Abstract
Fear has been suggested as the crucial diagnostic variable that may distinguish vaginismus from dyspareunia. Unfortunately, this has not been systematically investigated. The primary purpose of this study, therefore, was to investigate whether fear as evaluated by subjective, behavioral, and psychophysiological measures could differentiate women with vaginismus from those with dyspareunia/provoked vestibulodynia (PVD) and controls. A second aim was to re-examine whether genital pain and pelvic floor muscle tension differed between vaginismus and dyspareunia/PVD sufferers. Fifty women with vaginismus, 50 women with dyspareunia/PVD, and 43 controls participated in an experimental session comprising a structured interview, pain sensitivity testing, a filmed gynecological examination, and several self-report measures. Results demonstrated that fear and vaginal muscle tension were significantly greater in the vaginismus group as compared to the dyspareunia/PVD and no-pain control groups. Moreover, behavioral measures of fear and vaginal muscle tension were found to discriminate the vaginismus group from the dyspareunia/PVD and no-pain control groups. Genital pain did not differ significantly between the vaginismus and dyspareunia/PVD groups; however, genital pain was found to discriminate both clinical groups from controls. Despite significant statistical differences on fear and vaginal muscle tension variables between women suffering from vaginismus and dyspareunia/PVD, a large overlap was observed between these conditions. These findings may explain the great difficulty health professionals experience in attempting to reliably differentiate vaginismus from dyspareunia/PVD. The implications of these data for the new DSM-5 diagnosis of Genito-Pelvic Pain/Penetration Disorder are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Until the publication of fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association, 2013) dyspareunia and vaginismus were typically classified as distinct sexual pain disorders. For example, in the DSM-IV-TR, vaginismus was defined as “the involuntary spasm of the musculature of the outer third of the vagina that interferes with intercourse,” while dyspareunia was defined as “genital pain associated with sexual intercourse” (American Psychiatric Association, 2000). Most health professionals and non-DSM classifications appeared to accept this diagnostic differentiation (e.g., American Congress of Obstetricians and Gynecologists, 1995; Basson et al., 2004; Binik, 2010a, 2010b; Lahaie, Boyer, Binik, Amsel, & Khalifé, 2010; Merskey & Bogduk, 1994; World Health Organization, 1992).
This differentiation between dyspareunia and vaginismus is reflected in the development of divergent treatment approaches for these disorders. The standard treatment approach for vaginismus has focused on eliminating vaginal muscle spasm using relaxation/desensitization, progressive vaginal dilatation, and sexual education (e.g., Kaplan, 1974; Masters & Johnson, 1970; Sims, 1861; van Lankveld et al., 2006). On the other hand, treatments for dyspareunia have traditionally concentrated on treating the presumed underlying medical (e.g., infection, inflammation) or psychological (e.g., sexual abuse, marital problems, lack of sexual arousal) factors that are assumed to cause the pain. Such treatments have ranged from medication and surgery to sex and couple therapy (e.g., Foster et al., 2010; Landry, Bergeron, Dupuis, & Desrochers, 2008).
Unfortunately, the original classificatory decision made in the 19th century to define vaginismus and dyspareunia as separate syndromes was not based on empirical research (Binik, 2010a, 2010b). In fact, subsequently collected data have challenged this longstanding decision. First, several studies have shown that the differential diagnosis of vaginismus from dyspareunia is not reliable (Basson, 1996; de Kruiff, ter Kuile, Weijenberg, & van Lankveld, 2000; Engman, 2007; Engman, Lindehammer, & Wijman, 2004; Engman, Wijma, & Wijma, 2007, 2008; Reissing, Binik, & Khalifé, 2004; van Lankveld, Brewaeys, ter Kuile, & Weijenborg, 1995). In particular, attempts to differentiate provoked vestibulodynia (PVD) from vaginismus using measures of pelvic floor muscle spasm or genital pain have failed (de Kruiff et al., 2000; Reissing et al., 2004). This has led many to argue that the central defining characteristic of vaginismus, vaginal muscle spasm, may not be a valid or diagnostically reliable marker of the disorder (Engman et al., 2004; Frasson et al., 2009; Reissing et al., 2004; Shafik & El-Sibai, 2002; van der Velde, 1999; van der Velde, Laan, & Everaerd, 2001). Such findings have led to the recent DSM-5 decision to collapse vaginismus and dyspareunia into one category called “genito-pelvic pain/penetration disorder.” This disorder is defined as marked difficulty with at least one of the following: (a) vaginal intercourse/penetration, (b) genito-pelvic pain, (c) fear of vaginal intercourse/penetration/pain, or (d) heightened pelvic floor muscle tension during attempted penetration (American Psychiatric Association, 2013).
Despite the fact that it has not been possible to reliably discriminate vaginismus from dyspareunia/PVD on the basis of muscle spasm or genital pain, it has been suggested that fear may be a possible differentiator. Over a century ago, Walthard (1909) suggested that vaginismus was a phobic reaction to an excessive fear of pain. This idea was also discussed by Kaplan (1974) and supported by data collected by Ward and Ogden (1994). Unfortunately, this notion was not systematically pursued until Reissing et al. (2004) demonstrated that women with vaginismus undergoing a gynecological examination displayed a significantly higher number of defensive/avoidant behaviors than matched controls or women suffering from dyspareunia/PVD. Reissing et al. proposed that vaginismus might be better conceptualized as a specific phobia characterized by an excessive fear and avoidance of vaginal penetration situations. Although the behavioral measures of fear in the Reissing et al. study clearly differentiated vaginismus from dyspareunia/PVD, there were some significant methodological limitations to this research. The characterization of fear was solely based on behavior and did not include the assessment of subjective or physiological indicators of fear. There was no assessment of the reliability of the behavioral rating system for fear.
Therefore, the primary goal of the present study was to investigate whether the degree of fear displayed during a vaginal penetration situation such as a gynecological examination could discriminate women suffering from vaginismus from those with dyspareunia/PVD and controls. A variety of methods were used to measure fear, including self-report, blinded behavioral assessments, and psychophysiological indicators such as heart rate, skin conductance, and non-pelvic floor muscle tension. Specifically, we hypothesized that women in the vaginismus group would display significantly greater fear as compared with women in the dyspareunia/PVD group who in turn would experience more fear than control women. Our second hypothesis was that pelvic floor muscle tension, rather than the traditional involuntary spasm criterion would distinguish women in the vaginismus group from women in the dyspareunia/PVD and control groups. More specifically, women in the vaginismus group would display the highest degree of pelvic floor muscle tension during the gynecological examination followed by women in the dyspareunia/PVD group and controls. Our third hypothesis was that genital pain would discriminate the clinical groups (vaginismus and dyspareunia/PVD) from controls, but would not distinguish vaginismus from dyspareunia/PVD. Overall, these data would provide systematic information as to whether the DSM-5 decision to collapse vaginismus and dyspareunia into one disorder was empirically justified.
Method
The present study was reviewed and approved by the University Faculty of Medicine Institutional Review Board; written informed consent was obtained from all study participants.
Participants
The participants included 50 women with vaginismus (33 lifelong type and 17 acquired type), 50 women suffering from dyspareunia/PVD (32 lifelong type and 18 acquired type), and 43 controls. The participants were primarily young (mean age = 25 years, range, 18–41), well educated (76 % had an undergraduate degree or more), born in North America (73 % in North America, 10 % in Asia, 9 % in Europe, 8 % elsewhere) and unmarried (27 % single, 56 % dating, 14 % married, and 3 % other). No significant differences between study groups were found on age, level of education, relationship status, birthplace, or religion. Significant differences between groups were found, however, on primary language, χ2(2, N = 143) = 12.17, p < .05, and cultural identity, χ2(2, N = 143) = 7.15, p < .05. A significantly higher percentage of women in the vaginismus group reported having a primary language other than French or English as compared with women in the dyspareunia/PVD and control groups. In addition, a significantly higher percentage of women in the vaginismus and control groups reported a cultural identity other than “Canadian” or “French Canadian” as compared to women in the dyspareunia/PVD group. No significant group differences were found, however, on any of the dependent variables between: (a) women with vaginismus who reported “French” as their primary language compared to women with vaginismus who reported “English” or “other language” as their primary language; (b) women with vaginismus reporting a “Canadian” or “French Canadian” culture compared to those reporting “other” as their cultural identity; or (c) controls reporting a “Canadian” and “French Canadian” culture compared to those reporting “other” as their cultural identity.
