Abstract
Bisexual men are at increased risk for HIV/STI and early pregnancy involvement compared to heterosexual men, and minority stressors (e.g., enacted and internalized stigma) are associated with sexual risk behavior in samples of gay and bisexual men. However, few studies have specifically focused on bisexual men, and little is known about the unique predictors of sexual risk behavior in this population. Further, few studies have focused on positive sexual orientation-related factors such as identity affirmation, which may be protective against sexual risk behavior. As such, the goals of the current study were to examine minority stressors and identity affirmation as predictors of condomless sex among self-identified bisexual men, and whether these associations differed as a function of partner gender. We used four waves of data spanning 24 months from a subset of self-identified bisexual men in a larger cohort of gay and bisexual men ages 16–29 years at enrollment. At each wave, participants reported on up to four partners, allowing us to examine within-person associations. We used mixed effects negative binomial models to examine the associations between our predictors (discrimination, internalized binegativity, and identity affirmation) and condomless sex acts. In addition, we tested whether partner gender moderated each of the associations by including interaction effects in each of the models. Results indicated that higher levels of internalized binegativity and lower levels of identity affirmation were associated with less condomless sex with female partners, but they were not associated with condomless sex with male partners. Discrimination was not associated with condomless sex with male or female partners. These findings suggest that predictors of condom use among self-identified bisexual men differ as a function of partner gender, and they highlight the need to identify strategies to promote sexual health while also supporting positive identity development in this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Previous research has demonstrated that bisexual men are at increased risk for HIV/STI compared to heterosexual men. For example, in a nationally representative sample, 7.7% of self-identified bisexual men were HIV-positive compared to only .3% of self-identified heterosexual men who had never had sex with men (Caceres et al., 2018). Similarly, in a different nationally representative sample, 17.7% of self-identified bisexual men reported a lifetime diagnosis of genital warts, herpes, or syphilis compared to 5.3% of self-identified heterosexual men (Jeffries, 2010). There is also evidence that gay and bisexual adolescent men are at increased risk for pregnancy involvement compared to heterosexual adolescent men (Lindley & Walsemann, 2015; Saewyc, Poon, Homma, & Skay, 2008), but these studies have combined gay and bisexual adolescent men into a single group. Given that bisexual men are disproportionately affected by HIV/STI and early pregnancy involvement, it is critical to identify risk and protective factors in order to develop evidence-based prevention interventions. Previous research has demonstrated that minority stressors (e.g., enacted and internalized stigma) are modestly associated with sexual risk behavior (Balaji, Bowles, Hess, Smith, & Paz-Bailey, 2016; Newcomb & Mustanski, 2011), but these studies have also combined gay and bisexual men into a single group. Furthermore, few studies have focused on positive sexual orientation-related factors such as identity affirmation, which may be protective against sexual risk behavior. To fill these gaps, the goals of the current study were to examine minority stressors and identity affirmation as predictors of condomless sex among self-identified bisexual men, and whether these associations differed as a function of partner gender.
Numerous studies have found that experiences of enacted stigma (e.g., discrimination, physical assault) are associated with HIV risk behaviors (e.g., condomless anal sex with partners of positive or unknown HIV status, sex under the influence of alcohol or drugs) in diverse samples of men who have sex with men (MSM) (Balaji et al., 2016; Frye et al., 2015; Ha, Risser, Ross, Huynh, & Nguyen, 2015; Leluţiu-Weinberger et al., 2019; Meanley, Egan, & Bauermeister, 2018; Mizuno et al., 2012; Nakamura & Zea, 2010; Torres et al., 2013). There is also evidence that internalized stigma, or the internalization of negative attitudes toward sexual minorities, is associated with HIV risk behaviors among MSM. In a meta-analysis, Newcomb and Mustanski (2011) found a small overall effect size for the association between internalized homophobia and risky sexual behavior. Since then, additional studies have continued to find significant associations between internalized stigma and HIV risk behaviors among MSM, including greater number of anal sex partners and condomless anal sex (Amola & Grimmett, 2015; Puckett, Newcomb, Garofalo, & Mustanski, 2017; Ross et al., 2013). Despite this evidence, we are not aware of any previous studies that have specifically examined these associations among self-identified bisexual men. However, one recent study found that higher levels of internalized heterosexism at baseline predicted greater likelihood of HIV diagnosis one-year later in a sample of Black bisexual men (Watson, Allen, Pollitt, & Eaton, 2019), suggesting that internalized stigma may be associated with condomless sex among bisexual men as well.
