Abstract
Between one to two-thirds of HIV infections among gay, bisexual, and other men who have sex with men are from primary partners, and there has been increased research attention focused on strategies to increase PrEP adoption among male couples. While there is evidence that partner support is a strong correlate of pre-exposure prophylaxis (PrEP) adoption, there has been a lack of attention on PrEP communication dynamics among male couples. In this paper, we build upon this literature through analysis of dyadic data from a large cross-sectional survey of 543 concordant sero-negative and serodiscordant male couples to examine individual and relationship factors associated with reports of partner communication around PrEP, comfort in discussing PrEP, and perceived partner-level support for PrEP use. PrEP use was relatively low (16.2%), and although 87.5% of men reported their partners would support their PrEP use, only 26.3% had talked to their partner recently about PrEP. PrEP communication and perceived support for PrEP were significantly negatively associated with PrEP stigma and stigma based on sexuality (i.e., internalized homophobia and enacted external stigma based on sexuality), while men with sexual agreements were more comfortable talking about PrEP with their partner. There is a need to adapt current interventions, or develop new dyadic interventions, that provide opportunities for male couples to talk and learn about PrEP together, as a potential pathway to engage them toward PrEP use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The HIV epidemic in the United States continues to disproportionately impact gay, bisexual and other men who have sex with men (GBMSM). From 2009 to 2018, new HIV diagnoses among GBMSM remained unchanged, even as new diagnoses among all Americans declined 19% (Centers for Disease Control and Prevention, 2020; Linley et al. 2020). In 2012, agent-based modeling demonstrated the potential for increases in the use of existing prevention strategies—consistent condom use, regular HIV testing, and use of pre-exposure prophylaxis (PrEP)—to reduce new HIV infections among GBMSM by 25% over a 10-year period (Sullivan et al., 2012). However, the adoption of these prevention strategies, particularly PrEP, remains suboptimal, and annual HIV diagnoses have decreased by only 5% among GBMSM. However, the use of PrEP among GBMSM increased by approximately 500% from 6 to 35% between 2014 and 2017, with significant increases in PrEP use observed in all urban areas and in almost all demographic subgroups (Finlayson et al., 2019). The Centers for Disease Control and Prevention (CDC) reports that an estimated 1.25 million individuals in the USA have an indication for PrEP, while fewer than 10% of at-risk persons are currently using PrEP (Smith et al., 2015, 2018).
With the recognition that between one to two-thirds of HIV infections among GBMSM are from primary partners (Goodreau et al., 2012; Sullivan et al., 2009), there has been an increased focus of programmatic and research attention on increasing PrEP adoption among at-risk male couples (Cuervo & Whyte, 2015; Gamarel & Golub, 2020; Mitchell et al., 2016; Mitchell & Stephenson, 2015). Two of CDC’s three PrEP guidelines pertain to those who are in a relationship: (1) being in an ongoing relationship with an HIV-positive partner (i.e., discordant male couple); or (2) in a mutually non-exclusive monogamous relationship with a partner who recently tested HIV-negative. For single GBMSM, the availability of social support has been shown to ameliorate the effect of PrEP stigma on adoption, with young GBMSM with a larger number of other young GBMSM in their social network being more likely to use PrEP (Kuhns et al., 2017). PrEP users are also more likely to know other PrEP users and a larger number of people living with HIV, suggesting that social networks may provide a source of social support for PrEP use and a network to obtain information and share resources (Holt et al., 2019; Khanna et al., 2016; Pulsipher et al., 2016). Flores et al. (2020) demonstrated that for young GBMSM, the quality of communication with parents was associated with an increased likelihood of PrEP use.
Recent studies have extended on this literature to examine how communication and partner-level support may affect PrEP use among male couples. While there is strong evidence that PrEP stigma (including negative stereotypes such as the “PrEP whore” (Spieldenner, 2016)) is a significant barrier to PrEP adoption (Eaton et al., 2017), for male couples, additional forms of stigma may include perceptions that PrEP use undermines the fidelity of their relationship (Mitchell et al., 2016; Quinn et al., 2020; Starks et al., 2019). The effects of stigma on PrEP adoption can be ameliorated through communication and support among couples. Several studies have demonstrated that discussions around PrEP between couples can lead to significant shifts in HIV-related anxiety, congruence on sexual health goals, and help them reflect on their sexual behavior and sexual agreements (when relationship partners have an explicit conversation to decide and mutually understand which sexual and other relational behaviors they want to have with each other and if applicable, with other individuals (e.g., casual sex partners) (Hoff & Beougher, 2010; Mitchell, 2014) (Gamarel & Golub, 2015; Pantalone et al., 2020). For serodiscordant and concordant HIV-seronegative male couples, PrEP adoption may be framed as a pathway to increased intimacy through condomless anal sex (CAS) (Gamarel & Golub, 2015; Hoff et al., 2015). Mimiaga et al. (2014) note that for male couples, perceptions that partners are supportive of PrEP use are associated with increased PrEP adherence. Adopting PrEP has also been shown to increase confidence in having conversations around HIV status and condom use preferences by partner type (Pantalone et al., 2020). However, previous work has also demonstrated that many GBMSM report difficulty communicating about safer sex and PrEP use, and these difficulties may be heightened for substance using men and when men perceive their partner as a casual sex partner (Koblin et al., 2011; Mimiaga et al., 2014).
The prevalence of sexual agreements among male couples is common (58–99%), yet varies on whether data are collected from one or both relationship partners of the relationship (Hoff et al., 2010; Rios-Spicer et al., 2019). Sexual agreements have utility for HIV prevention. In qualitative interviews with 20 male couples in which at least one partner was either using or in the process of initiating PrEP, Malone et al. (2018) found that couples showed increased trust and communication when establishing an open sexual agreement (those that permit sexual behaviors with casual sex partners) and demonstrated high awareness of sexual risks and health practices in the context of PrEP use. Malone et al. suggest that PrEP adoption enabled more open risk communication within couples, leading to sexual agreements designed with safety, and sexual and emotional desires in mind.