The inclusion criteria for vaginismus were based on those of Reissing et al.’s (2004) study and focused on the inability to achieve and avoidance of vaginal penetration: (a) never having been able to experience vaginal penetration (i.e., penile-vaginal intercourse or gynecological examination or tampon insertion), despite attempts on at least 10 separate occasions; (b) never having been able to experience vaginal penetration despite attempts on at least two separate occasions and demonstration of “active avoidance” of vaginal penetration; or (c) current inability to experience vaginal penetration and “active avoidance” of vaginal penetration for at least 1 year, despite having experienced vaginal penetration at least once before this period. Active avoidance was defined as an average of less than one attempt at vaginal intercourse every 2 months over the past year and meeting one of the following two criteria: (a) never successfully completing a gynecological examination, or (b) never having used tampons.
The inclusion criteria for dyspareunia/PVD were based on those of Bergeron et al. (2001): (a) pain occurring during intercourse on at least 80 % of all episodes; (b) pain at the entrance of the vagina, elicited by direct touch or pressure at the vestibule which has a burning or cutting quality; and (c) pain that is personally distressing and has been present for at least 6 months.
The inclusion criteria for the control group were the following: (a) current ability to experience vaginal penetration without difficulty and/or pain; and (b) no history of vulvar/vaginal/pelvic pain or penetration difficulties during intercourse, gynecological examination, or tampon insertion.
The exclusion criteria for all three groups were any of the following: (a) current pregnancy or breast-feeding; (b) post-menopausal status; (c) major medical conditions (e.g., endometriosis, cancer) or treatments (e.g., radiation therapy) which may affect the genital/pelvic area; and (d) current major psychiatric conditions (e.g., schizophrenia, bipolar disorder).
Measures
Psychophysiological Monitoring
An ambulatory monitor (TEL 100C, Harvard Apparatus Canada) was used for psychophysiological monitoring (electrocardiograms [ECG], electrodermal activity [EDR], and electromyography [EMG]) with data recorded on an MP100 system (Biopac Systems Inc. AcqKnowledge). ECG recordings were accomplished via electrodes (100/PK, EL 503) placed on the right lower abdominal region and below the left collarbone. EMG-recording electrodes (100/PK, EL 503) were placed on the right trapezius muscle. EDR-recording electrodes (100/PK, EL 507) were positioned with an electrode paste (Gel 101) on the distal phalanges of the left, middle, and ring fingers.
Self-Report Measures
A structured interview adapted from Reissing et al.’s (2004) study was administered to collect information on sociodemographic background and medical, gynecological, and relationship history. The Specific Phobia section of the Structured Clinical Interview (SCID-I; First, Spitzer, Gibbon, & Williams, 1997) was added to the interview with the aim of evaluating whether participants met the DSM-IV-TR diagnostic criteria for a specific phobia of vaginal penetration (American Psychiatric Association, 2000). Some of the SCID-I questions were modified by adding the words “fear of vaginal penetration” at appropriate places. The SCID-I is a semi-structured diagnostic interview designed to assist clinicians, researchers, and trainees in making reliable DSM-IV-TR psychiatric diagnoses.
The following standardized questionnaires with well-demonstrated reliability and validity were administered: (a) the McGill Pain Questionnaire (MPQ; Melzack & Katz, 1992) assessed the sensory and affective dimensions of the pain that participants experienced during the gynecological examination; (b) the Pain Catastrophizing Scale (PCS; Sullivan, Bishop, & Pivik, 1995) assessed the cognitive and emotional aspects (i.e. magnification, rumination, helplessness) of participants’ non-genital and genital pain; (c) the Fear Survey Schedule-II (FSS-II; Geer, 1966) assessed participants’ comorbid fears/phobias for non-gynecological/sexually related situations (e.g., social, blood/injury, death injury, animals/insects, agoraphobia); (d) the Fear of Pain Questionnaire-III (FPQ-III; McNeil & Rainwater, 1998) assessed the fear and anxiety associated with a variety of pain related situations (e.g., breaking your arm, getting an injection, being burned, etc.); and (e) the Trait and State subscales of the State Trait Anxiety Inventory (STAI; Spielberger, Gorsuch, & Lushene, 1970) assessed the presence of trait and situational anxiety to the gynecological examination.
In addition, two questionnaires, the Vaginal Penetration Survey (VPS) and the Sexual Disgust Sensitivity Index (SDSI), were developed by the authors in order to assess the degree of fear and disgust participants experienced with imagined or attempted vaginal penetration situations. The VPS was based on the FSS-II (Geer, 1966) and comprised 21 items referring to imagined or attempted vaginal penetration situations that may cause fear or unpleasant feelings (e.g., “When I imagine or try to engage in activities involving vaginal penetration such as intercourse or tampon insertion, I fear it will be painful” or “When I imagine or try to engage in activities involving vaginal penetration such as intercourse or tampon insertion, I fear that I will be unable to find the vaginal opening”). Participants were asked to evaluate on a 5-point scale how much they were disturbed by each item nowadays, with response options ranging from 0 (not at all) to 4 (very much). The SDSI was based on the Disgust Sensitivity Scale (Haidt, McCauley, & Rozin, 1994), which measures disgust sensitivity across seven domains: animals, body products, death, envelope violations (i.e., injuries, wounds, etc.), food, hygiene, and sex. The SDSI consists of 22 items referring to sexual objects, practices, and experiences that may cause disgust (e.g., sight and smell of vaginal secretions, smell of semen, performing oral sex). Participants were asked to evaluate on a 5-point scale how much they were disgusted by each item, with response options ranging from 0 (not at all) to 4 (very much). Copies of these questionnaires can be obtained from the corresponding author. In this study, all questionnaires except the STAI demonstrated a Cronbach’s alpha higher than .90. Cronbach’s alpha for the state sub-scale of the STAI (STAI-S) was .53 and for Trait subscale (STAI-T) was .22.
Pain Sensitivity Testing
Pain sensitivity testing was carried out with a vulvalgesiometer to measure deltoid and vulvar pain thresholds (Pukall, Binik, & Khalifé, 2004). Each participant was first familiarized with the vulvalgesiometer by experiencing sample pressures on the deltoid muscle of the right arm. Testing started with the lowest pressure exerted by the vulvalgesiometer (3 g) and consecutively higher pressures were applied after an inter-stimulus interval of 10 s. Non-painful and painful intensity, unpleasantness, and emotional distress ratings were recorded with each application. Testing stopped once the participant reported a minimal level of pain, defined as a self-report pain intensity rating of 2 on 10. The same protocol as described above was carried out at the 9 o’clock position and at the base of the hymeneal ring on the vulvar vestibule (e.g., entrance of the vagina).
Gynecological Examination
A standardized pelvic examination used in previous research (Bergeron et al., 2001; Meana, Binik, Khalifé, & Cohen, 1997) was carried out by the participating gynecologist. The first author or a trained female research assistant was also present during the gynecological examination. The protocol consisted of seven steps in the following order: (a) digital examination of the labia minora; (b) insertion of a cotton swab; (c) insertion of one finger; (d) palpation of the uterus and adnexa; (e) insertion of two fingers; (f) evaluation of pelvic muscle tension; and (g) cotton swab (Q tip) test at 3, 6, and 9 o’clock with the sequence of testing randomized. The cotton-swab test is the generally accepted gynecological examination for diagnosing PVD and consists of the application of a cotton-swab to different areas of the vulvar vestibule (Friedrich, 1987). During each step of the gynecological examination, participants were asked to rate if any pain or anxiety was experienced, and if so, to rate the intensity on a verbal analogue scale from 0 (no pain; no anxiety) to 10 (worst pain ever experienced; worst anxiety ever experienced). The gynecologist also separately rated the degree of difficulty of insertion on a 4-point scale from 0 (no problem) to 3 (impossible) of a cotton-swab, of one finger and of two fingers). Vaginal/pelvic muscle tone was evaluated using Lamont’s (1978) 6-point rating scale from 0 (normal tone) to 5 (perineal and levator ani contractions). The gynecologist also globally rated the degree of pelvic floor muscle tension displayed by participants during the gynecological examination on an 11-point rating scale from 0 (no tension) to 10 (strong tension).
