Abstract
There is growing attention focused on local estrogen production in the breast tissue and its possible role in breast cancer initiation and progression. Understanding the underlying mechanisms for estrogen synthesis and the microenvironment consisting of tumor and its surrounding adipose tissue might open new avenues in breast cancer prevention, prognosis and treatment. In order to obtain insight, we compared peritumoral and tumor tissue expressions of CYP17A1 and CYP19A1 genes, which play an important role in estrogen biosynthesis. The paired tissue samples of 20 postmenopausal ER+/PR+ patients diagnosed with invasive ductal breast cancer were studied. In addition, 12 breast tissue samples obtained from premenopausal women without a history of breast cancer were also investigated as representative of normal conditions. Peritumoral adipose tissues expressed CYP19A1 approximately threefold higher than tumor itself (p = 0.001). A nonsignificant trend toward low expression of CYP17A1 was observed in peritumoral compared to tumor tissue (p = 0.687). Clinicopathological parameters and patient characteristics which are accepted as risk factors for breast cancer were also associated with individual and combined expressions of CYP17A1 and CYP19A1. This study offers that evaluation of CYP17A1 and CYP19A1 local expression levels might be useful for deciding on personalized treatment approaches and more accurate diagnosis, when evaluated together with several clinicopathological and disease risk factors. Considering the key role of these CYPs in estrogen synthesis, determining their expression levels may be useful as a postdiagnostic marker and for choosing the right treatment method in addition to the conventional approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancers are often hormonally driven and estrogen receptor positive (ER+). Approximately 70–80 % of all newly diagnosed breast cancers are positive for the estrogen receptor and also positive for progesterone receptor to a certain extent (Hammond et al. 2010). However, there is no decrease in breast cancer risk at menopause while circulating levels of ovarian estrogens are dramatically dropping (Walker and Martin 2007). One of the possible causes of the situation is the locally synthesized estrogens which act as a significant intracrine and paracrine factor (rather than a circulatory hormone) in postmenopausal women, especially in their breasts (Simpson et al. 2005). Estradiol and, to a lesser degree, other estrogens increase proliferation of breast epithelium and stroma and consequently increase the possibility of new mutations occurring in proliferating epithelium (Pattarozzi et al. 2008; Henderson and Feigelson 2000). Those effects also accumulate with continuous exposure to estrogens (Pike et al. 1993, Clemons and Goss 2001). Importance of this accumulated exposure is intensified by the increase in breast cancer risk with young age at menarche (<12 years), older age at first birth (>30 years), null parity, and older age of menopause (>45 years).
Genes encoding enzymes involved in estrogen synthesis and metabolism are attractive research subjects for cracking the underlying mechanism of ER+-driven breast cancers. Aromatase (encoded by CYP19A1) and cytochrome P450C17 (encoded by CYP17A1) are two of the key enzymes involved in estrogen biosynthesis. Aromatase expression and activity were shown to be enhanced in various cancers, including breast tumors, hepatocellular carcinoma, adrenocortical tumors, and testicular tumors (Bulun and Simpson 2008; Jongen et al. 2006; Carruba 2009; Bulun et al. 1997; Young et al. 1996; Aiginger et al. 1981). Paracrine interactions among malignant breast epithelial cells, proximal immature adipocytes, and vascular endothelial cells are responsible for estrogen biosynthesis and the absence of adipogenic differentiation in breast cancer tissue. It is most likely that malignant epithelial cells are the ones that secrete factors, which inhibit the differentiation of surrounding immature adipocytes for their maturation and stimulate aromatase expression in these undifferentiated immature adipocytes (Meng et al. 2001). The in vivo presence of malignant epithelial cells also enhances aromatase gene expression in endothelial cells in breast tissue (Zhou et al. 2001). Following the cessation of ovarian function during/after menopause or medical intervention that reduces or eliminates ovarian function, peripheral estrogen synthesis via aromatase activity becomes the primary source of estrogen production in women. In addition to aromatase, cytochrome P450C17 activity is also at a critical point crossing the pathways of steroid hormone biosynthesis and has been demonstrated in breast cancer tissues more than three decades ago (Abul-Hajj et al. 1979). So far, research conducted on CYP17A1 and breast cancer risk produced controversial results (Feigelson et al. 1997; Chen et al. 2008; Helzlsouer et al. 1998; Setiawan et al. 2007). Although the ethnic variations possibly explain some of the discrepancy between study results, there is still evidence indicating that some of the polymorphic variants of this gene may influence endogenous hormone levels via altering gene expression resulting in increased enzyme activity which then leads to increased amounts of bioavailable estrogen (Haiman et al. 1999).
