Abstract
This study aimed to investigate the effects of the 5-HT7 receptor agonist (LP44) and antagonist (SB269970) on LPS-induced in vivo tissue damage and cell culture by molecular methods. This study was conducted in two steps. For in vivo studies, 24 female rats were divided into four groups. Group I: healthy; II (2nd h): LPS 5 mg/kg administered intraperitoneally (i.p.); III (4th h): LPS 5 mg/kg administered i.p.; IV (8th h): LPS 5 mg/kg administered i.p. For in vitro studies, we used the A549 cell line. Groups: I control (healthy) (2–4 h); II LPS: 1 µg/ml E. Coli O55:B5 strain (2–4 h); III agonist (LP44) 10−9 M (2–4 h); IV antagonist (SB269970) 10−9 M (2–4 h); V LPS+agonist 10−9 M (LP44 1 µg/ml) (2–4 h); VI LPS+antagonist 10−9 M (2–4 h). In molecular analyses, we determined increased TNF-α, IL-1β, NF-κB, and 5-HT7 mRNA expressions in rat lung tissues and increased TNF-α, iNOS, and 5-HT7 mRNA expressions in the A549 cell line. In in vitro parameters, LP44 agonist administration-related decrease was observed. Our study showed that lung 5-HT7 receptor expression is increased in LPS-induced endotoxemia. All this data suggest that 5-HT7 receptor overexpression is an important protective mechanism during LPS-induced sepsis-related cell damage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sepsis is a complicated medical condition. It is an inflammatory response of the body, which also involves the development of multiple organ failure (Ruggieri et al. 2010). All around the world, 20–30 million people have sepsis every year and nearly 6 million of which are newborns and children, also 24,000 people die from sepsis every day (Reinhart et al. 2013). The inflammatory response which appears as a response to sepsis struggles to be regulated and balanced by mediators and cytokines.
Serotonin is released from the thrombocytes upon inflammation in cases such as endotoxemia, ischemia, and thrombosis (Mossner and Lesch 1998; Benedict et al. 1986). The serotonergic system which is engaged in sepsis plays a role in all inflammatory responses by several receptors. Considering their molecular pharmacological structures and stimulus transmission properties, there are 14 different 5-HT receptors, and they are divided into seven fundamental groups (5-HT1, 5-HT2, 5-HT3, 5-HT4, 5-HT5, 5-HT6, and 5-HT7). Some of these serotonergic receptors are involved in inflammatory and septic conditions. For example, in an endotoxic shock model, sarpogrelate, a 5-HT2A receptor antagonist, whose application reduced proinflammatory cytokines, enabled anti-inflammatory cytokines, protected hemodynamic disorders, and reduced lung inflammation and mortality (Nishiyama 2009). In another study, it was shown that the 5-HT2 receptor blocker cinanserin significantly reduced the shock edema in a burn (Hernekamp et al. 2013). On the other hand, in another study, 5-HT3 receptor antagonist granisetron, prevented inflammation and angiogenesis, which is increased in the inflammatory granulation tissue (Maleki-Dizaji et al. 2010).
The relationship between serotonin and receptors and sepsis and endotoxemia in the whole body has also been studied (Nishiyama 2009; Demling et al. 1985). However, the relationship between the 5-HT7 receptors which are dominant in the central system and newly discovered in the peripheral system could not be fully clarified yet. Being a biological monoamine, serotonin (5-HT) plays a role in many biological and pathological conditions (Yang et al. 2006). 5-HT7 is the last discovered serotonin receptor. This receptor is observed in the cardiovascular system, particularly in the coronary arteries (Nilsson et al. 1999), several regions in the brain (Leopoldo et al. 2011), the pulmonary arteries, and the aorta (Ullmer et al. 1995). There are four different 5-HT7 receptor isoforms: 5-HT7a, 5-HT7, 5-HT7c, 5-HT7d (Dean et al. 2006). Previously Albayrak et al. studied the effects of indomethacin and of 5-HT7 receptor agonist (AS-19) and antagonist (SB269970) in carrageenan-induced paw edema in rats. They observed that there may be anti-inflammatory and antioxidant effects of 5-HT7 receptor agonist and drew attention to the effects of 5-HT7 receptors in inflammation (Albayrak et al. 2013). The effects of 5-HT7 receptor agonist (AS-19) and antagonist (SB269970) on cecal ligation and puncture (CLP)-induced sepsis were studied, and it was found that AS-19 could reduce sepsis-related abnormal inflammatory response (Cadirci et al. 2013). However, the cell damage mechanism could not be shown in that study. It is quite important to show which cells have which effects in showing cell damage and its mechanism. More detailed studies are needed to show by which cells 5-HT7 is expressed in the lung tissue and to show the cell damage mechanism.
