Abstract
Although the research on specialty mental health probation (SMHP) is promising, there have been no randomized controlled trials (RCT) of the prototypical model advanced in the research literature and little focus on SMHP implementation. This study assesses the adoption of SMHP in two counties and examines its impact on mental health and criminal justice outcomes. Researchers conducted a RCT within a hybrid implementation-effectiveness study to examine intervention adoption as well as mental health treatment engagement and criminal justice outcomes for 100 individuals with serious mental illnesses on probation in one rural and one urban county in a southeastern state. Randomization produced equivalent treatment (n = 47) and control (n = 53) groups with no statistically significant differences between groups on demographic or background characteristics. Compared to standard probation officers, SMHP officers addressed the mental health needs of individuals with serious mental illness (i.e., adoption) at higher rates (p < 0.001). Compared to individuals on standard caseloads, individuals on SMHP had a higher rate of mental health engagement (e.g., mental health assessment, attending treatment appointment; p < 0.050); however, more individuals on SMHP caseloads had a new crime violation during follow-up compared with individuals on standard caseloads (p < 0.01). In conclusions, results suggest successful adoption of the intervention and increased mental health engagement among those on SMHP caseloads. Results are consistent with the mixed findings on the impact of SMHP on improving criminal justice outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Results from a Hybrid Implementation: Effectiveness Study of Specialty Mental Health Probation
The over-representation of people with mental illnesses in the criminal justice system is well-documented (Gottfried & Christopher, 2017; Prins, 2014; Sirdifield, 2012). Consequently, corrections agencies often become default care coordinators for individuals with mental illnesses and are tasked with connecting these individuals to necessary services and supports while also enforcing the terms of supervision (i.e., the conditions of probation; Hsieh et al., 2015). Although ensuring access to mental health treatment and other supports is important across all intercepts of the criminal justice system (e.g., jails, community corrections, prison; Munetz & Griffin, 2006), given that the number of individuals with mental illnesses on probation far surpasses the number incarcerated in jails or prisons (Maruschak & Minton, 2020), ensuring access to behavioral health treatment and other supports is particularly important for probation officers. To this end, specialized mental health probation (SMHP) approaches have emerged to address the complex needs of those on probation who have serious mental illnesses (SMI; Council of State Governments, 2002; Skeem & Eno Louden, 2006; Skeem et al., 2006).
Specialty mental health probation (SMHP) approaches aim to improve mental health and criminal justice outcomes among adults on probation with SMI. Although there is some variation in the structure of SMHP approaches, there are five core elements that define the model: (1) reduced caseload size; (2) designated caseloads for adults with mental illnesses; (3) ongoing mental health training for specialty mental health probation officers; (4) use of a problem-solving orientation to supervision (e.g., working with the individual to address barriers to compliance with the terms of probation); and (5) greater interface with resource providers to address the needs of those with mental health and other needs (Skeem et al., 2006). To date, three peer-reviewed studies examined the effectiveness of this prototypical SMHP model (Manchak et al., 2014; Skeem et al., 2017; Wolff et al., 2014).
These studies used quasi-experimental designs and advanced statistical methods (e.g., hierarchical logistic modeling and propensity score matching) to examine the effectiveness of SMHP. Findings suggest that, compared to adults with mental illnesses on standard caseloads, those receiving SMHP had a lower likelihood of re-arrest, fewer jail days, and fewer probation violations resulting in arrest. However, findings on the number of general probation violations were mixed in that one study reported greater violations among those on mental health caseloads, one study reported fewer violations, and one study reported no effect of SMHP on probation violations (Manchak et al., 2014; Skeem et al., 2017; Wolff et al., 2014). Regarding mental health outcomes, individuals on SMHP caseloads were more likely to be engaged in mental health and substance use treatment and showed greater improvements in mental health symptoms and other quality of life measures (Manchak et al., 2014; Wolff et al., 2014).