In this study, several issues regarding local estrogen synthesis in breast cancer were investigated. To evaluate the potential contribution of local CYP17A1 and CYP19A1 expressions to local estrogen synthesis, mRNA levels were determined in intratumoral breast tissue (T) and were compared to those in non-tumor cell bearing peritumoral breast tissue (P) of the same breast among postmenopausal patients harboring ER+/PR+ (estrogen and progesterone receptor positive) invasive ductal breast cancer. The results were correlated with individual parameters (clinicopathological characteristics, breast cancer risk factors) in order to investigate possible patterns which might effect the alteration in expression levels.
Next, to address potential difference in local estrogen synthesis between normal conditions (premenopausal with no history of breast cancer and in child-bearing period where major estrogen drive is still from the overs) and presence of a breast tumor, non-tumor bearing peritumoral breast tissue (P) mRNA levels were compared with normal breast tissue (N) mRNA levels from premenopausal women who underwent mammoplasty reduction surgery. Few studies have been conducted considering normal breast tissue estrogen levels (Vermeulen et al. 1986; Reed et al. 1991; Blankenstein et al. 1999), yet, to our knowledge, this is the first study reporting the CYP17A1 and CYP19A1 expression patterns via comparing peritumoral tissue versus normal breast tissue.
Finally, whether the combination of CYP17A1 and CYP19A1 expression levels in favor of estrogen synthesis in peritumoral tissue differ from intratumoral expression levels in patients were investigated. An affirmative result could be consistent with the hypothesis that peritumoral immature adipose cells promote hormone-sensitive tumor development via locally increased estrogen production, in a paracrine manner. An improved understanding of the relationship between intratumoral expression levels versus peritumoral (adjacent) breast tissue expression levels may provide an important information to uncover the underlying mechanisms, which could then assist in breast cancer prevention, prognosis, and treatment (Yaghjyan and Colditz 2011).
Materials and Methods
Patient Selection
Tumor and its neighboring normal adipose tissues (>200 mg) were obtained from 20 female patients who did not receive adjuvant chemotherapy before surgery and underwent mastectomy or breast-conserving surgery due to invasive ductal breast cancer at the department of Surgery in Cerrahpasa Medical School of Istanbul University during the period of January 2010–December 2012. Their mean age was 59 years (range 46–87 years). Surgically removed tissues were subjected to pathological examination to diagnose and confirm the correct sampling of tumor and adipose tissue at the pathology department of Cerrahpasa Medical Faculty, Istanbul University. One tumor (T) and one adjacent mammary adipose tissue sample (P) were obtained from each patient and snap-frozen in liquid nitrogen and kept at −80 °C until use for the extraction of total RNA. All patients were classified as luminal A (ER+/PR+, HER2−) and postmenopausal. Afterward, patients were divided into groups according to clinicopathologic features: positive and negative lymph node status, presence and absence of vascular invasion, high and low proliferative index, and lobular and ductal histopathological subtype. We also classified cases into two subgroups with different expression patterns possible effect of increasing (estrogen increasing expressional pattern: IP) or decreasing (estrogen decreasing expressional pattern: DP) local estrogen production. In addition, 12 tumor-free breast tissue samples (N) were obtained from premenopausal women with no history of breast cancer (age range 20–40 years) who underwent reduction mammoplasty surgery as the control group. None of them had any kind of cancer history (before surgery, breast ultrasonography was performed, and after surgery, specimens from these patients were pathologically clean) and any known metabolic disease. They were accepted to the surgery outpatient clinic with thoracic, upper back, and neck/shoulder pain or severe intertriginous dermatitis and cosmetic problems. This group was selected as controls because throughout our patient collection duration, healthy patients applied to our clinic for breast reduction surgery were ages between 20–40, and due to ethical reasons no healthy older patient was asked for a clinically unnecessary breast biopsy. The Scientific Research Projects Ethical Board of Istanbul University School of Medicine approved the study protocol (no: 2011/1808-804).
Immunohistochemical Analysis of Breast Cancer Samples
Only the tumor cells with distinct nuclear immunostaining for ER and PR were recorded as positive. The ER and PR status of the patients was defined by immunohistochemistry on formalin-fixed, paraffin-embedded sections of clinical specimens as part of routine pathological interpretation. Immunohistochemistry was performed using a rabbit monoclonal antihuman ER antibody (clone SP1; Thermo Scientific, MA, USA) and a polyclonal rabbit antihuman PR antibody (clone 16, Novocastra, Leica Microsystem, Wetzlar, Germany). ER/PR immunohistochemical stainings were evaluated by two pathologists independently. Nuclear staining of >10 % of cells were accepted as positive for ER or PR status. According to chromogen intensity, dark and intense staining of receptors was evaluated as strong intensity; otherwise, it was accepted as weak intensity.