In this study, we aimed to create both in vitro and in vivo sepsis models with LPS, unlike the CLP model, and aimed to look at the effects of 5-HT7 agonist and antagonist on acute lung damage. Unlike the CLP model, there are two important reasons for conducting our study with LPS. Firstly, we need to work on in vitro cell culture to show in which cells sepsis-induced increased 5-HT7 expression develops and the cellular damage mechanism of this increase. In the cell culture, studies can only be done with LPS. Secondly, standardization is quite difficult in CLP-induced sepsis model. Since the same dose of LPS was used in each animal group, the groups and sepsis model were standardized in our study.
Based on all this information, the purpose of our study was to show the potential protective effects of 5-HT7 receptors on LPS-induced lung cell damage through in vivo and in vitro methods.
Materials and Methods
Animals
In our study, a total of 24 Sprague–Dawley female rats were used, with weights ranging between 180 and 200 g. Rats were provided from the experimental animal laboratory at the Atatürk University Experimental Research and Application Centre (ATADEM). During the experiment, the rats were given sufficient amounts of (ad libitum) water and pellet feed. Before the experiment, the animals were sheltered and fed in groups at normal room temperature (22 °C), with 65–70 % moisture, and with light control 12 h light, 12 h dark in the animal laboratory.
Chemicals and Reagents
Xylazine (Xylasinbio, Intermed Ecza Deposu Ltd.Şti., Ankara, Turkey) was administered at 10 mg/kg intraperitoneal (i.p.) dose for sedation. Ketamine (Ketalar, Pfizer, 50 mg/ml flacon, Istanbul, Turkey) was administered at 90 mg/kg i.p. dose for anesthesia. LPS (dissolved in 0.09 % NaCl) was administered at 5 mg/kg i.p. dose. SB269970, 5-HT7 receptor antagonist, was dissolved in dimethyl sulfoxide (DMSO)+dulbecco’s modified eagle’s medium (DMEM). LP44, 5-HT7 receptor agonist, was dissolved in DMEM. Alveolar epithelial A549 cells were provided by the Department of Genetics and Bioengineering, Yeditepe University (Istanbul, Turkey). LPS (LPS, E. coli serotype 055:B5), LP44, and SB269970 were purchased from Sigma–Aldrich (St. Louis, MO, USA).
Experimental Design
In our study, one healthy group and three experimental groups were created. In each group, a total of 24 female rats were used. Before starting the experiment, all animals were weighed and taken to the experiment protocols which are specified in the following groups.
Group I: healthy (6 rats) 2 ml 0.09 % NaCl (i.p.)
Group II: LPS was administered at (6 rats) 5 mg/kg doses (i.p.). E. Coli O55:B5 strain. (Sacrificed in the 2nd h after LPS administration).
Group III: LPS was administered at (6 rats) 5 mg/kg doses (i.p.). (Sacrificed in the 4th h after LPS administration).
Group IV: LPS was administered at (6 rats) 5 mg/kg doses (i.p.). (Sacrificed in the 8th h after LPS administration).
E. Coli O55:B5 strains were used as lipopolysaccharide (LPS). LPS was dissolved in 2 ml 0.09 % NaCl. In the groups which were given LPS, a high-dose anesthetic was applied and the animals were euthanized in the 2nd, 4th, and 8th h. Lung tissues were collected for molecular analyses.
Cell Culture
A549 cells were grown in a 75 cm2 culture flask using DMEM medium with 10 % FBS, 100 U/ml penicillin, 100 μg/ml streptomycin, and 2 mM l-glutamine. Cells were cultured in a humidified atmosphere at 37 °C by passing 5 % CO2. A flask containing 70–80 % confluent cells was subcultured in a 96-well plate (10,000 cells/well) and in a 6-well plate (1,000,000 cells/well) for the treatment. To reduce the effect of serum-derived factors, the medium was replaced by a serum-free culture medium. LPS and SB269970 were dissolved in a cell culture medium. LP44 was dissolved in DMSO and all cells were exposed to a 0.1 % final DMSO concentration.
Cell Viability Assay
The assay was performed by seeding A549 in 96-well plates. After placing them to the plates, the cells were treated with LPS (1, 10, 50, and 100 µg/ml) or various concentrations of LP44 and SB269970 (10−10–10−6M), respectively for 24 h. In order to examine the effects of LP44 and SB269970 on LPS-induced cell damage, the cells were treated with LP44 and SB269970 (10−10–10−8 M) for 60 min and then were exposed to LPS (10 µg/ml) for 24 h. Following incubation, a 20 μl methylthiazol tetrazolium (MTT) solution (5 mg/ml) was added to each well and the cells were incubated for 4 h at 37 °C. Then, DMSO was added to dissolve the blue formazan product, and cell viability was determined by measuring the absorbance at a wavelength of 550 nm (Epoch Microplate Spectrophotometer, BioTek, USA).
