Abstract
To ensure that public health services provide comprehensive and inclusive health care to the general population, it is important for countries to estimate how many of their citizens experience gender dysphoria and wish to receive specialized hormone treatment or gender-affirming surgery. The aim of this study was to estimate the prevalence of individuals with gender dysphoria seeking transgender health care in a public teaching hospital in southern Brazil. In this retrospective follow-up study, we analyzed the medical records and sociodemographic data of individuals aged > 15 years living in Rio Grande do Sul, Brazil, that enrolled in a specialized program to receive hormone therapy and gender-affirming surgery between 2000 and 2018. This study is the first to attempt estimating the prevalence of gender dysphoria in Rio Grande do Sul; it describes novel data on the clinical profile of individuals with gender dysphoria treated in a public hospital specialized in providing transgender health care. Prevalence estimates were calculated based on statewide annual population data in the study period. Of 934 identified individuals, 776 (601 trans women and 175 trans men) were included in this study. The overall prevalence of individuals with gender dysphoria was 9.3 per 100,000 individuals (95% CI: 8.6 to 9.8). Meanwhile, there were 15 trans women per 100,000 people (95% CI: 14 to 16) and 4.1 trans men per 100,000 people (95% CI: 3.5 to 4.8). There was a progressive increase in the number of people seeking hormone therapy and gender-affirming surgery during the study period. Future research is needed to determine the size of the trans population in other regions of Brazil and to expand the knowledge regarding gender dysphoria to allow for the development of effective public policies for people with gender dysphoria.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Gender dysphoria (American Psychiatric Association [APA], 2013) or gender incongruence (World Health Organization [WHO], 2020) is characterized by distress and psychosocial impairment caused by the incongruence between a person’s gender identity and the sex they were assigned at birth. The planning of epidemiological studies focused on gender dysphoria is challenging due to methodological limitations related to the complex interplay among the various psychosocial, demographic, and clinical factors associated with the condition. Nevertheless, there has been an increase in the number of articles attempting to estimate the prevalence of gender dysphoria in various contexts (e.g., APA, 2013; Goodman et al., 2019; Meier & Labuski, 2013).
Winters and Conway (2011) have estimated that there are more than 15 million trans people in the world. The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) reports a prevalence of gender dysphoria ranging from 5 to 14 per 1000 adult men (0.015–0.014) and 2 to 3 per 1000 adult women (0.002–0.003) (APA, 2013). A meta-analysis with studies carried out in gender identity clinics found an overall gender dysphoria prevalence of 4.6 per 100,000 individuals: 6.8 for trans women and 2.6 for trans men (Arcelus et al., 2015). A Spanish study found a gender dysphoria prevalence of 22.1 trans individuals per 100,000 people (31.2 trans women per 100,000 individuals and 12.9 trans men per 100,000 people), with incidence of gender dysphoria of 2.5 trans individuals per 100,000 people (Becerra-Fernández et al., 2017). Regarding young trans self-identification, in the USA 0.7% aged between 13 and 17 years declared themselves trans (Flores et al., 2017), of 1.3% among high school students in San Francisco (Shields et al., 2013) and 1.2% in New Zealand (Clark et al., 2014).
In Brazil, the prevalence of gender dysphoria remains unknown, despite a recent increase in the demand for specialized assistance. This knowledge gap greatly impairs the ability, of the government to plan and implement realistic healthcare strategies (Lobato et al., 2007; Reisner et al., 2016). Current research efforts in Brazil have focused on understanding the sociodemographic factors, biological markers, quality of life, emotional vulnerabilities, and mental health effects associated with gender dysphoria (Costa et al., 2018; Fontanari et al., 2016; Silva et al., 2016, 2017). Recent changes in diagnostic classifications include a shift from the ICD-10 category “transsexualism” (Becerra-Fernández et al., 2017) to “gender incongruence” in the ICD-11 (WHO, 2020) and from “gender identity disorder” in the DSM-IV-TR (APA, 2000) to “gender dysphoria” in the DSM-5 (APA, 2013). Both the DSM and the ICD provide the diagnostic base for clinical practice for the care of individuals with gender dysphoria. Soll et al. (2017) have described both overlaps and differences between the ICD-10 and the DSM-5, with the latter being more comprehensive and inclusive, just as the ICD-11.
Another aspect concerns the methodology of previous studies with trans and gender dysphoria populations, especially the performance of regional measures over fragmented periods of time, as this makes prior study findings difficult to generalize (Lobato et al., 2007; Soll et al., 2017). As a result, most data regarding people with gender dysphoria come from large urban centers (Bauer & Scheim, 2013; Wiepjes et al., 2018), where most health centers providing specialized care for people with gender dysphoria are located (Reisner et al., 2015).
