Abstract
Accumulating evidence has shown that binge-type alcohol intake in mothers interferes with thiamine deficiency (TD) to promote the fetal alcohol syndrome (FAS). Developmental alcohol or TD exposures act either synergistically or separately to reproduce FAS features e.g. intrauterine growth retardation and related microcephaly characterized by extensive cellular death induced by one another neurotoxicant. However molecular and cellular mechanisms underlying apoptosis in both alcohol and TD toxicities are unknown. The current review addresses mechanisms of apoptosis underlying alcohol and TD toxicities for further understanding FAS pathology. This study indicates two different mitochondria pathways regulating cellular death: The first mechanism may engage alcohol which activates the c-subunit ring of the F0-ATP synthase to form MPT pore-dependent apoptosis; following the second mechanism, TD activates CyP-D translocation from mitochondrial matrix towards the mitochondrial inner membrane to form MPT pore-dependent necrosis. These studies shed light upon molecular and cellular mechanisms underlying apoptosis and necrosis in developemental brain disorders related to alcohol and thiamine deficiency, in hopes of developing new therapeutic strategies for FAS medication.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alcohol is a potent teratogen in humans, and prenatal alcohol exposure is a leading cause of intrauterine growth retardation and related microencephaly, brain damage often manifested by intellectual disability and behavioral disorders [1, 2]. Maternal alcohol use is often concurrent with other factors that pose a risk to the developing fetal brain such as poor nutrition and nutrient factors deficits. In particular, thiamine deficiency (TD) is frequently concomitant with chronic alcoholic diseases [3–6]. However, TD is more efficient than alcohol, in retarding both intrauterine and postnatal growths, inducing microencephaly, delaying cellular differentiation, disrupting axogenesis, synaptogenesis and damaging neural tissues [7–10]. This does not preclude both teratogen agents to exert synergistic deleterious actions on fetal brain and body development [7, 11]. Results of our previous studies suggest that in the fetal alcohol syndrome, alcohol provokes cellular atrophy and death by induction of B1 vitamin (thiamine) deficiency [12, 13]. Indeed, fetal brain exposure to thiamine deficiency increases oxidative stress and exacerbates neuroapoptosis, thereby impairing neuronal function and behavior [7, 10, 14].
Programmed cell death plays critical roles in a wide variety of physiological processes during fetal development and in adult tissues. In most cases, physiological cell death occurs by apoptosis as opposed to necrosis [15, 16]. Mitochondrial permeability transition plays a critical role in both apoptotic and necrotic cellular death [17]. The term “mitochondrial permeability transition (MPT)” refers to an abrupt increase in the permeability of the outer/inner mitochondrial membrane. Due to osmotic forces, MPT causes a massive influx of water into mitochondrial matrix, triggering the structural collapse of the organelle [16, 18] followed by the release of cytochrome c and pro-apoptotic proteins, which then translocate from the intermembrane space of the mitochondria into the cytosol [19]. In the cytosol, cytochrome c activates the caspase cascade (initiator: caspase 9 and effectors: caspases 3, 6, 7). Activation of one caspase by another constitutes the caspase cascade leading to cellular death [20]. MPT pore opening is regulated in different ways depending on the cell type, cytotixic agent and oxidative stress [21]. For instance, neurotoxicant-induced prolonged mitochondrial permeability transition results in a drastic ATP synthesis inhibition through the oxidative phosphorylation uncoupling and a marked increase in reactive oxygen species (ROS) production [22, 23]. On the one hand, the molecular machinery responsible for apoptosis has been well elucidated. Indeed, the mitochondria-dependent pathway for apoptosis is governed by Bcl-2 family proteins. Both pro-(Bak, Bax and Bid) and anti-apoptotic (Bcl-2, Mcl-1, Bcl-XL, A1 and Bcl-w) Bcl-2 family proteins exist, and many of these proteins physically bind each other, forming channel-like proteins by spatial disposition of pore-forming domains [15, 24]. When these proteins are tested, including Bcl-2, Bcl-XL, Bax and Bid, they have all been shown to form ion-conducting channels in synthetic membranes in vitro [25, 26], and are directly involved in the permeabilization of the mitochondrial outer membrane [27, 28]. Thus, the Bcl-2 family proteins induce the mitochondrial permeability transition (MPT) triggering apoptic cellular death. On the other hand, the mitochondria-dependent pathway for necrotic cellular death is only emerging and requires further investigation. Recently, Ying and Padanilam [29] reported that necrotic cell death can also be a regulated process. Necrosis regulation includes multiple cell death modalities such as necroptosis, parthanatos, ferroptosis, pyroptosis, and MPT pore-mediated necrosis. Opening of the MPT pore-mediated necrosis results in loss of mitochondrial inner membrane potential, disruption of ATP production, increased ROS production, organelle swelling, mitochondrial dysfunction and subsequent necrosis [29]. Cyclosporine-A treatment, a potent inhibitor of CypD, led to significant reduction in necroptosis markers, RIP1 and RIP3 [30]. In addition, anti-necroptosis chemical necrostatin-1 can also suppress apoptotic pathway to exert neuroprotection [31]. The MPT pore complex mediating necrotic cellular death is composed of at least three primary components, including the voltage-dependant anion channel, the adenine nucleotide translocator-1, and the mitochondrial matrix protein cyclophilin D (CyPD), [32–34]. Cyp-D is the only cyclophilin resident in mitochondria. It is nuclearly encoded by the Ppif gene and imported into the mitochondrial matrix where it regulates the threshold for opening MTP pore [35]. CyPD is known to sit in mitochondrial matrix to keep the MPT pore closed [36, 37]. Metabolic stress conditions, i.e. increased Ca2+ and ROS induced p53 translocation into mitochondrial matrix, where it forms a complex with cyclophilin-D followed by CyP-D translocation from mitochondrial matrix towards the mitochondrial inner membrane to form MPT pore-dependent necrosis programming; anti-oxidants inhibited p53 translocation and MPT pore opening [34, 38]. Moreover, increased abundance of cyclophilin-D within mitochondrial membranes enhances mitochondrial vulnerability to stress [39], whereas Knockout of cyclophilin D in Ppif−/− mice increases stability of brain mitochondria against Ca2+ stress [40].
Recent data indicate that F1F0-ATP synthase, a large protein embedded in the inner mitochondrial membrane forms MPT pore-dependent apoptosis. The function of ATP synthase is to synthesize ATP from ADP and inorganic phosphate (Pi) in the F1 sector (Fig. 1). Energy for ATP synthesis derived from a gradient of protons which cross the inner mitochondrial membrane from the intermembrane space into the matrix through the membrane-embedded F0 sector [41]. The proton gradient establishes an electrical membrane potential (Δψm). ATP synthase can also reverse and hydrolyze ATP to generate a proton gradient [42]. The emerging consensus is that the enzyme is constructed as two rotary motors, one in the F1 part in which γ/ε subunits undergo catalytic rotation for ATP synthesis, and the other in the F0 part where protons transport trough the c-subunit ring induces rotation of the later, producing an energy transferred to F1 moving sector for its catalytic rotation [41, 43]. Although essential for ATP production by mitochondria, recent findings have confirmed that the c-subunit of the ATP synthase also houses a large conductance uncoupling channel, the mitochondrial permeability transition pore (MPT pore), the persistent opening of which produces osmotic dysregulation of the inner mitochondrial membrane and cell death [44]. Thus, F0 sector can form a high-conductance voltage-dependent channel [45], because highly purified c subunit, a membrane-embedded F0 component, self-assembles into annular structures embedded within liposome bilayer [46, 47]. The c-subunit ring of the F0 is a candidate for the mitochondrial MPT pore. Conversely, another theory suggests that reconstituted dimers of the F1F0-ATP synthase form a channel with properties identical to those of the mitochondrial megachannel, the electrophysiological equivalent of the MPT pore [48, 49]. Consequently, ATP synthase may be a major target for the pathogenesis of both chronic alcohol and thiamine deficiency related to permanent mitochondrial energy production failure.