In contrast to previous studies focused on enacted and internalized stigma as predictors of sexual risk behavior, few studies have focused on positive sexual orientation-related factors such as identity affirmation (i.e., feelings of comfort and pride in one’s sexual identity) (Paul, Smith, Mohr, & Ross, 2014). Identity affirmation may be protective against sexual risk behaviors, because those who are more accepting of their identities may take better care of their health. We are not aware of any previous studies that have specifically examined the association between identity affirmation and condomless sex, but there is some evidence that sexual orientation identity affirmation is associated with better mental and physical health, more health-promoting behavior (e.g., physical activity), less health-risk behavior (e.g., smoking), and higher self-esteem (Fredriksen-Goldsen, Kim, Bryan, Shiu, & Emlet, 2017; Toomey, Anhalt, & Shramko, 2016). Furthermore, there is also evidence that having more positive views of and attitudes toward one’s sexual orientation as well as being more open about and comfortable with one’s identity are associated with less sexual risk behavior among gay and bisexual men (Rosario, Schrimshaw, & Hunter, 2006; White & Stephenson, 2014). However, these studies have not specifically focused on the extent to which bisexual men feel pride in their sexual identity.
Among the few studies that have examined predictors of condomless sex specifically among bisexual men, findings suggest that partner gender may be an important factor to consider in order to understand bisexual men’s sexual health. For example, Stokes et al. (1993) found that self-identified bisexual men were less likely to report consistent condom use with female partners than with male partners. Our own recent work (Feinstein, Moran, Newcomb, & Mustanski, 2019b) has also found that self-identified bisexual men were more likely to report condomless sex with female partners than with male partners. Furthermore, we also found that self-identified bisexual men were more likely to report alcohol and marijuana use before sex with female partners than with male partners, and that the association between partner gender and condomless sex became nonsignificant after accounting for substance use before sex. These findings suggest that self-identified bisexual men may be more likely to have condomless sex with female partners than with male partners because of their use of substances before sex. Of note, one study did not find a significant association between partner gender and condomless sex in a sample of young MSM (Mustanski, Newcomb, & Clerkin, 2011), but nearly two-thirds of their sample identified as gay and only 12% of sexual partnerships were with female partners.
In sum, bisexual men are at increased risk for HIV/STI and early pregnancy involvement compared to heterosexual men, but little is known about risk factors for condomless sex in this population. Given recent evidence that bisexual men report more condomless sex with female partners than with male partners, it is important to examine whether risk factors for condomless sex extend to partners of different genders. As such, in an effort to extend our previous work with this sample (Feinstein et al., 2019b), the goals of the current study were to examine: (1) the extent to which discrimination, internalized binegativity, and identity affirmation were associated with condomless sex among self-identified bisexual men; and (2) whether these associations differed depending on the gender of one’s partner. We used four waves of data spanning 24 months from a cohort of young MSM ages 16–29. At each wave (6 months apart), participants reported on their behavior with up to four partners during the prior 6 months, enabling us to examine within-person associations. In order to isolate the unique effects of minority stressors and identity affirmation on condomless sex, we controlled for participant demographics and known correlates of sexual risk behavior (e.g., relationship status, substance use before sex; described in detail in the “Method” section).
Method
Participants
Data for the current study came from an ongoing longitudinal cohort study of young MSM focused on the multilevel influences that impact HIV and substance use in this population (the RADAR study). The study consists of three cohorts of young MSM first recruited in 2007, 2010, and 2015. Participants were recruited in the metropolitan Chicago area and completed study visits every 6 months. Criteria for inclusion were being ages 16–29 at baseline, assigned male at birth, English-speaking, and either identified as a sexual minority or reported having sex with a man in the previous year. Participants in all three cohorts could recruit their serious partners and up to three peers into the cohort as long as they met inclusion criteria.
Procedure
Study visits included completing a psychosocial survey and a network interview as well as the collection of biomedical specimens. Surveys were administered using a computer-assisted self-interview and participants were paid $50 for each study visit. All study procedures were approved by the Institutional Review Board, and a waiver of parental permission was granted for participants ages 16–17 (Mustanski, 2011). In December 2016, we began asking participants who identified as bisexual about their internalized binegativity and their experiences with anti-bisexual discrimination at all study visits. The current study used data collected through June 2018. Consistent with our previous work with this sample (Feinstein et al., 2019b), only young MSM who identified as bisexual and male for at least one visit during this period, were HIV-negative, and reported at least one cisgender male or female partner were included in the current study (analytic N = 142). Participants were asked about their sexual orientation and gender identity at every visit, so a specific visit could be excluded for a participant if their sexual orientation or gender identity changed between visits to no longer meet these criteria. The analytic sample provided data for 600 partnerships during this period (24.0% cisgender female partners and 76.0% cisgender male partners). Demographic characteristics are shown in Table 1.
Measures
Demographics
Participants reported their age, race/ethnicity, and education level on a demographic survey. These were included in analyses as covariates. For race/ethnicity, White was treated as the reference group. Education level was recoded as a dichotomous variable based on whether the participant’s education level was college or higher.