Behavioral Measures of FEAR
During the gynecological examination, two behavioral measures indicative of fear were used. First, the gynecologist separately rated the level of defensive/avoidant reactions following the insertion of a Q-tip, following the insertion of one finger, and following the insertion of two fingers. Defensive/avoidant reactions were defined by Reissing et al. (2004) as behaviors interfering with, delaying, or terminating the examination and were rated on a 5-point scale from 0 (no problematic reaction during the examination) to 4 (the participant terminated the examination). Second, the participant’s face and body were filmed during the gynecological examination with a Canon Elura 80 Digital Camcorder in order to evaluate the frequency and intensity of displayed behavioral reactions of fear and pain. The recording of each participant’s exam was uploaded onto a computer and edited using iMovie software, before being burnt onto a DVD. Two trained research assistants who were blind to group membership independently viewed recordings on a MacBook laptop using QuickTime software and were asked to code the videos by following a checklist of eight categories of behaviors: (a) neck arching; (b) facial grimacing; (c) participant closing legs; (d) gynecologist having to open legs of participants; (e) pelvic withdrawal; (f) participants’ placing one or both hands on head; (g) verbal expressions (e.g., ahh, ouch, stop); and (h) paraverbal vocalizations (e.g., sigh or gasp). The above behaviors were separated in two main categories: protective behaviors and communicative behaviors. Protective behaviors included closing legs, pelvic withdrawal, and placing one or both hands on head while communicative behaviors included neck arching, facial grimacing, and verbal and paraverbal behaviors. Each behavior’s occurrence was coded in terms of its frequency and intensity on a 3-point scale: mild, moderate, or severe. This behavioral observation system was based on previously developed coding systems for laboratory pain and affective behavior studies (Ekman & Friesen, 1978; Keefe & Block, 1982; Prkachin, Hughes, Schultz, Joy, & Hunt, 2002; Sullivan, Adams, & Sullivan, 2004; Sullivan, Martel, Tripp, Savard, & Crombez, 2006). This system was adapted to the gynecological examination by viewing a sample of 80 women including women with vaginismus, dyspareunia/PVD, and controls undergoing a gynecological examination to record the behavioral reactions of fear and pain displayed.
The training of the raters started with a 3-h session during which the pain behavior definitions and coding procedure were reviewed and video clips were shown to illustrate the different categories of behaviors including the varying intensities. Raters began coding 5 h per week in addition to weekly/biweekly training sessions to increase inter-rater reliability. During the training sessions, non-eligible participant videos were watched with the researchers to discuss coding decisions with regards to the different behavior frequencies and intensities. Using a sample of 44 women meeting the criteria outlined above for vaginismus (n = 15), dyspareunia/PVD (n = 15), and controls (n = 14), the validity and reliability of the behavioral observation system was investigated. It was found to have high inter-rater reliability, good internal consistency, and good construct and discriminant validity. Inter-rater reliability was measured through the correlation of rater 1 and rater 2’s scores for the 44 participants, which were the total frequency and average intensity ratings for each behavior. The correlations regarding the frequency of behaviors were all over .8, ranging from r = .85 for verbal vocalizations (p < .001) to r = .99 for opening legs (p < .001). With regards to intensity ratings, the correlations were all above r = .7, with the exception of paraverbal vocalizations (r = .58, p < .001). Paired samples t tests were conducted to evaluate whether raters significantly differed in their coding of particular behaviors. No significant differences were found for 11 out of the 15 frequency and intensity ratings. Rater 2 scored significantly more behaviors than Rater 1 for neck arching frequency (t[43] = 2.12, p < .05), closing legs frequency (t[43] = 2.17, p < .05) and pelvic withdrawal frequency (t[43] = 5.37, p < .01) whereas Rater 1 scored significantly more instances of hands on head than Rater 2 (t[43] = 2.71, p = .01).
Internal consistency of the behavioral observation system was investigated through the correlation of each category of behavior with the total frequency of behavior scores (i.e., the co-investigator average of the overall number of pain behaviors for each participant). All correlations were significant (ps < .002), except for hands on head frequency (r = .21, p > .05) and intensity ratings (r = .29, p > .05). Discriminant validity was assessed through a one-way ANOVA examining whether the gynecologist’s diagnosis differed based on the amount of behaviors shown by each participant. Participants diagnosed with a sexual pain disorder (i.e., vaginismus or dyspareunia/PVD) demonstrated significantly more behaviors (M = 43.98, SD = 30.77) than controls (M = 9.88, SD = 8.07), F(1, 43) = 15.33, p < .001.
Procedure
Our sample was recruited via local media announcements, advertisements, and health professionals’ referral. Advertisements were aimed at women who were either experiencing “difficulties with vaginal penetration,” “pain with vaginal intercourse” or “no pain with intercourse.” Potential participants called our laboratory and were screened by the first author or a trained research assistant to insure their eligibility and to explain the study procedures including psychophysiological monitoring, a structured interview, questionnaire administration, gynecological examination, and pain threshold testing. During the telephone screening interview, potential participants described whether difficulties and/or pain were experienced with different vaginal penetration situations (tampon insertion, gynecological examination, and vaginal intercourse). If participants met the criteria for the vaginismus, dyspareunia/PVD, or control groups, an appointment for the experimental session was scheduled. If participants did not meet eligibility criteria for the study, appropriate referral information was given if requested.
The experimental session was carried out in the participating gynecologist’s office and lasted approximately 3–4 h. The study procedures were re-explained at the start of the session and written informed consent was obtained. Great care was taken throughout the session to maximize the comfort of the participant. Participants were informed that they could withdraw from the study at any time and receive full reimbursement for their time and participation. Participants were also allowed to control the timing of experimental procedures (e.g., to take a break if a specific procedure was painful or uncomfortable) or to not participate in a specific part of the experimental protocol. The first author or research assistant was present throughout the study and helped to minimize distress, if necessary, by reassurance, breathing exercises, explanations, etc. They also asked participants when appropriate if they wanted to take a break or not participate in a specific part of the protocol. The experimental session consisted of the following procedures in a standardized order: (a) placement of the ambulatory monitor for psychophysiological monitoring; (b) administration of the structured interview; (c) administration of the following standardized questionnaires: MPQ, PCS, SCID-I, FSS-II, FPQ, Spielberger Trait Anxiety Inventory; (d) deltoid pain sensitivity testing; (e) vestibular pain sensitivity testing; (f) gynecological examination; (g) re-administration of the MPQ with and PCS with respect to genital pain); and (h) removal of ambulatory monitoring equipment. Following these procedures, all participants, whether they completed the entire procedure or not were debriefed and offered relevant information concerning diagnosis and treatment. There was no further follow-up unless requested. All participants received $75 as compensation for their participation. There were no other explicit incentives to participate though it is our impression in this study and in other similar ones that women participate as a way of getting information and to facilitate coping with a situation they have avoided. The first author or a trained research assistant carried out all the experimental procedures except for the gynecological examination; one of them was also present during the gynecological examination. As a result, they were aware of the participants’ group membership and previous diagnoses; these, however, were not disclosed to the examining gynecologist.
Statistical Analysis
Differences between groups on completion rates of questionnaires and procedures as well as on socio-demographic and general health variables were analyzed using chi square analyses for discrete variables and ANOVAs for continuous variables. Tukey’s HSD post hoc tests were used to evaluate significant ANOVA results. Differences on gynecological examination pain dependent variables and on questionnaire data between lifelong and acquired vaginismus participants were analyzed using multiple t tests. Differences on questionnaire scores between those who completed the gynecological protocol and those who discontinued were analyzed using multiple t tests. Differences in pain thresholds between 3, 6, and 9 o’clock were analyzed using ANOVA.
Given the large number of dependent variables in the present study, fear, vaginal muscle tension, and genital pain total scores were computed. The fear total score was computed by taking the mean of the 43 standardized self-report, psychophysiological, and behavioral fear variables. The vaginal muscle tension total score was computed by taking the mean of the five standardized vaginal muscle tension variables, while the genital pain total score was computed by taking the mean of the 18 standardized genital pain variables. Group differences on these total scores were analyzed using ANOVAs followed by Tukey’s HSD post hoc tests.