In 1998, based on the regulations issued by the Federal Council of Medicine of Brazil for specialized health services for transgender individuals, the Transdisciplinary Gender Identity Program (PROTIG) was established in the Hospital de Clínicas de Porto Alegre, a teaching hospital associated with the Federal University of Rio Grande do Sul. Subsequently, the Brazilian Unified Health System incorporated specialized health care activities for trans people that are currently being provided and supervised by the Ministry of Health (Brasil, 2008).
The PROTIG, a pioneering program in Brazil, is located in Rio Grande do Sul, the fifth most populous state in the country, which has a population of approximately 11,329,605 people, of which 1,479,101 live in the capital, Porto Alegre (Brazilian Institute of Geography and Statistics [IBGE], 2013). Considering the above, the aim of this study was to estimate the prevalence of individuals with gender dysphoria with a request for medical interventions in the state of Rio Grande do Sul and to describe the sociodemographic characteristics of the population receiving transgender health services and surgical procedures from 2000 to 2018.
Method
Participants
This retrospective cross-sectional study was approved by the ethics committee of the Hospital de Clínicas de Porto Alegre (approval no. 170639). The medical records of individuals with gender dysphoria enrolled in the PROTIG from January 2000 to December 2018 were reviewed, including those of individuals from different regions of Brazil who moved to Rio Grande do Sul in search of specialized treatment, such as hormone therapy and gender-affirming surgery. The inclusion criteria for participants were the following: having been diagnosed gender dysphoria based on ICD-10 or DSM-5 criteria; having been enrolled in the PROTIG for at least 3 months (with first the consultation taking place between 2000 and 2018), being over 15 years old; and living in Rio Grande do Sul. The medical records of patients who did not receive medical care or whose clinical requirements were not related to gender identity were excluded from the study.
Considering the updates in nomenclature and diagnostic guidelines in both the ICD (WHO, 1992) and the DSM (APA, 2013), all patients included in the prevalence analyses met the diagnostic criteria for “transsexualism” (ICD10-F64), “gender identity disorder in adolescents and adults” (DSM-IV-TR) or “gender dysphoria” (DSM-5).
The PROTIG is one of five public hospital programs specialized in performing surgeries related to gender identity in Brazil. Surgical procedures for trans women include penile inversion vaginoplasty and, starting in 2017, placement of breast implants. Surgical procedures for trans men include mastectomy, hysterectomy, and colpectomy. Referrals to the program are regulated by the Ministry of Health. Once a referral is confirmed, the patient is evaluated by a multidisciplinary team. After being diagnosed with gender dysphoria and completing a 2-year follow-up as part of the PROTIG, the patient becomes a candidate for surgery. According to the hospital's infrastructure and regulatory standards, depending on the availability of the operating room and the surgery team, two surgeries are usually performed each month, one for trans women and one for trans men.
After the first consultation, a follow-up visit is scheduled within three months to reassess gender-affirming surgery candidates’ health conditions. After assessment by a psychiatric team and diagnostic confirmation of gender dysphoria, additional appointments are scheduled with specialists from other teams, such as psychology, endocrinology, social assistance and nursing, urology, gynecology, and others.
To ensure the reliability of the collected data (such as candidates’ sex assigned at birth and city of residence), three trained researchers familiarized with the hospital’s medical record system reviewed all data. Cases were classified either as trans men (female sex assigned at birth) or trans women (male sex assigned at birth).
Statistical Analysis
The sample included trans women and trans men classified by age at the time of their first PROTIG consultation (between 15 and 69 years old). For each age bracket, state-wide population data from 2000 to 2018 were obtained from the Brazilian Institute of Geography and Statistics (IBGE, 2013), agency in charge of the nationwide population census in Brazil, than for census purposes, registers individuals’ home address rather than their birth address.
The average follow-up time was calculated for each participant, expressed in months from the first to the last visit before surgery. Mean and SD describe continuous variables and frequencies, while percentages represent categorical variables. The prevalence of gender dysphoria and 95% confidence intervals (CI 95%) were calculated by dividing the number of cases in the study by the total population of Rio Grande do Sul estimated by the IBGE for each year from 2000 to 2018. Linear regression analysis was performed to calculate the annual increase in the search for gender-affirmation services. All analyses were performed using SPSS.
Results
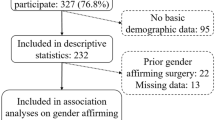
From 2000 to 2018, 934 individuals sought gender-affirmation care from the PROTIG, as shown in Fig. 1. Of these, 776 people met the inclusion criteria: 601 were trans women and 175 were trans men. During this period, there was an increase in the number of people who were able to access the specialized services provided by the PROTIG, as shown in Fig. 2.
Flowchart of the sample. an = 2: intersection between the exclusion criteria “having less than three months in the specialized hospital service” and “less than 15 years”. bn = 7: intersection between the exclusion criteria “less than three months in the specialized hospital service” and “origin outside Rio Grande do Sul”
The mean age of participants at the time of their first consultation was 28.31 years (± SD 9.01), 28.22 years (± SD 8.60) for trans women, and 28.63 years (± SD 10.32) for trans men. Although participants’ place of birth was outside the state for 3.6% (n = 28) of the sample, their home addresses (obtained from the hospital registry) were considered for this study (Table 1).