Anti-Bisexual Experiences
Participants reported on their experiences with anti-bisexual discrimination using the Brief Anti-Bisexual Experiences Scale (Brief ABES; Dyar, Feinstein, & Davila, 2019). The Brief ABES is an 8-item version of the Anti-Bisexual Experiences Scale (Brewster & Moradi, 2010). Similar to the original measure, it assesses three types of anti-bisexual discrimination, including sexual orientation instability assumptions (e.g., “People have acted as if bisexuality is ‘just a phase’ I am going through”), sexual irresponsibility assumptions (e.g., “People have treated me as if I am obsessed with sex because I am bisexual”), and experiences of interpersonal hostility (e.g., “People have not wanted to be my friend because I identify as bisexual”). Items were rated on a six-point scale asking how often each item occurred ranging from 1 (“Never”) to 6 (“Almost all of the time [more than 70% of the time]”). The scale is administered twice, once asking about experiences with lesbian and gay people (Cronbach’s alpha = .90) and again asking about experiences with heterosexual people (Cronbach’s alpha = .89).
Internalized Binegativity and Identity Affirmation
The Bisexual Identity Inventory (BII; Paul et al., 2014) was used to measure both internalized binegativity and identity affirmation. Internalized binegativity was measured using five items that asked about negative attitudes or feelings related to one’s bisexual identity (e.g., “It’s unfair that I am attracted to people of more than one gender.”). Identity affirmation was measured using six items that asked about bisexual identity acceptance (e.g., “I am grateful for my bisexual identity.”). All items on the BII were rated on a seven-point scale ranging from 1 (“Strongly Disagree”) to 7 (“Strongly Agree”). Cronbach’s alpha was high for both BII scales (internalized binegativity = .79, identity affirmation = .90).
Condomless Sex
Measurement of condomless sex was done at each visit using the HIV Risk Assessment for Sexual Partnerships (H-RASP) (Swann, Newcomb, & Mustanski, 2018). The H-RASP is a self-administered interview of sexual behavior and situational context at the sexual partnership level. Participants completed the H-RASP at every time point and could report on up to four of their most recent sexual partnerships that had occurred in the prior 6 months. The H-RASP has been demonstrated to have good validity in comparison with diary data (Swann et al., 2018) and network interviews (Hogan et al., 2016).
The data collected on the H-RASP included partner demographic factors. Participants were asked to report on the gender identity of each partner with response options: (1) male, (2) female, (3) male assigned at birth with a different gender identity, and (4) female assigned at birth with a different gender identity. They were also asked to report on their partner’s HIV status the last time they had sex. Response options were: (1) HIV-negative, (2) HIV-positive, and (3) I don’t know their HIV status. We recoded HIV status into a new HIV concordance variable. Partnerships where the participant and their partner had the same status were coded 1 for concordant. For partnerships where the two had different statuses or partner HIV status was unknown, the partnership was coded as 0 for discordant. Participants were also asked to report on the seriousness of their relationship with each partner. Response options were recoded as “1” for serious versus “0” for casual (which encompassed the response options “casually dating but not serious,” “sleeping with this person but not dating,” “one night stand,” and “stranger or anonymous person”).
Participants were also asked context-specific questions about their partnerships. Participants were asked for each partnership if they had taken pre-exposure prophylaxis (PrEP) medication to reduce their risk of HIV transmission. Response options were “no” (0) and “yes” (1). Participants reported on how frequently they drank alcohol prior to sex with that partner in the last 6 months on a five point scale ranging from never (1) to always (5). We dichotomized responses for the present analyses (0 = never, 1 = any alcohol consumption prior to sex). The same question was asked for marijuana use and was recoded in the same way as alcohol before sex.
Condomless sex was measured for both male and female partnerships. For male partners, participants were asked separately about insertive and receptive anal sex. For female partners, participants were asked separately about anal and vaginal sex. The number of condomless sex acts was assessed using two questions: (1) “How many times did you have [vaginal/anal] sex with [partner name] during the past 6 months?” and (2) “Of the [number] time(s) you’ve had [vaginal/anal] sex with [partner name], how many of these times did you have sex without using a condom?” Responses were Winsorized at three standard deviations above the mean to limit the effect of outliers. The number of acts was combined across insertive and receptive anal sex for male partners and anal and vaginal sex for female partners.
Statistical Analyses
Mixed effects negative binomial models were used to model the effects of anti-bisexual experiences, internalized binegativity, and identity affirmation on condomless sex acts. The mixed-effects approach was necessary to account for multiple partnerships (Level 1) stemming from the participants (Level 2) in our sample. We employed negative binomial models to adjust for the skewed nature of a count variable like condomless sex acts. Analyses were performed in R version 3.4 with the “glmmTMB” package (Magnusson et al., 2016; R Core Team, 2017). Results for the models are reported in the form of incidence rate ratios (IRRs). IRRs are interpreted as the rate of change in number of condomless sex acts for every one-unit change in the predictor. Partnerships were only included in the present analyses if the participant identified as bisexual, reported a male gender identity, and their partner was identified by the participant as either cisgender male or cisgender female. As noted, participants were asked about their sexual orientation and gender identity at every visit, so a specific visit could be excluded for a participant if their sexual orientation or gender identity changed between visits to no longer meet these criteria. Partnerships that appeared in multiple visits were flagged and included as a covariate in analyses in accordance with previous partnership-level research (Feinstein et al., 2019b; Mustanski, Starks, & Newcomb, 2014).