Following the results of the above statistical analyses and to avoid redundancy, five separate principal components analyses (PCAs) with varimax rotation were performed on the following continuous measures: (a) 14 self-report fear measures (i.e., self-reported anxiety following each gynecological procedure and scores on the PCS, FPQ-III, FSS-II, VPS, SDS, STAI-S, and STAI-T); (b) eight psychophysiological measures of fear (i.e., heart rate, heart rate variability, mean EMG and EDR peaks taken during the pain sensitivity testing and gynecological examination); (c) 19 behavioral measures of fear (i.e., gynecologist’s rating of level of defensive/avoidant reactions during the insertion of a Q-tip, of one finger, and of two fingers; frequency and intensity of the eight categories of behavior from the behavioral observation system; number of protective and communicative behaviors); (d) 18 pain variables (i.e., self-reported pain intensities following each gynecological procedure, Present Pain Index and Pain Rating Index of the MPQ, deltoid and vulvar vestibule pain threshold); and (f) five vaginal muscle tension variables (i.e., scores on the Lamont scale; gynecologist’s rating of degree of muscle tension on an 11-point-rating scale; gynecologist’s rating of degree of difficulty inserting a Q-tip, one finger, and two fingers). The variables were standardized within groups to eliminate the influence of mean differences on the correlations. Missing data were replaced with the group mean. The criterion used to extract the factors (or components) from the PCA was having an eigenvalue greater than one. Component scores were calculated by totaling the variables, standardized across groups, which loaded highest on that particular component.
The components extracted from the PCA were entered into a stepwise discriminant function analysis to determine the most parsimonious set of components that could significantly separate the groups. The first analysis was conducted on the three groups (vaginismus, dyspareunia/PVD, and controls) using all components. To further investigate our fear hypothesis, a second discriminant analysis was conducted on the three groups using just the fear components. Finally, to examine which fear, vaginal muscle tension, and/or genital pain components could best distinguish vaginismus from dyspareunia/PVD, a third discriminant analysis was conducted on the vaginismus and dyspareunia groups using all components.
Finally, a taxometric analytic method, MAXCOV-HITMAX (Meehl, 1995), was used to explore whether differences between vaginismus and dyspareunia/PVD on fear, genital pain, and vaginal muscle tension were categorical (i.e., taxonic or discrete groups) or dimensional (i.e., continuous along a scale where the two poles represent the most extreme group differences) in nature. MAXCOV-HITMAX is a taxometric method that examines the maximum covariation between two variables as a function of a third. The sample is subdivided into a sequence of ordered subsamples based on their scores on the third variable. The covariance between the other two variables is then calculated for each of these subsamples. If the differences are dimensional in nature, the covariances will be randomly distributed around a single value resulting in a flat profile when plotted. If a categorical difference (i.e., taxonic) exists, the plot will be convex (an inverted U) where the covariances between two variables or more will vary as a function of a third. MAXCOV-HITMAX is generally computed on large samples (N > 300) since it involves dividing the sample into a set of ordered subsamples, each for its own analysis (Cole, 2004; Meehl, 1995). We, therefore, consider the results of our analyses exploratory. Cole (2004) suggested the use of a sliding window for the selection of subgroups with one subgroup overlapping an adjacent subgroup, when the sample sizes are small. Following Cole’s suggestion, the sample was divided into ten overlapping categories for fear, ten overlapping categories for genital pain, and five for pelvic floor muscle and covariances were calculated between the remaining two variables for each category. Cole’s suggestion was also attempted on twenty overlapping categories; however, the resulting graph did not help to clarify the taxonic structure.
Results
Differences Between Groups on Completion of Experimental Procedures
No significant differences were found between groups on willingness to undergo or finish the pain sensitivity testing or on completion of the following questionnaires: PCS with reference to general pain, VPS, SDS, FPQ-III, FSS-II, STAI-T, and STAI-S. Three women in the vaginismus group declined to undergo the vestibular pain sensitivity testing; none declined in the dyspareunia/PVD and control groups. Significant differences between groups were found, however, on willingness to complete all or part of the gynecological examination procedure, χ2(2, N = 143) = 36.86, p < .01 with a significantly higher number of women in the vaginismus group (n = 23) not completing at least one part of the gynecological examination as compared to three women in the dyspareunia/PVD group and one woman in the control group. The following number of women with vaginismus declined to participate in the specified portion of the gynecological examination procedure: (a) digital examination of the labia minora = 3; (b) insertion of the cotton swab = 6; (c) insertion of one finger = 6; (d) palpation of the uterus and adnexa = 14; (f) insertion of two fingers = 16; (g) evaluation of pelvic muscle tension = 12; and (h) cotton swab (Q tip) test at 3, 6, and 9 o’clock carried out in counterbalanced order = 14. Three women with PVD declined palpation of uterus and adnexa and three declined the cotton swab test. Four controls declined palpation of the uterus and adnexa and one declined the evaluation of pelvic muscle tension. Declining one part of the procedure did not necessarily result in declining all subsequent procedures though this was the general trend. As a result of this non-participation, significant differences between groups were found on completion of the MPQ, χ2(2, N = 143) = 8.66, p < .05 and PCS with reference to pain experienced during the gynecological examination, χ2(2, N = 143) = 9.77, p < .01 with a significantly higher number of women in the vaginismus group not completing these questionnaires. Controls who did not experience any pain during the gynecological examination could not be asked to complete the PCS with reference to the pain experienced during the gynecological examination.
We also investigated potential differences between lifelong and acquired vaginismus participants by carrying out multiple two-tailed t tests using a α = .05 criterion on the following dependent variables: pain sensitivity testing; vestibular pain threshold during cotton swab testing at 3, 6, and 9 o’clock; pain at insertion of cotton swab; pain at insertion of one and two fingers; pain during palpation of uterus and adnexae; pain during muscle palpation at 3, 6, and 9 o’clock; total scores on the DSI, VPS, FSS, FPQ, SSAIS, PCS gynecological pain score, and STAI. Of these 21 comparisons, only VPS total score was significantly different between lifelong and acquired vaginismus participants. In the same manner, we also investigated potential differences in questionnaire data for those who completed all parts of the protocol versus those who did not. There were no significant differences in any of these comparisons. We also separately investigated for vaginismus and dyspareunia/PVD participants’ potential threshold differences between 3, 6, and 9 o’clock using one-way ANOVAs with repeated measures. None of these ANOVAs yielded a significant effect.
Differences Between Groups on Fear, Genital Pain, and Vaginal Muscle Tension Total Scores
Fear Total Score
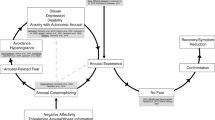
A one-way ANOVA revealed significant differences between groups on the fear total score, F(2, 140) = 87.63, p < .001 (see Fig. 1). Tukey’s HSD post hoc comparisons revealed that women in the vaginismus group had significantly higher mean scores than women in the dyspareunia and control groups (ps < .001) Women in the dyspareunia/PVD group also showed significantly higher mean scores on the fear total score than controls (p < .001).
Genital Pain Total Score
A one-way ANOVA revealed significant group differences on the genital pain total score, F(2, 140) = 62.96, p < .001 (see Fig. 1). Tukey’s HSD post hoc comparisons revealed that women in the vaginismus and dyspareunia/PVD groups had significantly higher mean scores than women in the control group (ps < .001). No significant group differences were found on the genital pain total score between the vaginismus and dyspareunia/PVD groups.
Vaginal Muscle Tension Total Score
A one-way ANOVA revealed significant group differences on the vaginal muscle tension total score, F(2, 140) = 27.47, p < .001 (see Fig. 1). Tukey’s HSD post hoc comparisons revealed that women in the vaginismus group had significantly higher mean scores than women in the dyspareunia/PVD and control groups (ps < .001). No significant group differences were found on the vaginal muscle tension total score between the dyspareunia/PVD and control groups.
To further examine the structure of between-group differences on fear, genital pain, and vaginal muscle tension, each participant was plotted according to their score on the combinations of the three factors taken two at a time (see Figs. 2, 3, and 4). The plots from Figs. 2, 3, and 4 suggest a large overlap between the vaginismus and dyspareunia/PVD groups on the fear and genital pain total scores. The plots from Figs. 3 and 4 further suggest that a subgroup of women in the vaginismus group scored highly on the vaginal muscle tension total score and differed from the remaining sample.