Although the evidence supporting the effectiveness of SMHP is growing, critical gaps in the research persist. First, although the aforementioned studies of SMHP employed rigorous statistical analyses to account for potential differences in treatment and comparison groups (Manchak et al., 2014; Skeem et al., 2017; Wolff et al., 2014), a true experimental design is needed to sufficiently control for threats to internal validity and to ensure group equivalence. Second, two of the three articles reported on the same longitudinal study in which propensity score matching was used to compare traditional caseloads with specialty mental health caseloads (Manchak et al., 2014; Skeem et al., 2017). Consequently, the field is in need of additional research on the efficacy of the SMHP model.
Third, and most notably, there has been little systematic study of the implementation of SMHP and this is a problem because the lack of focus on implementation can delay the speed of translation from research knowledge into routine uptake (Curran et al., 2012). SMHP is a complex intervention that attends to and balances mental health and criminal justice needs within a community corrections setting and requires probation officers to apply knowledge and practice skills beyond what may be typically expected. Given the complexity of the model, it is important to assess the degree to which SMHP can be implemented successfully.
A key indicator of implementation is adoption, which refers to “the intention, initial decision, or action to try to employ an innovation or evidence-based practice” (Proctor et al., 2011, p. 69). Although adoption can be measured at the agency level (e.g., probation agency’s decision to adopt the model), it is important to assess behaviors and actions indicative of model implementation at the officer level (e.g., addressing the mental health needs of individuals with SMI on their caseloads).
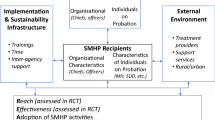
Given these significant gaps in the SMHP literature—the lack of randomized controlled trials of SMHP and the lack of research on SMHP’s implementation—this article reports findings from a hybrid type I implementation effectiveness study (Curran et al., 2012) that examines one essential implementation outcome—adoption—and the impact of SMHP on probation violations and treatment engagement in the context of a small-scale randomized controlled trial. This study addresses the following research objectives: (a) to examine the adoption of SMHP practices (i.e., addressing mental health needs of individuals on probation); (b) to compare mental health treatment engagement (e.g., medication access, psychiatric assessments, appointment attendance) between individuals on SMHP caseloads and those on standard probation caseloads; and (c) to compare probation violations and violation types between individuals on SMHP caseloads and those on standard probation caseloads.
Method
Study Design
The design of the SMHP intervention was consistent with the prototypical model advanced by Skeem et al. (2006), including reduced caseload size, designated mental health caseloads, ongoing mental health training for SMHP officers, coordination with internal and external resources to address individuals’ needs, and using a problem-solving orientation to address probation compliance. On average, SMHP officers’ caseload size was 47 (SD = 10.42) and standard officers’ caseload size was 67 (SD = 11.09). Although the goal was to create designated mental health caseloads comprised exclusively of individuals with SMI, during the pilot phase of SMHP, officers had mixed caseloads (i.e., some individuals with SMI and some without SMI). SMHP officers completed approximately 60 h of mental health training, including: (1) five web-based training modules about mental health conditions, medications, symptoms, and protocol for referrals; (2) Crisis Intervention Team training (Compton et al., 2008); and (3) a series of in-person trainings and booster sessions provided by the research team.
To enhance the implementation of SMHP’s core components, the research team developed two strategies. First, the research team used monthly clinical case consultation—monthly meetings between probation officers, probation chiefs, and a licensed clinical social worker—to enhance SMHP officers’ ability to apply the knowledge and skills learned in training, guide officers on ways to engage in problem-solving, and facilitate and reinforce SMHP officers’ collaboration and coordination with treatment providers. Second, the research team hosted stakeholder engagement events as the SMHP initiative was being launched in each county. During these events, treatment providers and providers of other community resources were invited to attend and meet the SMHP officers, hear more about the SMHP program, and engage in informal networking. In addition, research team members continued to broker contact between SMHP officers and agencies over the course of the study. These implementation strategies, as well as the core components of the SMHP model, enhance officers’ ability to address the mental health needs of individuals with SMI, which is the primary SMHP objective.