Real-Time PCR
Relative tumor necrosis factor-α (TNF-α), inducible nitric oxide synthase (iNOS), and 5-HT7 receptor mRNA expression analyses were performed with the StepOne Plus real-time polymerase chain reaction (PCR) system (Applied Biosystem) using cDNA synthesized from A549 and rat lung tissue RNAs. Real-time PCR was performed using primers generated for: human TNF-α forward: 5′-AGGTTCTCTTCCTCTCACATAC-3′; reverse: 5′-ATCATGCTTTCAGTGCTCATG-3′; rat TNF-α forward: 5′-GCTCCCTCTCATCAGTTCCA-3′; reverse: 5′-CTCCTCTGCTTGGTGGTTTG-3′; human 5-HT7 receptor forward: 5′-TTCTCTCCGTCTGGCTTCTC-3′; reverse: 5′-GCACACCTTATCATCATTTACATTCT-3′; rat 5-HT7 receptor forward: 5′-AGACTGCTCAAACACGAAAGG-3′; reverse: 5′- AAGGCTCCCACGATGATCC-3′; rat IL-1β forward: 5′-AGTGCTGACAATCTGTATGTACC-3′; reverse: 5′- ACTAGGCTTTGCTCTTCTCTTAC-3′; rat NFkB forward: 5′-ATCATCAACATGAGAAACGATCTGTA’; reverse: 5′-CAGCGGTCCAGAAGACTCAG-3′; human iNOS forward: GAAGCGGAGACCCAAGAGA; reverse: TCGCAAAGAGGATGGTGACT; human β-actin forward: 5′-GCAAGCAGGAGTATGACG AGT-3′; reverse: 5′-CAAGAAAGGGTGTAACGCAACTAA-3′; and rat β-actin forward: 5′-TGGTGGGTATGGGTCAGAAG-3′; reverse: 5′-GACAATGCCGTGTTCAATGG-3′ (Primer Design Ltd, Southampton, UK). The results were expressed as relative fold and compared with the control groups. Expression data of β-actin in each cell group were used as an endogenous control. For each cell group, triplicate determinations were performed for both targets in a 96-well optical plate using 9 µl of cDNA (100 ng), 1 µl of Primer Perfect Probe mix, and 10 µl of QuantiTect Probe PCR master mix (Qiagen) in each 20 µl reaction. The plates were heated for 2 min at 50 °C, 10 min at 95 °C, and a subsequent 40 cycles of 15 s at 94 °C and 60 s at 60 °C. All data were expressed as fold changes in expression compared with the cell groups using the 2−ΔΔCt method (Livak and Schmittgen 2001).
Statistical Analysis
All data were subjected to one-way analysis of variance using the IBM SPSS Statistics 20.0 software program (SPSS Inc., Chicago, Illinois, USA). Differences among the groups were determined using the Tukey test and were considered significant when the p value was less than 0.05 in a 95 % confidence interval. All results were given as mean+standard deviation (SD).
Results
Studies of Gene Expression of In Vivo Study of Sepsis
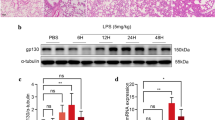
In the LPS-induced endotoxemia model, mRNA expressions of the interleukin-1β (IL-1β), TNF-α, and nuclear factor kappa B (NF-κB) cytokines in the 2nd, 4th, and 8th h following LPS application were measured in the rats (Fig. 1a–c). When we look at the mRNA expressions of the inflammatory cytokines in the rats’ lung tissues, and compare the rat groups in which endotoxemia was created with LPS and the healthy group, a significant increase was seen for each 2nd, 4th, and 8th h measured. While the highest mRNA expressions were observed in the 4th h for TNF-α, the highest value was measured in the 2nd h for IL-1β and NF-κB (Fig. 1a–c).
a–d LPS-induced expression of IL-1 (a),TNF-α (b), NF-κB (c), 5-HT7(d) receptor mRNAs at 2nd h, 4th, and 8th h in rats. Gene expression was detected by quantitative real-time PCR analysis. Results were normalized to β-actin (housekeeping gene control). The relative expression levels were calculated by the 2−ΔΔCT method and were indicated as ‘fold change’ compared with control groups. Differences statistically significant; *p < 0.05, **p < 0.01, ***p < 0.001 when compared with healthy group according to one-way ANOVA–Tukey test
The mRNA expressions of the 5-HT7 receptors in the lung tissues of rats with LPS-induced endotoxemia were significantly increased when compared to that of healthy rat groups at all hours (Fig. 1d).