RNA Extraction and cDNA Synthesis
Approximately 100–150 mg of tissue was grinded with liquid nitrogen using a ceramic mortar and pestle. TRIzol® reagent (Invitrogen, Carlsbad, CA, USA) was used in conjunction with the PureLink® RNA Mini Kit (Ambion, Carlsbad CA, USA) to isolate total RNA from samples. A slight modification was made in the manufacturer’s protocol by introduction of an additional centrifugation step before chloroform addition in order to avoid excess fat content of the samples. This improved the RNA yields and decreased RT-PCR interference. RNA concentrations following RNA isolation were determined using NanoDrop 1000 spectrophotometer (Thermo Scientific, Wilmington, DE,. USA). cDNA synthesis from isolated total RNA was performed according to High Capacity RNA-to-cDNA Kit protocol (Applied Biosystems, Carlsbad CA, USA). Total RNA concentration was adjusted to 100 ng/reaction.
Real-Time PCR
qRT-PCR analysis was performed according to protocol of the TaqMan® Gene Expression Assay (Applied Biosystems, Carlsbad CA, USA) kit by using Applied Biosystems® 7500 Real-Time PCR. FAM and MGB fluorophores were attached at the 5′ and 3′ end of each probe, respectively (Table 1). Briefly, 20 μl of total PCR reaction contained: 1 μl of 20× TaqMan® Gene Expression Assay, cDNA, 10 μl of 2× TaqMan® Gene Expression Master Mix, 4 μl of cDNA template, and 2 μl RNase-free water. PCR reaction was conducted as follows: 50 °C (2 min) for UNG incubation, 95 °C (10 min) for polymerase activation, and then 40 cycles at 95 °C (15 s)/60 °C (1 min). TATA binding box protein (TBP) gene was used as the internal control group. The gene expression levels were analyzed with ΔΔCt method (Livak and Schmittgen 2001).
Statistical Analysis
All calculations were performed using SPSS Statistical Program version 21.0 (SPSS Inc. Chicago, IL, USA). The significance of differences in mRNA levels was determined by the Wilcoxon signed-rank (WSR) test or McNemar (MN) test as needed. Moreover, kappa values (κ) were obtained and results were interpreted according to the study previously reported (Landis and Koch 1977). Briefly κ ranges generally from 0 to 1.0 (although negative numbers are possible), where large numbers mean better reliability and values near or less than 0 suggest that the agreement is attributable to chance alone. All reported p values are from two-sided tests, and a value less than 0.05 was considered statistically significant.
Results
A total of 20 breast cancer patients were studied. The primary characteristics of the study population are given in Table 2. The mean age (±SD) of the study group was 59.65 ± 11.94 years. Most patients had disease of histological grade II or higher (17/20, 85.0 %), and stage of the disease is IIa or worse (15/20, 75.0 %). Our study group was homogeneous according to receptor status and disease type, in which all patients were ER+/PR+ positive and diagnosed with invasive ductal carcinoma. Half of the group had lymphatic vascular invasion. Presence of an in situ component, perineural invasion, and Ki67 expression was detected in most of the cases. On the other hand, only few cases presented axilla invasion, necrosis, and calcification. None of the patients had blood vessel invasion. According to indicated risk factors, more than half of the patients were bearing the “low-risk” conditions, except body mass index (BMI), oral contraceptive use, and age at menopause (Table 3 ).
Two different groups were taken into consideration in order to compare the expression profiles. Expression levels in peritumoral (P) tissues were compared to tumor (T) tissues as well as to normal (N) tissues (Table 4). In addition, according to the common findings in literature of how these CYPs’ mRNAs act over local estrogen production in breast, we defined increasing patterns (IP) and decreasing patterns (DP) for local estrogen production in breast tumor and its microenvironment, in order to investigate what they would display in combination (Table 5). Expressional alterations were defined according to a 1.5-fold difference. Cases observed as “no alteration” were evaluated together with the downregulated group due to statistical relevance.
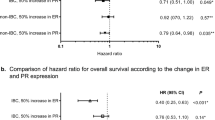
According to tissue types, CYP17A1 expression levels were ordered as N > P > T. CYP19A1 was highly expressed in P compared to both other types. Among all cases, there was a strong upregulation of CYP19A1 and a slight downregulation of CYP17A1 in peritumoral tissue compared to paired tumor tissues (Fig. 1). Approximately, threefold higher CYP19A1 expression levels were observed in peritumoral tissues compared to tumor tissues (Z = −3.397, p = 0.001 [WSR]). However, the downregulation of CYP17A1 was unable to reach statistical significance (Z = −0.402, p = 0.687 [WSR]).