Standard officers (i.e., the control group) differed from SMHP officers in that standard probation officers received only basic mental health training and were expected to follow routine agency protocol for addressing mental health needs of individuals on their caseloads (i.e., referral for services). Standard probation officers did not receive additional mental health training or a reduction in caseload size. In addition, they were not expected to coordinate and collaborate with treatment providers to the same extent as SMHP officers.
The research team used a hybrid type I design (Curran et al., 2012) to examine the adoption of SMHP (Proctor et al., 2011) and its impact on mental health and criminal justice outcomes. The effectiveness arm of the hybrid study involved a randomized control trial (RCT) of SMHP in one urban and one rural county in a southeastern state. In each county, adults on probation who met study eligibility criteria and agreed to participate in the study were randomly assigned to either the treatment group (SMHP) or the control group (standard probation). The implementation arm of the study examined the adoption of SMHP in each county. Specifically, the research team examined the adoption of the SMHP model by comparing the extent to which officers addressed the mental health needs of individuals with SMI between SMHP officers and standard probation officers. Adoption was defined and measured using administrative data documenting the number of mental health-related action steps (e.g., obtain mental health assessment) in which officers engaged their probationers during supervision meetings.
Study Recruitment and Enrollment
Study recruitment and enrollment occurred in two phases. First, using administrative records, the research team identified individuals on probation caseloads who screened positive for a potential mental health disorder as evidenced by the state’s brief mental health screen (Van Deinse et al., 2018), had at least 9 months left on their probation term, and were not already assigned to a specialty caseload (e.g., gang, domestic violence, sex offender). The research staff contacted the probation officers of each potentially eligible individual and asked them to use a brief script to discuss the pilot study. If an individual expressed interest in hearing more about the study, the probation officer invited the research team member to meet with the individual immediately after the individual’s next scheduled probation supervision meeting. Beyond sharing the description of the study, probation officers were not involved in any recruitment or enrollment activities and did not participate in the research team’s recruitment meetings.
During the study recruitment and intake process, research team members met privately with individuals to describe the study and to review informed consent documents. Individuals willing to participate were then given a brief study competency quiz to ensure an adequate understanding of the study’s purpose, procedures, risks, and benefits before proceeding with the consent and enrollment process. After consent was obtained, the research staff used a diagnostic assessment tool, the Mini International Neuropsychiatric Interview, a well known standardized tool with established reliability and validity (MINI; Sheehan et al., 1998), to confirm that the individual met the criteria for at least one of the following diagnoses: major depressive disorder, bipolar disorder, psychotic disorder, and/or post-traumatic stress disorder (PTSD).
Then, demographic information was collected and a battery of standardized measures was administered, including assessments of substance use, mental health symptoms, interpersonal and family supports, mental health stigma, relationship between the individual and their probation officers, and the number and nature of personal and formal support networks. Data collection occurred between September 2014 and April 2016. Additionally, administrative data pertaining to participants’ probation violations and data regarding mental health-related action steps across multiple domains were obtained from the state’s Department of Public Safety at the conclusion of the study.
This study was approved by the Institutional Review Board at the University of North Carolina at Chapel Hill.
Sample
Over the course of the study, administrative data from by the state’s Department of Public Safety identified 758 individuals in the two counties who were potentially eligible for the study, 32% (n = 242) of whom were referred by probation officers to the research team to confirm study eligibility, describe the research study, and complete the informed consent process and baseline data collection. Of these 242 individuals referred for screening, 26% (n = 64) were deemed not eligible for the study (e.g., transferred out of county, did not meet criteria for mental illness, etc.).
Of the 178 individuals who were eligible for the study, 35% (n = 63) did not consent to participate, 2% (n = 3) lacked the capacity to consent for the study (e.g., did not understand what they were being asked to do); and 63% (n = 112) consented to the study. Of the 112 individuals who provided informed consent and completed baseline measures, 9% (n = 10) were later found to be ineligible for or were otherwise excluded from the study (e.g., were assigned to a different specialty caseload, preferred not to switch probation officers), and 2% (n = 2) withdrew consent. Our final study sample includes 100 individuals who were randomized to either specialty mental health probation (n = 47) or remained in regular probation (n = 53).