While there is strong evidence that partner-level support and communication are critical for PrEP uptake (Pantalone et al., 2020), our understanding of the factors that are associated with communication and perceived support for PrEP use among male couples is lacking. In this paper, we build upon this literature through analysis of dyadic data from a large cross-sectional survey of 543 male couples to examine individual and relationship factors associated with partner-level communication about PrEP and perceived partner-level support for PrEP use. Understanding the characteristics and typologies of couples who are able to communicate and support each other in PrEP use has the potential to inform prevention interventions that teach couples the communication skills toward uptake, use, and support for PrEP in their relationships.
Method
Participants
Project CHAPS (Couples Health and Attitudes toward Pre-exposure Prophylaxis (PrEP)) sought to understand PrEP use dynamics among male couples via a national online survey (conducted between October 2017 and June 2018) with concordant HIV sero-negative and sero-discordant male couples. Participants were recruited from across the U.S. using advertisements on social media websites and dating websites/mobile apps (Facebook, Instagram, Scruff and Grindr). Advertisements included images of a diverse (in age, race, and ethnicity) range of male couples, with text that promoted a study on the health of same-sex male couples (i.e., “Are you and your man on the same page about HIV prevention? We want to know, take our survey!”). The text did not refer to PrEP to reduce selection bias.
Individual-level eligibility was established separately for both partners of the couple, and had to be met by both for enrollment. Individual eligibility included reporting: (1) a cisgender male identity (assigned male at birth and currently identifies as male), (2) being in a relationship with another cisgender male for three or more months, (3) having a HIV seronegative or unknown status or known HIV seropositive status (only one partner per couple was eligible to report being HIV positive), and (4) having had CAS with their primary relationship partner within the prior three months. Upon providing consent, the individual (Partner A) was directed to the partner referral system, in which they entered contact information (email and telephone number) and a name for his partner (Partner B). Partner B then received an email informing him that his partner (Partner A) had signed up for study and had provided his contact information along with a link to a landing page to access the same screener and consent process. The link provided to Partner B was connected to Partner A’s metadata such that their survey responses were both assigned the same randomly generated study ID number as a hidden data field (a couple level ID number). Once both partners were consented, individual emails were sent to each partner asking them to individually complete an online survey via a unique link with their study ID embedded. Each partner was compensated $50; compensation was not dependent on both partners completing the survey. The study protocol was approved by the University of Michigan’s Institutional Review Board (HUM00125711). Further information on the recruitment and verification processes used for enrollment are available in more detail in Stephenson et al. (2020) and Mitchell et al. (2020a, b).
Procedure
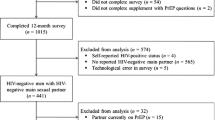
Advertisements on social media generated 221,258 impressions (number of times the advertisements were shown on a social medial page), between October 2017 and January 2018, resulting in 4589 clicks (not necessarily all unique individuals). Of the 4589 clicks, 3826 individuals (83.3%) were assessed for eligibility. Of these, 2740 were either unmatched or ineligible: 1293 (33.8%) were unlinked due to their partner not enrolling into the screening, 48 (2.0%) had incomplete partner data because at least one partner did not finish the survey, 22 (0.9%) were ineligible due to one partner not meeting the eligibility criteria, 492 individuals (12.9%) were fraudulent, and 885 (23.2%) started the screening but did provide any responses, and were therefore were deemed invalid. In total, 1086 individuals, representing 543 complete couples (28.4%), were matched eligible and completed the survey.
Measures
The survey included measures of individual characteristics of age, race, ethnicity, education attainment, employment status, sexual orientation, and self-reported HIV status. Participants were asked if they had heard of PrEP (“PrEP refers to taking a pill called pre-exposure prophylaxis (PrEP)—also called Truvada—everyday to reduce your risk of acquiring HIV”). To better understand potential facilitators and barriers toward PrEP use among at-risk male couples, participants who reported never using PrEP were asked whether they had talked to their partner about PrEP recently (“In the past 3 months have you had a conversation with [name] about one or both of you starting PrEP?): the question was restricted to a 3 month recall period to reduce recall bias. Participants were also asked about their comfort in talking to their partner about PrEP (“How comfortable would you be/were you talking with [name] about starting PrEP?”) (very comfortable, somewhat comfortable, neither comfortable or uncomfortable, somewhat uncomfortable, very uncomfortable), and their perceptions of their partner’s support for PrEP use (“Do you think [name] would support your PrEP use?”) (yes, no, I don’t know).
Relationship characteristics included relationship length, cohabitation, and dyadic variables that were created to describe whether the participants were in an interracial relationship or a HIV sero-discordant relationship. Participants were asked whether they and their partner had a sexual agreement; those who reported having a sexual agreement were asked if the agreement was “closed” (sex with outside partners was not allowed) or “open” (sex with outside partners was allowed with or without restrictions). Participants were asked to report on their level of trust in their partner using the using the 8-item Dyadic Trust scale (Larzelere & Huston, 1980) (sample Chronbach alpha = 0.68), and included items such as “[name] is more interested in his own welfare than your own.” Participants were asked about their communication style with their partner using the 11-item Communication style—Communication Patterns Questionnaire Short Form (CPQSF) (Christensen, 1987, 1988; Christensen & Sullaway, 1984) (sample Cronbach alpha = 0.74), and included items such as “both of us avoid discussing the problem.”