Schema of the structure of human mitochondrial F1F0-ATP synthase or complex V, adapted from Jonckheere et al. [77]. ATP synthase, consists of two functional domains, F1 and F0. F 1 comprises 5 different subunits (three α, three β, and one γ, δ and ε) and is situated in the mitochondrial matrix. F0 contains subunits c, a, b, d, F6, OSCP and the accessory subunits A6L (including also e, f, g subunits which were not represented). Subunits c, a, b, A6L of F0 sector are spanning the membrane. F1 subunits γ, δ and ε constitute the central stalk of complex V. Subunits b, d, F6 and OSCP form the peripheral stalk. Protons pass from the intermembrane space to the matrix through F0, which transfers the energy created by the proton electrochemical gradient to F1 [77]. Precisely, protons pass F0 via subunit a to the c-ring. The released energy causes rotation of two rotary motors: the ring of c subunits in F0 (relative to subunit a), along with subunits γ, δ and ε in F1 to which it is attached. Rotation of subunit γ within the F1 α3β3 hexamer provides energy for ATP synthesis. This is called “rotary catalysis”. There are three catalytic sites, situated at interfaces of α- and β-subunits, where ATP is synthesized and hydrolyzed [77]
In animal models of FAS, both alcohol and TD induced either apoptic or necrotic cellular death [50]. However, molecular mechanisms underlying alcohol and TD-triggered MPT pore opening are unknown. For instance, ethanol-induced apoptosis is partially MPT-dependent [51, 52], while there is no available information on TD-induced MPT pore opening. Is thiamine deficiency-induced cellular death, a model of oxidative stress, MPT-dependent?
This review focus on a better understanding of cellular and molecular mechanisms underlying alcohol and TD toxicities on neuroapoptosis.
Alcohol induces apoptotic cellular death
Widespread neuroapoptosis is a devastating neurodegenerative event underlying microcephaly and intellectual disability related to FAS [53–55]. Neurotoxic effects of neonatal alcohol exposure on cellular death depend on brain region, neuronal population and treatment period [56–58]. Alcohol-induced neuronal death is mainly mediated by the mitochondrial apoptotic pathway also known as intrinsic apoptotic pathway [59, 60]. The Bcl-2 family proteins are critical factors triggering intrinsic apoptotic pathway [58]. Indeed, ethanol exposure up-regulates pro-apoptotic Bax and Bad, but down-regulates anti-apoptotic Bcl2 in neonatal rat brain [61, 62]. If Bax was up-regulated, there would be an increase of cytochrome c in cytosol that enhanced susceptibility to apoptosis [63]. However, literature provided no penetrating insight into the mechanisms underlying ethanol’s neurotoxicity. For instance, it is unclear under what conditions alcohol induces MPT pore opening? What Bax (cytoslic or mitochondrial) opens the MPT pore? What mitochondrial membrane (inner or outer) is permeabilized by Bax? What is the effectiveness of oxidative stress on the neurotoxic actions of alcohol? What vulnerability to alcohol for neuronal populations?
Alcohol-induced MPT pore opening is unspecific and cytosol-dependent
Direct exposure to ethanol, of brain mitochondria isolated from 7-day-old mouse pups, displayed no change in MPT pore regulation. When isolated from ethanol-treated 7-day-old mouse pups, brain mitochondria did not display any more change in MPT pore regulation [52]. Conversely, in vitro studies using either primary cultures of cerebellar granule cells [64, 65] or cultured hippocampal cells line, Jung et al. [66] show that ethanol exposure at physiologically relevant concentrations causes neuron death, supporting the notion that ethanol can kill neuron directly resulting in rapid mitochondrial membrane swelling and the collapse of membrane potential [66]. These observations indicate that ethanol-induced MPT pore opening is mediated by cytosolic factors. Moreover, MPT pore opening is tested for its sensitivity to both ethanol and related oxidative stress by the use of cyclosporine A which acts as specific inhibitor of MPT pore opening. By binding to cyclophilin D (a possible component of the MPT pore), cyclosporine A inhibits MPT pore opening, prevents mitochondrial dysfunction and ultimately cellular death [38]. According to Lamarche et al. [52], cyclosporine A provokes a non-specific inhibition of alcohol-induced MPT pore, suggesting that ethanol and related oxidative stress are not critical keys opening pore. Consequently, alcohol-induced MPT pore is not specific to cyclosporine A inhibition, but only partially sensitive to it [67]. The role of oxidative stress in ethanol-induced neuron death is further explored by the treatment of antioxidants. Pycnogenol (PYC) is a potent antioxidant resulting in bioflavonoids combination. PYC and the antioxidant vitamin E protect against ethanol-induced apoptosis of cultured cerebellar granule cells in a dose-dependent manner [68]. These results support the hypothesis that oxidative stress is involved in ethanol-induced neuroapoptosis. However, Kane et al. [69] reported that in cerebellar granule cells, isolated from 4-day-old rats exposed to ethanol in vivo, neither ROS production nor neuron death are showed. In addition, 17β-estradiol protects more efficiently against the ethanol-dependent oxidative stress-induced MPT pore opening than PYC an efficient antioxidant [66]. These findings suggest that ethanol-related oxidative stress provokes partial opening of MPT pore [66]. Following these observations, ethanol-induced death of neonatal granule cells would be partially shared between proapoptotic Bax and ethanol-increased ROS production [70]. However, literature does not provide any evidence that Bax is an undisputed component of MPT pore. Moreover, many aspects of alcohol-induced mitochondrial energy production failure do not regulate this model of MPT including Bax as pore component. In addition, regulation of this model of pore-forming Bax is not compatible with underlying mechanisms of alcohol-induced disruption of intracellular calcium metabolism and signaling, leading to apoptotic cellular death. Since ethanol-induced MPT pore opening is unspecific, how do new cell types respond to alcohol exposure as there are diversifying and migrating cell populations in developing brain?
Alcohol-induced MPT pore opening is cellular type-dependent and F1F0-ATP synthase-mediated
Researchers have designed primary cells culture as ideal model to study the ethanol-induced neuroapoptosis in vitro where cells maintained in depolarizing conditions do not proliferate [58]. To clarify mechanisms of cellular death, two different types of primary cells culture obtained from mouse embryo brain, e.g. astrocytes and neurons were exposed to ethanol for 3 days [52]. Astrocytes show transient MPT pore opening, while neurons (10–20%) exhibit permanent MPT pore opening with similar percentage of cell death. Ethanol-treated 7-day-old mouse pups displayed widespread caspase-3 activation in neurons, but not in astrocytes [52]. Similar results are reported in vivo studies where cerebellar granule cells have greater sensitivity to ethanol-induced neuroapoptosis compared to Purkinje cells [71]. In the developing rat hippocampus, alcohol kills more easily pyramidal cells in regions CA1, CA3 and DG, but the magnitude of apoptotic cell death was significantly greater in CA1 than in CA3 and DG, which did not differ [56, 57, 72]. Ethanol induces programmed cell death by raising the concentration of free cytoplasmic Ca2+. The source of Ca2+ is attributed to the entry of extracellular Ca2+, it’s externalization from the endoplasmic reticulum [73]. Ethanol initiates Ca2+ mobilization in multiple cell types; however alcohol-triggered apoptosis or programmed cell death is cell type and stage specific-dependent [72, 74].