Differences Between Groups on the SCID-I
SCID-I (Specific Phobia)
Significant differences between groups were found on the number of women meeting the diagnostic criteria for a specific phobia of vaginal penetration, χ2(2, N = 143) = 19.66, p < .01, with a significantly higher number of women in the vaginismus (n = 19) and dyspareunia/PVD (n = 13) groups meeting the diagnosis compared to women in the control group (n = 0).
Data Reduction
The five PCAs extracted three components for self-report measures of fear, three components for psychophysiological measures of fear, six components for behavioral measures of fear, five components for genital pain, and two components for vaginal muscle tension (see Table 1).
Discrimination Between the Vaginismus, Dyspareunia/PVD, and Control Groups
A discriminant function analysis performed on all 17 components found that the vaginismus, dyspareunia/PVD, and control groups could be significantly discriminated by two standardized discriminant functions (Function 1: genital pain, and Function 2: vaginal muscle tension and protective behaviors). Using these functions, 72 % of women with vaginismus, 80 % of women with dyspareunia/PVD, and 93 % of women in the control group were correctly classified. Twenty-four percent of women in the vaginismus group were misclassified as dyspareunia/PVD, while 4 % were misclassified as controls. Sixteen percent of women in the dyspareunia/PVD group were misclassified as vaginismus and 4 % were misclassified as controls. No controls were misclassified as vaginismus and 7 % were misclassified as dyspareunia/PVD.
Genital pain (component 4, Table 1) had the highest loading (0.86) on function 1. Genital pain (component 4) comprised scores on the MPQ and self-reported pain intensities with the Q-tip test. Vaginal muscle tension (component 2, Table 1) had the highest loading (.56) on function 2. Vaginal muscle tension (component 2) consisted of the gynecologist’s rating of the degree of difficulty experienced inserting a cotton swab and inserting one finger. Behavioral measures of fear (component 3, Table 1) also loaded highly (.50) on function 2 and comprised the frequencies of behavioral measures of fear.
As can be seen in Fig. 2, function 1 (genital pain) discriminates well between women in the control group and women in the vaginismus and dyspareunia/PVD groups. Function 2 (vaginal muscle tension and protective behaviors) does not discriminate as well between women in the vaginismus, dyspareunia/PVD, and control groups. A large overlap can be observed between the vaginismus and dyspareunia/PVD groups on function 1 (genital pain) as well as between all three groups on function 2 (vaginal muscle tension and protective behaviors).
Discrimination Between Vaginismus, Dyspareunia/PVD, and Controls Based on Fear Measures Only
The discriminant analysis based on the fear variables included the three self-report fear components, the four behavioral fear components, and the three psychophysiological fear components. This analysis found that the vaginismus, dyspareunia/PVD, and control groups could be significantly discriminated by two standardized discriminant functions (function 1: behavioral and self-report measures of fear, and function 2: psychophysiological measures of fear). Using these functions, 74 % of women with vaginismus, 78 % of women with dyspareunia/PVD, and 90.7 % of women in the control groups were correctly classified. Fourteen percent of women in the vaginismus group were misclassified as dyspareunia/PVD and 12 % were misclassified as controls. Eighteen percent of women in the dyspareunia/PVD group were misclassified as vaginismus and 4 % were misclassified as controls. Regarding controls, 2.3 % were misclassified as vaginismus and 7 % were misclassified as dyspareunia/PVD.
Behavioral measures of fear (component 2 and 3, Table 1) and self-report measures of fear (component 2, Table 1) had the highest loadings (0.77, 0.58, and 0.62) on function 1 (behavioral and self-report measures of fear). Behavioral measures of fear component 2 were composed of the intensities of behavioral measures of fear while behavioral measures of fear component 3 comprised the frequencies of behavioral measures of fear. Self-report measures of fear component 2 was composed of scores on the DSI, VPS, FSS-II, FPQ-III, PCS (with reference to the gynecological examination) and the gynecologist’s rating of the participant’s degree of fear during the gynecological examination. Psychophysiological measures of fear (component 1 and 2, Table 1) had the highest loadings (−0.48, 0.46) on function 2 (psychophysiological measures of fear) and comprised heart rate and EMG taken during the gynecological examination and pain sensitivity testing.
As can be seen in Fig. 3, function 1 (behavioral and self-report measures of fear) discriminates well between women in the control group and women in the vaginismus and dyspareunia/PVD groups. Function 2 (psychophysiological measures of fear) does not discriminate as well between women in the vaginismus, dyspareunia/PVD, and control groups. Again, a large overlap can be observed between the vaginismus and dyspareunia/PVD groups on function 1 (behavioral and self-report measures of fear) as well as between all three groups on function 2 (psychophysiological measures of fear).
Discrimination Between Vaginismus and Dyspareunia/PVD
In an attempt to clarify the distinction between the two clinical groups, a discriminant analysis was performed on the vaginismus and dyspareunia/PVD groups without including the controls using all 17 components. The discriminant analysis was significant. Using this function, 78 % of women in the vaginismus group and 86 % of women in the dyspareunia/PVD group were correctly classified. Behavioral measures of fear (component 3, Table 1) and vaginal muscle tension (component 2, Table 1) had the highest loadings (0.58 and 0.55) on the discriminant function and consisted of the gynecologist’s rating of the degree of difficulty experienced while inserting a cotton swab and inserting one finger, and comprised the frequencies of behavioral measures of fear during the gynecological examination. Women in the vaginismus group scored higher on the behavioral measures of fear component 1 and on the vaginal muscle tension component 1 than women in the dyspareunia/PVD group.
Dimensional Versus Categorical Differences Between Vaginismus and Dyspareunia/PVD
The results of our exploratory taxometric analyses using the MAXCOV-HITMAX method on fear, vaginal muscle tension, and genital pain are illustrated in the three plots depicted in Fig. 4. As can be observed from the plotted covariations for both fear and vaginal muscle tension, the curves suggest a taxonic structure as a clearly defined peak can be observed on the right hand side of the graph. A similar but less clearly defined peak is observed for genital pain. More specifically, the plots appear to depict a group of women scoring in the upper 20th percentile of fear and vaginal muscle tension that is distinct from the remaining 80 % of women. This group comprised mainly women in the vaginismus group.
Discussion
Overall, the current findings supported all proposed hypotheses, and have important implications for the new DSM-5 diagnosis, genito-pelvic pain/penetration disorder. Consistent with our first hypothesis, fear, as measured by self-report, physiological, and behavioral measures was significantly greater in women suffering from vaginismus as compared to women suffering from dyspareunia/PVD, all of whom displayed significantly more fear than controls. The discriminant analyses demonstrated that behavioral measures of fear distinguished women suffering from vaginismus from those with dyspareunia/PVD and controls. Not only did women with vaginismus display greater fear during the gynecological examination, a significantly greater number were unwilling to undergo parts of the gynecological examination. These data support and extend Reissing et al.’s (2004) results by having measured fear on multiple dimensions as well as by using blinded raters and a standardized observational system to measure behavior during the gynecological examination. These findings also suggest that women suffering from vaginismus are either more fearful of vaginal penetration than women suffering from dyspareunia/PVD or use more avoidant coping strategies in response to attempted penetration, or both. Recent findings suggest that women suffering from vaginismus not only fear vaginal penetration situations, but also may have a general heightened fear/anxiety susceptibility (Borg, Peters, Weijmar Schultz, & de Jong, 2012; Cherner & Reissing, 2013; Nasab & Farnoosh, 2003; Watts & Nettle, 2010). Why this heightened susceptibility becomes focused on vaginal penetration remains unclear.