First, in preliminary analyses, we tested the bivariate association between partner gender and condomless sex acts as well as the bivariate associations between our primary predictors (internalized binegativity, identity affirmation, anti-bisexual experiences from heterosexual people, and anti-bisexual experiences from gay and lesbian people) and condomless sex acts. Then, in our main analyses, we tested whether partner gender moderated the associations between our primary predictors and condomless sex acts. In order to isolate the unique effects of our predictors of interest, every model controlled for participant demographics (age, race/ethnicity, and education level) and partner/relationship factors (partner gender, relationship status, repeat partner status, PrEP use, HIV concordance, alcohol use before sex, and marijuana use before sex). In each model, we tested to see if partner gender moderated the effects of our primary predictors by including the interaction effect between partner gender and the predictor. Each of the primary predictors was mean-centered for use in interaction terms. If an interaction effect was significant, we ran a comparison of the adjusted means of the outcome variable across the two partner genders (cisgender male and cisgender female) at one standard deviation below and above the mean for the primary predictor.
Results
Preliminary Analyses
Bivariate negative binomial models demonstrated significant differences in the number of condomless sex acts (IRR = 2.29, p < .001) between male and female partners, such that participants reported more sex acts with female partners. There were no significant bivariate differences in the number of condomless sex acts based on internalized binegativity (IRR = .89, p = .370), identity affirmation (IRR = 1.23, p = .074), anti-bisexual experiences from gay/lesbian people (IRR = .93, p = .657), or anti-bisexual experiences from heterosexual people (IRR = 1.01, p = .954).
Internalized Binegativity
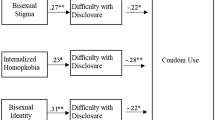
The negative binomial model for internalized binegativity is presented in Table 2. The main effects of internalized binegativity (IRR = 1.08, p = .493) and female partner gender (IRR = 1.20, p = .512) were not significant. However, there was a significant interaction between internalized binegativity and female partner gender (IRR = .55, p = .011). Participants reported significantly fewer condomless sex acts with female partners if they reported high internalized binegativity (IRR = .29, p = .019; see Fig. 1). In contrast, internalized binegativity was not significantly associated with condomless sex acts with male partners (IRR = 1.21, p = .493). Of note, the strongest effects in the model were between several covariates (serious relationship, repeat partner, alcohol use before sex, and marijuana use before sex) and condomless sex.
Identity Affirmation
There was a similar pattern of results for identity affirmation (see Table 2). Neither identity affirmation (IRR = 1.09, p = .414) nor female partner gender (IRR = 1.20, p = .267) were significantly associated with condomless sex acts. However, there was a significant interaction between identity affirmation and female partner gender (IRR = 1.54, p = .010). Participants reported significantly fewer condomless sex acts with female partners if they reported low identity affirmation (IRR = 3.90, p < .001; see Fig. 2). In contrast, identity affirmation was not significantly associated with condomless sex acts with male partners (IRR = 1.25, p = .414). All of the covariates that were significant in the internalized binegativity model were also significant in the identity affirmation model.
Anti-Bisexual Experiences
Results for anti-bisexual experiences are presented in Table 3. The main effects of anti-bisexual experiences from heterosexual people (IRR = 1.09, p = .587) and female partner gender (IRR = 1.47, p = .139) were not significant, nor was their interaction (IRR = 1.03, p = .899). Similarly, the main effects of anti-bisexual experiences from gay/lesbian people (IRR = .95, p = .764), female partner gender (IRR = 1.52, p = .111), and their interaction were not significant (IRR = .95, p = .826).
Discussion
Despite evidence that bisexual men are at increased risk for HIV/STI and early pregnancy involvement compared to heterosexual men, there has been a lack of empirical attention to the unique predictors of condomless sex in this population. To fill this gap, we examined minority stressors and identity affirmation as predictors of condomless sex in a sample of self-identified bisexual men. The few studies that have focused on bisexual men have shown that condom use among bisexual men differs depending on the gender of their partners, suggesting that condomless sex may be more likely with female partners (Feinstein et al., 2019b; Stokes et al., 1993; for an exception, see Mustanski et al., 2011); thus, we also examined whether these associations differed as a function of partner gender.