CYP17A1 and CYP19A1 gene expression comparison plot for peritumoral, tumor (a) and peritumoral, normal (b) tissue types. Distribution of peritumoral and tumor tissue CYP17A1 expression levels (1.5 cut off) among patients (c) and fold change difference (*WSR test, two-tailed, not significant) (d). Distribution of peritumoral and tumor tissue CYP19A1 expression levels (1.5 cut off) among patients (e) and fold change difference (*WSR test, two-tailed, significant) (f). Normal breast tissue expression levels were used as controls in calculations
Tables 6 and 7 summarize tissue expression levels (normal and tumor tissue) for different subgroups of patient characteristics. DP and IP conditions in association with patient characteristics are also shown in Table 8.
Effect of Patient Characteristics to Expression Levels in P Compared to T
Patients with early stage and low-grade (grade I) breast cancer tend to have lower levels of CYP17A1 (κ = 0.182, p = 0.039 [MN], κ = 0.035, p = 0.012 [MN]) (Table 6). In all the cases with axilla invasions, high expression levels of CYP19A1 were found (κ = 0.375, p = 0.012 [MN]) (Table 7). Downregulation of CYP17A1 was found to be statistically associated with the absence of in situ component (κ = 0.138, p = 0.002 [MN]). Moreover, we observed DP in most patients together with in situ component presence (κ = 0.239, p = 0.016 [MN]) (Table 8). Patients with weak (≤10 %) PR statuses had low levels of CYP17A1 expression (κ = 0.182, p = 0.039 [MN]). CYP19A1 expression was upregulated in 80 % of the patients who has a family member with a history of any cancer (κ = 0.129, p = 0.039 [MN]). It was found that 75 % of the patients with no history of cancer and who had children after 30 years of age, exhibited upregulated CYP19A1 expression (κ = −0.129, p = 0.013 [MN], κ = 0.053, p = 0.039 [MN]). Early age at menarche was associated with downregulation of CYP19A1 (κ = −0.290, p = 0.021[MN]). Patients with no children tend to have low levels of CYP17A1 (κ = 0.107, p = 0.021[MN]). CYP19A1 expressions appeared to be upregulated in patients who did not use oral contraceptive (κ = −0.048, p = 0.003 [MN]). DP also appeared to be associated with this group of patients (κ = −0.019 p = 0.012 [MN]).
Effect of Patient Characteristics to Expression Levels in P Compared to N
Patients with histological grade I tend to have lower levels of CYP17A1 (κ = −0.016, p = 0.003 [MN]) (Table 6). Association between having early stage breast cancer and low level expression of CYP17A1 were found statistically significant (κ = 0.083, p = 0.012 [MN]). Moreover, in cases with high-grade or high-stage breast cancer, E production seems to be promoted (κ = 0.008, p = 0.006; κ = 0.130, p = 0.021 [MN]) (Table 8). Downregulation of CYP17A1 was found to be statistically associated in all patients with the absence of in situ component (κ = 0.091, p = 0.0005 [MN]). Nevertheless, estrogen production tend to increase in cases with the presence of the in situ component (κ = 0.113 p = 0.001 [MN]). Patients with weak (≤10 %) PR statuses exhibited low levels of CYP17A1 expression (κ = 0.250, p = 0.004). This group of patients was also associated to DP (κ = 0.130, p = 0.021 [MN]). Upregulation of CYP19A1 was observed in 80 % of the patients who has a family member with a history of any cancer (κ = 0.129, p = 0.039 [MN]) (Table 7). All patients with a previous cancer diagnosis, was found to have low levels of CYP19A1 (κ = −0.441, p = 0.049 [MN]). Upregulated CYP19A1 expression was associated with patients who had first-degree relatives with breast cancer (κ = 0.182, p = 0.004 [MN]). CYP17A1 was downregulated in most patients (75 %) with children (κ = −0.129, p = 0.013 [MN]). Multiparity was also found to be associated with IP (κ = −0.102, p = 0.022 [MN]). CYP17A1 and CYP19A1 expressions were found to be low (≥50) in older patients. CYP19A1 expression in patients who did not use oral contraceptives was upregulated (κ = −0.061, p = 0.003 [MN]). Most of the patients (66.7 %) with early onset of menopause (<45) were associated with DP (κ = 0.008, p = 0.006 [MN]).
There was no statistically significant association between factors such as BMI, smoking, alcohol consumption, lymphovascular invasion, perineural invasion, necrosis, calcification, Ki67 and expressional differences neither as individual nor combined (DP and IP) in P, T, or N group (data not shown).