Mitochondria are target subcellular organelles of ethanol. Excessive cell apoptosis was found in the cerebra of prenatal alcohol exposure fetuses. Proliferation and differentiation of fetal cerebral mitochondria were inhibited by alcohol. Impaired mitochondria development plays a role in the CNS defects induced by prenatal alcohol exposure [75]. Thus, prenatal alcohol exposure impairs mitochondrial structure and function and decreases F-ATP synthase activity in both the brain and liver [76]. Mitochondrial F-ATP synthase consists of two functional domains (Fig. 1): F1, situated in the mitochondrial matrix, and F0, located in the inner mitochondrial membrane [77]. On the one hand, alcohol permanently impaired F-ATP synthase structure by altering the synthesis of both F1 and F0 components, thereby impeding their interactions. For instance, F1 is composed of 3α/3β/γ/δ/ε subunits [49]. Mashimo et al. [78] reported that alcohol increased the α and β subunits of F1 in dose-dependent manner. Two of the F0 subunits, subunit (a) and subunit A6L which are encoded by the mtDNA ATP6 and ATP8 genes, respectively [79], were reduced in mitochondria from ethanol-fed animals [80]. However, these nuclear-encoded mitochondrial proteins may be regulated like a translational, rather than a transcriptional mechanism [78]. Moreover, the ATPase activity in ethanol-fed rats was inhibited 61% by addition of oligomycin; a decrease in oligomycin sensitivity could be attributed to an alteration in the functioning of the oligomycin sensitivity-conferring protein (OSCP corresponding to bacterial δ), [81]. On the other hand, the function of ATP synthase is to synthesize ATP from ADP and inorganic phosphate (Pi) in the F1 sector. After ethanol consumption, ATP turnover was threefold increased and a large part of the ATP production was diverted to redox re-equilibrium [82]. Indeed, ethanol hyperpolarizes mitochondrial membrane potential (DeltaPsim) and increases mitochondrial fraction in cultured mouse myocardial cell; it also dose-dependently increased ROS production. These cell pathophysiological reactions suggest the depression of mitochondrial ATPase and mitochondrial respiratory chain [83]. In addition, liver mitochondria from rats fed ethanol chronically demonstrated a 35% decrease in mitochondrial ATPase activity. Treatment of mitochondria from ethanol-fed rats with the detergent, Lubrol-WX, caused the release of 36% of the F1 from the resulting inner membrane particles. In comparison, only 5% of the F1 was dissociated when control mitochondria were subjected to the Lubrol treatment [81]. These observations indicate that alcohol inhibits ATP synthase activity and reduces ATP production, thereby diverting the tricarboxylic acid cycle toward the anaerobic degradation of glucose and the accumulation of intracellular lactic acid which may lead to cellular death [10]. Taken together, it appears that ethanol destabilizes profoundly not only ATP synthase function, but also its structure which is weakened by alcohol-induced important loss of proteins components.
Recent studies indicate that ATP synthase is not just an enzyme but rather a nanomotor inducing MPT pore likely to cause cellular death [44], i.e. after structural damage caused by alcohol. Indeed, ethanol-induced cellular death may be mediated by the inner mitochondrial F-ATP synthase able to form MPT pore. Thus, F0 sector can form a high-conductance voltage-dependent channel [45], because highly purified c subunit, a membrane-embedded F0 component, self-assembles into annular structures embedded within liposome bilayer [46, 47]. The c-subunit ring of the F0 is a candidate for the mitochondrial MPT pore. Recombinant F1 beta-subunit applied exogenously to the purified c-subunit enhances the probability of pore closure [47]. Prolonged high matrix Ca2+ enlarges the c-subunit ring and unhooks it from cyclophilin D/cyclosporine A binding sites in the ATP synthase F1, providing a mechanism for MPT pore opening [84]. However, the mammalian F-ATP synthase does not require CyPD for a pore-forming component [48]. Thus, the channel of the MPT forms within the c-ring itself after Ca2+-dependent extrusion of F1, i.e., of the γ/δ/ε subunits [84]. The “F0 channel” could not be closed by subunits γ, δ, or ε, while it was blocked by subunit β, suggesting that this is the mechanism through which pore closure occurs in situ [84]. In cultured neonatal rat cardiomyocytes exposed to ethanol, the cellular protein abundances in the α and β subunits of ATP synthase increased in dose-dependent manner [78], suggesting a possible dislocation of F1 components, e.g. α/β/γ/δ/ε subunits, related to alcohol intoxication. According to Kouzoukas et al. [85] alcohol releases intracellular Ca(2+) from endoplasmic reticulum stores, resulting in a sustained increase in intracellular calcium which may be a key determinant in the mechanism underlying alcohol-induced neuronal death. On the one hand, alcohol-increased cytosolic Ca2+ levels trigger Ca2+ movement into the mitochondrial matrix by the opening of a Ca2+ sensitive ion channel in the inner mitochondrial membrane, resulting in accumulation of Ca2+ in the matrix [86, 87]. Ca2+ overload can produce an uncoupling process halting ATP production and opening permeability transition pore by dislocation of the rotor stalk γ/ε/c subunits [88]. Such a Ca2+ release channel is heavily regulated, so that only after prolonged opening does pathological channel opening occur [89], which may be correlated with energy failure as a result of arrest of ATP synthesizing activity. On the other hand, chronic ethanol exposure may activate MPT pore opening by physiological calcium oscillations [90]. The inner membrane of rat liver mitochondria contains a reversible Ca(2+)-dependent pore, opening of which is largely blocked by cyclosporin A. McGuinness et al. [91] reported the presence of two classes of high and low-affinity cyclosporin A binding sites in mitochondria. Cyclosporin A inhibits pore opening by interacting with the low-capacity site comparable to ethanol-induced Ca(2+)-dependent pore. Taken together, the signaling cascades of cell dying processes, triggered by chronic ethanol exposure-damaged ATP synthase, start when ethanol hyperpolarizes mitochondrial membrane potential (DeltaPsim) which impaired proton gradient and its translocation through mitochondrial membrane, thereby stopping the rotation of γ/ε/c subunits complex and reducing ATP production leading to intracellular acidification. Prolonged blockade of rotor stalk γ/ε/c subunits, in addition to intracellular acidification and increased calcium entry into mitochondria, causes F1 γ/ε subunits dislocation and their extrusion from the mouth of F0 c-subunit ring membrane-embedded, thereby opening MTP pore within c-subunit ring. Credibly, chronic ethanol exposure impedes chemical interactions between γ/ε/c subunits.
Alcohol-induced neuronal death is intrinsic apoptotic pathway
Two apoptotic pathways (intrinsic and extrinsic) have been described, either of which may culminate in the activation of caspase-3. On the one hand, the intrinsic pathway is regulated by Bax and Bcl-XL and involves Bax-induced mitochondrial outer (cytosolic side) membrane permeability pore and release of cytochrome c as antecedent events leading to caspase-3 activation [51, 59, 92]. After possible activation of cytosolic Bax by ethanol, Bax undergoes subsequent translocation into outer mitochondrial membrane to form MPT pore [93, 94]. Indeed, ethanol exposure on postnatal day 4 (P4) induces in the rat cerebellum significant increases in expression levels of pro-apoptotic factors Bad and Bax mRNA, while significant decreases in anti-apoptotic Bcl2 mRNA were shown [62]. In addition, ethanol exposure elicited further increases in cytosolic pro-apoptotic Bid and mitochondrial tBid (its truncated, apoptotically active fragment), when administration was at P4; Bax:tBid heterodimers were also markedly increased [95]. These observations suggest that ethanol alters nuclear transcription of proteins in the Bcl2 family genes [62] and increases interactions of cytosolic pro-apoptotic Bid and Bad with Bax at the origin of MPT pore formation. Consequently, a primary mode of Bax-induced initiation of the apoptosis cascade following ethanol insult involves interactions with proteins of the MPT pore complex and not channel formation, which make it independent from MPT pore constituents [96], and dead receptors [64]. On the other hand, activation of caspase-8 is a key event preceding caspase-3 activation in the extrinsic pathway [64, 97]. Ethanol caused no change in activated caspase-8 (the death receptor pathway cellular membrane-initiated), which suggests that the extrinsic pathway is not involved in ethanol-induced apoptosis [98]. Therefore, it appears that ethanol-induced neuroapoptosis is an intrinsic pathway, which is triggered by cytosolic calcium concentration and acidification, and modulated by cytosolic Bcl-2 family proapoptotic proteins [98].