Previous research has found a small positive association between internalized stigma and sexual risk behavior among gay and bisexual men in general (Newcomb & Mustanski, 2011), and there is some evidence that having a more established and positive sexual identity is associated with less sexual risk behavior as well (Rosario et al., 2006; White & Stephenson, 2014). However, we found that higher levels of internalized binegativity and lower levels of identity affirmation were associated with less condomless sex with female partners, and they were not associated with condomless sex with male partners. There are at least two potential explanations for these unexpected findings. First, bisexual men who feel worse about their sexuality (i.e., those with higher internalized binegativity and lower identity affirmation) may have internalized the myth that bisexual men “bridge” HIV/STI from male to female partners (Friedman et al., 2017; Jeffries, 2010). In turn, they may be more likely to use condoms with female partners as a way to avoid reinforcing this myth. Second, bisexual men who feel better about their sexuality may experience more positive affect in general, and there is some evidence that positive affect is associated with engagement in condomless anal sex among men who have sex with men (Mustanski, 2007; Sarno, Mohr, & Rosenberger, 2017). It will be important for future research to directly test these potential explanations.
Given that higher levels of internalized stigma and lower levels of identity affirmation were associated with less condomless sex with female partners, it could be inferred that interventions focused on reducing internalized stigma and affirming bisexual identities may inadvertently contribute to sexual risk behavior with female partners. That said, by combining intervention content focused on reducing internalized stigma and affirming bisexual identities with intervention content focused on promoting sexual health, it may be possible to achieve both goals without unintended consequences. Israel et al. (2019) recently developed an online intervention to reduce internalized binegativity. Their intervention guided participants to re-evaluate and challenge negative stereotypes about bisexuality, to externalize negative messages they may have received about bisexuality, and to adopt affirming attitudes toward bisexuality. Compared to participants in the control condition, those who completed the intervention reported lower post-test levels of internalized and anticipated binegativity as well as higher post-test levels of identity affirmation and positive affect. Content and exercises from their intervention could be included in a sexual health promotion intervention specifically for bisexual men, which could then hopefully achieve promotive effects on self-acceptance and sexual risk reduction. It will be important to test this combined approach to enhancing self-acceptance and reducing sexual risk behavior in future research. That said, few studies have directly examined what bisexual people want from interventions (for an exception, see Feinstein, Dodge, Korpak, Newcomb, & Mustanski, 2019a), and there is a critical need for additional research, especially qualitative research, to advance our understanding of bisexual people’s perceived health needs and their intervention preferences.
In contrast to our findings for condomless sex with female partners, internalized binegativity and identity affirmation were not associated with condomless sex with male partners. This may be due to male partners being perceived as riskier (i.e., more likely to have HIV or another STI), in which case bisexual men may use condoms with male partners regardless of their levels of internalized binegativity and identity affirmation. Consistent with this possibility, previous research has found that behaviorally bisexual men perceive male partners as riskier than female partners in relation to HIV risk (Dodge et al., 2008; Malebranche et al., 2010). Of note, the differences between our findings and previous findings highlight the importance of focusing specifically on bisexual men, accounting for partner gender, and accounting for other known correlates of condomless sex. For example, although Rosario et al. (2006) found that more positive attitudes toward homosexuality/bisexuality were associated with a lower likelihood of engaging in unprotected receptive anal sex, their sample was relatively small (N = 80), only 31% of their participants identified as bisexual, and their analyses did not account for substance use before sex or whether partners were serious or casual (both of which are known correlates of condomless sex). Similarly, although White and Stephenson (2014) had a large sample (N = 703), the vast majority (91.6%) identified as gay and their analyses did not account for substance use before sex.
Finally, we did not find a significant association between anti-bisexual discrimination and condomless sex in our sample. This is in contrast to previous findings that experiences of enacted stigma (e.g., discrimination, physical assault) are associated with HIV risk behaviors (e.g., condomless anal sex with partners of positive or unknown HIV status, sex under the influence of alcohol or drugs) among MSM (Balaji et al., 2016; Frye et al., 2015; Ha et al., 2015; Leluţiu-Weinberger et al., 2019; Meanley et al., 2018; Mizuno et al., 2012; Nakamura & Zea, 2010; Torres et al., 2013). It is possible that the associations between experiences of enacted stigma and HIV risk behaviors found in other studies would have become nonsignificant after accounting for substance use. In fact, other studies have found indirect associations between experiences of stigma and HIV risk behaviors through substance use (Ferlatte, Hottes, Trussler, & Marchand, 2014; Ha et al., 2015), highlighting the importance of accounting for known predictors of condomless sex.
It is important to note that the strongest correlates of condomless sex in our models were several of our covariates. Consistent with previous research, being in a serious relationship and having a repeat partner over time (e.g., Newcomb, Moran, Feinstein, & Mustanski, 2018) as well as using alcohol and marijuana before sex (see Mustanski et al., 2011) were all associated with more condomless sex regardless of partner gender. Therefore, while our findings suggest that internalized binegativity and identity affirmation play a role in bisexual men’s condom use with female partners, they also suggest that other factors play stronger roles in their condom use with both male and female partners. Based on these findings, it is important to account for these well-documented correlates of condom use when examining other potential predictors of condomless sex.