Rio Grande do Sul total population of individuals aged 15 to 69 years was 8,377,637 in 2018. Therefore, the overall prevalence of trans persons with gender dysphoria (between 2000 and 2018) was 9.3 per 100,000 individuals (95% CI = 8.6 to 9.8) or 1:10,796. The prevalence of trans women was 15 per 100,000 individuals (95% CI = 14 to 16) or 1:6887. The prevalence of trans men was 4.1 per 100,000 individuals (95% CI = 3.5 to 4.8) or 1:24.220. Further, there was an annual increase in the demand for services provided by the PROTIG (B = 0.760; p < 001), as shown in Table 2.
The endocrinology team evaluated 356 participants (249 trans women and 107 trans men) who expressed interest in hormone therapy. For trans women wishing to undergo penile inversion vaginoplasty (n = 203) and breast implant placement (n = 13), the mean wait time to receive the surgery was 37.9 months and 106.6 months, respectively. For trans men wishing to undergo mastectomy (n = 30), hysterectomy (n = 29), and colpectomy (n = 15), the mean wait time was 45.8 months, 65.9 months, and 55.7 months, respectively.
Discussion
By reviewing the cases of individuals treated at our specialized health service between 2000 and 2018, we were able to estimate the prevalence of gender dysphoria among the inhabitants of the southernmost state of Brazil.
Our findings showed that there was a higher demand for specialized hospital services for trans people, compared with prior international studies (e.g., Aitken et al., 2015; Arcelus et al., 2015; Goodman et al., 2019; Reisner et al., 2016; Wiepjes et al., 2018; Zucker, 2017). Further, we observed that more trans women were referred to our service, relative to trans men, in line with prior studies (e.g., Bauer & Scheim, 2013; Goodman et al., 2019). Despite the annual increase in the number of individuals seeking or undergoing gender-affirming therapy, our findings differ from previous estimates; in a systematic review and meta-analysis of studies published from 1968 to 2014, Collin et al. (2016) showed that only six studies estimated the prevalence of transgender individuals seeking or undergoing gender-affirming surgery (9.2/100,000 (95% CI: 4.9 to 13.6). None of the studies included in the aforementioned review were conducted in Latin America, corroborating a recent narrative review including 43 publications from 17 countries (Goodman et al., 2019).
In their review of studies published from 1968 to 2018, Goodman et al. (2019) aimed to calculate the proportion of transgender and gender-non-conforming people. Nine of the reviewed studies included individuals who received or requested treatment for gender affirmation; these studies produced estimates of the prevalence of transgender and gender-non-conforming individuals ranging from 1 to 35/100,000 in the general population. However, data on the population of individuals diagnosed with “transsexualism,” “gender dysphoria,” or “gender identity disorder” were found in 13 studies, ranging from 0.7 to 28 per 100,000 people (0.7 to 36 for those with male sex assigned at birth and 0.7 to 19 for those with female sex assigned at birth). It should be noted that population-based self-report studies usually exhibit even higher prevalence rates. These population numbers often include individuals of diverse genders who do not want medical interventions, but they can also include individuals who have little or no access to specialized care.
Some aspects of our results must be discussed in light of developments in the medical understanding of transsexuality in Brazil. In 1997, after a long debate, the Brazilian Federal Medical Council (Conselho Federal de Medicina, 1997) proposed the first medical care guidelines for gender dysphoria through Resolution 1452. Resolution 1482 asserted that individuals with gender dysphoria must be assisted solely at university hospitals by a transdisciplinary team for at least two years before any surgical procedure can be performed. This guideline covers gender-affirming surgical procedures for both trans women and trans men. From 1997 to 2008, Resolution 1482 remained mostly unchanged, except for extending the possibility for clinical and surgical procedures to be performed at non-university hospitals. Despite official acceptance by the medical council, the vast majority of people in Brazil had little to no knowledge about gender dysphoria, and among those who did, for several years, many were against the idea of providing specialized care for trans people. In the state of Rio Grande do Sul, individuals with gender dysphoria fought a 10-year legal battle before they were able to receive care within the public health system (Brasil, 2013). Thus, not many specialized health services were created during this period, as there was social resistance in recognizing gender dysphoria as a medical condition that deserved insurance coverage. Another factor that negatively influenced the establishment of services aimed at transgender people wishing to undergo gender-affirming surgery in Brazil was the extensive political debate that grew in some organizations regarding the view that gender dysphoria should not be seen as a “pathological condition.” This debate gave surgical services, already overwhelmed by demand, an excuse to deny offering this type of surgery even after its formal inclusion in the public health system.