Study participants had a mean age of 35.95 (SD = 12.53) and just over half (54%, n = 54) were male. A majority (67%, n = 67) of the sample had at least a high school education and more than half were unemployed (53%, n = 53). Approximately 43% (n = 43) of individuals identified as White or Caucasian, 39% (n = 39) identified as Black or African American, 4% (n = 4) identified as American Indian/Alaskan Native, 6% (n = 6) identified as Hispanic and 13% (n = 13) identified belonging to a racial category other than those provided.
At the time of enrollment in the study, nearly half (48%, n = 48) had health insurance, and 69% (n = 69) had a prior probation term. The mean length of the current probation sentence was 25.04 months (SD = 13.72). Over half (54%, n = 54) were enrolled in mental health services at the time of study enrollment and the most common primary mental health diagnosis was bipolar disorder (63%, n = 63), followed by depression (25%, n = 25), psychosis (6%, n = 6), and PTSD (6%, n = 6) (Fig. 1).
Measures
To assess differences between the treatment and control groups, the research team collected data pertaining to demographic information, prior probation sentence, self-report service engagement, and administered a battery of standardized measures including: the Symptom Checklist-10 (Rosen et al., 2000), the Dual Role Relationship Inventory Revised (Skeem et al., 2007), and the Internalized Stigma of Mental Illness (ISMI; Ritsher et al., 2003). The research team also obtained data pertaining to criminogenic risk, needs, and supervision level derived from the state’s risk and needs assessment.
In addition, administrative data were obtained from the Department of Public Safety at the end of the study period. The data included probation officer action steps (e.g., referral to mental health treatment or substance use services) and probation violations for all 100 study participants. Action steps are discrete follow-up tasks that probation officers and their supervisees agree to during supervision meetings, such as attend substance use treatment meetings, participate in a mental health evaluation, or participate in mental health treatment. The probation officer then follows up on the status of these tasks (e.g., complete, incomplete) at subsequent probation supervision meetings.
In addition, data regarding probation violations were also obtained and included the date and type of violation. Action steps and probation violations included in the final sample were those that occurred during a 1-year follow-up period for each study participant.
Demographic Variables
Age was collected at baseline and was a continuous variable measured in years. Race was a categorical variable with six options: White/Caucasian, Black/African American, American Indian/Alaskan Native, Asian, Native Hawaiian/Pacific Islander, or Other. Gender was a dichotomous variable (i.e., male or female) and education was a categorical variable with the following options: (1) none; (2) elementary school; (3) middle school; (4) high school or GED; (5) some college, associates, or technical degree; (6) bachelor’s degree; or (7) graduate or professional degree. Employment was a categorical variable with five values: (1) unemployed, (2) employed part-time, (3) employed full time, (4) disabled or unable to work, or (5) student. Health insurance status was a dichotomous variable indicating whether or not an individual had health insurance of any type.
Officer Adoption of SMHP
Adoption refers to “the intention, initial decision, or action to try to employ an innovation or evidence-based practice” (Proctor et al., 2011, p. 69). For the purposes of this study, adoption was conceptualized as the uptake of SMHP within the probation agency, defined by the degree to which designated SMHP officers initiated action steps addressing individuals’ mental health needs during probation supervision. During supervision, all officers, including those not assigned a mental health caseload, are expected to follow up on mental health needs for any individual who has a positive screen on the state’s mental health screening tool. All officers are then expected to work with their supervisees to establish action steps related to treatment engagement and adherence, such as attending a mental health assessment and medication adherence. Given the core components of the SMHP model (e.g., enhanced mental health training for SMHP officers, reduced caseload size, focus on problem-solving), the research team conceptualized SMHP adoption as SMHP officers’ initiation and frequency of addressing mental health among those on their caseload as measured by greater utilization of mental health action steps compared to standard probation officers.
