Li B, Mu J, Zhou Z, Wang W, Zhao L, Dong J, Zeng Y, Du J, Kuang Y, Sun X, He L, Sang Q, Wang L (2020) Novel mutations in LHCGR (luteinizing hormone/choriogonadotropin receptor): expanding the spectrum of mutations responsible for human empty follicle syndrome. J Assist Reprod Genet 37(11):2861–2868
Zou J, Wu D, Liu Y, Tan S (2019) Association of luteinizing hormone/choriogonadotropin receptor gene polymorphisms with polycystic ovary syndrome risk: a meta-analysis. Gynecol Endocrinol 35(1):81–85
Acknowledgements
The authors thank all the participants for volunteering in the study. The authors also thank the Multi-disciplinary Research Unit, SKIMS, Srinagar funded by the Department of Health Research, Govt of India, for providing necessary research facilities for carrying out this study.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
MAG conceived the study; MJM, MAG, ZAS, and SS designed the study. MJM and AR collected the data, and MJM and RR performed experiments. IAS, MJM, and MAG analyzed and interpreted the data. MJM, IAS, and MAG wrote the first draft of the manuscript. All the authors reviewed and approved the final draft of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The author has no relevant financial and non-financial interests to disclose.
Ethical Approval
This study was approved by the institutional ethics committee of SKIMS (SKIMS-IEC) under protocol number RP 55/19.
Consent to Participate
Informed consent was obtained from all participants included in this study.
Consent to Publish
No object or image was obtained or copied from any publication. The images used in this manuscript are my own.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Makhdoomi, M.J., Shah, I.A., Rashid, R. et al. Effect Modification of LHCGR Gene Variant (rs2293275) on Clinico-Biochemical Profile, and Levels of Luteinizing Hormone in Polycystic Ovary Syndrome Patients. Biochem Genet 61, 1418–1432 (2023). https://doi.org/10.1007/s10528-022-10327-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10528-022-10327-z