In its early years, the PROTIG was not well known among the general population. Since there were no referrals from the federal health system from 2000 to 2008, our program focused exclusively on the population from Rio Grande do Sul, while our operational costs were financed by regional health funds. Our first national referral to provide gender dysphoria care (exclusively to trans women) occurred in 2008. Full assistance wasn't granted to both trans women and trans men until 2013 (Fig. 3). This could explain the reduction in the trans men population in our estimates, particularly in 2009, as well as their progressive access to the service over the years, especially after 2012. In addition, the increase in trans men’s access to specialized health care services may not only reflect an increase in the provision of comprehensive care to this population, but could also reflect the increase in this group’s representation in gender clinics (Aitken et al., 2015; Olson et al., 2015; Zucker, 2017). When reviewing and updating the epidemiology of gender dysphoria, Zucker (2017) highlighted that there had been a general increase in gender dysphoria diagnoses over the last two decades, as well as an increase in the proportion of adolescents assigned female at birth who had been diagnosed with gender dysphoria, compared with individuals assigned male at birth.
Compared with other studies (Dhejne et al., 2014; Judge et al., 2014; Proctor et al., 2016), in our study, the average age of the subjects was lower, and was relatively similar between genders. Throughout the study period, the sample’s overall mean age declined yearly. Our results showed that for each passing year, individuals started accessing specialized services at a younger age. One reason for this could be that there is a greater availability of information regarding the existence of specialized service within the public health service, as well as political participation and greater participation of non-governmental organizations. These circumstances may have led more trans people to seek hormone therapy and gender-affirming surgery. In other words, trans people started looking for assistance earlier, compared with other countries (Reisner et al., 2016; Wiepjes et al., 2018; Zucker, 2017). Different authors have highlighted the positive role of globalized information (shared through the internet and the media) on raising awareness of transgender-specific health care services, as it can even reach individuals living in small cities (Flores et al., 2016; Lobato et al., 2007; Zucker, 2017). A cross-sectional study of more than 5000 transgender and gender-diverse youths referred to gender pediatric clinics in the UK and Australia evidenced an association between the increased availability of information regarding transgender and gender-diverse and the search for gender clinics (Pang et al., 2020). The findings of this study contribute to the discussion of social media as a contributing factor in the search for specialized health services for trans people.
Our study revealed that 31.4% of participants reported having completed high school (equivalent to 12 years of schooling). This shows that the education level of PROTIG patients is higher than the statewide average, reported to be 6.8 for individuals over 15 years old and 9.5 for people over 25 years old (IBGE, 2018). Their relatively higher education may have contributed to PROTIG participants seeking treatment at the specialized service. However, this does not necessarily represent the entire trans population, especially if we consider the access and structure of specialized health policies for this group in the Unified Health System (Costa et al., 2018).
Further, we observed racial/ethnic disparities in our sample, with 86.3% of participants identifying themselves as white. According to official sources, 79% of the population in the state are white, 4.6% are black, and 21.3% are pardo (mixed black and white), which refers to Brazilians of mixed race (IBGE, 2019). In Brazil, 46.8% of people identify themselves as pardo, 42.7% as white, and 9.4% as black (based on data from the Permanent National Household Sample Survey) (IBGE, 2019). Our findings suggest that, relative to the overall population, there is a difference in the ethnic/racial characteristics of transgender people with gender dysphoria who access specialized health services. Even though our data were collected from one single specialized health service, the results contribute to estimates of the transgender population with gender dysphoria in public health services in Brazil. In line with previous international studies, we also noted a disparity in the ethnic/racial makeup of individuals accessing specialized services for trans people, whether for hormonal treatment or gender-affirming surgery (Boehmer, 2002; Flores et al., 2016; Proctor et al., 2016; Valentine & Shipherd, 2018). The lack of information in medical records, reduced access to health services, experiences of stigma and discrimination, and the information gap regarding the intersectionality of race/ethnicity in transgender people (Collins, 2000; de Vries, 2015) make it difficult to assess the heterogeneity of this population. This, in turn, affects the development of specialized public health strategies and interventions aimed for transgender people.
Our sample was composed of individuals who declared themselves unmarried (that is, without a stable/fixed affective relationship with a partner) at the time their hospital record was created. The limited number of categories ("single," "married," and "others") defined in the hospital records made it difficult to further discuss any specificities regarding affective relationships/romantic relationships, sexual orientation, sexual behavior, and their impact on transgender social support. It is understood that partners of trans people can provide important social support and assist them in accessing resources aimed for gender affirmation (Ehrbar & Gorton, 2010; Meier & Labuski, 2013). There is undeniably a considerable variability in affective relationships and civil records for both trans and cis people. Meier and Labuski (2013), for example, point out that transgender people can freely have relationships with various types of partners (cis and trans), like all people. Affective relationships are also an important aspect to be considered in demographic surveys for trans people. We understand as a limitation the information gap on sexual orientation in relation to the participants' birth sex, especially to support discussions about sexual attraction (genophilic/androphilic) and immunological mechanisms, already observed in this group (VanderLaan et al., 2017). Therefore, in order to estimate and improve epidemiological data on sexual attraction, affective relationship status and social support, new research topics structured on this objective are oriented.