Thiamine deficiency induces both apoptotic and necrotic cellular death
In vitro [50] and vivo [7, 12, 13] studies showed that TD induces more severe cellular death than alcohol. However, ethanol and TD showed synergistic toxicity on cellular death [5, 41, 50]. Moreover, TD triggers more oxidative stress and cellular damage than alcohol [10, 99]. Comparatively to alcohol, TD results from a more general impairment of oxidative phosphorylation due to a shortage of ATP generation cofactors and may be relevant to energy-related disorders [100]. Indeed, thiamine deficiency induces severe neuronal death [101]. According to Bettendorff et al. [102], when neuroblastoma cells were transferred to a medium of low thiamine concentration, oxygen consumption and ATP levels decreased while lactate production increased. At least 25% of mitochondria were swollen and electron translucent. Cell mortality increased to 75% within 5 days while overt signs of necrosis appeared [103]. Figure 2 shows comparative developmental neurotoxicity of alcohol and TD: it appears that alcohol and TD induce apoptotic cellular death with similar intensity, while TD provokes more extensive necrotic cellular death and damage than alcohol [13]. These observations suggest that alcohol and TD induce cellular death by different pathways [7, 12]. Why does TD cause more severe cellular death than alcohol?
Patterns of neurofunctional alterations in offspring pupped either alternately by prenatal, perinatal and postnatal thiamine-deprived dams, or in offspring pupped by ethanol-treated dams during gestation and lactation. Following every treatment, average rates of neurofunctional alterations relative to controls are assessed on seven developmental abilities performed by each pup from postnatal day 10–45 (N = 11 pups tested for each treatment). General profile of curves indicates that among the three patterns of developmental thiamine deficiencies (TD), only perinatal TD exhibits a closer relationship with developmental alcohol exposure. Both developmental TD and ethanol exposure produce two waves of neurofunctional alterations, peaking at P15 (postnatal day 15) and P25, respectively. The first peak is described as prenatal event and interferes with the periods of intense cellular proliferation and migration: it characterizes enhanced physiological apoptosis induced invariably with the same intensity by either alcohol or TD. The second peak of vulnerability is described like both perinatal and postnatal events; it interferes with the periods of cellular differentiation, synapses formation, axonal growth and myelinogenesis: It characterizes alcohol or TD-induced tissue damage and necrotic cellular death. The results show that alcohol and TD induce apoptotic cellular death with similar intensity, while TD provokes more extensive necrotic cellular death than alcohol. From Bâ [6]
TD-induced apoptotic or necrotic cellular death is developmental stage and ROS-dependent
Figure 2 indicates that TD-induced either apoptotic or necrotic cellular death is developmental stage-dependent. Thus, during prenatal period corresponding to cell proliferation and migration, TD induces preferentially physiological apoptosis to the same extend than alcohol. Conversely, postnatal period corresponds to axogenesis and dendritic branching leading to neuronal network and tissue constructions. During that period of tissue formation, TD causes more devastative tissue damage and necrotic cellular death than alcohol.
These observations are confirmed by microphotography analysis performed on the histology of hippocampal CA3 pyramidal cells obtained from different treatments (Fig. 3). Figure 3c shows that prenatal thiamine deficiency was characterized by a singular deficit of CA3 pyramidal cells comparative to regular diet or control (Fig. 3b), without any direct impact on nucleus or cytoplasm shape, like physiological apoptosis. Similarly, developmental alcohol exposure (Fig. 3e) induced apoptosis in the same extend with direct impact on nucleus or cytoplasm shape expressed by more cornered, irregular and sparse pyramidal cells in the hippocampal CA3 field (Fig. 3e), comparative to regular diet (Fig. 3b). These observations suggest that ROS mediates partially alcohol toxicity by membrane lipid peroxidation. Conversely, Fig. 3d shows typical features of severe postnatal thiamine deficiency with characteristic breakings on cellular membranes illustrated by more cornered than pyramidal shaped cells in the hippocampal CA3 field [10]. Moreover, postnatal thiamine deficiency resulted in a significant increase in pro-apoptotic-related morphological and biochemical changes characterized by cells containing condensed chromatin (Fig. 3d), thereby illustrating necrotic cellular death. What molecular interpretation is to be given to both aspects of cellular death induced by thiamine deficiency, developmental stage-dependent?
Comparative effects of developmental thiamine deficiencies (TD) and ethanol exposure on the hilar CA3 pyramidal cells of the hippocampus. Parasagittal sections of the left ventral hippocampus were carried out in 45-day-old rats. Paraffin 10 µm thick sections were stained with a combination of hematoxylin–eosin and indigo carmine; sections of the midtemporal hippocampus were assessed. a The arrows demarcate the portion of CA3 region on which microphotography was performed to show any treatment effects; bar 100 µm. b Control; c prenatal TD exposed pups; d postnatal TD exposed; e developmental alcohol exposure induced from gestation to lactation. Bar 20 µm. Extract from data published elsewhere [10, 12, 13]
Indeed, MPT pore-mediated cellular death preferably occurred rather through necrosis than apoptosis [104], and is critically involved in necrotic cellular death induced by Ca2+ overloading and ROS overproduction [105]. In addition, thiamine deprivation reduced in brain mitochondria the activities of oxidant-scavenging enzymes e.g. superoxide dismutase, glutathione peroxydase and catalases, inducing oxidative stress in brain mitochondria and increasing the lipid peroxidation [106]. At both cellular and mitochondrial levels, dysregulation of these oxidant-scavenging enzymes directly leads to the opening of the MPT pore followed by induction of apoptotic makers, namely chromatin margination and condensation, vacuolization of the cytosol and damage of the plasma membrane [107]. While ethanol-induced apoptotic cellular death is partially mediated by ROS increase [70], TD triggers necrotic cellular death by ROS overproduction related to extensive oxidative stress [10, 99]. These observations suggest that TD-derived free radicals overproduction induced more drastic and necrotic cellular death than alcohol. We can assume that relative to alcohol, TD may prolong MPT pore opening which increases free passage of diverse molecules into the mitochondria, including protons and results in oxidative phosphorylation uncoupling that leads to ATP depletion with ROS accumulation and subsequent necrotic cellular death [22, 108]. Consequently, thiamine deficiency-induced severe cellular death may be mediated by at least two different mitochondria pathways: the first amplifying physiological apoptosis during neurogenesis is F1F0-ATP synthase-mediated; the second mediating necrotic death during tissue formation is ROS-induced CyP-D activation [33]. What role cyclophilin D plays (CyP-D) in MPT pore formation and regulation and ultimate injury tissues?
Mitochondrial CyP-D opens MPT pore-dependent necrosis in TD-induced neurotoxicity
CyP-D belongs to cyclophilin proteins family that have got seven major isoforms found in subcellular compartments including the cytoplasm (CyP-D, CyP-NK, CyP-40), endo (sarco) plasmic reticulum (CyP-B, CyP-C), nucleus (CyP-E) and mitochondria (CyP-D), [109]. Mitochondrial CyP-D is a nuclear encoded protein that contains a mitochondrial targeting presequence which is cleaved after its translocation from mitochondria matrix into the inner membrane [110]. Expression of CyP-D, a soluble mitochondrial matrix protein, is associated with MPT pore opening and cellular death [33]. Knockout of CyP-D, a component of MPT pore, protects from injury, in the manner of drugs that blockade MPT pore [36]. CyP-D can also act as a redox sensor in mitochondria [23, 111] and regulates Ca2+ exchange between endoplasmic reticulum and mitochondria [112]. Reducing oxidative stress or Ca2+ overload prevent necrotic cellular death [36, 38]. Diminished thiamine induces oxidative stress accompanied by endoplasmic reticulum calcium stores modifications and ATP depletion [113] which provoke MPT pore opening in the inner mitochondrial membrane [114]. The oxidative stress related to TD damages the endoplasmic reticulum structure observable by electron microscopy [115]. Therefore, we can assume that TD-induced oxidative stress is paralleled by widespread contamination of reactive oxygen species, which damage endoplasmic reticulum membrane and lead to Ca2+ releasing from stores. The resulting cytoplasmic Ca2+ overloading flows into mitonchondria and activates CyP-D translocation from the matrix to make up channel-like proteins into the inner membrane [116], thereby inducing MPT pore opening with subsequent release of cytochrome c and caspase cascade activation which triggers necrotic cellular damage and death. Indeed, the MPT pore opening is regulated by CypD under the control of mitochondrial matrix Ca2+ concentration [40]. CyP-D-dependent MPT pore mediates some forms of necrotic, but not apoptotic cellular death [117, 118]. However, Bcl-2 family members-induced cellular death does not depend on CyP-D. Thus, CyP-D and MPT are required for mediating Ca2+ overloading and oxidative damage-induced necrotic cellular death, but not Bcl-2 family members-regulated death [17]. These observations indicate that different structural components of MPT pore complexes are required for mediating either apoptotic or necrotic cellular death.