The current findings should be interpreted in the context of several limitations. First, while our focus on partner gender was a strength of our study, we were unable to examine condomless sex with transgender partners because too few participants reported any transgender partners at any visits. Second, our use of partner-level analyses was another strength of our study, but we cannot say whether findings extend to specific sexual encounters where additional variability may exist (i.e., the event level). Participants were also limited to providing detailed information on up to four partners at each visit. While this may have affected our results, only 12.7% of participants reported more than four partners during at least one of the visits included in the analyses. Furthermore, out of all of the visits included in the analyses, more than four partners were only reported at 8.6% of those visits. Third, although we accounted for participant PrEP use and HIV concordance between partners, we were unable to account for participant adherence to PrEP or partner PrEP use, both of which can influence condom use (Newcomb et al., 2018). Fourth, we did not collect data on use of birth control among female partners or participant fertility intentions, both of which could influence condom use with female partners. It will be important for future research to examine whether the current findings are replicated after controlling for these variables. That said, while these variables could influence condom use with female partners, it is unknown if controlling for them would affect the extent to which internalized binegativity and identity affirmation are associated with condom use with female partners. That remains an empirical question. Fifth, our sample reported relatively low mean levels of discrimination and internalized binegativity, and relatively high mean levels of identity affirmation. As such, it will be important for future research to examine the associations between these variables and condomless sex in samples of bisexual men who experience more stigma-related stress and feel less pride in their identities. Finally, despite a large racially/ethnically diverse sample, all participants were from the Chicago area.
Despite these limitations, the current study was the first to examine the role of partner gender in the associations among minority stressors, identity affirmation, and condomless sex in a sample of self-identified bisexual men. Findings highlight the need to identify strategies to promote sexual health among self-identified bisexual men while also supporting positive identity development. Although HIV prevention interventions have been developed for behaviorally bisexual men, none have been tailored to the unique needs of self-identified bisexual men (see Feinstein et al., 2019a). Therefore, in order to address the sexual health needs of self-identified bisexual, interventions need to be developed for this population and they need to address the role of partner gender (e.g., include content focused on sexual risk and protection with partners of different genders) as well as identity-related factors (e.g., internalized stigma, identity affirmation).
References
Amola, O., & Grimmett, M. A. (2015). Sexual identity, mental health, HIV risk behaviors, and internalized homophobia among black men who have sex with men. Journal of Counseling and Development, 93(2), 236–246. https://doi.org/10.1002/j.1556-6676.2015.00199.x.
Balaji, A. B., Bowles, K. E., Hess, K. L., Smith, J. C., & Paz-Bailey, G. (2016). Association between enacted stigma and HIV-related risk behavior among MSM. National HIV Behavioral Surveillance System. https://doi.org/10.1007/s10461-016-1599-z.
Brewster, M. E., & Moradi, B. (2010). Perceived experiences of anti-bisexual prejudice: Instrument development and evaluation. Journal of Counseling Psychology, 57(4), 451–468. https://doi.org/10.1037/a0021116.
Caceres, B. A., Brody, A. A., Halkitis, P. N., Dorsen, C., Yu, G., & Chyun, D. A. (2018). Sexual orientation differences in modifiable risk factors for cardiovascular disease and cardiovascular disease diagnoses in men. LGBT Health, 5, 284–294.
Dodge, B., Jeffries, W. L., & Sandfort, T. G. (2008). Beyond the down low: Sexual risk, protection, and disclosure among at-risk Black men who have sex with both men and women (MSMW). Archives of Sexual Behavior, 37, 683–696.
Dyar, C., Feinstein, B. A., & Davila, J. (2019). Development and validation of a brief version of the Anti-Bisexual Experiences Scale. Archives of Sexual Behavior, 48, 175–189.
Feinstein, B. A., Dodge, B., Korpak, A. K., Newcomb, M. E., & Mustanski, B. (2019a). Improving the health of cisgender men who identify as bisexual: What do they want from interventions? Sexuality Research and Social Policy, 16, 385–391.
Feinstein, B. A., Moran, K. O., Newcomb, M. E., & Mustanski, B. (2019b). Differences in HIV risk behaviors between self-identified gay and bisexual young men who are HIV-negative. Archives of Sexual Behavior, 48, 261–275.
Ferlatte, O., Hottes, T. S., Trussler, T., & Marchand, R. (2014). Evidence of a syndemic among young Canadian gay and bisexual men: uncovering the associations between anti-gay experiences, psychosocial issues, and HIV risk. AIDS and Behavior, 18(7), 1256–1263. https://doi.org/10.1007/s10461-013-0639-1.