The number of surgical procedures performed for individuals with gender dysphoria should also be discussed. Various factors could explain the low number of surgical procedures during the study period, including hospital infrastructure (insufficient dedicated beds, adequate operating rooms, and teams of surgeons qualified for gender-affirming surgery). Further, referral criteria tend to be restrictive in the public health service. Usually, only two surgical procedures are performed per month. However, if any institutional or medical team-related difficulties arise, surgeries are postponed until the following month. The placement of breast implants for trans women is performed less frequently than penile inversion vaginoplasty, as breast implant surgeries were not available until 2017. Since then, the placement of breast prosthesis is being carried out according to a waiting order with priority for trans women with more treatment time in the service. Thus, among trans people not yet receiving treatment from the public health service, there is a great demand for gender-affirmative procedures. We do not have information about individuals who receive private medical care (gender-affirming surgery, hormone therapy, or other procedures).
In this study, we identified an increase in the number of individuals seeking specialized health care for gender dysphoria in Rio Grande do Sul, Brazil. We believe that multiple factors are related to the estimates of access of trans people in this service. When comparing the earlier years of the program with the later years, there is an increase in the proportion of trans men who received care. As was already mentioned, this could be due to a series of adaptations and their structuring of public policies for trans health at the national and state level. It is important to continue the formalization of hospital-based medical care protocols, the development of a medical team specialized in hormone therapy and gender-affirming surgery, and to increase the availability of consultations through the Unified Health System in Rio Grande do Sul. The dissemination of information regarding the PROTIG through the media, the larger offer of free consultations, and referrals made by public health services to PROTIG (hospital service) facilitated increased access to the program. Furthermore, the program has served as a training ground for students and health care professionals (including doctors, psychologists, and nurses), aiding in the development of new specialists.
Our findings corroborate that there is an urgent need to expand treatment and surgery services for trans people in hospitals and across the country. In addition, as has been pointed out by previous studies (e.g., Coleman et al., 2012; Reisner et al., 2016; Wiepjes et al., 2018), it is essential to train public health teams from a multidisciplinary perspective. We believe that the collaborative work of personnel from different disciplines (e.g., science, politics, and health services) can contribute to minimizing the social exclusion of trans people, improve the health of minority groups, and could positively contribute to the discussion surrounding hormone therapy and gender-affirming surgery (Coleman et al., 2012; Reisner et al., 2016; Silva et al., 2017; Wiepjes et al., 2018; Zucker, 2017).
In addition, a Brazilian study on the self-reported experience of gender incongruity emphasized the importance of the health conditions of trans people be part of a new chapter on conditions related to sexual health in the ICD-11 manual (Lobato et al., 2019). In Brazil’s current sociopolitical climate (where conservatism and socioeconomic disparity hinder trans people’s access to specialized public health services), the maintenance of gender dysphoria in medical manuals is seen as a guarantee of free access to specialized health services for trans people seeking hormone therapy and gender-affirming surgery (Costa et al., 2015; Lobato et al., 2019).
To the best of our knowledge, this is the first study to estimate the prevalence of trans people with gender dysphoria in Brazil, based on data collected from a public hospital. We should note that some data errors might have resulted from this study’s retrospective design. Not all transgender people with gender dysphoria want to undergo gender-affirming surgery or hormone therapy to affirm their gender identity; therefore, not all trans people seek to this referral service. This is a confounding factor that might have translated into underestimation of gender dysphoria cases in our study (Arcelus et al., 2015; Lobato et al., 2007). Further, we did not take into account individuals who were unable to access our services or who did not seek them; therefore, it would be helpful to also perform future studies with a sample representative of Brazil’s general population. Despite these limitations, we were able to summarize epidemiological data and provide novel information regarding health promotion in Brazil. Additionally, the results provide a snapshot of trans people’s clinical demands. This study also highlights the care provided to individuals with gender dysphoria in Brazil and provides elements for the elaboration of new specialized health strategies.
Conclusion
The present findings show an increase in the number of people with gender dysphoria seeking specialized health services for hormone therapy and gender-affirming surgery. Our study is the first to evaluate gender dysphoria estimates for the population of Brazil and that this analysis originated from data from a regional service in the country. However, due to its limitations concerning the generalization of its findings, we recommend that further studies be developed on this subject. Expanding the sample size of future studies is critical to outlining the health demands of transgender people in Brazil, which could help guide treatment policies and clarify the underlying mechanisms of the underrepresentation of minorities in public hospital services.
References
Aitken, M., Steensma, T. D., Blanchard, R., VanderLaan, D. P., Wood, H., Fuentes, A., Spegg, C., Wasserman, L., Ames, M., Fitzsimmons, C. L., ... Zucker, K. J. (2015). Evidence for an altered sex ratio in clinic-referred adolescents with gender dysphoria. Journal of Sexual Medicine, 12(3), 756–763. https://doi.org/10.1111/jsm.12817
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). American Psychiatric Association.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Press.