Data pertaining to action steps were obtained from officers’ electronic case plans where all officers document proceedings from each of the probation supervision meetings, including whether action steps were initiated as well as the status of those action steps. An action step was coded as a mental health action step if it indicated one of the following: (a) obtain a mental health evaluation, (b) attend a mental health assessment as scheduled, (c) participate in psychiatric counseling, and (d) follow all instructions for any medications prescribed and provide officer with verification of prescriptions.
Mental Health Treatment Engagement
For the effectiveness arm of the study, the same administrative data set was used to examine mental health and criminal justice outcomes—mental health treatment engagement and probation violations. As described above, probation officers work with individuals on their caseloads to initiate mental health action steps related to treatment engagement, assessment, and adherence. For the purposes of this study, the effectiveness outcome of mental health treatment engagement refers to whether or not individuals on probation completed their mental health actions steps, such as obtaining a mental health assessment or attending treatment appointments. A mental health action step was determined to be successfully completed if it was marked in the case plan as being achieved.
Addressing Additional Life Areas
Similarly, we used administrative data to examine other areas in which probation officers and their supervisees initiated and engaged in action steps in a number of other life domains, including substance use, education, employment, family relationships, financial independence, prosocial supports and legal assistance, when needed. For each of these additional domains, we were able to determine if an action step (e.g., obtain GED or vocational training) was initiated and completed. Evaluating these additional domains also provided an opportunity to assess the extent to which treatment and control groups documented the initiation and completion of action steps equally across all domains.
Probation Violations
Probation violations occur when an individual fails to comply with the terms of supervision, including committing new crimes. In this study, formal probation violations (i.e., those filed with the court system) were examined at 6 and 12 months after study intake for each individual by calculating: (a) the total number of any type of violations within the 1-year follow-up period, (b) the total number of violations due to new crimes (e.g., misdemeanor or felony conviction) within the follow-up period, and (c) the total number of technical violations (e.g., curfew violations, failure to comply with terms of supervision, positive drug and alcohol tests). The research team also calculated the total number of individuals in the treatment and control groups who had at least one of each type of violation.
Data Analysis
Univariate descriptive statistics were used to examine the characteristics of the total sample and bivariate statistics were used to examine potential group differences between individuals randomly assigned to SMHP and those assigned to standard probation. Pearson’s chi-square tests and Fisher’s Exact tests were used to explore the associations between categorical variables (e.g., group assignment and gender) and independent samples t-tests were used to examine mean differences in continuous variables. Analyses were performed on the entire sample and then repeated to examine results in the urban and rural counties separately. Lastly, given the nested data (i.e., probationers nested within probation officers) we computed intraclass correlation coefficients (ICC) to determine if more sophisticated models were needed to account for dependency among observations. Results of the ICC were not statistically significant and produced values close to 0. All statistical tests were conducted using Stata 16 (StataCorp, 2019) and two-tailed tests with alpha set at 0.05 were used.
Results
The following section summarizes results from bivariate analyses of study randomization, adoption of SMHP, mental health treatment engagement, and probation violations. In addition to aggregate findings, the results are separated by rural and urban county. Of the 100 individuals in the sample, 47 were randomly assigned to SMHP (rural county, n = 21; urban county, n = 26) and 53 were randomly assigned to standard probation (rural county, n = 20; urban county, n = 33). Between the two counties there were four SMHP officers and participants in the treatment group were randomly assigned to one of the two SMHP officers in their respective counties. Individuals assigned to standard probation were assigned to the next available probation officer in their county (n = 35). Randomization of the 100 individuals was successful such that characteristics between the treatment and control groups were equivalent, balanced, and comparable. That is, there were no statistically significant differences between the two groups in terms of age, education, gender, race, employment status, previous probation sentence, length of probation sentence, enrollment in mental health services at baseline, mental health diagnosis, and other attributes (see Table 1). Further, there were no statistically significant differences in risk, need, and supervision levels among those in the treatment group compared to the standard probation group.