For individual risk behaviors, participants reported sexual behavior in the prior 6 months: their number of sex partners, gender of each partner, the number of anal sex partners and the number of CAS partners, in addition to condom use with their primary partner. Individual experiences of depressive symptomology were measured using the 11-item Iowa short form of the Center for Epidemiologic Studies Depression Scale (CES-D-11) (Carpenter et al., 1998). Given the noted associations between substance use and effective communication around PrEP (Koblin et al., 2011; Mimiaga et al., 2014), participants reported their recent (3 month) use of non-prescription drugs and alcohol using the ASSIST and AUDIT scales (Bush et al., 1998; Saunders et al., 1993; WHO, 2016). Previous studies have demonstrated that men who experience stigma—either external or internal—based on their sexuality, experience lower levels of PrEP uptake (Spieldenner, 2016), and therefore it is plausible that these experience of stigma may also limit the ability and willingness to communicate around PrEP. Two forms of experience of sexuality-based stigma were measured: enacted stigma (Szymanski, 2006) and internalized homophobia (Smolenski et al., 2010). PrEP-related stigma were measured using the 5-item PrEP Stigma scale (Fortenberry et al., 2002).
The willingness to use PrEP, and to talk to a partner about PrEP, may be shaped by an individual’s functional knowledge of HIV prevention. Knowledge of HIV prevention was measured using the 15-item HIV Knowledge scale (Carey & Schroder, 2002) (sample Cronbach alpha = 0.65). Perceptions of individual risk for contracting HIV were measured using 8-item Perceived Risk of HIV scale (Napper et al., 2012) (sample Cronbach alpha = 0.78). Participants were asked to estimate the prevalence of HIV among GBMSM in the US, using a sliding scale from 0–100%. Perceived support from friends for PrEP use was measured using two items: “How many of your gay or bisexual friends are currently using PrEP? and “How many of your gay and bisexual friends would support you using PrEP?”, with response options of “none of them,” “a few of them,” “almost all of them,” and “all of them.”
Statistical Analysis
Analysis considers three outcomes: (a) whether they had talked to their partner about PrEP in the previous 3 months (binary), (b) whether they believe their partner would support their PrEP use (categorical), and (c) comfort in talking to their partner about PrEP (ordinal). Comfort in talking to partners was reversed coded, such that higher values equated to more perceived comfort in talking to partners about PrEP (very uncomfortable, somewhat uncomfortable, neither comfortable or uncomfortable, somewhat comfortable, and very comfortable). Of the 1086 individuals/543 couples, 120 individuals participants had missing data on potential correlates of PrEP outcomes (i.e., substance use, PrEP stigma): resulting in 966 individuals/483 couples. There were no demographic differences (age, education or race/ethnicity) between those with and without missing data. The analysis sample is restricted to those who have never used PrEP, resulting in an analysis sample of 750 individuals/375 couples.
To assess interdependent dyadic associations with PrEP communication and support-related outcomes, the analysis employed an Actor-Partner Independence Model (APIM) approach to simultaneously estimate actor and partner effects on each of the three outcomes (Cook & Kenny, 2005). An actor effect estimates the affect that Partner A’s characteristics has on one of the outcomes for Partner A. A partner effect estimates the affect that Partner B’ characteristics has on one of the outcomes for Partner A, or the affect that Partner A’s characteristics has on one of the outcomes for Partner B (Cook & Kenny, 2005; Napper et al., 2012). Multilevel generalized linear mixed models (MLM) were employed to estimate actor effects of characteristics for all three outcomes, as well as to estimate partner effects of characteristics for all three outcomes. All models accounted for the interdependence of individual participants nested within indistinguishable dyads and included a random intercept for the dyad. Statistical analyses were conducted using STATA v15.
Results
Characteristics of Individuals and Couples in the Sample
The sample of male couples was highly educated, employed fulltime, predominately white, and relatively young: non-Hispanic white (74.7%), between the ages of 25 to 34 (59.8%), college graduates (36.1%) or had graduate degrees (34.9%), and in fulltime employment (81.4%). The sample was predominantly gay identifying (92.1%) (Table 1). The largest proportion of relationship lengths was between 1 and 3 years (33.3%) and more than 5 years (33.2%), and most reported cohabiting with their partner (81.8%). Almost one-in-five reported being in a HIV sero-discordant relationship (17.0%), and 33.3% were in an interracial relationship.
In terms of sexual agreements, 40.5% of participants reported not having a sexual agreement, while 28.3% reported they had an agreement of monogamy and 31.3% reported that they currently had an open sexual agreement with their partner (Table 1). Reported substance use and binge drinking were high. Almost three-quarters of participants reported at least one episode of binge drinking in the past 3 months (73.6%) and 53.4% reported some substance use in the past 3 months (60% of which was marijuana use).
Within couples, partners had high concurrence on several key relationship factors: relationship length (92.0%), cohabitation, HIV status, and inter-racial relationship (all 100% concurrence) (Table 1). Partners reported relatively similar levels of binge drinking and substance use (60.5% and 76.7% concurrence, respectively). However, partners reported widely different levels of number of recent CAS partners (4.7% concurrence), depressive symptomology (13.1% concurrence) and recent experience of sexuality based stigma (internalized homophobia 13.1% and experiences of stigma 8.5% concurrence). In terms of PrEP, 8.2% of couples had both partners who were currently using PrEP, 9.9% of couples had both partners report the same willingness to use PrEP in the future, and 34.9% of couples had both partners report the same perceived ability to adhere to PrEP.
PrEP Use, Partner Communication, and Perceptions of Partner Support for PrEP
The majority (n = 1001 of 1086, 92%) of participants had heard of PrEP. Approximately one-quarter of the sample had ever used PrEP (21.8%) and 16.2% reported currently using PrEP. In terms of future likelihood of PrEP use, 13.9% reported that they were very likely to use PrEP, while 25.9% were likely, 37.4% unlikely and 22.6% very unlikely. Approximately one-quarter of the sample reported that they had talked to their partner about PrEP in the previous 3 months (26.3%), and 52.6% reported feeling very comfortable talking to their partner about PrEP. However, 17.3% reported being somewhat or very uncomfortable talking to their partner about PrEP. The majority of men (87.5%) perceived their partner would support their use of PrEP.