Arcelus, J., Bouman, W. P., Van Den Noortgate, W., Claes, L., Witcomb, G., & Fernandez-Aranda, F. (2015). Systematic review and meta-analysis of prevalence studies in transsexualism. European Psychiatry, 30(6), 807–815. https://doi.org/10.1016/j.eurpsy.2015.04.005
Bauer, G. R., & Scheim, A. I. (2013). Sampling bias in transgender studies. The Lancet Infectious Diseases, 13(10), 832. https://doi.org/10.1016/S1473-3099(13)70242-1
Becerra-Fernández, A., Rodríguez-Molina, J. M., Asenjo-Araque, N., Lucio-Pérez, M. J., Cuchí-Alfaro, M., García-Camba, E., Pérez-López, G., Menacho-Román, M., Berrocal-Sertucha, M. C., Ly-Pen, D., & Aguilar-Vilas, M. V. (2017). Prevalence, incidence, and sex ratio of transsexualism in the autonomous region of Madrid (Spain) according to healthcare demand. Archives of Sexual Behavior, 46(5), 1307–1312. https://doi.org/10.1007/s10508-017-0955-z
Boehmer, U. (2002). Twenty years of public health research: Inclusion of lesbian, gay, bisexual, and transgender populations. American Journal of Public Health, 92(7), 1125–1130. https://doi.org/10.2105/ajph.92.7.1125
Brasil. Ministério da Saúde, Diário Oficial da União. (2008). Diretrizes Nacionais para o Processo Transexualizador no Sistema Único de Saúde (Portaria nº 1.707). Retrieved from http://bvsms.saude.gov.br/bvs/saudelegis/gm/2008/prt1707_18_08_2008.html.
Brasil. Ministério da Saúde, Diário Oficial da União. (2013). Redefine e amplia o Processo Transexualizador no Sistema Único de Saúde (Portaria nº 2.803). Retrieved from http://bvsms.saude.gov.br/bvs/saudelegis/gm/2013/prt2803_19_11_2013.html.
Instituto Brasileiro de Geografia e Estatística. (2013). Estimativas da população residente nos municípios brasileiros com data de referência em 1º de julho de 2013. Retrieved from https://www.ibge.gov.br/cidades-e-estados/rs.html.
Instituto Brasileiro de Geografia e Estatística, Diretoria de Pesquisas, Coordenação de Trabalho e Rendimento. (2018). Pesquisa nacional por amostra de domicílios contínua - PNAD contínua: educação 2018. Retrieved from https://biblioteca.ibge.gov.br/visualizacao/livros/liv101657_informativo.pdf.
Instituto Brasileiro de Geografia e Estatística, Diretoria de Pesquisas, Coordenação de Trabalho e Rendimento. (2019). Pesquisa nacional por amostra de domicílios contínua 2012–2019. Retrieved from https://biblioteca.ibge.gov.br/visualizacao/livros/liv101707_informativo.pdf.
Clark, T. C., Lucassen, M. F., Bullen, P., Denny, S. J., Fleming, T. M., Robinson, E. M., & Rossen, F. V. (2014). The health and well-being of transgender high school students: Results from the New Zealand Adolescent Health Survey (Youth’12). Journal of Adolescent Health, 55(1), 93–99. https://doi.org/10.1016/j.jadohealth.2013.11.008
Coleman, E., Bockting, W., Botzer, M., Cohen-Kettenis, P., DeCuypere, G., Feldman, J., Fraser, L., Green, J., Knudson, G., Meyer, W. J., ... Zucker, K. (2012). Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. International Journal Transgenderism, 13(4), 165–232. https://doi.org/10.1080/15532739.2011.700873
Collin, L., Reisner, S. L., Tangpricha, V., & Goodman, M. (2016). Prevalence of transgender depends on the “case” definition: A systematic review. Journal of Sexual Medicine, 13(4), 613–626. https://doi.org/10.1016/j.jsxm.2016.02.001
Collins, P. H. (2000). Black feminist thought: Knowledge, consciousness, and the politics of empowerment. Routledge.
Costa, A. B., da Rosa Filho, H. T., Pase, P. F., Fontanari, A. M., Catelan, R. F., Mueller, A., Cardoso, D., Soll, B., Schwarz, K., Schneider, M. A., & Gagliotti, D. A. (2018). Healthcare needs of and access barriers for Brazilian transgender and gender diverse people. Journal of Immigrant and Minority Health, 20(1), 115–123. https://doi.org/10.1007/s10903-016-0527-7
Costa, A. B., Fontanari, A. M., Jacinto, M. M., da Silva, D. C., Lorencetti, E. K., da Rosa Filho, H. T., Mueller, A., de Garcia, C. G., Nardi, H. C., Koller, S. H., & Lobato, M. I. (2015). Population-based HIV prevalence and associated factors in male-to-female transsexuals from Southern Brazil. Archives of Sexual Behavior, 44(2), 521–524. https://doi.org/10.1007/s10508-014-0386-z
de Vries, K. M. (2015). Transgender people of color at the center: Conceptualizing a new intersectional model. Ethnicities, 15(1), 3–27. https://doi.org/10.1177/1468796814547058
Dhejne, C., Öberg, K., Arver, S., & Landén, M. (2014). An analysis of all applications for sex reassignment surgery in Sweden, 1960–2010: Prevalence, incidence, and regrets. Archives of Sexual Behavior, 43, 1535–1545. https://doi.org/10.1007/s10508-014-0300-8
Conselho Federal de Medicina (CFM). (1997). Dispõe sobre a cirurgia de transgenitalismo (Resolução CFM nº 1.482/97). Retrieved from http://www.portalmedico.org.br/resolucoes/cfm/1997/1482_1997.htm.