To examine the adoption of SMHP, the research team compared the number of cases in which mental health actions steps were initiated (i.e., the number of individuals with whom officers addressed mental health needs; Table 2) in the treatment and control groups in both the rural and urban counties. SMHP officers initiated mental health action steps with 84.78% (n = 39) of the individuals on their caseloads compared to standard probation officers who initiated mental health action steps with 30.19% (n = 6) of the individuals on their caseloads (X2 = 29.73, df = 1, p < 0.001). These results were consistent in both the rural and urban counties (Table 3). Notably, there were no statistically significant differences in the number of cases in which action steps were completed in other life areas (e.g., substance use, employment, financial).
To examine whether SMHP promotes engagement in mental health treatment, the research team examined the percentage of mental health action steps that were successfully completed by individuals with SMI on SMHP caseloads compared to those on standard caseloads (Table 2). Of the individuals who established mental health actions steps with their officers, 79.49% (n = 31) of those on SMHP caseloads completed their mental health action steps compared with 50% (n = 8) of those on standard caseloads (X2 = 3.85, df = 1, p < 0.050). These results were consistent in both the rural and urban counties (Table 3). There were no statistically significant differences between the treatment and control group in the number of individuals who completed their action steps in other life areas.
Regarding probation violations, the number of total probation violations, technical violations, and violations due to new crimes were comparable across the two groups (Table 4). Similarly, there were no statistically significant differences in the number of individuals with any type of violation or technical violation between the SMHP group and the standard probation group. However, a higher percentage of those in the SMHP group (17.02%, n = 8) had a violation due to new crime compared to the percentage of individuals in the standard probation group (1.89%, n = 1; p < 0.01). These results were consistent in both the rural and urban counties (Table 5).
Discussion
This hybrid type I study implemented a RCT to examine adoption of SMHP and the impact of SMHP on mental health and criminal justice outcomes. The analysis involved administrative data available on all study participants at two follow-up points. Results were consistent between the rural and urban counties and indicated that, compared with standard probation officers, SMHP officers are more likely to address the mental health needs of individuals with SMI on their caseloads and initiate action steps focused on mental health treatment engagement and adherence. However, both SMHP officers and standard probation officers initiated action steps in other areas (e.g., substance use, financial, family) at equal rates. Additionally, individuals with SMI who were assigned to SMHP caseloads had higher rates of completing their mental health action steps compared to those who were assigned to standard probation, suggesting that SMHP increases mental health treatment engagement.
With regard to criminal justice outcomes, there were few differences between SMHP caseloads and standard caseloads with respect to violations. However, a higher percentage of individuals on SMHP caseloads had violations due to a new crime. These findings are consistent with the peer-reviewed research literature on SMHP, which indicates greater mental health treatment engagement and mixed findings regarding criminal justice outcomes (Manchak et al., 2014; Skeem et al., 2017; Wolff et al., 2014).
Limitations
Despite the strengths of this study, there are several limitations to consider. First, given barriers to obtaining verified rates of mental health treatment engagement from service providers or other administrative data sources, data regarding treatment engagement (i.e., successfully completing a mental health treatment action step) were based on officer- and individual self-report. It is possible that individuals may have reported to their officers mental health treatment engagement inaccurately, thus, potentially inflating estimates. However, in many cases, probation officers are tasked with verifying appointments and attendance with behavioral health service providers, particularly with individuals mandated to treatment.
Although the findings from the ICC were not statistically significant, it is still important to note the potential limitation associated with nested data. Individuals on probation are nested within probation officer caseloads such that officers may initiate mental health action steps across their caseload and contribute a much higher number of action steps to the data. Consequently, differences in initiated and completed mental health action steps could be due to one SMHP officer contributing a large number of initiated and completed mental health action steps and not necessarily because the SMHP intervention impacts this outcome (i.e., overestimating the impact of the intervention on outcomes). Nesting could be addressed by using a multilevel model, such as hierarchical linear modeling. Such an approach was not used for this study because of the small sample size, lack of statistical power, and non-significant ICCs. In addition, this study examined the percentage of individuals with whom probation officers established action steps rather than the average number of action steps per person, thus eliminating problematic nesting effects from a given probation officer imitating multiple action steps per person.