Actor-Partner Effects on PrEP Partner Communication and Perceived Support
Relative to men with only high school education, those with higher levels of education were more likely to report they had talked to their partner about PrEP in the past 3 months. No individual demographic factors were associated with reports of comfort in talking to their partner about PrEP or beliefs that their partner will support PrEP use (Tables 2, 3).
Men’s own and their partner’s reports of recent binge drinking (men beta − 0.137, p value .017: partner beta − 1.432, p value .001) and substance use (men − 0.210, p value .018: partner beta − 1.564, p value < .001) were associated with being less likely to report being comfortable talking to their partner about PrEP. However, men who reported recent binge drinking (aOR 1.64, p value .050) or substance use (aOR 1.95, p value .002) were more likely to report that they had talked to the partner about PrEP in the past 3 months. Similarly, men whose partners reported recent substance use were more likely to report that they had talked to their partner recently about PrEP (aOR 1.34, p value .006) and to perceive that their partner would support their PrEP use (aOR 1.23, p value .002).
Relative to men who had tested for HIV in the past 3 months, men with all other histories of HIV testing were less likely to report that they had talked to their partner about PrEP and that they perceived their partner would support their PrEP use. Men with greater levels of HIV knowledge were significantly less likely to report that they had talked to their partner about PrEP (aOR 0.85, p value .032) and that they perceived their partner would support their PrEP use (aOR 0.78, p value .022), but there were no associations between partners HIV knowledge and any of the outcomes.
Men who reported higher levels of PrEP stigma were less likely to say that they had talked to their partner about PrEP recently (aOR 0.71, p value .002) and that they believed their partner would support their PrEP use (aOR 0.53, p value .002), and were less likely to feel comfortable talking to their partners about PrEP (beta − 0.069, p value < .001). No associations between partner’s reports of PrEP stigma were found for any of the outcomes. Similarly, men who reported higher perceived risk of HIV acquisition were more likely to report that their partner would support their PrEP use (aOR 1.10, p value .00) and that they had talked to their partner about PrEP recently (aOR 1.13, p value < .001), but less likely to report being comfortable talking to their partner about PrEP (beta − 0.017, p value .040).
Men who reported experiencing higher levels of internalized homophobia were significantly less likely to report being comfortable talking to their partner about PrEP (beta 0.027, p value .002). If a participant’s partner reported higher levels of internalized homophobia, he was less likely to report that he had talked to his partner about PrEP in the past 3 months (aOR 0.67, p value .034) and to report that his partner would support his PrEP use (aOR 0.34, p value .023). There were no significant associations between the participant’s or their partner’s reports of enacted sexuality-based stigma and any of the three outcomes.
Men who reported that more of their GBMSM friends were using PrEP were more likely to report talking to their partner recently about PrEP (aOR 1.86, p value .029). However, the participant’s or their partners perceptions of the number of GBMSM friends using PrEP or the number of GBMSM friends who would support PrEP use were not associated with comfort in talking to the partner about PrEP or perceived partner support for PrEP. The only significant association found for the recent experience of depressive symptomology was that men with higher recent symptomology reported decreased odds that their partner would be supportive of their PrEP use (aOR 0.87, p value .006).
The participant’s number of outside condomless anal sex (CAS) partners was not associated with talking with their partner about PrEP, however it was significantly associated with increased comfort in talking about PrEP (beta 0.062, p value < .001). The partners’ report of the number of CAS partners was associated with an likelihood of talking to the partner recently about PrEP (aOR 1.76, p value .034), and perceived support for PrEP (aOR 2.67, p value .034). Men in sero-discordant relationships were more likely to have talked to their partners recently about PrEP (aOR 1.81, p value .040), to perceive their partner would support their PrEP use (aOR 2.41, p value < .001), but had lower comfort in talking to their partners about PrEP (beta − 0.157, p value .001). Relative to men in relationships in which there was no sexual agreement, men in relationships that were monogamous (aOR 6.02, p value < .001) or open (aOR 2.41, p value < .001) were more likely to have talked to their partner recently about PrEP, were more comfortable in talking about PrEP (monogamy beta 0.824, p value < .001: open beta 0.229, p value .026), and perceived their partner supported their PrEP use (monogamy aOR 9.05, p value .000: open aOR 1.02 p value .038).
Discussion
Partnered men in this online recruited sample of US male concordant seronegative and serodiscordant couples reported relatively low levels of current PrEP use, while simultaneously reporting high levels of HIV-related risks, including high levels of binge drinking, substance use and CAS partners. Men overwhelmingly reported that their partner would support their PrEP use, yet only one-quarter of men reported that they had talked to their partner about PrEP. It is possible that couples may have discussed PrEP in their relationship more than 3 months ago or this finding may indicate that PrEP may remain an abstract notion in couples’ relationships that they may not have considered as a viable prevention strategy or at least communicated about it. Educational status was the only significant demographic correlate of PrEP communication (perhaps driven by greater awareness and access to resources with education), indicating that PrEP communication and support dynamics are primarily driven by risk and relationship characteristics.
The results demonstrate the central role of stigma in shaping men’s ability to communicate and support their partner in PrEP use. Both PrEP stigma and internalized homonegativity were negatively associated with reported comfort in communicating about PrEP and perceptions that their partner would support their PrEP use. Both of these forms of stigma are derived from negative stereotypes around PrEP use (i.e., binaries of clean versus unclean behavior) (Spieldenner, 2016) and same-sex attraction, and the internalized senses of shame and embarrassment that these produce may limit couples ability to talk about PrEP. Similarly, men reporting depressive symptomology—which may be linked to experiences of stigma—reported decreased perceptions that their partner would support their PrEP use. While several interventions exist that allow couples to test for HIV and develop HIV prevention plans together (e.g., Bazzi et al., 2016; Stephenson et al., 2017), it is critical that current and future interventions offer male couples with opportunities to address and talk about stigma, as well as hone in on communicate skills to mitigate these types of potential barriers to HIV prevention.