TD and alcohol interact with different structural components of MPT pore complexes
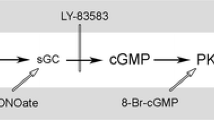
Recent studies indicate that TD can use caspase-3 classical pathway to amplify physiological apoptosis [14, 119] like alcohol intoxication [98]. However, several experimental issues indicate that TD develops predominantly the mitochondria-dependent pathway for necrotic cellular death. On the one hand, the present study shows that the MPT pore-dependent apoptosis in alcohol intoxication is mediated by F1F0-ATP synthase, reversible Ca2+-dependent pore and low-affinity cyclosporin A binding pore. On the other hand, overproduction of reactive oxygen species (ROS) mainly triggers the CyP-D-dependent MPT pore mediating necrotic cellular death during TD-induced neurotoxicity and generates injury tissues following oxidative stress [32]. Pharmacological investigations indicate that the cyclophilin D (CyP-D)-binding drug, namely cyclosporine A inhibits efficiently the MPT pore-dependent necrosis [116], while it blockades only partially the MPT pore-dependent apoptosis [52], highlighting substantial differences in mechanisms of cellular death between alcohol and TD. Indeed, in TD-induced neurotoxicity, three proteins have been accepted as key structural components of the MPT pore-dependent necrosis: the voltage dependent anion channel in the outer membrane, the adenine-nucleotide translocase in the inner membrane and cyclophilin D in the mitochondrial matrix [24, 114]. Knockout studies have eliminated the voltage-dependent anion channel as an essential component of MPT pore and attributed a regulatory, rather than structural role to the adenine nucleotide translocase [105]. Similar knockout studies have confirmed a role for cyclophilin D (CyP-D) in pore opening, probably mediated by its peptidyl-propyl cis–trans isomerase activity that facilitates a conformational change in an inner membrane protein [32, 120]. An important finding from this study indicates two different mitochondria pathways regulating cellular death: the first mechanism may engage alcohol which activates the c-subunit ring of the F0-ATP synthase to form MPT pore-dependent apoptosis; following the second mechanism, TD activates CyP-D translocation from mitochondrial matrix towards the mitochondrial inner membrane to form MPT pore-dependent necrosis. A distinction is therefore made between the two pathways by designating the first mechanism “low-affinity cyclosporin A binding pore” and the second mechanism by “high-affinity cyclosporin A binding pore”. Indeed, the two types of cell death seem to be overlapping. In physiological conditions, c-subunit conductance can switch reversibly between open and closed states regulated traditionally by Ca2+, CsA, CypD and Bcl-xL which bind to F1 components [44]. Cytosolic and mitochondrial Ca2+ overload can produce a rapid increase in permeability of the mitochondrial inner membrane to solutes inducing MPT pore-dependent apoptosis. The pore diameter expands during Ca2+-induced increases in MPT conductance. However, an increase in mitochondrial outer membrane permeability may also be triggered by an acute inner membrane depolarization [121], when MPT pore opening is prolonged by ROS overproduction associated with structural breakdown of the mitochondrial matrix accompanied by outer mitochondrial membrane rupture and cell death [121]. Such a pathological MPT pore opening is associated with necrotic cell death.
Together, these observations demonstrate that alcohol and TD trigger two different mechanisms of MTP pore opening: Alcohol promotes neuroapoptosis while TD triggers both neuroapoptotic and necrotic cellular deaths (Fig. 2). The two neurotoxicants can act synergistically to provoke extensive cellular death and tissue necrosis related to FAS. Consequently, current mechanistic understanding the mitochondria-mediated both apoptotic and necrotic signaling pathways may be promising therapeutic strategy to identify a new generation of drugs treating the FAS pathology. In particular, investigations on neuroprotective effects of pharmacological inhibition of cyclophilin D are challenges for the dawning of mitochondrial medicine [116].
References
Krulewitch CJ (2005) Alcohol consumption during pregnancy. Annu Rev Nurs Res 23:101–134
Ripabelli G, Cimmino L, Grasso GM (2006) Alcohol consumption, pregnancy and fetal alcohol syndrome: implications in public health and preventive strategies. Ann Ig 18:391–406
Butterworth RF (1995) Pathophysiology of alcoholic brain damage: synergistic effects of ethanol, thiamine deficiency and alcoholic liver disease. Metab Brain Dis 10:1–8
Mulholland PJ, Self RL, Stepanyan TD, Little HJ, Littleton JM, Prendergast MA (2005) Thiamine deficiency in the pathogenesis of chronic ethanol-associated cerebellar damage in vitro. Neuroscience 135:1129–1139
Mancinelli R, Ceccanti M (2009) Biomarkers in alcohol misuse: their role in the prevention and detection of thiamine deficiency. Alcohol Alcohol 44:177–182
Bâ A (2011) Comparative effects of alcohol and thiamine deficiency on the developing central nervous system. Behav Brain Res 225:235–242
Roecklin B, Levin SW, Comly M, Mukherjee AB (1985) Intrauterine growth retardation induced by thiamine deficiency and pyrithiamine during pregnancy in the rat. Am J Obstet Gynecol 151:455–460
Bâ A (2012) Effects of thiamine deficiency on food intake and body weight increment in adult female and growing rats. Behav Pharmacol 23:575–581
Bâ A (2012) Paradoxical effects of alcohol and thiamine deficiency on the eye opening in rat pups. J Matern Fetal Neonatal Med 25:2435–2440
Bâ A (2008) Metabolic and structural role of thiamine in nervous tissues. Cell Mol Neurobiol 28:923–931
Bâ A (2009) Alcohol and B1 vitamin deficiency-related stillbirths. J Matern Fetal Neonatal Med 22:452–457
Bâ A, Seri BV, Aka KJ, Glin L, Tako A (1999) Comparative effects of developmental thiamine deficiencies and ethanol exposure on the morphometry of the CA3 pyramidal cells. Neurotoxicol Teratol 21:579–586
Bâ A, N’Douba V, d’Almeida MA, Seri BV (2005) Effects of maternal thiamine deficiencies on the pyramidal and granule cells of the hippocampus of rat pups. Acta Neurobiol Exp 65:387–398
Bâ A (2005) Functional vulnerability of developing central nervous system to maternal thiamine deficiencies in the rat. Dev Psychobiol 47:408–414
Reed JC (2000) Mechanisms of apoptosis. Am J Pathol 157:1415–1430
Grimm S, Brdiczka D (2007) The permeability transition pore in cell death. Apoptosis 12:841–855
Baines CP, Kaiser RA, Purcell NH, Blair NS, Osinska H, Hambleton MA, Brunskill EW, Sayen MR, Gottlieb RA, Dorn GW, Robbins J, Molkentin JD (2005) Loss of cyclophilin D reveals a critical role for mitochondrial permeability transition in cell death. Nature 434:658–662