Ehrbar, R. D., & Gorton, R. N. (2010). Exploring provider treatment models in interpreting the standards of care. International Journal of Transgenderism, 12, 198–210. https://doi.org/10.1080/15532739.2010.544235
Flores, A. R., Brown, T. N. T., & Herman, J. L. (2016). Race and ethnicity of adults who identify as transgender in the United States. The Williams Institute. Retrieved from https://williamsinstitute.law.ucla.edu/publications/race-ethnicity-trans-adults-us/.
Flores, A. R., Herman, J. L., Brown, T. N. T., Wilson, B. D. M., & Conron, K. J. (2017). Age of individuals who identify as transgender in the United States. The Williams Institute. Retrieved from https://williamsinstitute.law.ucla.edu/publications/age-trans-individuals-us.
Fontanari, A. M., Costa, A. B., Aguiar, B., Tusset, C., Andreazza, T., Schneider, M., da Rosa, E. D., Soll, B. M., Schwarz, K., da Silva, D. C., & Borba, A. O. (2016). Reduced serum concentrations of brain-derived neurotrophic factor (BDNF) in transsexual Brazilian men. Neuroscience Letters, 630, 109–113. https://doi.org/10.1016/j.neulet.2016.07.034
Goodman, M., Adams, N., Corneil, T., Kreukels, B., Motmans, J., & Coleman, E. (2019). Size and distribution of transgender and gender nonconforming populations: A narrative review. Endocrinology and Metabolism Clinics of North America, 48, 303–321. https://doi.org/10.1016/j.ecl.2019.01.001
Judge, C., O’Donovan, C., Callaghan, G., Gaoatswe, G., & O’Shea, D. (2014). Gender dysphoria—Prevalence and co-morbidities in an Irish adult population. Frontiers in Endocrinology, 13(5), 87. https://doi.org/10.3389/fendo.2014.00087
Lobato, M. I., Koff, W. J., Schestatsky, S. S., Chaves, C. P., Petry, A., Crestana, T., Amaral, J. T., Onófrio, F. D., Salvador, J., Silveira, E., & Henriques, A. A. (2007). Clinical characteristics, psychiatric comorbidities and sociodemographic profile of transsexual patients from an outpatient clinic in Brazil. International Journal of Transgenderism, 10, 69–77. https://doi.org/10.1080/15532730802175148
Lobato, M. I., Soll, B. M., Brandelli Costa, A., Saadeh, A., Gagliotti, D. A., Fresán, A., Reed, G., & Robles, R. (2019). Psychological distress among transgender people in Brazil: Frequency, intensity and social causation—An ICD-11 field study. Brazilian Journal of Psychiatry, 41(4), 310–315. https://doi.org/10.1590/1516-4446-2018-0052
Meier, S. C., & Labuski, C. M. (2013). The demographics of the transgender population. In A. K. Baumle (Ed.), International handbook on the demography of sexuality (pp. 289–327). Springer Press.