Substance use, binge drinking and perception of risk for HIV were all associated with an increase in perceived partner support for PrEP and having recently talked about PrEP with their partner but were also associated with decreased comfort in talking about PrEP. Serodiscordant couples were more likely to have talked about PrEP and perceive their partner to be supportive toward PrEP use, but also felt less comfortable talking about PrEP. It is possible that the conversations that couples did have about PrEP were difficult and uncomfortable, reducing their willingness to have further discussions about PrEP. Or it may be that the discussions they had around PrEP did not go well, reducing their willingness to have further PrEP discussions with their partner. These possibilities, again, highlight the need for skills-based interventions—particularly for serodiscordant relationships and those with risk-related behaviors—to provide couples with a space and the skills to communicate effectively and comfortably about PrEP.
However, men with more CAS casual sex partners and those with sexual agreements were more likely to have talked to their partners about PrEP and reported greater comfort talking to their partners about PrEP. Previous work has shown that couples who are able to communicate about sexual behavior and HIV prevention—including PrEP—often create sexual agreements that are designed with safety, and sexual and emotional desires in mind (Malone et al., 2018). Similar results were demonstrated by Kahle et al. (2020) who reported that partnered men with sexual agreements were more likely to perceive that their partner supported PrEP use. For couples who are able to communicate effectively enough to create sexual agreements, these skills may translate into an increased ability for them to talk about PrEP. Also, it is equally possible that discussions about PrEP may be part of couples’ conversations about their sexual agreement.
Men who had not recently tested for HIV were less likely to have talked to their partners about PrEP and to perceive their partner would support PrEP use. It is possible that routine engagement in HIV testing provides men with knowledge about HIV prevention options that they can discuss with their partners, or conversely, that discussions around PrEP and HIV prevention lead men to engage in HIV testing. Previous work demonstrates that partnered GBMSM perceive themselves to be at lower risk of HIV and test less frequently for HIV than single men (Mitchell & Petroll, 2012; Stephenson et al., 2015). Reframing public health messaging of the need for HIV testing, which focuses largely on single men with risks of casual sex, to include couples is a necessary step in increasing engagement in HIV prevention among male couples.
The results also corroborate those of previous studies that demonstrate the role of peer support in increasing PrEP among single GBMSM (Holt et al., 2019; Khanna et al., 2016; Pulsipher et al., 2016). For male couples, networks of friends and other couples who are also using PrEP may provide opportunities for sharing information, access to resources, and emotional support to deal with side-effects or experiences of stigma. Peer support interventions have currently focused on single GBMSM (Patel et al., 2018; Young et al., 2018), and should also be considered as a focus of intervention for male couples.
There are several important limitations to the current analysis. As noted, the sample is largely white, educated and gay-identifying, limiting generalization to all GBMSM. The sample was recruited online, and is limited to those with internet access and social media presence, and chose to consent and participate in the study. Recent work has demonstrated that online samples are demographically and behaviorally comparable to those recruited through venue-based sampling (Hernandez-Romieu et al., 2014). The cross-sectional study design precludes identifying causality, and longitudinal studies are clearly needed with male couples to disentangle the nature of several of the associations identified. A 3 month recall period was used to measure whether men had talked to their partner about PrEP: it is possible that men has talked to their partner about PrEP more than 3 months ago—especially given the longer relationship durations of couples in the sample—and thus the prevalence of PrEP communication is under-estimated. Questions on PrEP communication were asked only of men who had never used PrEP: there is a need to also examine PrEP communication among PrEP users and those who may have discontinued use.
Conclusion
While the results presented here may be limited by the lack of racial, ethnic and economic diversity in the sample—and should be explored further with more diverse samples—they do highlight several new aspects of PrEP communication among male couples. In this sample, PrEP communication was characterized by high levels of perceived support for PrEP but low frequency of recent conversations between partners around PrEP. Men often reported that conversations around PrEP would be uncomfortable. These results, combined with the negative associations between PrEP and sexuality-based internal stigma and PrEP communication, demonstrate a need for interventions that aim to provide a space for couples to learn about and talk about PrEP together. Couples HIV Counseling and Testing (CHTC) in which couples test for HIV and develop a HIV prevention or care plan together, remains the only dyadic HIV prevention option (Stephenson et al., 2017; Sullivan et al., 2014), (although others are in development) (Gamarel et al., 2019; Macapagal et al., 2019; Mitchell et al., 2020a, b) and there is a need ensure that the content is expanded to facilitate dyadic conversations around PrEP but to also continue to develop and test skills-based interventions as a pathway to engaging male couples in PrEP use.
References
Bazzi, A. R., Fergus, K. B., Stephenson, R., Finneran, C. A., Coffey-Esquivel, J., Hidalgo, M. A., Hoehnle, S., Sullivan, P. S., Garofalo, R., & Mimiaga, M. J. (2016). A dyadic behavioral intervention to optimize same sex male couples’ engagement across the HIV care continuum: Development of and protocol for an innovative couples-based approach (partner steps). JMIR Research Protocols, 5(3), e168. https://doi.org/10.2196/resprot.6271
Bush, K., Kivlahan, D. R., McDonell, M. B., Fihn, S. D., & Bradley, K. A. (1998). The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Archives of Internal Medicine, 158(16), 1789–1795. https://doi.org/10.1001/archinte.158.16.1789
Carey, M. P., & Schroder, K. E. (2002). Development and psychometric evaluation of the brief HIV Knowledge Questionnaire. AIDS Education and Prevention, 14(2), 172–182.
Carpenter, J., Andrykowski, M., Wilson, J., Hall, L., Rayens, M. K., Sachs, B., & Cunningham, L. (1998). Psychometrics for two short forms of the center for epidemiologic studies-depression scale. Issues in Mental Health Nursing, 19(5), 481–494. https://doi.org/10.1080/016128498248917
Centers for Disease Control and Prevention. (2020). Estimated HIV incidence and prevalence in the United States, 2014–2018. HIV Surveillance Supplemental Report 2020;25(No. 1). http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published May 2020. Accessed June 2020.