Discussion and Conclusion
Local productions of estrogens in breast as well as the effects of estrogens on progression of breast tumors are attractive areas of research. Although a relationship between local estrogen production and the risk of breast cancer has been identified, an accurate prediction of cancer risk in an individual is not possible at this point. The variation in hormone levels within the different groups of people is yet to be understood. These results suggest that additional mechanisms, i.e., up-/downregulation of other enzymes involved in steroid synthesis pathway may influence intratumoral estrogen levels across individual tumor samples. Composite evaluations of these mechanisms including risk factors such as family and reproductive histories, may lead not only to a more accurate assessment of risk in individual women but also to a better understanding of the role of estrogen in the pathogenesis of breast cancer (Clemons and Goss 2001; Li et al. 2005; Sidoni et al. 2003).
Limited information is available on how these factors are related with gene expression levels, key factors in local estrogen production. To our knowledge, current study provides information for the first time about expression levels of CYP19A1 and CYP17A1 within both tumor and its peritumoral adipose tissues compared to that in healthy breast tissue. The relationship between these expression levels and the breast health risk factors along with clinicopathological parameters to explain the effect of tumor progression were also reported.
Postmenopausal women’s ovaries cease to synthesize estrogens; however, the risk of breast cancer continues to increase with age. The main reason is the continuous estrogen exposure of breast tissues in postmenopausal women (Zhu and Conney 1998). Apparently, the major contribution comes from the adipose tissue. In adipose tissue, aromatase is expressed in the immature adipocytes and fibroblasts which surround the lipid-filled adipocytes, rather than in the adipocytes themselves. These cells utilize circulating androgens as substrates and convert them to estrogens, in particular, estradiol via aromatase (Simpson and Brown 2013). Estrogens can diffuse throughout the adipose tissue of the breast in particular and then enter the breast duct where they stimulate epithelial cell proliferation (Fig. 2).
Principle roles of CYP17A1 and CYP19A1, considering fibroblasts and stromal epithelial interactions for local estrogen production in invasive ductal carcinoma. Locally synthesized estrogens by fibroblasts enter the duct to simulate epithelial proliferation. Malignant breast epithelial cells secrete anti-adipogenic cytokines such as TNF and IL-11 to inhibit differentiation of adipose fibroblasts in order to reside their capacity to express CYP19A1 and form estradiol. Precursors to be aromatized are supplied locally via CYP17A1 activity, particularly in early stages of breast cancer.TNF tissue necrosis factor, IL-11 interleukin 11, PRG progesterone, A androstenedione, TES testosterone, E. estrone, E 2 estradiol
Aromatase expression is almost exclusive to immature adipocytes and adipose tissue related fibroblasts of the breast (Sasano et al. 2009; Geisler 2003). Santen et al. (1997) have shown that stromal cells in breast carcinomas are the major source of estrogens in the tumor. In the current study, CYP19A1 levels in peripheral tissues were nearly three times higher than those in the nearby tumor tissue (p = 0.001 [WSR]), supporting the previous findings. Miyoshi et al. (2003) observed higher CYP17A1 mRNA levels in small tumors (≤2 cm), suggesting that CYP17A1 mRNA upregulation might play some role in the early stage of tumor development. In the current study, most of the patients (75 %) had late onset breast cancer, which may be associated with unaltered CYP17A1 expression in peripheral tissues and slight downregulation in tumors. On the contrary, in peripheral tissues at the early onstage of the disease, when both CYPs were together, they appeared to decrease of local estrogen production via regulating the levels of expression (p = 0.021 [MN]). It was also possible to observe this via histological grade parameter where high-grade tumor tissues were found downregulated (p = 0.012 [MN]), while grade I tumor tissues exhibited higher levels of CYP17A1 expression (p = 0.013 [MN]). Thus, it can be speculated that tumor tissues are more active for estrogen production than peripheral tissues in the early phases of breast cancer and later on production site shifts to peripheral fibroblasts.
The most significant prognostic factor for women with breast cancer is axillary lymph node invasion status (Donegan 1997). Nodal metastases double the risk of distant disease, and the presence or absence of axillary lymph node metastases is also a determining factor for the use of systemic adjuvant chemotherapy (Hortobagyi and Buzdar 1995). Here CYP19A1 in neighboring adipose tissues were highly expressed in all cases with positive axillary invasion (p = 0.012 [MN]), and thus it may be suggested as an additional parameter for such decisions like adjuvant chemotherapy.