Bonora M, Bononi A, De Marchi E, Giorgi C, Lebiedzinska M, Marchi S, Patergnani S, Rimessi A, Suski JM, Wojtala A, Wieckowski MR, Kroemer G, Galluzzi L, Pinton P (2013) Role of the c subunit of the FO ATP synthase in mitochondrial permeability transition. Cell Cycle 12:674–683
Ashkenazi A (2008) Directing cancer cells to self-destruct with pro-apoptotic receptor agonists. Nat Rev Drug Discov 7:1001–1012
Yin XM (2000) Signal transduction mediated by Bid, a pro-death Bcl-2 family proteins, connects the death receptor and mitochondria apoptosis pathways. Cell Res 10:161–167
Devun F, Walter L, Belliere J, Cottet-Rousselle C, Leverve X, Fontaine E (2010) Ubiquinone analogs: a mitochondrial permeability transition pore-dependent pathway to selective cell death. PLoS ONE 5:e11792
Zorov DB, Filburn CR, Klotz LO, Zweier JL, Sollott SJ (2000) Reactive oxygen species (ROS)-induced ROS release: a new phenomenon accompanying induction of the mitochondrial permeability transition in cardiac myocytes. J Exp Med 192:1001–1014
Ott M, Gogvadze V, Orrenius S, Zhivotovsky B (2007) Mitochondria, oxidative stress and cell death. Apoptosis 12:913–922
Schwarz M, Andrade-Navarro MA, Gross A (2007) Mitochondrial carriers and pores: key regulators of the mitochondrial apoptotic program? Apoptosis 12:869–876
Minn AJ, Velez P, Schendel SL, Liang H, Muchmore SW, Fesik SW, Fill M, Thompson CB (1997) Bcl-xL forms an ion channel in synthetic lipid membranes. Nature 385:353–357
Schendel S, Azimov R, Pawlowski K, Godzik A, Kagan B, Reed J (1999) Ion channel activity of the BH3 only Bcl-2 family member, BID. J Biol Chem 274:21932–21936
Letai A (2005) Pharmacological manipulation of Bcl-2 family members to control cell death. J Clin Invest 115:2648–2655
Wensveen FM, Alves NL, Derks IAM, Reedquist KA, Eldering E (2011) Apoptosis induced by overall metabolic stress converges on the Bcl-2 family proteins Noxa and Mcl-1. Apoptosis 16:708–721
Ying Y, Padanilam BJ (2016) Regulation of necrotic cell death: p53, PARP1 and cyclophilin D-overlapping pathways of regulated necrosis? Cell Mol Life Sci 73:2309–2324
Fakharnia F, Khodagholi F, Dargahi L, Ahmadiani A (2017) Prevention of Cyclophilin D-mediated mPTP opening using cyclosporine-A alleviates the elevation of necroptosis, autophagy and apoptosis-related markers following global cerebral ischemia-reperfusion. J Mol Neurosci 61:52–60
Chang P, Dong W, Zhang M, Wang Z, Wang Y, Wang T, Gao Y, Meng H, Luo B, Luo C, Chen X, Tao L (2014) Anti-necroptosis chemical necrostatin-1 can also suppress apoptotic and autophagic pathway to exert neuroprotective effect in mice intracerebral hemorrhage model. J Mol Neurosci 52:242–249
Leung AW, Halestrap AP (2008) Recent progress in elucidating the molecular mechanism of the mitochondrial permeability transition pore. Biochem Biophys Acta 1777:946–952
Javadov S, Kuznetsov A (2013) Mitochondrial permeability transition and cell death: the role of cyclophilin D. Front Physiol 4:76
Qin LS, Jia PF, Zhang ZQ, Zhang SM (2015) ROS-p53-cyclophilin-D signaling mediates salinomycin-induced glioma cell necrosis. J Exp Clin Cancer Res 34:57
Radhakrishnan J, Bazarek S, Chandran B, Gazmuri RJ (2015) Cyclophilin-D: a resident regulator of mitochondrial gene expression. FASEB J 29:2734–2748
Halestrap AP (2006) Calcium, mitochondria and reperfusion injury: a pore way to die. Biochem Soc Trans 34:232–237
Hausenloy DJ, Lim SY, Ong SG, Davidson SM, Yellon DM (2010) Mitochondrial cyclophilin-D as a critical mediator of ischaemic preconditioning. Cardiovasc Res 88:67–74
Schinzel AC, Takeuchi O, Huang Z, Fisher JK, Zhou Z, Rubens J, Hetz C, Danial NN, Moskowitz MA, Korsmeyer SJ (2005) Cyclophilin D is a component of mitochondrial permeability transition and mediates neuronal cell death after focal cerebral ischemia. Proc Natl Acad Sci USA 102:12005–12010
Matas J, Young NT, Bourcier-Lucas C, Ascah A, Marcil M, Deschepper CF, Burelle Y (2009) Increased expression and intramitochondrial translocation of cyclophilin-D associates with increased vulnerability of the permeability transition pore to stress-induced opening during compensated ventricular hypertrophy. J Mol Cell Cardiol 46:420–430
Gainutdinov T, Molkentin JD, Siemen D, Ziemer M, Debska-Vielhaber G, Vielhaber S, Gizatullina Z, Orynbayeva Z, Gellerich FN (2015) Knockout of cyclophilin D in Ppif−/− mice increases stability of brain mitochondria against Ca²+ stress. Arch Biochem Biophys 579:40–46
Weber J, Senior AE (2003) ATP synthesis driven by proton transport in F1F0-ATP synthase. FEBS Lett 545:61–70
Campanella M, Parker N, Tan CH, Hall AM, Duchen MR (2009) IF (1): setting the pace of the F(1)F(o)-ATP synthase. Trends Biochem Sci 34:343–350
Capaldi RA, Aggeler R (2002) Mechanism of the F1F0-type ATP synthase, a biological rotary motor. Trends Biochem Sci 27:154–160
Jonas EA, Porter GA Jr, Beutner G, Mnatsakanyan N, Alavian KN (2015) Cell death disguised: the mitochondrial permeability transition pore as the c-subunit of the F(1)F(O) ATP synthase. Pharmacol Res 99:382–392
Sorgato MC, Moran O, De Pinto V, Keller BU, Stühmer W (1989) Further investigation on the high-conductance ion channel of the inner membrane of mitochondria. J Bioenerg Biomembr 21:485–496
Arechaga I, Butler PJ, Walker JE (2002) Self-assembly of ATP synthase subunit c rings. FEBS Lett 515:189–193
Meier T, Matthey U, Henzen F, Dimroth P, Müller DJ (2001) The central plug in the reconstituted undecameric c cylinder of a bacterial ATP synthase consists of phospholipids. FEBS Lett 505:353–356
Giorgio V, von Stockum S, Antoniel M, Fabbro A, Fogolari F, Forte M, Glick GD, Petronilli V, Zoratti M, Szabó I, Lippe G, Bernardi P (2013) Dimers of mitochondrial ATP synthase form the permeability transition pore. Proc Natl Acad Sci USA 110:5887–5892
Bernardi P (2013) The mitochondrial permeability transition pore: a mystery solved? Front Physiol 4:95
Ke Z-J, Wang X, Fan Z, Luo J (2009) Ethanol promotes thiamine deficiency-induced neuronal death: involvement of double-stranded Rna-activated protein kinase. Alcohol Clin Exp Res 33:1097–1103
Higuchi H, Adachi M, Miura S, Gores GJ, Ishii H (2001) The mitochondrial permeability transition contributes to acute ethanol-induced apoptosis in rat hepatocytes. Hepatology 34:320–328
Lamarche F, Carcenac C, Gonthier B, Cottet-Rousselle C, Chauvin C, Barret L, Leverve X, Savasta M, Fontaine E (2013) Mitochondrial permeability transition pore inhibitors prevent ethanol-induced neuronal death in mice. Chem Res Toxicol 26:78–88
Maier SE, Chen WJ, Miller JA, West JR (1997) Fetal alcohol exposure and temporal vulnerability: regional differences in alcohol-induced microencephaly as a function of the timing of binge-like alcohol exposure during rat brain development. Alcohol Clin Exp Res 21:1418–1428