Viability of A549 Cells
To study the cytotoxic effect of LPS, the A549 cells were treated with or without different concentrations of 5-HT7 receptor agonist LP44 and SB269970 (10−10–10−6 M) for 24 h, and cell viability was determined by MTT assay. A549 cells treated with LPS at 1 μg/ml concentrations were found to have no effect on cell viability, while a significant decrease in cell viability was observed from 10 μg/ml onward (Fig. 2a). The cytotoxic effects of LP44 and SB269970 were determined up to 10−7 M (Fig. 2b, c). A cytotoxic concentration of LPS (10 μg/ml) and non-cytotoxic concentrations of LP44 and SB269970 from 10−10 to 10−8 M were used in the subsequent experiments. The cells were incubated with varying LP44 and SB26990 concentrations for 60 min before 10 µg/ml LPS in a serum-free medium. As presented in (Fig. 2d, e), for this experiment, the A549 cells were treated with 10 μg/ml LPS in the presence or absence of LP44 at a concentration of 10−10–10−8 M. LP44 up to 10−8 M concentration significantly increased cell growth in the presence of 10 μg/ml LPS (p < 0.001). However, SB269970 had no effect on cell viability in the presence of LPS (Fig. 2e). The results suggested that 5-HT7 receptor agonist LP44 possesses the ability to attenuate the cell injury induced by LPS, and this shows that the protective effects of LP44 increased in a dose-dependent manner.
a–e Effect of different concentrations of LPS, LP44, and SB269970 on the viability of A549 cells. A549 cells were treated with or without different concentrations of LPS (1–100 μg/ml), LP44, and SB269970 (10−6–10−10 M) or in a 96-well plate for 24 h, and the cell viability was measured by MTT assay. Results were expressed as % viability of cells compared to control (mean ± SD). Differences statistically significant, *p < 0.05, **p < 0.01, ***p < 0.001 when compared with control and # p < 0.05, ## p < 0.01, ### p < 0.001 compared with LPS group according to one-way ANOVA–Tukey test
Studies of Gene Expression In Vitro Studies
The mRNA expression levels of TNF-α, iNOS, and 5-HT7 receptor for treated and untreated A549 cells were analyzed. As shown in (Fig. 3a, b), TNF-α expression levels increased significantly in LPS-exposed groups 386-fold (2nd h) and 1797-fold (4th h) compared to that in the control groups (p < 0.001). The increase in the TNF-α mRNA expression decreased to 21- and 177-fold in the LP44+LPS group when compared to the control group. This reduction in LP44+LPS groups was statistically significant compared to the LPS groups (p < 0.001). There was no significant difference between the LPS and LPS+SB269970 groups (351-fold for 2nd h and 1546-fold for 4th h). The LP44 and SB269970 groups by themselves had no effect on TNF-α mRNA expression levels, either at the 2nd h or the 4th h (Fig. 3a, b).
a–f Effect of LP44 and SB269970 on LPS-induced expression of TNF-α (a, b), iNOS (c, d), and 5-HT7 (e, f) mRNAs at 2nd h and 4th h in A549 cells. A549 cells were treated with or without LPS or LPS with LP44 (10−9 Μ) and SB269970 (10−8 Μ) or alone for 2nd and 4th h in six-well plate. The cDNA was prepared from total RNA and subjected to real-time PCR using specific TaqMan probes of TNF-α, iNOS, and 5-HT7 receptor. Expressions were normalized with the housekeeping gene β-actin. Data shown are mean ± SD. Differences statistically significant, *p < 0.05, **p < 0.01, ***p < 0.001 when compared with control and # p < 0.05, ## p < 0.01, ### p < 0.001 compared with LPS group according to one-way ANOVA–Tukey test
iNOS expression levels increased significantly in LPS-exposed groups 2-fold (2nd h) and 9-fold (4th h) compared to that in the control groups (p < 0.001). The increase in the iNOS mRNA expression decreased to 1- and 4-fold in the LP44+LPS group when compared to the control group. This reduction in LP44+LPS groups was statistically significant compared to the LPS groups (p < 0.001). There was no significant difference between the LPS and LPS+SB269970 groups (2-fold for 2nd h and 10-fold for 4th h). The LP44 and SB269970 groups by themselves had no effect on iNOS mRNA expression levels, either at the 2nd h or the 4th h (Fig. 3c, d).