The expression levels of ER, PR, and HER2 are used to determine the prognosis and management of breast cancer. In particular, both ER positive and PR positive (rather than only ER positive) tumors may respond better to hormonal therapy. Moreover, the absence of PR expression in primary breast cancer is strongly and independently associated with poor prognosis (Purdie et al. 2014). Association between weak PR and low expression levels of both CYP17A1 and CYP19A1 in tumor tissues that we observed in this study showed that these expression levels could be taken into consideration to identify patients who might benefit from additional adjuvant chemotherapy, extended endocrine therapy, and/or treatments targeting growth factor receptor pathways. Although there are preferred regimens in hormone treatment, such as aromatase inhibitors or ER blockers (Fisher et al. 2005), predicting which treatment could be most beneficial for a particular patient is yet unclear. Evaluating the expressional levels of certain CYPs, due to their key role in estrogen synthesis, may be valuable for selecting the right treatment in addition to the conventional approach.
CYP19A1 upregulation in peripheral tissues is associated with familial incidences of cancer, breast cancer in particular (p = 0.039, p = 0.004 [MN]). Accumulation of different genotypes for different mutations of CYP19A1 may affect expression levels, thus altering aromatase activity and subsequently affecting the endogenous estrogen levels (Surekha et al. 2014; Tüzüner et al. 2010).
Expression patterns of CYP17A1 and CYP19A1 may influence the degree of estrogen exposure on breast epithelial cells. Since the effects of various hormonal risk factors might depend on the expression levels in different tissues, this possible diversity was of interest. Patients bearing “high-risk” factors such as early onset of menstruation, null parity and being older than 50 years produced low levels of CYP19A1 in peritumoral and tumor tissue which was not in agreement with the previous findings (Clemons and Goss 2001). However, late age at pregnancy and the association with upregulation of aromatase expression in peritumoral tissue supported previous results (p = 0.039 [MN]) (Russo et al. 2005; Britt et al. 2007). Pregnancy may have direct effect on immature adipocytes, causing them to differentiate and maturate which can no longer express aromatase. Nevertheless, tumor cells prevent these fibroblasts to become mature adipocytes, and therefore, women who had children after 30 years of age are probably more prone to this effect.
We acknowledge that this study has certain limitations. Regardless of the small number of cases, appropriate analysis was conducted to eliminate this limitation. The main challenge was to collect adequate amount of fresh breast tissue paired as tumor and neighboring adipose tissues, due to the breast-conserving surgery applications. We also excluded the patients who had adjuvant chemotherapy before surgery from the study in order to eliminate the additional effects on the mRNA levels to be observed.
Lifetime exposure to estrogen and other physiological factors, including environmental exposures, could play a critical role in the etiology of breast cancer. Finding effective therapy approaches for cancer is crucial, as is early diagnosis. In conclusion, this study suggests that evaluation of various clinicopathological and disease risk factors along with the expression levels of CYP17A1 and CYP19A1 might help clinicians to decide on treatment strategies and diagnosis for individual cases. However, future studies must be conducted using greater sample size and addition of aromatase and other key enzyme activities evaluations in steroidogenesis pathway which effect local estrogen levels for confirmation and getting more strong and reliable results.
References
Abul-Hajj YJ, Iverson R, Kiang DT (1979) Metabolism of pregnenolone by human breast cancer. Evidence for 17 alpha-hydroxylase and 17,20-lyase. Steroids 34:817–827
Aiginger P, Kolbe H, Kühböck J, Spona J, Geyer G (1981) The endocrinology of testicular germinal cell tumors. Acta Endocrinol (Copenh) 97:419–426
Blankenstein MA, van de Ven J, Maitimu-Smeele I, Donker GH, de Jong PC, Daroszewski J, Szymczak J, Milewicz A, Thijssen JH (1999) Intratumoral levels of estrogens in breast cancer. J Steroid Biochem Mol Biol 69:293–297
Britt K, Ashworth A, Smalley M (2007) Pregnancy and the risk of breast cancer. Endocr Relat Cancer 14:907–933