Christensen, A. (1987). Detection of conflict patterns in couples. In K. Hahlweg & M. J. Goldstein (Eds.), Understanding major mental disorder: The contribution of family interaction research (pp. 250–265). Family Process Press.
Christensen, A. (1988). Dysfunctional interaction patterns in couples. In P. Noller & M. A. Fitzpatrick (Eds.), Perspectives on marital interaction (pp. 31–52). Multilingual Matters.
Christensen, A., & Sullaway, M. (1984). Communication patterns questionnaire. Unpublished manuscript, University of California, Los Angeles.
Cook, W. L., & Kenny, D. A. (2005). The actor-partner interdependence model: A model of bidirectional effects in developmental studies. International Journal of Behavioral Development, 29(2), 101–109. https://doi.org/10.1080/01650250444000405
Cuervo, M., & Whyte, J. (2015). The effect of relationship characteristics on HIV risk behaviors and prevention strategies in young gay and bisexual men. Journal of the Association of Nurses in AIDS Care, 26(4), 399–410. https://doi.org/10.1016/j.jana.2015.03.003
Eaton, L. A., Kalichman, S. C., Price, D., Finneran, S., Allen, A., & Maksut, J. (2017). Stigma and conspiracy beliefs related to Pre-exposure Prophylaxis (PrEP) and interest in using PrEP among black and white men and transgender women who have sex with men. AIDS and Behavior, 21(5), 1236–1246. https://doi.org/10.1007/s10461-017-1690-0
Finlayson, T., Cha, S., Xia, M., Trujillo, L., Denson, D., Prejean, J., Kanny, D., Wejnert, C., Abrego, M., Al-Tayyib, A., Anderson, B., & National HIV Behavioral Surveillance Study Group. (2019). Changes in HIV preexposure prophylaxis awareness and use among men who have sex with men—20 urban areas, 2014 and 2017. MMWR Morbidity and Mortality Weekly Report, 68(27), 597–603. https://doi.org/10.15585/mmwr.mm6827a1
Flores, D. D., Meanley, S. P., Wood, S. M., & Bauermeister, J. A. (2020). Family characteristics in sex communication and social support: implications for emerging adult men who have sex with men’s PrEP engagement. Archives of Sexual Behavior, 49(6), 2145–2153. https://doi.org/10.1007/s10508-020-01648-4
Fortenberry, J. D., McFarlane, M., Bleakley, A., Bull, S., Fishbein, M., Grimley, D. M., Malotte, C. K., & Stoner, B. P. (2002). Relationships of stigma and shame to gonorrhea and HIV screening. American Journal of Public Health, 92(3), 378–381.
Gamarel, K. E., Darbes, L. A., Hightow-Weidman, L., Sullivan, P., & Stephenson, R. (2019). The development and testing of a relationship skills intervention to improve hiv prevention uptake among young gay, bisexual, and other men who have sex with men and their primary partners (We Prevent): Protocol for a randomized controlled trial. JMIR Research Protocols, 8(1), e10370. https://doi.org/10.2196/10370
Gamarel, K. E., & Golub, S. A. (2015). Intimacy motivations and pre-exposure prophylaxis (PrEP) adoption intentions among HIV-negative men who have sex with men (MSM) in romantic relationships. Annals of Behavioral Medicine, 49(2), 177–186. https://doi.org/10.1007/s12160-014-9646-3
Gamarel, K. E., & Golub, S. A. (2020). Sexual goals and perceptions of goal congruence in individuals’ PrEP adoption decisions: A mixed-methods study of gay and bisexual men who are in primary relationships. Annals of Behavioral Medicine, 54(4), 237–248. https://doi.org/10.1093/abm/kaz043
Goodreau, S. M., Carnegie, N. B., Vittinghoff, E., Lama, J. R., Sanchez, J., Grinsztejn, B., Koblin, B. A., Mayer, K. H., & Buchbinder, S. P. (2012). What drives the US and Peruvian HIV epidemics in men who have sex with men (MSM)? PLoS ONE, 7(11), e50522. https://doi.org/10.1371/journal.pone.0050522
Hernandez-Romieu, A. C., Sullivan, P. S., Sanchez, T. H., Kelley, C. F., Peterson, J. L., Del Rio, C., Salazar, L. F., Frew, P. M., & Rosenberg, E. S. (2014). The comparability of men who have sex with men recruited from venue-time-space sampling and facebook: A cohort study. JMIR Research Protocols, 3(3), e37. https://doi.org/10.2196/resprot.3342
Hoff, C. C., & Beougher, S. C. (2010). Sexual agreements among gay male couples. Archives of Sexual Behavior, 39(3), 774–787. https://doi.org/10.1007/s10508-008-9393-2
Hoff, C. C., Beougher, S. C., Chakravarty, D., Darbes, L. A., & Neilands, T. B. (2010). Relationship characteristics and motivations behind agreements among gay male couples: Differences by agreement type and couple serostatus. AIDS Care, 22(7), 827–835. https://doi.org/10.1080/09540120903443384
Hoff, C. C., Chakravarty, D., Bircher, A. E., Campbell, C. K., Grisham, K., Neilands, T. B., Wilson, P. A., & Dworkin, S. (2015). Attitudes towards PrEP and anticipated condom use among concordant HIV-negative and HIV-discordant male couples. AIDS Patient Care and STDs, 29(7), 408–417. https://doi.org/10.1089/apc.2014.0315
Holt, M., Lea, T., Bear, B., Halliday, D., Ellard, J., Murphy, D., Kolstee, J., & de Wit, J. (2019). Trends in attitudes to and the use of HIV pre-exposure prophylaxis by Australian gay and bisexual men, 2011–2017: Implications for further implementation from a diffusion of innovations perspective. AIDS and Behavior, 23(7), 1939–1950. https://doi.org/10.1007/s10461-018-2368-y
Kahle, E. M., Sharma, A., Sullivan, S., & Stephenson, R. (2020). The influence of relationship dynamics and sexual agreements on perceived partner support and benefit of PrEP use among same-sex male couples in the U.S. AIDS and Behavior, 24(7), 2169–2177. https://doi.org/10.1007/s10461-020-02782-9
Khanna, A. S., Michaels, S., Skaathun, B., Morgan, E., Green, K., Young, L., & Schneider, J. A. (2016). Preexposure prophylaxis awareness and use in a population-based sample of young black men who have sex with men. JAMA Internal Medicine, 176, 1–136. https://doi.org/10.1001/jamainternmed.2015.6536
Koblin, B. A., Mansergh, G., Frye, V., Van Tieu, H., Hoover, D. R., Bonner, S., Flores, S. A., Hudson, S. M., Colfax, G. N., & Project MIX Study Team. (2011). Condom-use decision making in the context of hypothetical pre-exposure prophylaxis efficacy among substance-using men who have sex with men: Project MIX. Journal of Acquired Immune Deficiency Syndromes, 58(3), 319–327. https://doi.org/10.1097/QAI.0b013e31822b76d2
Kuhns, L. M., Hotton, A. L., Schneider, J., Garofalo, R., & Fujimoto, K. (2017). Use of Pre-exposure Prophylaxis (PrEP) in young men who have sex with men is associated with race, sexual risk behavior and peer network size. AIDS and Behavior, 21(5), 1376–1382. https://doi.org/10.1007/s10461-017-1739-0
Larzelere, R. E., & Huston, T. L. (1980). The dyadic trust scale: Toward understanding interpersonal trust in close relationships. Journal of Marriage and the Family, 42, 595–604.