Additionally, the 5-HT7 receptor mRNA gene expression (Fig. 3e, f) significantly increased in LPS groups at 2nd h and 4th h (6- and 27-fold, respectively), while administration of LP44 to LPS groups decreased those levels significantly at 2nd h. At 4th h, LP44-treated LPS groups showed that 5-HT7 receptor expression increased significantly to 73-fold compared to the control groups (p < 0.001). SB269970-treated LPS groups showed that 5-HT7 receptor expression increased by 9- and 108-fold at both times as compared to the control groups (<0.001). LP44 and SB269970 by themselves had no effect on the expression levels of 5-HT7 receptor at 2nd h, while LP44 and SB269970 significantly increased expressions at 4th h 48- and 31-fold compared to the control groups.
Discussion
Despite the studies done, sepsis still plays a considerable role in death today. It is a clinical entity with ongoing high mortality in pediatric and adult intensive care units. Therefore, new medications in many sepsis-related models and the new pathways which can shed light on the sepsis mechanism are still being studied. We have examined the effect of 5-HT7 receptors on the etiopathogenesis of the sepsis and obtained very important results before. However, our previous studies only focused on a single model, i.e., the in vivo CLP model. The CLP sepsis model is a model which is quite close to the sepsis model created in the clinic and constitutes a long term and slowly increasing cytokine response (Dejager et al. 2011; Buras et al. 2005; Schabbauer 2012). However, there is another sepsis model, which is LPS induced, instead of CLP induced in experimental animals. The most important aspect of this model is that it progresses with a very rapid and excessively strengthening cytokine storm (Dejager et al. 2011; Buras et al. 2005). We encounter LPS as the only model in in vitro cell culture studies which are done to examine the effects of sepsis at the cellular level (Kang et al. 2015). In this study, unlike CLP, both in vitro and in vivo sepsis models were induced with LPS. The effects of 5-HT7 agonist and antagonist were studied. In the sepsis model which was induced, in vivo (rat lung tissue) and in vitro (A549 cell line) 5-HT7 receptor existence was examined. Moreover, in vivo tissue cytokine levels (TNF-α, IL-1β, NF-κB), and in vitro TNF-α, iNOS, and 5-HT7 levels were also examined.
In the LPS-induced sepsis mechanism process, ligand activation occurs upon connecting TLR4 to the ligand, and it stimulates the protein kinase families, which are activated by mitogen and NF-κB by means of the intracellular part. With this stimulation, the genes of the cytokine and proinflammatory products such as IL-1β and TNF-α are activated. This process is the natural immune response of the host (Tosi 2005; Tizard 2004; Chen et al. 2005). TNF-α and IL-1β are macrophage-derived proinflammatory cytokines that play an important role in the pathogenesis of septic shock and multiple organ disorder (Damas et al. 1992). These inflammatory mediators have a quite important role in the pathogenesis of sepsis-induced acute lung damage (Bhatia and Moochhala 2004). NF-κB is a transcription factor and is a dimeric transcription factor in relation to the regulation of genes in pathological events such as inflammation and apoptosis (Baeuerle 1998; Waddick and Uckun 1999). It enables the expressions of proinflammatory proteins (e.g.,: iNOS, TNF-α) and the formation of the cellular response, growth, and immune system (Shishodia and Aggarwal 2004). The enzymes which are stimulated and released with NF-κB activation stimulate the defense of the host by cytokines and mediators against microbes and induce inflammatory events. Once this process starts, the pathogen can be eliminated. If inflammatory reaction cannot be limited, it might lead to the destruction of the host cells (Akça 2007).
In our study, it was observed that in the LPS-induced sepsis model, as we expected, the proinflammatory cytokine levels increased in the rats. In the LPS organism, NF-κB activation occurs depending on its activation with the LPS–LBP complex combination. Depending on this activation, TNF-α and IL-1β inflammatory cytokines are activated. The organism’s first reaction to the sepsis is an increase in the TNF-α cytokine level. NF-κB and IL-1β reached the highest level in the 2nd h after LPS administration. One of the most important characteristics of the LPS-induced sepsis model is that the increase in the cytokine is too rapid and in an excessive amount (Eskandari et al. 1992; Evans et al. 1989). As for TNF-α, on the other hand, it was observed that the gene expression levels reached the highest level in the 4th h in the PCR study which was done on the lung tissue. Another important result of our in vivo study is the 5-HT7 lung expression levels which occur based on the hours after the inducement of the sepsis. When we consider the results, 5-HT7 expression increased quite substantially based on time. This shows that 5-HT7 receptors play an important role in the LPS-induced sepsis model. These results are similar to the CLP-induced sepsis model which was developed by us before (Cadirci et al. 2013). However, in order to determine whether this 5-HT7 expression is in the lung tissue or supportive tissues and how the potentially responsible cells will respond to 5-HT7 agonists and antagonists, we examined the effects of 5-HT7 on the agonist LP44 and antagonist SB269970 in sepsis in the sepsis model which is created in vitro in the A549 cell line.