Bulun SE, Simpson ER (2008) Aromatase expression in women’s cancers. Adv Exp Med Biol 630:112–132
Bulun SE, Noble LS, Takayama K, Michael MD, Agarwal V, Fisher C, Zhao Y, Hinshelwood MM, Ito Y, Simpson ER (1997) Endocrine disorders associated with inappropriately high aromatase expression. J Steroid Biochem Mol Biol 61:133–139
Carruba G (2009) Aromatase in nontumoral and malignant human liver tissues and cells. Ann NY Acad Sci 1155:187–193
Chen Y, Gammon MD, Teitelbaum SL, Britton JA, Terry MB, Shantakumar S, Eng SM, Wang Q, Gurvich I, Neugut AI, Santella RM, Ahsan H (2008) Estrogen-biosynthesis gene CYP17 and its interactions with reproductive, hormonal and lifestyle factors in breast cancer risk: results from the Long Island Breast Cancer Study Project. Carcinogenesis 29:766–777
Clemons M, Goss P (2001) Estrogen and the risk of breast cancer. N Engl J Med 344:276–285
Donegan WL (1997) Tumor-related prognostic factors for breast cancer. CA Cancer J Clin 47:28–51
Feigelson HS, Coetzee GA, Kolonel LN, Ross RK, Henderson BE (1997) A polymorphism in the CYP17 gene increases the risk of breast cancer. Cancer Res 57:1063–1065
Fisher B, Costantino JP, Wickerham DL, Cecchini RS, Cronin WM, Robidoux A, Bevers TB, Kavanah MT, Atkins JN, Margolese RG, Runowicz CD, James JM, Ford LG, Wolmark N (2005) Tamoxifen for the prevention of breast cancer: current status of the National Surgical Adjuvant Breast and Bowel Project P-1 study. J Natl Cancer Inst 97:1652–1662
Geisler J (2003) Breast cancer tissue estrogens and their manipulation with aromatase inhibitors and inactivators. J Steroid Biochem Mol Biol 86:245–253
Haiman CA, Hankinson SE, Spiegelman D, Colditz GA, Willett WC, Speizer FE, Kelsey KT, Hunter DJ (1999) The relationship between a polymorphism in CYP17 with plasma hormone levels and breast cancer. Cancer Res 59:1015–1020
Hammond ME, Hayes DF, Wolff AC, Mangu PB, Temin S (2010) American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Oncol Pract 6:195–197
Helzlsouer KJ, Huang HY, Strickland PT, Hoffman S, Alberg AJ, Comstock GW, Bell DA (1998) Association between CYP17 polymorphisms and the development of breast cancer. Cancer Epidemiol Biomarkers Prev 7:945–949
Henderson BE, Feigelson HS (2000) Hormonal carcinogenesis. Carcinogenesis 21:427–433
Hortobagyi GN, Buzdar AU (1995) Current status of adjuvant systemic therapy for primary breast cancer: progress and controversy. CA Cancer J Clin 45:199–226
Jongen VH, Hollema H, Van Der Zee AG, Heineman MJ (2006) Aromatase in the context of breast and endometrial cancer. A review. Minerva Endocrinol 31:47–60
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Li T, Sun L, Miller N, Nicklee T, Woo J, Hulse-Smith L, Tsao MS, Khokha R, Martin L, Boyd N (2005) The association of measured breast tissue characteristics with mammographic density, other risk factors for breast cancer. Cancer Epidemiol Biomarkers Prev 14:343–349
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods 25:402–408
Meng L, Zhou J, Hironobu S, Suzuki T, Zeitoun K, Bulun SE (2001) TNFalpha and IL-11 secreted by malignant breast epithelial cells inhibit adipocyte differentiation by selectively downregulating C/EBPalpha and PPARgamma: mechanism of desmoplastic reaction. Cancer Res 61:2250–2255
Miyoshi Y, Ando A, Ooka M, Shiba E, Taguchi T, Tamaki Y, Noguchi S (2003) Association of CYP17 genetic polymorphism with intra-tumoral estradiol concentrations but not with CYP17 messenger RNA levels in breast cancer tissue. Cancer Lett 195:81–86
Pattarozzi A, Gatti M, Barbieri F, Würth R, Porcile C, Lunardi G, Ratto A, Favoni R, Bajetto A, Ferrari A, Florio T (2008) 17beta-estradiol promotes breast cancer cell proliferation-inducing stromal cell-derived factor-1-mediated epidermal growth factor receptor transactivation: reversal by gefitinib pretreatment. Mol Pharmacol 73:191–202
Pike MC, Spicer DV, Dahmoush L, Press MF (1993) Estrogens, progestogens, normal breast cell proliferation, and breast cancer risk. Epidemiol Rev 15:17–35
Purdie CA, Quinlan P, Jordan LB, Ashfield A, Ogston S, Dewar JA, Thompson AM (2014) Progesterone receptor expression is an independent prognostic variable in early breast cancer: a population-based study. Br J Cancer 110:565–572
Reed MJ, Aherne GW, Ghilchik MW, Patel S, Chakraborty J (1991) Concentrations of oestrone and 4-hydroxyandrostenedione in malignant and normal breast tissues. Int J Cancer 49:562–565