Klintsova AY, Helfer JL, Calizo LH, Dong WK, Goodlett CR, Greenough WT (2007) Persistent impairment of hippocampal neurogenesis in young adult rats following early postnatal alcohol exposure. Alcohol Clin Exp Res 31:2073–2082
Farber NB, Creeley CE, Olney JW (2010) Alcohol-induced neuroapoptosis in the fetal macaque brain. Neurobiol Dis 40:200–206
Livy DJ, Miller EK, Maier SE, West JR (2003) Fetal alcohol exposure and temporal vulnerability: effects of binge-like alcohol exposure on the developing rat hippocampus. Neurotoxicol Teratol 25:447–458
Miki T, Harris SJ, Wilce PA, Takeuchi Y, Bedi KS (2004) Effects of age and alcohol exposure during early life on pyramidal cell numbers in the CA1–CA3 region of the rat hippocampus. Hippocampus 14:124–134
Luo J (2012) Mechanisms of ethanol-induced death of cerebellar granule cells. Cerebellum 11:145–154
Chu J, Tong M, de la Monte SM (2007) Chronic ethanol exposure causes mitochondrial dysfunction and oxidative stress in immature central nervous system neurons. Acta Neuropathol 113:659–673
Nowoslawski L, Klocke BJ, Roth KA (2005) Molecular regulation of acute ethanol-induced neuron apoptosis. J Neuropathol Exp Neurol 64:490–497
Moore DB, Walker DW, Heaton MB (1999) Neonatal ethanol exposure alters Bcl-2 family mRNA levels in the rat cerebellar vermis. Alcohol Clin Exp Res 23:1251–1261
Ge Y, Belcher SM, Pierce DR, Light KE (2004) Altered expression of Bcl2, Bad and Bax mRNA occurs in the rat cerebellum within hours after ethanol exposure on postnatal day 4 but not on postnatal day 9. Brain Res Mol Brain Res 129:124–134
Osterhout DJ, Marin-Husstege M, Abano P, Casaccia-Bonnefil P (2002) Molecular mechanisms of enhanced susceptibility to apoptosis in differentiating oligodendrocytes. J Neurosci Res 69:24–29
Pantazis NJ, Dohrman DP, Goodlett CR, Cook RT, West JR (1993) Vulnerability of cerebellar granule cells to alcohol-induced cell death diminishes with time in culture. Alcohol Clin Exp Res 17:1014–1021
Luo J, West JR, Pantazis NJ (1997) Nerve growth factor and basic fibroblast growth factor protect rat cerebellar granule cells in culture against ethanol-induced cell death. Alcohol Clin Exp Res 21:1108–1120
Jung ME, Wilson AM, Ju X, Wen Y, Metzger DB, Simpkins JW (2009) Ethanol withdrawal provokes opening of the mitochondrial membrane permeability transition pore in an estrogen-preventable manner. J Pharmacol Exp Ther 328:692–698
Heaton MB, Moore DB, Paiva M, Madorsky I, Mayer J, Shaw G (2003) The role of neurotrophic factors, apoptosis-related proteins, and endogenous antioxidants in the differential temporal vulnerability of neonatal cerebellum to ethanol. Alcohol Clin Exp Res 27:657–669
Siler-Marsiglio KI, Shaw G, Heaton MB (2004) Pycnogenol and vitamin E inhibit ethanol-induced apoptosis in rat cerebellar granule cells. J Neurobiol 59:261–271
Kane CJ, Chang JY, Roberson PK, Garg TK, Han L (2008) Ethanol exposure of neonatal rats does not increase biomarkers of oxidative stress in isolated cerebellar granule neurons. Alcohol 42:29–36
Heaton MB, Paiva M, Madorsky I, Siler-Marsiglio K, Shaw G (2006) Effect of bax deletion on ethanol sensitivity in the neonatal rat cerebellum. J Neurobiol 66:95–101
Maier SE, West JR (2001) Regional differences in cell loss associated with binge-like alcohol exposure during the first two trimesters equivalent in the rat. Alcohol 23:49–57
Smith CC, Guévremont D, Williams JM, Napper RM (2015) Apoptotic cell death and temporal expression of apoptotic proteins Bcl-2 and Bax in the hippocampus, following binge ethanol in the neonatal rat model. Alcohol Clin Exp Res 39:36–44
Putney JW (2009) Capacitative calcium entry: from concept to molecules. Immunol Rev 231:10–22
Kilburn BA, Chiang PJ, Wang J, Flentke GR, Smith SM, Armant DR (2006) Rapid induction of apoptosis in gastrulating mouse embryos by ethanol and its prevention by HB-EGF. Alcohol Clin Exp Res 30:127–134
Xu Y, Liu P, Li Y (2005) Impaired development of mitochondria plays a role in the central nervous system defects of fetal alcohol syndrome. Birth Defects Res A Clin Mol Teratol 73:83–91
Marin-Garcia J, Ananthakrishnan R, Goldenthal MJ (1996) Mitochondrial dysfunction after fetal alcohol exposure. Alcohol Clin Exp Res 20:1029–1032
Jonckheere AI, Smeitink JAM, Rodenburg RJT (2012) Mitochondrial ATP synthase: architecture, function and pathology. J Inherit Metab Dis 35:211–225
Mashimo K, Arthur PG, Ohno Y (2015) Ethanol dose- and time-dependently Increases α and β subunits of Mitochondrial ATP synthase of cultured neonatal rat cardiomyocytes. J Nippon Med Sch 82:237–245
Anderson S, Bankier AT, Barrell BG, de Bruijn MH, Coulson AR, Drouin J, Eperon IC, Nierlich DP, Roe BA, Sanger F, Schreier PH, Smith AJ, Staden R, Young IG (1981) Sequence and organization of the human mitochondrial genome. Nature 290:457–465
Coleman WB, Cahill A, Ivester P, Cunningham CC (1994) Differential effects of ethanol consumption on synthesis of cytoplasmic and mitochondrial encoded subunits of the ATP synthase. Alcohol Clin Exp Res 18:947–950
Montgomery RI, Coleman WB, Eble KS, Carol C (1987) Ethanol-elicited alterations in the Oligomycin sensitivity and structural stability of the mitochondrial Fo*F1 ATPase. J Biol Chem 262:13285–13289
Beauvieux MC, Gin H, Roumes H, Kassem C, Couzigou P, Gallis JL (2015) Time-dependent effect of ethanol force-feeding on glycogen repletion: NMR evidence of a link with ATP turnover in rat liver. Alcohol 49:607–615
Mashimo K, Ohno Y (2006) Ethanol hyperpolarizes mitochondrial membrane potential and increases mitochondrial fraction in cultured mouse myocardial cells. Arch Toxicol 80:421–428
Alavian KN, Beutner G, Lazrove E, Sacchetti S, Park HA, Licznerski P, Li H, Nabili P, Hockensmith K, Graham M, Porter GA Jr, Jonas EA (2014) An uncoupling channel within the c-subunit ring of the F1F0-ATP synthase is the mitochondrial permeability transition pore. Proc Natl Acad Sci USA 111:10580–10585
Kouzoukas DE, Li G, Takapoo M, Moninger T, Bhalla RC, Pantazis NJ (2013) Intracellular calcium plays a critical role in the alcohol-mediated death of cerebellar granule neurons. J Neurochem 124:323–335
Budd SL, Nicholls DG (1996) Mitochondria, calcium regulation, and acute glutamate excitotoxicity in cultured cerebellar granule cells. J Neurochem 67:2282–2291
Bolnick JM, Karana R, Chiang PJ, Kilburn BA, Romero R, Diamond MP, Smith SM, Armant DR (2014) Apoptosis of alcohol-exposed human placental cytotrophoblast cells is downstream of intracellular calcium signaling. Alcohol Clin Exp Res 38:1646–1653
RA, Hunter DR (1979) The ca2+-induced membrane transition in mitochondria. II Nature of the ca2+ trigger site. Arch Biochem Biophys 195:460–467
Kinnally KW, Campo ML, Tedeschi H (1989) Mitochondrial channel activity studied by patch-clamping mitoplasts. J Bioenerg Biomembr 21:497–506