The first response to bacterial infections is NO synthesis from the macrophages. NO has a role in nonspecific immunity. NO contributes to immunity by having a fatal cytotoxic effect on the bacteria, viruses, and tumor cells upon stimulation of the macrophages by bacteria endotoxins, protozoa, viruses, parasite antigens, and the stimulated macrophages producing iNOS. NO shows this cytotoxic effect through inducing glycolysis of many pathogens (such as bacteria and parasites) and ATP-producing tumor cells, oxidative phosphorylation, and inhibiting some Fe-containing enzymes TCA cycle (Lepoivre et al. 1991, 1997; Aladağ et al. 2000; Özkan and Akgül 2010; El Nehir and Karakaya 2004). While NO concentrations are found at 100–500 nm levels under normal physiological conditions, NO concentrations increase nearly ten times as a result of the stimulation of iNOS by factors such as TNF-α, IL-1, interferon, and endotoxin (Kuyumcu et al. 2004; Kürkçü 2008; İstanbul 2004). Although the NO which is produced in high amounts by iNOS is shown to be damaging and toxic, the NO which is produced in structurally low levels by eNOS is necessary for protecting endothelium function (Albrecht et al. 2003). In the LPS-induced in vitro endotoxemia model 5-HT7 receptor agonist LP44 reduced the LPS-induced iNOS amount at the 2nd h. LPS and SB269970 antagonists, on the other hand, were observed to increase the LPS-increased iNOS amount more.
It was shown that the TNF-α mRNA expression increased in the A549 cell line group which was given LPS, and it was shown that this increase was recovered by the administration of 5-HT7 receptor agonist. There was no extra change in the TNF-α mRNA expression in antagonist group. These results have suggested us that the increased 5-HT7 expression in the sepsis could play a protective role. In conditions which can lead to cellular damage such as LPS administration, cells might be trying to overcome this damage by increasing 5-HT7 expression. There are limited studies about the relationship between 5-HT7 receptors and the immune system. These receptors were found in the T-cells in the peripheral system and were shown to be quite important in the activation and regular functioning of these cells (Leon-Ponte et al. 2007). We have also examined their effects on sepsis and inflammation in our previous studies (Albayrak et al. 2013; Cadirci et al. 2013). The serotonin source in lung tissue is intravascular thrombocytes, and it has been shown in recent studies that they are also secreted from the neuroendocrine and neuroepithelial bodies which are found in the airway epithelium (Cazzola and Matera 2000; Livermore et al. 2015). In their study in 2010, Segura et al. showed that asthma physiopathology also involved 5-HT7 receptors (Segura et al. 2010). Moreover, another study showed that the expression of some serotonin receptors increased in the lung tissue in smokers (Dupont et al. 2014). As supporting evidence for all these studies, 5-HT7 agonist application prevented cell damage and increased cell vitality in the LPS-induced cell damage in the cell culture.
Conclusion
As a result, the increase in 5-HT7 expression in LPS-induced sepsis is considered an important protective mechanism in our study. The agonist application’s prevention of this damage is one of the most important pieces of evidence of this result. At the same time, it was found in our study that 5-HT7 expression and defense mechanism did not result from the supportive cells in the lung or the immune cells, but directly from the lung cells.