Russo J, Moral R, Balogh GA, Mailo D, Russo IH (2005) The protective role of pregnancy in breast cancer. Breast Cancer Res 7:131–142
Santen RJ, Santner SJ, Pauley RJ, Tait L, Kaseta J, Demers LM, Hamilton C, Yue W, Wang JP (1997) Estrogen production via the aromatase enzyme in breast carcinoma: which cell type is responsible? J Steroid Biochem Mol Biol 61:267–271
Sasano H, Miki Y, Nagasaki S, Suzuki T (2009) In situ estrogen production and its regulation in human breast carcinoma: from endocrinology to intracrinology. Pathol Int 59:777–789
Setiawan VW, Schumacher FR, Haiman CA, Stram DO, Albanes D, Altshuler D, Berglund G, Buring J, Calle EE, Clavel-Chapelon F, Cox DG, Gaziano JM, Hankinson SE, Hayes RB, Henderson BE, Hirschhorn J, Hoover R, Hunter DJ, Kaaks R, Kolonel LN, Kraft P, Ma J, Le Marchand L, Linseisen J, Lund E, Navarro C, Overvad K, Palli D, Peeters PH, Pike MC, Riboli E, Stampfer MJ, Thun MJ, Travis R, Trichopoulos D, Yeager M, Ziegler RG, Spencer Feigelson H, Chanock SJ (2007) CYP17 genetic variation and risk of breast and prostate cancer from the National Cancer Institute Breast and Prostate Cancer Cohort Consortium (BPC3). Cancer Epidemiol Biomarkers Prev 16:2237–2246
Sidoni A, Cavaliere A, Bellezza G, Scheibel M, Bucciarelli E (2003) Breast cancer in young women: clinicopathological features and biological specificity. Breast 12:247–250
Simpson ER, Brown KA (2013) Obesity and breast cancer: role of inflammation and aromatase. J Mol Endocrinol 51:T51–T59
Simpson ER, Misso M, Hewitt KN, Hill RA, Boon WC, Jones ME, Kovacic A, Zhou J, Clyne CD (2005) Estrogen—the good, the bad, and the unexpected. Endocr Rev 26:322–330
Surekha D, Sailaja K, Rao DN, Padma T, Raghunadharao D et al (2014) Association of CYP19 polymorphisms with breast cancer risk: a case-control study. J Nat Sci Biol Med 5:250–254
Tüzüner BM, Oztürk T, Kisakesen HI, Ilvan S, Zerrin C, Oztürk O, Isbir T (2010) CYP17 (T-34C) and CYP19 (Trp39Arg) polymorphisms and their cooperative effects on breast cancer susceptibility. In Vivo 24:71–74
Vermeulen A, Deslypere JP, Paridaens R, Leclercq G, Roy F, Heuson JC (1986) Aromatase, 17 beta-hydroxysteroid dehydrogenase and intratissular sex hormone concentrations in cancerous and normal glandular breast tissue in postmenopausal women. Eur J Cancer Clin Oncol 22:515–525
Walker RA, Martin CV (2007) The aged breast. J Pathol 211:232–240
Yaghjyan L, Colditz GA (2011) Estrogens in the breast tissue: a systematic review. Cancer Causes Control 22:529–540
Young J, Bulun SE, Agarwal V, Couzinet B, Mendelson CR, Simpson ER, Schaison G (1996) Aromatase expression in a feminizing adrenocortical tumor. J Clin Endocrinol Metab 81:3173–3176
Zhou J, Gurates B, Yang S, Sebastian S, Bulun SE (2001) Malignant breast epithelial cells stimulate aromatase expression via promoter II in human adipose fibroblasts: an epithelial-stromal interaction in breast tumors mediated by C/EBPbeta. Cancer Res 61:2328–2334
Zhu BT, Conney AH (1998) Functional role of estrogen metabolism in target cells: review and perspectives. Carcinogenesis 19:1–27
Funding
This study has been supported by The Scientific Research Projects Coordination Unit of Istanbul Technical University (No 36004).
Author Contributions
This study was designed, directed, and coordinated by Mete Bora Tüzüner and Oğuz Öztürk. Oğuz Öztürk, as the principal investigator, provided conceptual and technical guidance for all aspects of the research. Hakan Bermek suggested and commented on the design of the experiments. Hande Turna contributed to patient selection and data collection. Tülin Öztürk, Şennur İlvan, and Zerrin Calay performed and analyzed immunohistochemistry experiments and also contributed to specimen selection. Allison Pınar Eronat and Fatih Seyhan performed RNA extractions and cDNA constructions from the tissue samples. Mete Bora Tüzüner planned and performed qRT-PCR studies and analyzed the data with Halil İbrahim Kısakesen and Hülya Yılmaz Aydoğan. The manuscript was written by Mete Bora Tüzüner and Oğuz Öztürk and commented on by all authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of this research.
Rights and permissions
About this article
Cite this article
Tüzüner, M.B., Öztürk, T., Eronat, A.P. et al. Evaluation of Local CYP17A1 and CYP19A1 Expression Levels as Prognostic Factors in Postmenopausal Invasive Ductal Breast Cancer Cases. Biochem Genet 54, 784–802 (2016). https://doi.org/10.1007/s10528-016-9756-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10528-016-9756-7