Linley, L., Johnson, A. S., Song, R., Wu, B., Hu, S., Gant, Z., Green, T.A., Gunnels, B., Hall, H.I., Hernandez, A., & Friend, M. (2020). Estimated HIV incidence and prevalence in the United States, 2014–2018.
Macapagal, K., Feinstein, B. A., Puckett, J. A., & Newcomb, M. E. (2019). Improving young male couples’ sexual and relationship health in the 2GETHER Program: Intervention techniques, environments of care, and societal considerations. Cognitive and Behavioral Practice, 26(2), 254–269. https://doi.org/10.1016/j.cbpra.2018.07.004
Malone, J., Syvertsen, J. L., Johnson, B. E., Mimiaga, M. J., Mayer, K. H., & Bazzi, A. R. (2018). Negotiating sexual safety in the era of biomedical HIV prevention: Relationship dynamics among male couples using pre-exposure prophylaxis. Culture, Health & Sexuality, 20(6), 658–672. https://doi.org/10.1080/13691058.2017.1368711
Mimiaga, M. J., Closson, E. F., Kothary, V., & Mitty, J. A. (2014). Sexual partnerships and considerations for HIV antiretroviral pre-exposure prophylaxis utilization among high-risk substance using men who have sex with men. Archives of Sexual Behavior, 43(1), 99–106. https://doi.org/10.1007/s10508-013-0208-8
Mitchell, J. W. (2014). Characteristics and allowed behaviors of gay male couples’ sexual agreements. Journal of Sex Research, 51(3), 316–328. https://doi.org/10.1080/00224499.2012.727915
Mitchell, J. W., Chavanduka, T. M. D., Sullivan, S., & Stephenson, R. (2020a). Recommendations from a descriptive evaluation to improve screening procedures for web-based studies with couples: Cross-sectional study. JMIR Public Health and Surveillance, 6(2), e15079. https://doi.org/10.2196/15079
Mitchell, J. W., Lee, J.-Y., Woodyatt, C., Bauermeister, J., Sullivan, P., & Stephenson, R. (2016). HIV-negative male couples’ attitudes about pre-exposure prophylaxis (PrEP) and using PrEP with a sexual agreement. AIDS Care, 28(8), 994–999. https://doi.org/10.1080/09540121.2016.1168911
Mitchell, J. W., Lee, J.-Y., Wu, Y., Sullivan, P. S., & Stephenson, R. (2020b). Feasibility and acceptability of an electronic health HIV prevention toolkit intervention with concordant HIV-negative, same-sex male couples on sexual agreement outcomes: Pilot randomized controlled trial. JMIR Formative Research, 4(2), e16807. https://doi.org/10.2196/16807
Mitchell, J. W., & Petroll, A. E. (2012). Patterns of HIV and sexually transmitted infection testing among men who have sex with men couples in the United States. Sexually Transmitted Diseases, 39(11), 871–876. https://doi.org/10.1097/olq.0b013e3182649135
Mitchell, J. W., & Stephenson, R. (2015). HIV-negative partnered men’s willingness to use pre-exposure prophylaxis and associated factors among an internet sample of U.S. HIV-negative and HIV-discordant male couples. LGBT Health, 2(1), 35–40. https://doi.org/10.1089/lgbt.2014.0092
Napper, L. E., Fisher, D. G., & Reynolds, G. L. (2012). Development of the perceived risk of HIV scale. AIDS and Behavior, 16(4), 1075–1083. https://doi.org/10.1007/s10461-011-0003-2
Pantalone, D. W., Holloway, I. W., Goldblatt, A. E. A., Gorman, K. R., Herbitter, C., & Grov, C. (2020). The impact of pre-exposure prophylaxis on sexual communication and sexual behavior of urban gay and bisexual men. Archives of Sexual Behavior, 49(1), 147–160. https://doi.org/10.1007/s10508-019-01478-z
Patel, V. V., Ginsburg, Z., Golub, S. A., Horvath, K. J., Rios, N., Mayer, K. H., Kim, R. S., & Arnsten, J. H. (2018). Empowering with PrEP (E-PrEP), a peer-led social media-based intervention to facilitate HIV preexposure prophylaxis adoption among young Black and Latinx gay and bisexual men: Protocol for a cluster randomized controlled trial. JMIR Research Protocols, 7(8), e11375. https://doi.org/10.2196/11375
Pulsipher, C. A., Montoya, J. A., Plant, A., Curtis, P., Holloway, I., & Leibowitz, A. A. (2016). Addressing PrEP disparities among young gay and bisexual men in California. California HIV/AIDS Research Program. Retrieved March, 12, 2018.