References
Akça AGH (2007) Immuniteye Genel Bakış ve Paraziter Hastalıklarda Immunite. Tıbbi ve Veteriner Immunoparazitoloji, Türkiye: Parazitoloji Derneği Yayınları. Yayın No:21. İzmir, p 430–431
Aladağ MA, Türköz Y, Özerol İH (2000) Nitrik oksit ve nörofizyopatolojik etkileri. Turkiye Klinikleri J Med Sci 20(2):107–111
Albayrak A, Halici Z, Cadirci E, Polat B, Karakus E, Bayir Y et al (2013) Inflammation and peripheral 5-HT7 receptors: the role of 5-HT7 receptors in carrageenan induced inflammation in rats. Eur J Pharmacol 715(1–3):270–279
Albrecht EW, Stegeman CA, Heeringa P, Henning RH, van Goor H (2003) Protective role of endothelial nitric oxide synthase. J Pathol 199(1):8–17
Baeuerle PA (1998) Pro-inflammatory signaling: last pieces in the NF-κB puzzle? Curr Biol 8(1):R19–R22
Benedict CR, Mathew B, Rex KA, Cartwright J Jr, Sordahl LA (1986) Correlation of plasma serotonin changes with platelet aggregation in an in vivo dog model of spontaneous occlusive coronary thrombus formation. Circ Res 58(1):58–67
Bhatia M, Moochhala S (2004) Role of inflammatory mediators in the pathophysiology of acute respiratory distress syndrome. J Pathol 202(2):145–156
Buras JA, Holzmann B, Sitkovsky M (2005) Animal models of sepsis: setting the stage. Nat Rev Drug Discov 4(10):854–865
Cadirci E, Halici Z, Bayir Y, Albayrak A, Karakus E, Polat B et al (2013) Peripheral 5-HT7 receptors as a new target for prevention of lung injury and mortality in septic rats. Immunobiology 218(10):1271–1283
Cazzola M, Matera MG (2000) 5-HT modifiers as a potential treatment of asthma. Trends Pharmacol Sci 21(1):13–16
Chen X-M, O’Hara SP, Nelson JB, Splinter PL, Small AJ, Tietz PS et al (2005) Multiple TLRs are expressed in human cholangiocytes and mediate host epithelial defense responses to Cryptosporidium parvum via activation of NF-κB. J Immunol 175(11):7447–7456
Damas P, Ledoux D, Nys M, Vrindts Y, De Groote D, Franchimont P et al (1992) Cytokine serum level during severe sepsis in human IL-6 as a marker of severity. Ann Surg 215(4):356
Dean B, Pavey G, Thomas D, Scarr E (2006) Cortical serotonin7, 1D and 1F receptors: effects of schizophrenia, suicide and antipsychotic drug treatment. Schizophr Res 88(1–3):265–274
Dejager L, Pinheiro I, Dejonckheere E, Libert C (2011) Cecal ligation and puncture: the gold standard model for polymicrobial sepsis? Trends Microbiol 19(4):198–208
Demling RH, Wong C, Fox R, Hechtman H, Huval W (1985) Relationship of increased lung serotonin levels to endotoxin-induced pulmonary hypertension in sheep. Effect of a serotonin antagonist. Am Rev Respir Dis 132(6):1257–1261
Dupont LL, Bracke KR, De Maeyer JH, Compan V, Joos GF, Lefebvre RA et al (2014) Investigation of 5-HT 4 receptors in bronchial hyperresponsiveness in cigarette smoke-exposed mice. Pulm Pharmacol Ther 28(1):60–67
El Nehir S, Karakaya S (2004) Radical scavenging and iron-chelating activities of some greens used as traditional dishes in Mediterranean diet. Int J Food Sci Nutr 55(1):67–74
Eskandari MK, Bolgos G, Miller C, Nguyen DT, DeForge LE, Remick DG (1992) Anti-tumor necrosis factor antibody therapy fails to prevent lethality after cecal ligation and puncture or endotoxemia. J Immunol 148(9):2724–2730
Evans GF, Snyder YM, Butler LD, Zuckerman SH (1989) Differential expression of interleukin-1 and tumor necrosis factor in murine septic shock models. Circ Shock 29(4):279–290
Hernekamp JF, Hu S, Schmidt K, Walther A, Kneser U, Kremer T (2013) Cinanserin reduces plasma extravasation after burn plasma transfer in rats. Burns J Int Soc Burn Inj 39(6):1226–1233
Kang Q, Chen Y, Zhang X, Yu G, Wan X, Wang J et al (2015) Heat shock protein A12B protects against sepsis-induced impairment in vascular endothelial permeability. J Surg Res 202(1):87–94
Kürkçü E (2008) Deneysel olarak oluşturulmuş meme tümörlerinde curcumin’in arginaz enzim aktivitesi, ornitin ve nitrik oksit düzeylerine etkisi
Kuşcuoğlu U (2004) Deneysel omurilik yaralanmasında agmatin’in doza bağlı nöroprotektif etkilerinin incelenmesi. İstanbul
Kuyumcu A, Düzgün AP, Özmen MM, Besler HT (2004) Travma ve enfeksiyonda nitrik oksidin rolü. Turk J Trauma Emerg Surg 10(3):149–159
Leon-Ponte M, Ahern GP, O’Connell PJ (2007) Serotonin provides an accessory signal to enhance T-cell activation by signaling through the 5-HT7 receptor. Blood 109(8):3139–3146