Consistent with our second hypothesis, pelvic floor muscle tension significantly distinguished women suffering from vaginismus from those with dyspareunia/PVD and from controls. This finding is consistent with Reissing et al.’s (2004) study using digital palpation to evaluate pelvic floor muscle tension. Results from studies using surface electromyography (sEMG) to measure pelvic floor muscle tension as the major measurement method are, however, inconsistent (Engman et al., 2004; Frasson et al., 2009; Reissing et al., 2004; Shafik & El-Sibai, 2002; van der Velde, 1999). These divergent findings may be secondary to limitations with sEMG methodology including placement variability, crosstalk, noise, and movement artifact (Gentilcore-Saulnier, McLean, Goldfinger, Pukall, & Chamberlain, 2009). Although results using digital palpation appear more consistent across studies, it should be emphasized that digital palpation remains a highly subjective assessment technique and may be influenced by the patient’s affective reaction such as fear and pain (Reissing et al., 2004). For instance, in the present study, women suffering from dyspareunia/PVD were not found to differ from controls on pelvic floor muscle tension; this result is inconsistent with several other studies (Engman et al., 2004; Gentilcore-Saulnier et al., 2009; Reissing et al., 2004). Morin, Bergeron, Khalifé, Mayrand, & Binik (2014) developed a pelvic floor muscle evaluation instrument (ultrasonography) to overcome some of these shortcomings. It is likely that in the future, ultrasonography will become an important method of assessing pelvic floor functioning in women with genito-pelvic pain since it does not require vaginal insertion and is relatively independent of subjective influence (Majida et al., 2009). This method has already been found useful in detecting pelvic floor muscle dysfunction in women suffering from dyspareunia/PVD as well as in men with chronic pelvic pain (Davis, Morin, Binik, Khalife, & Carrier, 2011; Morin et al., 2014). It is not clear whether situationally induced fear induces heightened pelvic floor muscle tension as part of a more “general defense reaction” (van der Velde et al., 2001) or whether pre-existing elevated levels of pelvic floor muscle tension increase susceptibility to vaginismus and dyspareunia/PVD or are the result of elevated fear/anxiety or both.
Our third hypothesis that women suffering from vaginismus like those suffering from dyspareunia/PVD experience significantly greater genital pain during attempted vaginal penetration than controls was also supported. This is consistent with several other studies demonstrating that a large percentage of women suffering from vaginismus also experience vulvar pain with attempted vaginal penetration and that this pain does not differ significantly in intensity, quality, or location from women with dyspareunia/PVD (Basson, 1996; de Kruiff et al., 2000; Engman et al., 2008; Reissing et al., 2004; ter Kuile, van Lankveld, Vlieland, Willekes, & Weijenborg, 2005). These findings suggest that the DSM-IV-TR clinical description of vaginismus was incomplete since the experience of genital pain was not emphasized. This further supports the notion that the differential diagnosis of dyspareunia/PVD from vaginismus based on the experience of genital pain may not be reliable.
Reissing et al. (2004) suggested that vaginismus could be conceptualized as a “vaginal penetration phobia.” In the DSM-IV, specific phobias are characterized by:
A marked and persistent fear that is excessive or unreasonable cued by the presence or anticipation of a specific object or situation. Exposure to the phobic stimulus almost invariably provokes an immediate anxiety response, which may take the form of a situationally bound or situationally predisposed panic attack. The person recognizes that the fear is excessive or unreasonable. The phobic situation(s) is avoided or else endured with intense anxiety or distress” (American Psychiatric Association, 2000, p. 449).
Self-report, behavioral, and psychophysiological measures demonstrated significant fear and avoidance in women with vaginismus during the gynecological examination suggesting that women with vaginismus have several characteristics in common with individuals suffering from a specific phobia. One problem with characterizing women with vaginismus as phobic is that over a third of women in our sample did not believe that their “fear was excessive or unreasonable” and therefore did not meet the diagnostic criteria for a specific phobia of vaginal penetration. The current DSM-5 definition replaces this criterion of “excessive or unreasonable fear” with the criterion of “fear or anxiety is out of proportion to the actual danger posed by the specific object or situation.” We believe that use of this new criterion would result in many more women with vaginismus also meeting the diagnostic criteria for phobia. Conceptualizing vaginismus as a specific phobia may be useful therapeutically as indicated by a recent studies using exposure as a primary treatment (ter Kuile et al., 2009; ter Kuile, Melles, de Groot, Tuijnman-Raasveld, & van Lankveld, 2013).
This characterization, however, may have some disadvantages. For example, defining vaginismus as a specific phobia may lead to ignoring other potentially important symptoms such as genital pain and pelvic floor muscle tension. In addition, differences in fear of vaginal penetration between women suffering from vaginismus and those with dyspareunia/PVD may not only be related to the degree of fear but also to the use of different coping styles (Borg, Peters, Weijamar Schultz, & de Jong, 2012). Future studies should further investigate whether differences exist between women suffering from vaginismus and dyspareunia/PVD on their primary appraisal of vaginal penetration situations as well as on their coping response to stressful events in general. The idea that women with vaginismus have different appraisal styles with respect to vaginal penetration situations is supported by recent work on the development of the Vaginal Penetration Cognition Questionnaire (Klaassen & ter Kuile, 2009).
Overall, results from this study only partially support the DSM-5 decision to collapse vaginismus and dyspareunia into one category named “genito-pelvic pain/penetration disorder.” Our findings demonstrate that fear and pelvic floor muscle tension can statistically distinguish women suffering from vaginismus from those with dyspareunia/PVD. The preliminary taxometric analyses also suggest that a small subgroup of women suffering from vaginismus appear to be categorically different from the remaining women with vaginismus as well as from women suffering from dyspareunia/PVD. However, these analyses also suggest that the structure of the differences on fear, pelvic floor muscle tension, and genital pain appear to be dimensional for the majority of women suffering from vaginismus and dyspareunia/PVD. Although computationally heavy statistical procedures are capable of distinguishing vaginismus from dyspareunia/PVD based on fear and pelvic floor muscle tension variables, this task is not likely feasible for health professionals in a clinical setting. In fact, clinical research has confirmed that health professionals do not succeed in reliably distinguishing these conditions (Engman et al., 2007, 2008; Reissing et al., 2004; ter Kuile et al., 2005). This is not surprising given the large overlap observed in Figs. 2 and 3 between both conditions on several dimensions.
Collapsing vaginismus and dyspareunia into the DSM-5 category of genito-pelvic pain/penetration disorder has certain advantages, however, such as increasing diagnostic reliability and forcing clinicians to carefully assess all the relevant dimensions of vaginismus and dyspareunia/PVD (i.e., vaginal penetration, genital pain, fear, and pelvic floor muscle dysfunction). The new category also does not rely on the invalid criterion of vaginal spasm. The use of this new diagnosis would hopefully motivate multidisciplinary teams including gynecologists, sex therapists, and pelvic floor physiotherapists to be involved in the assessment and treatment of vaginismus and dyspareunia/PVD. On the other hand, this new category may blur the search for possible differences and treatments specific to one of the four diagnostic dimensions.
The present study has several limitations. First, the sample size (n = 43–50 per group) for the three groups was relatively small and may have resulted in inadequate power to detect important differences or to adequately exploit taxometric methodology. Second, a significant number of women in the vaginismus group discontinued parts of the gynecological examination. There is no ethical way of circumventing this problem since by definition women with vaginismus will not participate in some penetration procedures. The missing data from these women were replaced by the means of the group in which the participant was categorized. This method of dealing with missing values can be considered a very conservative strategy, as it is highly likely that women who discontinued the gynecological examination would have displayed greater fear and pelvic floor muscle tension during the gynecological examination. Third, the participants were unlikely to have been a representative sample of women suffering from vaginismus in the general population. Those fearing and avoiding vaginal penetration situations the most might be the least likely to participate in a study involving a gynecological examination. On the other hand, some women highly fearful of penetration situations told us that they participated in this study because they felt that a research situation would provide them with the best opportunity to overcome their fears. Overall, this selection issue has been a problem common to most research and clinical studies of vaginismus since until recently a pelvic examination was required to make a diagnosis. Fourth, our analyses were based primarily on results from an attempted gynecological examination. Difficulties with or the inability to experience a gynecological examination are highly correlated with difficulties with or inability to experience intercourse but they are not identical. Fifth, our sample included women with both lifelong and acquired vaginismus. Several research groups have limited their samples to those with lifelong problems implying that lifelong and acquired groups are distinct syndromes (see Reissing et al., 2014). In our view, there is not a substantial body of empirical or theoretical evidence to support this view and it ignores approximately one third of currently diagnosable women (for a discussion, see Binik, 2014). In this study, we found no systematic differences on dependent variables between lifelong and acquired vaginismus. Finally, the dyspareunia group included only women suffering from PVD. A more heterogeneous sample of women suffering from dyspareunia may have resulted in different results and greater discrimination between the vaginismus and dyspareunia groups. Finally, although the gynecologist centered methods for evaluating pelvic floor muscle tension and spasm have been the standard for over 150 years, they are potentially overly sensitive to subjective influence.