Quinn, K. G., Zarwell, M., John, S. A., Christenson, E., & Walsh, J. L. (2020). Perceptions of PrEP use within primary relationships among young Black gay, bisexual, and other men who have sex with men. Archives of Sexual Behavior, 49(6), 2117–2128. https://doi.org/10.1007/s10508-020-01683-1
Rios-Spicer, R., Darbes, L., Hoff, C., Sullivan, P. S., & Stephenson, R. (2019). Sexual agreements: A scoping review of measurement, prevalence and links to health outcomes. AIDS and Behavior, 23(1), 259–271. https://doi.org/10.1007/s10461-018-2212-4
Saunders, J. B., Aasland, O. G., Babor, T. F., de la Fuente, J. R., & Grant, M. (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on early detection of persons with harmful alcohol consumption—II. Addiction, 88(6), 791–804. https://doi.org/10.1111/j.1360-0443.1993.tb02093.x
Smith, D. K., Van Handel, M., & Grey, J. (2018). Estimates of adults with indications for HIV pre-exposure prophylaxis by jurisdiction, transmission risk group, and race/ethnicity, United States, 2015. Annals of Epidemiology, 28(12), 850-857.e859. https://doi.org/10.1016/j.annepidem.2018.05.003
Smith, D. K., Van Handel, M., Wolitski, R. J., Stryker, J. E., Irene Hall, H., Prejean, J., Koenig, L. J., & Valleroy, L. A. (2015). Vital signs: Estimated percentages and numbers of adults with indications for preexposure prophylaxis to prevent HIV acquisition—United States, 2015. MMWR. Morbidity and Mortality Weekly Report, 64(46), 1291–1295. https://doi.org/10.15585/mmwr.mm6446a4
Smolenski, D. J., Diamond, P. M., Ross, M. W., & Rosser, B. R. S. (2010). Revision, criterion validity, and multigroup assessment of the Reactions to Homosexuality Scale. Journal of Personality Assessment, 92(6), 568–576. https://doi.org/10.1080/00223891.2010.513300
Spieldenner, A. (2016). PrEP whores and HIV prevention: The queer communication of HIV pre-exposure prophylaxis (PrEP). Journal of Homosexuality, 63(12), 1685–1697. https://doi.org/10.1080/00918369.2016.1158012
Starks, T. J., Doyle, K. M., Shalhav, O., John, S. A., & Parsons, J. T. (2019). An examination of gay couples’ motivations to use (or forego) pre-exposure prophylaxis expressed during couples HIV testing and counseling (CHTC) sessions. Prevention Science, 20(1), 157–167. https://doi.org/10.1007/s11121-018-0892-7
Stephenson, R., Chavanduka, T. M. D., Sullivan, S., & Mitchell, J. W. (2020). Correlates of successful enrollment of same-sex male couples into a web-based HIV prevention research study: Cross-sectional study. JMIR Public Health and Surveillance, 6(1), e15078. https://doi.org/10.2196/15078
Stephenson, R., Freeland, R., Sullivan, S. P., Riley, E., Johnson, B. A., Mitchell, J., McFarland, D., & Sullivan, P. S. (2017). Home-based HIV testing and counseling for male couples (Project Nexus): A protocol for a randomized controlled trial. JMIR Research Protocols, 6(5), e101. https://doi.org/10.2196/resprot.7341
Stephenson, R., White, D., Darbes, L., Hoff, C., & Sullivan, P. (2015). HIV testing behaviors and perceptions of risk of HIV infection among MSM with main partners. AIDS and Behavior, 19(3), 553–560. https://doi.org/10.1007/s10461-014-0862-4
Sullivan, P. S., Carballo-Diéguez, A., Coates, T., Goodreau, S. M., McGowan, I., Sanders, E. J., Smith, A., Goswami, P., & Sanchez, J. (2012). Successes and challenges of HIV prevention in men who have sex with men. The Lancet, 380(9839), 388–399. https://doi.org/10.1016/s0140-6736(12)60955-6
Sullivan, P. S., Salazar, L., Buchbinder, S., & Sanchez, T. H. (2009). Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS, 23(9), 1153–1162. https://doi.org/10.1097/QAD.0b013e32832baa34
Sullivan, P. S., White, D., Rosenberg, E. S., Barnes, J., Jones, J., Dasgupta, S., O’Hara, B., Scales, L., Salazar, L. F., Wingood, G., DiClemente, R., & Stephenson, R. (2014). Safety and acceptability of couples HIV testing and counseling for US men who have sex with men. Journal of the International Association of Providers of AIDS Care, 13(2), 135–144. https://doi.org/10.1177/2325957413500534
Szymanski, D. M. (2006). Does internalized heterosexism moderate the link between heterosexist events and lesbians’ psychological distress? Sex Roles, 54(3–4), 227–234. https://doi.org/10.1007/s11199-006-9340-4
WHO. (2016). Global health sector strategy on HIV 2016–2021 (p. 60). World Health Organization.
Young, L. E., Schumm, P., Alon, L., Bouris, A., Ferreira, M., Hill, B., Khanna, A. S., Valente, T. W., & Schneider, J. A. (2018). PrEP Chicago: A randomized controlled peer change agent intervention to promote the adoption of pre-exposure prophylaxis for HIV prevention among young Black men who have sex with men. Clinical Trials, 15(1), 44–52. https://doi.org/10.1177/1740774517730012
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Stephenson, R., Chavanduka, T.M.D., Sullivan, S. et al. Partner Support and Communication for Pre-exposure Prophylaxis (PrEP) Use Among Male Couples. Arch Sex Behav 51, 2549–2562 (2022). https://doi.org/10.1007/s10508-021-02118-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10508-021-02118-1