Fredriksen-Goldsen, K. I., Kim, H.-J., Bryan, A. E. B., Shiu, C., & Emlet, C. A. (2017). The cascading effects of marginalization and pathways of resilience in attaining good health among LGBT older adults. The Gerontologist, 57, S72–S83.
Friedman, M. R., Stall, R., Plankey, M., Shoptaw, S., Herrick, A. L., Surkan, P. J., et al. (2017). Stability of bisexual behavior and extent of viral bridging behavior among men who have sex with men and women. Archives of Sexual Behavior, 46, 903–912.
Frye, V., Nandi, V., Egan, J., Cerda, M., Greene, E., Van Tieu, H., & Koblin, B. A. (2015). Sexual orientation- and race-based discrimination and sexual HIV risk behavior among urban MSM. AIDS and Behavior, 19(2), 257–269. https://doi.org/10.1007/s10461-014-0937-2.
Ha, H., Risser, J. M. H., Ross, M. W., Huynh, N. T., & Nguyen, H. T. M. (2015). Homosexuality-related stigma and sexual risk behaviors among men who have sex with men in Hanoi, Vietnam. Archives of Sexual Behavior, 44(2), 349–356. https://doi.org/10.1007/s10508-014-0450-8.
Hogan, B., Melville, J. R., Philips II, G. L., Janulis, P., Contractor, N., Mustanski, B. S., & Birkett, M. (2016). Evaluating the paper-to-screen translation of participant-aided sociograms with high-risk participants. Paper presented at the Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems.
Israel, T., Choi, A. Y., Goodman, J. A., Matsuno, E., Lin, Y.-J., Kary, K. G., & Merrill, C. R. S. (2019). Reducing internalized binegativity: Development and efficacy of an online intervention. Psychology of Sexual Orientation and Gender Diversity, 6, 149–159.
Jeffries, W. L. T. (2010). HIV testing among bisexual men in the United States. AIDS Education and Prevention, 22, 356–370.
Leluţiu-Weinberger, C., Rendina, H. J., Mirandola, M., Gios, L., Folch, C., Rafila, A., & Pachankis, J. E. (2019). The role of gay-related stigma in HIV-risk behavior among sexual minority men in Europe. AIDS and Behavior, 23, 684–694. https://doi.org/10.1007/s10461-018-2306-z.
Lindley, L., & Walsemann, K. (2015). Sexual orientation and risk of pregnancy among New York City high-school students. American Journal of Public Health, 105, 1379–1386. https://doi.org/10.2105/ajph.2015.302553.
Magnusson, A., Skaug, H., Nielsen, A., Berg, C., Kristensen, K., Maechler, M., … Brooks, M. (2016). glmmTMB: Generalized linear mixed models using template model builder. Retrieved from https://github.com/glmmTMB/.
Malebranche, D. J., Arriola, K. J., Jenkins, T. R., Dauria, E., & Patel, S. N. (2010). Exploring the “bisexual bridge”: A qualitative study of risk behavior and disclosure of same-sex behavior among black bisexual men. American Journal of Public Health, 100, 159–164.
Meanley, S., Egan, J. E., & Bauermeister, J. A. (2018). Policing heteronormativity and sexual risk-taking among young adult men who have sex with men in the Detroit metro area. AIDS and Behavior, 22, 3991–4000. https://doi.org/10.1007/s10461-018-2257-4.
Mizuno, Y., Borkowf, C., Millett, G. A., Bingham, T., Ayala, G., & Stueve, A. (2012). Homophobia and racism experienced by Latino men who have sex with men in the United States: correlates of exposure and associations with HIV risk behaviors. AIDS and Behavior, 16(3), 724–735. https://doi.org/10.1007/s10461-011-9967-1.
Mustanski, B. (2007). The influence of state and trait affect on HIV risk behaviors: A daily diary study of MSM. Health Psychology, 26, 618–626.
Mustanski, B. (2011). Ethical and regulatory issues with conducting sexuality research with LGBT adolescents: A call to action for a scientifically informed approach. Archives of Sexual Behavior, 40(4), 673–686. https://doi.org/10.1007/s10508-011-9745-1.
Mustanski, B., Newcomb, M. E., & Clerkin, E. M. (2011). Relationship characteristics and sexual risk-taking in young men who have sex with men. Health Psychology, 30, 597–605.
Mustanski, B., Starks, T., & Newcomb, M. E. (2014). Methods for the design and analysis of relationship and partner effects on sexual health. Archives of Sexual Behavior, 43(1), 21–33. https://doi.org/10.1007/s10508-013-0215-9.
Nakamura, N., & Zea, M. C. (2010). Experiences of homonegativity and sexual risk behaviour in a sample of Latino gay and bisexual men. Culture, Health and Sexuality, 12(1), 73–85. https://doi.org/10.1080/13691050903089961.