In conclusion, although measures of fear and pelvic floor muscle tension were able to discriminate vaginismus from dyspareunia/PVD, our findings also suggest a large overlap between both conditions on these dimensions and on the dimension of genital pain. The unwillingness to experience/attempt vaginal penetration appears to be the single best differentiator of vaginismus from dyspareunia/PVD, but this may be a function of fear and associated coping styles. Translating these findings into reliable and valid diagnostic criteria for clinicians still remains a challenge.
References
American Congress of Obstetricians and Gynecologists. (1995). ACOG technical bulletin: Sexual dysfunction. International Journal of Gynecology and Obstetrics, 51(3), 265–277. doi:10.1016/0020-7292(95)80034-4
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: Author.
Basson, R. (1996). Lifelong vaginismus: A clinical study of 60 consecutive cases. Journal of the Society of Obstetricians and Gynecologists of Canada, 18, 551–561. Retrieved from http://sogc.org/jogc-digital/
Basson, R., Leiblum, S., Brotto, L., Derogatis, L., Fourcroy, J., Fugl-Meyer, K., … Weijmar Schultz, W. (2004). Revised definitions of women’s sexual dysfunction. Journal of Sexual Medicine, 1(1), 40–48. doi:10.1111/j.1743-6109.2004.10107.
Bergeron, S., Binik, Y. M., Khalifé, S., Pagidas, K., Glazer, H. I., Meana, M., et al. (2001). A randomized comparison of group cognitive-behavioral therapy, surface electromygraphic biofeedback, and vestibulectomy in the treatment of dyspareunia resulting from vulvar vestibulitis. Pain, 91(3), 297–306. doi:10.1016/S0304-3959(00)00449-8.
Binik, Y. M. (2010a). The DSM diagnostic criteria for dyspareunia. Archives of Sexual Behavior, 39, 278–291. doi:10.1007/s10508-009-9563-x.
Binik, Y. M. (2010b). The DSM diagnostic criteria for vaginismus. Archives of Sexual Behavior, 39, 292–303. doi:10.1007/s10508-009-9560-0.
Binik, Y. M. (2014). Will vaginismus remain a “lifelong” baby? Response to Reissing et al. (2014). Archives of Sexual Behavior, 43, 1215–1217. doi:10.1007/s10508-014-0336-9.
Borg, C., Peters, M. L., Weijmar Schultz, W., & de Jong, P. J. (2012). Vaginismus: Heightened harm avoidance and pain catastrophizing cognitions. Journal of Sexual Medicine, 9(2), 558–567. doi:10.1111/j.1743-6109.2011.02535.x.
Cherner, R. A., & Reissing, E. D. (2013). A comparative study of sexual function, behavior, and cognitions of women with lifelong vaginismus. Archives of Sexual Behavior, 42, 1605–1614. doi:10.1007/s10508-013-0111-3.
Cole, D. A. (2004). Taxometrics in psychopathology research: An introduction to some of the procedures and related methodological issues. Journal of Abnormal Psychology, 113(1), 3–9. doi:10.1037/0021-843X.113.1.3.
Davis, S. N. P., Morin, M., Binik, Y. M., Khalife, S., & Carrier, S. (2011). Use of pelvic floor ultrasound to assess pelvic floor muscle function in urological chronic pelvic pain syndrome in men. Journal of Sexual Medicine, 8(11), 3173–3180. doi:10.1111/j.1743-6109.2011.02452.x.
de Kruiff, M. E., ter Kuile, M. M., Weijenborg, P. T., & van Lankveld, J. J. (2000). Vaginismus and dyspareunia: Is there a difference in clinical presentation? Journal of Psychosomatic Obstetrics and Gynecology, 21(3), 149–155. doi:10.3109/01674820009075622.
Ekman, P., & Friesen, W. (1978). Facial action coding system: A technique for the measurement of facial movement. Palo Alto, CA: Consulting Psychologists Press.
Engman, M. (2007). Partial vaginismus–definition, symptoms and treatment. Unpublished doctoral dissertation, Linkoping University, Linkoping, Sweden.
Engman, M., Lindehammar, H., & Wijma, B. (2004). Surface electromyography diagnostics in women with partial vaginismus with or without vulvar vestibulitis and in asymptomatic women. Journal of Psychosomatic Obstetrics and Gynecology, 25(3–4), 281–294. doi:10.1080/01674820400017921.
Engman, M., Wijma, K., & Wijma, B. (2007). Itch and burning pain in women with partial vaginismus with or without vulvar vestibulitis. Journal of Sex and Marital Therapy, 33(2), 171–186. doi:10.1080/00926230601098506.
Engman, M., Wijma, B., & Wijma, K. (2008). Post-coital burning pain and pain at micturition: Early symptoms of partial vaginismus with or without vulvar vestibulitis? Journal of Sex and Marital Therapy, 34(5), 413–428. doi:10.1080/00926230802156210.
First, M., Spitzer, R., Gibbon, M., & Williams, J. B. (1997). Structured clinical interview for DSM-IV axis I disorders (SCID-I). New York: Biometric Research Department.
Foster, D. C., Kotok, M. B., Huang, L. S., Watts, A., Oakes, D., Howard, F. M., … Dworkin, R. H. (2010). Oral desipramine and topical lidocaine for vulvodynia: A randomized controlled trial. Obstetrics and Gynecology, 116(3), 583–593. doi:10.1097/AOG.0b013e3181e9e0ab
Frasson, E., Grazziotin, A., Priori, A., Dall’Ora, E., Didone, G., Garbin, E. L., & Bertolasi, L. (2009). Central nervous system abnormalities in vaginismus. Clinical Neurophysiology, 120(1), 117–122. doi:10.1016/j.clinph.2008.10.156.
Friedrich, E. G. (1987). Vulvar vestibulitis syndrome. Journal of Reproductive Medicine, 32, 110–114.
Geer, R. (1966). Development of a scale to measure fear. Behaviour Research and Therapy, 3(1), 45–53. doi:10.1016/0005-7967(65)90040-9.
Gentilcore-Saulnier, E., McLean, L., Goldfinger, C., Pukall, C. F., & Chamberlain, S. (2009). Pelvic floor muscle assessment outcomes in women with and without provoked vestibulodynia and the impact of a physical therapy program. Journal of Sexual Medicine, 7(2 Pt 2), 1003–1022. doi:10.1111/j.1743-6109.2009.01642.x.
Haidt, J., McCauley, C., & Rozin, P. (1994). Individual differences in sensitivity to disgust: A scale sampling seven domains of disgust elicitors. Personality and Individual Differences, 16(5), 701–713. doi:10.1016/0191-8869(94)90212-7.
Kaplan, H. S. (1974). The new sex therapy. New York: Brunner/Mazel.
Keefe, F. J., & Block, A. R. (1982). Development of an observation method for assessing pain behavior in chronic low back pain patients. Behavior Therapy, 13(4), 363–375. doi:10.1016/s0005-7894(82)80001-4.
Klaassen, M., & ter Kuile, M. M. (2009). Development and initial validation of the Vaginal Penetration Cognition questionnaire (VPCQ) in a sample of women with vaginismus and dyspareunia. Journal of Sexual Medicine, 6(6), 1617–1627. doi:10.1111/j.1743-6109.2009.01217.x.
Lahaie, M. A., Boyer, S. C., Binik, Y. M., Amsel, R., & Khalifé, S. (2010). Vaginismus: A review of the literature on the classification/diagnosis, etiology, and treatment. Women’s Health, 6(5), 705–719. doi:10.2217/whe.10.46.
Lamont, J. A. (1978). Vaginismus. American Journal of Obstetrics and Gynecology, 131(6), 633–636. Retrieved from http://www.ajog.org/
Landry, T., Bergeron, S., Dupuis, M. J., & Desrochers, G. (2008). The treatment of provoked vestibulodynia: A critical review. Clinical Journal of Pain, 24(2), 155–171. doi:10.1097/AJP.0b013e31815aac4d.