Hajnóczky G, Buzas CJ, Pacher P, Hoek JB, Rubin E (2005) Alcohol and mitochondria in cardiac apoptosis: mechanisms and visualization. Alcohol Clin Exp Res 29:693–701
McGuinness O, Yafei N, Costi A, Crompton M (1990) The presence of two classes of high-affinity cyclosporin A binding sites in mitochondria. Evidence that the minor component is involved in the opening of an inner-membrane Ca(2+)-dependent pore. Eur J Biochem 194:671–679
Galluzzi L, Zamzami N, de La Motte Rouge T, Lemaire C, Brenner C, Kroemer G (2007) Methods for the assessment of mitochondrial membrane permeabilization in apoptosis. Apoptosis 12:803–813
Tsuruta F, Sunayama J, Mori Y, Hattori S, Shimizu S, Tsujimoto Y, Yoshioka K, Masuyama N, Gotoh Y (2004) JNK promotes Bax translocation to mitochondria through phosphorylation of 14-3-3 proteins. Embo J 23:1889–1899
Heaton MB, Paiva M, Siler-Marsiglio K (2011) Ethanol influences on Bax translocation, mitochondrial membrane potential, and reactive oxygen species generation are modulated by vitamin E and brain-derived neurotrophic factor. Alcohol Clin Exp Res 35:1122–1133
Heaton MB, Paiva M, Kubovec S (2015) Differential effects of ethanol on bid, tBid, and Bax:tBid interactions in postnatal day 4 and postnatal day 7 rat cerebellum. Alcohol Clin Exp Res 39:55–63
Heaton MB, Siler-Marsiglio K, Paiva M, Kotler A, Rogozinski J, Kubovec S, Coursen M, Madorsky V (2013) Ethanol influences on Bax associations with mitochondrial membrane proteins in neonatal rat cerebellum. Dev Neurobiol 73:127–141
Park YH, Jeong MS, Jang SB (2014) Death domain complex of the TNFR-1, TRADD, and RIP1 proteins for death-inducing signaling. Biochem Biophys Res Commun. Biochem Biophys Res Commun 443:1155–1161
Young C, Klocke BJ, Tenkova T, Choi J, Labruyere J, Qin YQ, Holtzman DM, Roth KA, Olney JW (2003) Ethanol-induced neuronal apoptosis in vivo requires Bax in the developing mouse brain. Cell Death Differ 10:1148–1155
Gibson GE, Blass JP (2007) Thiamine-dependent processes and treatment strategies in neurodegeneration. Antioxid Redox Signal 9:1605–1619
Hernandez-Vazquez AJ, Garcia-Sanchez JA, Moreno-Arriola E, Salvador-Adriano A, Ortega-Cuellar D, Velazquez-Arellano A (2017) Thiamine deprivation produces a liver ATP deficit and metabolic and genomic effects in mice: findings are parallel to those of biotin deficiency and have implications for energy disorders. J Nutrigenet Nutrigenomics 9:287–299
Oliveira FA, Galan DT, Ribeiro AM, Santos Cruz J (2007) Thiamine deficiency during pregnancy leads to cerebellar neuronal death in rat offspring: role of voltage-dependent K+ channels. Brain Res 1134:79–86
Bettendorff L, Goessens G, Sluse F, Wins P, Bureau M, Laschet J, Grisar T (1995) Thiamine deficiency in cultured neuroblastoma cells: effect on mitochondrial function and peripheral benzodiazepine receptors. J Neurochem 64:2013–2021
Bettendorff L, Sluse F, Goessens G, Wins P, Grisar T (1995) Thiamine deficiency–induced partial necrosis and mitochondrial uncoupling in neuroblastoma cells are rapidly reversed by addition of thiamine. J Neurochem 65:2178–2184
Nakagawa T, Shimizu S, Watanabe T, Yamaguchi O, Otsu K, Yamagata H, Inohara H, Kubo T, Tsujimoto Y (2005) Cyclophilin D-dependent mitochondrial permeability transition regulates some necrotic but not apoptotic cell death. Nature 434:652–658
Baines CP, Kaiser RA, Sheiko T, Craigen WJ, Molkentin JD (2007) Voltage-dependent anion channels are dispensable for mitochondrial-dependent cell death. Nat Cell Biol 9:550–555
Sharma A, Bist R, Bubber P (2013) Thiamine deficiency induces oxidative stress in brain mitochondria of Mus musculus. J Physiol Biochem 69:539–546
Deryabina Y, Isakova E, Antipov A, Saris NE (2013) The inhibitors of antioxidant cell enzymes induce permeability transition in yeast mitochondria. J Bioenerg Biomembr 45:491–504
Halestrap AP (2009) What is the mitochondrial permeability transition pore? J Mol Cell Cardiol 46:821–831
Lee J, Kim SS (2010) An overview of cyclophilins in human cancers. J Int Med Res 38:1561–1574
Connern CP, Halestrap AP (1992) Purification and N-terminal sequencing of peptidyl-prolyl cis–trans-isomerase from rat liver mitochondrial matrix reveals the existence of a distinct mitochondrial cyclophilin. Biochem J 284:381–385
Linard D, Kandlbinder A, Degand H, Morsomme P, Dietz KJ, Knoops B (2009) Redox characterization of human cyclophilin D: identification of a new mammalian mitochondrial redox sensor? Arch Biochem Biophys 491:39–45
Rieusset J, Fauconnier J, Paillard M, Belaidi E, Tubbs E, Chauvin MA, Durand A, Bravard A, Teixeira G, Bartosch B, Michelet M, Theurey P, Vial G, Demion M, Blond E, Zoulim F, Gomez L, Vidal H, Lacampagne A, Ovize M (2013) Disruption of cyclophilin D-mediated calcium transfer from the ER to mitochondria contributes to hepatic ER stress and insulin resistance. Hepatology 58:1195
Huang HM, Chen HL, Gibson GE (2010) Thiamine and oxidants interact to modify cellular calcium stores. Neurochem Res 35:2107–2116
Javadov S, Karmazyn M, Escobales N (2009) Mitochondrial permeability transition pore opening as a promising therapeutic target in cardiac diseases. J Pharmacol Exp Ther 330:670–678
Wang X, Wang B, Fan Z, Shi X, Ke ZJ, Luo J (2007) Thiamine deficiency induces endoplasmic reticulum stress in neurons. Neurosciences 144:1045–1056
Uchino H, Hatakeyama K, Morota S, Tanoue T, Nishiyama T, Usui D, Taguchi C, Suzuki M, Hansson MJ, Elmér E (2013) Cyclophilin-D inhibition in neuroprotection: dawn of a new era of mitochondrial medicine. Acta Neurochir 118:311–315
Tsujimoto Y, Shimizu S (2007) Role of the mitochondrial membrane permeability transition in cell death. Apoptosis 12:835–840
Zhu X, Hogan SP, Molkentin JD, Zimmermann N (2016) Cyclophilin D regulates necrosis, but not apoptosis, of murine eosinophils. Am J Physiol Gastrointest Liver Physiol 310:G609–G617
Chornyy S, Parkhomenko J, Chorna N (2007) Thiamine deficiency caused by thiamine antagonists triggers upregulation of apoptosis inducing factor gene expression and leads to caspase 3-mediated apoptosis in neuronally differentiated rat PC-12 cells. Acta Biochim Pol 54:315–322
Rasola A, Bernardi B (2007) The mitochondrial permeability transition pore and its involvement in cell death and in disease pathogenesis. Apoptosis 12:815–833
Galluzzi L, Blomgren K, Kroemer G (2009) Mitochondrial membrane permeabilization in neuronal injury. Nat Rev Neurosci 10:481–494
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares no conflicts of interest on this work.
Rights and permissions
About this article
Cite this article
Bâ, A. Alcohol and thiamine deficiency trigger differential mitochondrial transition pore opening mediating cellular death. Apoptosis 22, 741–752 (2017). https://doi.org/10.1007/s10495-017-1372-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10495-017-1372-4