Olson, J., Schrager, S. M., Belzer, M., Simons, L. K., & Clark, L. F. (2015). Baseline physiologic and psychosocial characteristics of transgender youth seeking care for gender dysphoria. Journal of Adolescent Health, 57(4), 374–380. https://doi.org/10.1016/j.jadohealth.2015.04.027
Pang, K. C., de Graaf, N. M., Chew, D., Hoq, M., Keith, D. R., Carmichael, P., & Steensma, T. D. (2020). Association of media coverage of transgender and gender diverse issues with rates of referral of transgender children and adolescents to specialist gender clinics in the UK and Australia. JAMA Network Open, 3(7), e2011161. https://doi.org/10.1001/jamanetworkopen.2020.11161
Proctor, K., Haffer, S. C., Ewald, E., Hodge, C., & James, C. V. (2016). Identifying the transgender population in the medicare program. Transgender Health, 1(1), 250–265. https://doi.org/10.1089/trgh.2016.0031
Reisner, S. L., Poteat, T., Keatley, J., Cabral, M., Mothopeng, T., Dunham, E., Holland, C. E., Max, R., & Baral, S. D. (2016). Global health burden and needs of transgender populations: A review. Lancet, 388(10042), 412–436. https://doi.org/10.1016/S0140-6736(16)00684-X
Reisner, S. L., Vetters, R., Leclerc, M., Zaslow, S., Wolfrum, S., Shumer, D., & Mimiaga, M. J. (2015). Mental health of transgender youth in care at an adolescent urban community health center: A matched retrospective cohort study. Journal of Adolescent Health, 56(3), 274–279. https://doi.org/10.1016/j.jadohealth.2014.10.264
Shields, J. P., Cohen, R., Glassman, J. R., Whitaker, K., Franks, H., & Bertolini, I. (2013). Estimating population size and demographic characteristics of lesbian, gay, bisexual, and transgender youth in middle school. The Journal of Adolescent Health, 52(2), 248–250. https://doi.org/10.1016/j.jadohealth.2012.06.016
Silva, D. C., Fontanari, A. M., De Garcia, C. C., Costa, A. B., Brambila, M., Schwarz, K., Bridi Filho, C., Schneider, M. A., Soll, B., & Lobato, M. I. (2017). Gender identity program: The scope of health treatment of transsexuals in Brazil. Journal of Sexual Medicine, 14, 342. https://doi.org/10.1016/j.jsxm.2017.04.616
Silva, D. C., Schwarz, K., Fontanari, A. M., Costa, A. B., Massuda, R., Henriques, A. A., Salvador, J., Silveira, E., Rosito, T. E., & Lobato, M. I. (2016). WHOQOL-100 before and after sex reassignment surgery in Brazilian male-to-female transsexual individuals. Journal of Sexual Medicine, 13(6), 988–993. https://doi.org/10.1016/j.jsxm.2016.03.370
Soll, B. M., Robles-García, R., Brandelli-Costa, A., Mori, D., Mueller, A., Vaitses-Fontanari, A. M., Cardoso-da-Silva, D., Schwarz, K., Abel-Schneider, M., Saadeh, A., & Lobato, M. I. (2017). Gender incongruence: A comparative study using ICD-10 and DSM-5 diagnostic criteria. Revista Brasileira de Psiquiatria, 40(2), 174–180. https://doi.org/10.1590/1516-4446-2016-2224
Valentine, S. E., & Shipherd, J. C. (2018). A systematic review of social stress and mental health among transgender and gender non-conforming people in the United States. Clinical Psychology Review, 66, 24–38. https://doi.org/10.1016/j.cpr.2018.03.003
Vanderlaan, D. P., Blanchard, R., Zucker, K. J., Massuda, R., Fontanari, A. M., Borba, A. O., Costa, A. B., Schneider, M. A., Mueller, A., Soll, B. M., & Schwarz, K. (2017). Birth order and androphilic male-to-female transsexualism in Brazil. Journal of Biosocial Science, 49(4), 527–535. https://doi.org/10.1017/S0021932016000584
Wiepjes, C. M., Nota, N. M., de Blok, C. J., Klaver, M., de Vries, A. L., Wensing-Kruger, S. A., de Jongh, R. T., Bouman, M. B., Steensma, T. D., Cohen-Kettenis, P., & Gooren, L. J. (2018). The Amsterdam Cohort of Gender Dysphoria Study (1972–2015): Trends in prevalence, treatment, and regrets. Journal of Sexual Medicine, 15(4), 582–590. https://doi.org/10.1016/j.jsxm.2018.01.016
Winters, S., & Conway, L. (2011). How many trans people are there? A 2011 update incorporating new data. Retrieved from https://www.transgenderasia.org/paper-how-many-trans-people-are-there.htm.
World Health Organization (WHO). (1992). The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. Retrieved from https://apps.who.int/iris/handle/10665/37958.
World Health Organization (WHO). (2020). Europe brief—Transgender health in the context of ICD-11. Retrieved from https://www.euro.who.int/en/health-topics/health-determinants/gender/gender-definitions/whoeurope-brieftransgender-health-in-the-context-of-icd-1.
Zucker, K. J. (2017). Epidemiology of gender dysphoria and transgender identity. Sexual Health, 14(5), 404–411. https://doi.org/10.1071/SH17067
Acknowledgements
The authors would like to thank Mrs. Rita de Cássia Souza de Oliveira for administrative support, the Medical File and Health Information Service (SAMIS), the Information Technology Management Coordination (CGTI), especially analyst Maria Tereza Pons and the Fundo de Incentivo à Pesquisa e Eventos (FIPE)—Hospital de Clínicas de Porto Alegre (HCPA).
Funding
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brazil (CAPES)—Finance Code 001 and Fundo de Incentivo à Pesquisa e Eventos (FIPE)—Hospital de Clínicas de Porto Alegre (HCPA).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Silva, D.C., Salati, L.R., Fontanari, A.M.V. et al. Prevalence of Gender Dysphoria in Southern Brazil: A Retrospective Study. Arch Sex Behav 50, 3517–3526 (2021). https://doi.org/10.1007/s10508-021-02036-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10508-021-02036-2