Majida, M., Braekken, I. H., Umek, W., Bo, K., Saltyte Benth, J., & Ellstrom Engh, M. (2009). Interobserver repeatability of three- and four-dimensional transperineal ultrasound assessment of pelvic floor muscle anatomy and function. Ultrasound in Obstetrics and Gynecology, 33(5), 567–573. doi:10.1002/uog.6351.
Masters, W. H., & Johnson, V. E. (1970). Human sexual inadequacy. London: Little, Brown.
McNeil, D. W., & Rainwater, A. J. (1998). Development of the Fear of Pain questionnaire-III. Journal of Behavioral Medicine, 21(4), 389–410. doi:10.1023/A:1018782831217.
Meana, M., Binik, Y. M., Khalifé, S., & Cohen, D. (1997). Dyspareunia: Sexual dysfunction or pain syndrome? Journal of Nervous and Mental Disease, 185(9), 561–569. doi:10.1097/00005053-199709000-00005.
Meehl, P. E. (1995). Bootstraps taxometrics: Solving the classification problem in psychopathology. American Psychologist, 50(4), 266–275. doi:10.1037/0003-066X.50.4.266.
Melzack, R., & Katz, J. (1992). The McGill Pain questionnaire: Appraisal and current status. In D. C. Turk & R. Melzack (Eds.), Handbook of pain assessment (pp. 152–164). New York: Guilford.
Merskey, H., & Bogduk, N. (1994). Classification of chronic pain (2nd ed.). Washington, DC: IASP Press.
Morin, M., Bergeron, S., Khalifé, S., Mayrand, M., & Binik, Y. M. (2014). Morphometry of the pelvic floor muscles in women with and without provoked vestibulodynia using real time 4D ultrasound. Journal of Sexual Medicine, 11(3), 776–785. doi:10.1111/jsm.12367.
Nasab, M., & Farnoosh, Z. (2003). Management of vaginismus with cognitive-behavioral therapy, self-finger approach: A study of 70 cases. Iranian Journal of Basic Medical Sciences, 28, 69–71. Retrieved from http://www.mums.ac.ir/basic_medical/en/index.
Prkachin, K. M., Hughes, E., Schultz, I., Joy, P., & Hunt, D. (2002). Real-time assessment of pain behavior during clinical assessment of low back pain patients. Pain, 95(1–2), 23–30. doi:10.1016/S0304-3959(01)00369-4.
Pukall, C. F., Binik, Y. M., & Khalifé, S. (2004). A new instrument for pain assessment in vulvar vestibulitis syndrome. Journal of Sex and Marital Therapy, 30(2), 69–78. doi:10.1080/00926230490275065.
Reissing, E. D., Binik, Y. M., Khalifé, S., Cohen, D., & Amsel, R. (2004). Vaginal spasm, pain, and behavior: An empirical investigation of the diagnosis of vaginismus. Archives of Sexual Behavior, 33(1), 5–17. doi:10.1023/B:ASEB.0000007458.328.52.c8.
Reissing, E. D., Borg, C., Spoelstra, S. K., ter Kuile, M. M., Both, S., de Jong, P. J., … Weijmar Schultz, W. C. M. (2014). “Throwing the baby out with the bathwater”: The demise of vaginismus in favor of genito-pelvic pain/penetration disorder. Archives of Sexual Behavior, 43, 1209–1213. doi:10.1007/s10508-014-0322-2.
Shafik, A., & El-Sibai, O. (2002). Study of the pelvic floor muscles in vaginismus: A concept of pathogenesis. European Journal of Obstetrics, Gynecology, and Reproductive Biology, 105, 67–70. doi:10.1016/S0301-2115(02)00115-X.
Sims, J. M. (1861). On vaginismus. Transactions of the Obstetrics Society of London, 3, 356–367.
Spielberger, C. D., Gorsuch, R. L., & Lushene, R. E. (1970). STAI manual for the state-trait anxiety inventory. Palo Alto, CA: Consulting Psychologist Press.
Sullivan, M. J., Adams, H., & Sullivan, M. E. (2004). Communicative dimensions of pain catastrophizing: Social cueing effects on pain behaviour and coping. Pain, 107(3), 220–226. doi:10.1016/j.pain.2003.11.003.
Sullivan, M. J. L., Bishop, S., & Pivik, J. (1995). The Pain Catastrophizing scale: Development and validation. Psychological Assessment, 7(4), 524–532. doi:10.1037/1040-3590.7.4.524.
Sullivan, M. J., Martel, M. O., Tripp, D., Savard, A., & Crombez, G. (2006). The relation between catastrophizing and the communication of pain experience. Pain, 122(3), 282–288. doi:10.1016/j.pain.2006.02.001.
ter Kuile, M., van Lankveld, J., Vlieland, C. V., Willekes, C., & Weijenborg, P. T. M. (2005). Vulvar vestibulitis syndrome: An important factor in the evolution of lifelong vaginismus? Journal of Psychosomatic Obstetrics & Gynecology, 26(4), 245–249. doi:10.1080/01674820500165935.
ter Kuile, M. M., Bulté, I., Weijenborg, P. T. M., Beekman, A., Melles, R., & Onghena, P. (2009). Therapist-aided exposure for women with lifelong vaginismus: A replicated single case design. Journal of Consulting and Clinical Psychology, 77(1), 149–159. doi:10.1037/a0014273.
ter Kuile, M. M., Melles, R., de Groot, H. E., Tuijnman-Raasveld, C. C., & van Lankveld, J. J. D. M. (2013). Therapist-aided exposure for women with lifelong vaginismus: A randomized waiting-list control trial of efficacy. Journal of Consulting and Clinical Psychology, 81(6), 1127–1136. doi:10.1037/a0034292.
van der Velde, J. (1999). A psychophysiological investigation of the pelvic floor: The mechanism of vaginismus. Unpublished doctoral dissertation, University of Amsterdam.
van der Velde, J., Laan, E., & Everaerd, W. (2001). Vaginismus, a component of a general defensive reaction. An investigation of pelvic floor muscle activity during exposure to emotion-inducing film excerpts in women with and without vaginismus. International Urogynecology Journal and Pelvic Floor Dysfunction, 12(5), 328–331. doi:10.1007/s001920170035.
van Lankveld, J. J., Brewaeys, A. M., ter Kuile, M. M., & Weijenborg, P. T. (1995). Difficulties in the differential diagnosis of vaginismus, dyspareunia and mixed sexual pain disorder. Journal of Psychosomatic Obstetrics and Gynecology, 16(4), 201–209. doi:10.3109/01674829509024470.
van Lankveld, J. J., ter Kuile, M. M., de Groot, H. E., Melles, R., Nefs, J., & Zandbergen, M. (2006). Cognitive-behavioral therapy for women with lifelong vaginismus: A randomized waiting-list controlled trial of efficacy. Journal of Consulting and Clinical Psychology, 74(1), 168–178. doi:10.1037/0022-006X.74.1.168.
Walthard, M. (1909). Die psychogene aetiologie und die psychotherapie des vaginismus. Muenchener Medizinische Wochenschschrift, 56, 1997–2000.
Ward, E., & Ogden, J. (1994). Experiencing vaginismus sufferers’ beliefs about causes and effects. Sexual and Marital Therapy, 9(1), 33–45. doi:10.1080/02674659408409565.
Watts, G., & Nettle, D. (2010). The role of anxiety in vaginismus: A case-control study. Journal of Sexual Medicine, 7(1 Pt 1), 143–148. doi:10.1111/j.1743-6109.2009.01365.x
World Health Organization. (1992). Manual of the international statistical classification of diseases, injuries, and causes of death (10th ed.). Geneva: Author.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lahaie, MA., Amsel, R., Khalifé, S. et al. Can Fear, Pain, and Muscle Tension Discriminate Vaginismus from Dyspareunia/Provoked Vestibulodynia? Implications for the New DSM-5 Diagnosis of Genito-Pelvic Pain/Penetration Disorder. Arch Sex Behav 44, 1537–1550 (2015). https://doi.org/10.1007/s10508-014-0430-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10508-014-0430-z