Newcomb, M. E., Moran, K., Feinstein, B. A., & Mustanski, B. (2018). Pre-exposure prophylaxis (PrEP) use and condomless anal sex: Evidence of risk compensation in a cohort of young men who have sex with men. Journal of Acquired Immune Deficiency Syndromes, 77, 358–364.
Newcomb, M. E., & Mustanski, B. (2011). Moderators of the relationship between internalized homophobia and risky sexual behavior in men who have sex with men: a meta-analysis. Archives of Sexual Behavior, 40(1), 189–199. https://doi.org/10.1007/s10508-009-9573-8.
Paul, R., Smith, N. G., Mohr, J. J., & Ross, L. E. (2014). Measuring dimensions of bisexual identity: Initial development of the bisexual identity inventory. Psychology of Sexual Orientation and Gender Diversity, 1, 452–460.
Puckett, J. A., Newcomb, M. E., Garofalo, R., & Mustanski, B. (2017). Examining the conditions under which internalized homophobia is associated with substance use and condomless sex in young MSM: The moderating role of impulsivity. Annals of Behavioral Medicine, 51(4), 567–577. https://doi.org/10.1007/s12160-017-9878-0.
R Core Team. (2017). R: A language and environment for statistical computing. Retrieved from https://www.R-project.org/.
Rosario, M., Schrimshaw, E. W., & Hunter, J. (2006). A model of sexual risk behaviors among young gay and bisexual men: Longitudinal associations of mental health, substance abuse, sexual abuse, and the coming-out process. AIDS Education and Prevention, 18(5), 444–460.
Ross, M. W., Berg, R. C., Schmidt, A. J., Hospers, H. J., Breveglieri, M., Furegato, M., & Weatherburn, P. (2013). Internalised homonegativity predicts HIV-associated risk behavior in European men who have sex with men in a 38-country cross-sectional study: Some public health implications of homophobia. British Medical Journal Open, 3(2), e001928. https://doi.org/10.1136/bmjopen-2012-001928.
Saewyc, E. M., Poon, C. S., Homma, Y., & Skay, C. L. (2008). Stigma management? The links between enacted stigma and teen pregnancy trends among gay, lesbian, and bisexual students in British Columbia. Canadian Journal of Human Sexuality, 17(3), 123–139.
Sarno, E. L., Mohr, J. J., & Rosenberger, J. G. (2017). Affect and condom use among men who have sex with men: A daily study. AIDS and Behavior, 21, 1429–1443.
Stokes, J. P., McKirnan, D., & Burzette, R. (1993). Sexual behavior, condom use, disclosure of sexuality, and stability of sexual orientation in bisexual men. Journal of Sex Research, 30, 203–213.
Swann, G., Newcomb, M. E., & Mustanski, B. (2018). Validation of the HIV risk assessment of sexual partnerships (H-RASP): Comparison to a two month prospective diary study. Archives of Sexual Behavior, 47(1), 121–131. https://doi.org/10.1007/s10508-017-1033-2.
Toomey, R. B., Anhalt, K., & Shramko, M. (2016). An examination of the validity and reliability of a measure of sexual orientation identity exploration, resolution, and affirmation. Self and Identity, 15, 488–504.
Torres, H. L., Delonga, K., Lee, S., Gladstone, K. A., Barrad, A., Huckaby, S., & Gore-Felton, C. (2013). Sociocontextual factors: Moving beyond individual determinants of sexual risk behavior among gay and bisexual adolescent males. Journal of LGBT Youth, 10(3), 173–185. https://doi.org/10.1080/19361653.2013.799000.
Watson, R. J., Allen, A., Pollitt, A. M., & Eaton, L. A. (2019). Risk and protective factors for sexual health outcomes among black bisexual men in the U.S.: Internalized heterosexism, sexual orientation disclosure, and religiosity. Archives of Sexual Behavior, 48, 243–253. https://doi.org/10.1007/s10508-018-1216-5.
White, D., & Stephenson, R. (2014). Identity formation, outness, and sexual risk among gay and bisexual men. American Journal of Men’s Health, 8(2), 98–109. https://doi.org/10.1177/1557988313489133.
Funding
This research was supported by a grant from the National Institute on Drug Abuse (U01DA036939; PI: Mustanski). Brian Feinstein’s time was supported by a grant from the National Institute on Drug Abuse (K08DA045575; PI: Feinstein). Elissa Sarno’s time was supported by a grant from the National Institute on Alcohol Abuse and Alcoholism (F32AA028194; PI: Sarno). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Review Board at Northwestern University.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Feinstein, B.A., Swann, G., Sarno, E.L. et al. Minority Stressors and Identity Affirmation as Predictors of Condomless Sex Among Self-Identified Bisexual Men: The Role of Partner Gender. Arch Sex Behav 50, 1057–1065 (2021). https://doi.org/10.1007/s10508-020-01775-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10508-020-01775-y