Leopoldo M, Lacivita E, Berardi F, Perrone R, Hedlund PB (2011) Serotonin 5-HT7 receptor agents: structure-activity relationships and potential therapeutic applications in central nervous system disorders. Pharmacol Ther 129(2):120–148
Lepoivre M, Fieschi F, Coves J, Thelander L, Fontecave M (1991) Inactivation of ribonucleotide reductase by nitric oxide. Biochem Biophys Res Commun 179(1):442–448
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(-delta delta C(T)) method. Methods 25(4):402–408
Livermore S, Zhou Y, Pan J, Yeger H, Nurse CA, Cutz E (2015) Pulmonary neuroepithelial bodies are polymodal airway sensors: evidence for CO2/H+ sensing. Am J Physiol Lung Cell Mol Physiol 308(8):L807–L815
Maleki-Dizaji N, Eteraf-Oskouei T, Fakhrjou A, Maljaie SH, Garjani A (2010) The effects of 5HT3 receptor antagonist granisetron on inflammatory parameters and angiogenesis in the air-pouch model of inflammation. Int Immunopharmacol 10(9):1010–1016
Mossner R, Lesch KP (1998) Role of serotonin in the immune system and in neuroimmune interactions. Brain Behav Immun 12(4):249–271
Nilsson T, Longmore J, Shaw D, Pantev E, Bard JA, Branchek T et al (1999) Characterisation of 5-HT receptors in human coronary arteries by molecular and pharmacological techniques. Eur J Pharmacol 372(1):49–56
Nishiyama T (2009) Acute effects of sarpogrelate, a 5-HT2A receptor antagonist on cytokine production in endotoxin shock model of rats. Eur J Pharmacol 614(1–3):122–127
Özkan C, Akgül Y (2010) Deneysel Nefrotoksisite Oluşturulan Tavşanlarda Nitrik Oksit Donörü (L-Arginin) ve Nitrik Oksit Sentaz İnhibitörlerinin (Aminoguanidin, L-NAME) Bazı Biyokimyasal Parametrelere Etkileri. Yüzüncü Yıl Üniversitesi Veteriner Fakültesi Dergisi 21(1):35–41
Reinhart K, Daniels R, Kissoon N, O’Brien J, Machado FR, Jimenez E (2013) The burden of sepsis-a call to action in support of World Sepsis Day 2013. J Crit Care 28(4):526–528
Ruggieri AJ, Levy RJ, Deutschman CS (2010) Mitochondrial dysfunction and resuscitation in sepsis. Crit Care Clin 26(3):567–575
Schabbauer G (2012) Polymicrobial sepsis models: CLP versus CASP. Drug Discov Today Dis Models 9(1):e17–e21
Segura P, Vargas M, Córdoba-Rodríguez G, Chávez J, Arreola J, Campos-Bedolla P et al (2010) Role of 5-HT2A, 5-HT4 and 5-HT7 receptors in the antigen-induced airway hyperresponsiveness in guinea-pigs. Clin Exp Allergy 40(2):327–338
Shishodia S, Aggarwal BB (2004) Nuclear factor-κB: a friend or a foe in cancer? Biochem Pharmacol 68(6):1071–1080
Tizard IR (2004) Veterinary immunology: an introduction, 7th edn. Saunders, Readfield, pp 293–299
Tosi MF (2005) Innate immune responses to infection. J Allergy Clin Immunol 116(2):241–249
Türköz YÖE (1997) Nitrik oksit’in etkileri ve patolojik rolleri
Ullmer C, Schmuck K, Kalkman HO, Lubbert H (1995) Expression of serotonin receptor mRNAs in blood vessels. FEBS Lett 370(3):215–221
Waddick KG, Uckun FM (1999) Innovative treatment programs against cancer: II. Nuclear factor-kappaB (NF-kappaB) as a molecular target. Biochem Pharmacol 57(1):9–17
Yang GB, Qiu CL, Zhao H, Liu Q, Shao Y (2006) Expression of mRNA for multiple serotonin (5-HT) receptor types/subtypes by the peripheral blood mononuclear cells of rhesus macaques. J Neuroimmunol 178(1–2):24–29
Acknowledgments
This study was supported by the TUBITAK 1001 project (TUBITAK-112S627) and was conducted in the pharmacology of the Faculty of Medicine at Ataturk University, 25240 Erzurum/Turkey. This study is a part of Master thesis of Gulsen AYAZ.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None of the authors has a commercial interest, financial interest, and/or other relationship with manufacturers of pharmaceuticals, laboratory supplies, and/or medical devices or with commercial providers of medically related services.
Rights and permissions
About this article
Cite this article
Ayaz, G., Halici, Z., Albayrak, A. et al. Evaluation of 5-HT7 Receptor Trafficking on In Vivo and In Vitro Model of Lipopolysaccharide (LPS)-Induced Inflammatory Cell Injury in Rats and LPS-Treated A549 Cells. Biochem Genet 55, 34–47 (2017). https://doi.org/10.1007/s10528-016-9769-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10528-016-9769-2