In addition, it is possible that differences in record keeping (e.g., entering action steps into the officers’ records management system) may be a confounding factor impacting study results. Specifically, it is possible that the SMHP officers had more consistent record keeping and follow-up practices compared to the standard probation officers. However, given the lack of statistically significant differences in initiating and completing action steps in other life areas (e.g., substance use, employment, financial) as reported above, it is unlikely that the difference in mental health actions steps initiated and completed is merely due to better record keeping practices of SMHP officers.
Further, this study uses a single variable—initiation of mental health action steps—to measure adoption of SMHP. Although assessing the degree to which SMHP officers addressed mental health needs of those on their probation caseloads is a critical first step, a more robust assessment of implementation is needed. SMHP is a complex and multi-component intervention that spans the mental health and criminal justice systems. Consequently, future studies should assess the implementation of the core components of SMHP using implementation outcome taxonomies (e.g., Proctor et al., 2011). For instance, as the empirical base for SMHP expands, researchers should develop a fidelity instrument that assesses implementation of each of the five core components. Although some components can be objectively measured (e.g., designated mental health caseloads, reduced caseload size) the fidelity instrument will need to clearly specify implementation outcomes for a problem-solving orientation, ongoing mental health training, and interfacing with internal and external resources.
Lastly, although implementation of SMHP was intended to adhere to the core components of the prototypical model advanced by Skeem et al. (2006), caseloads were not exclusively populated with individuals with SMI (i.e., a mix of individuals with SMI and those without SMI). Thus, although our findings cannot speak to the outcomes of SMHP that adheres to full fidelity with respect to this aspect of the prototypical model, our findings illuminate the impact of SMHP when delivered with partial fidelity in regards to designated caseloads. In this context, our findings are promising in that, even without caseload fidelity, SMHP resulted in superior mental health engagement outcomes for our sample.
Implications
Despite these limitations, this study makes notable contributions to the research on SMHP. First, given the complexity of the SMHP model and other similar interventions that span behavioral health and criminal justice systems, it is important to measure implementation outcomes (e.g., adoption) in addition to intervention outcomes. SMHP requires that probation officers obtain a specialized skillset and knowledge base beyond their original scope of practice (i.e., enforcing the terms of supervision). For instance, SMHP officers ask individuals on their caseloads about their mental health, attempt to discern symptoms of mental illness from what may be perceived as non-compliance, interface with mental health service providers to navigate service connections, and apply de-escalation techniques as needed (Eno Louden et al., 2012; Van Deinse et al., 2020). Assessing the uptake of these enhanced skillsets into routine probation officer practice necessitates discrete measures of adoption or uptake of SMHP practices.
Second, results in this study, which is the first randomized trial of SMHP, support the findings from the three previous studies of prototypical SMHP (Manchak et al., 2014; Skeem et al., 2017; Wolff et al., 2014). Taken together the evidence on SMHP effectiveness is mixed. Results from each of the studies are consistent in terms of showing improvements in mental health-related outcomes (e.g., treatment engagement). However, evidence that SMHP reduces future criminal justice involvement is insufficient and, in some cases, suggests that those on SMHP caseloads have a greater number of general violations but fewer arrests and jail days (Manchak et al., 2014; Skeem et al., 2017; Wolff et al., 2014).
This finding is consistent with other “first generation” interventions focused on connecting individuals to mental health treatment to reduce recidivism (Epperson et al., 2014). The body of research indicating that mental illness alone is not a direct and causal predictor of criminal justice involvement (Bonta et al., 1998, 2014; Epperson et al., 2014) helps explain why targeting mental health treatment-focused interventions for individuals with mental illnesses has had no consistent impact on criminal justice outcomes. Although demonstrated success in enhancing service connection and mental health treatment engagement is important, interventions with co-primary mental health and criminal justice aims should consider a public health approach that addresses individual-, interpersonal-, and community-level antecedents of criminal justice involvement (Epperson et al., 2014).
Conclusion
SMHP has emerged as a promising practice to address the mental health needs of individuals with SMI who are on probation. This study is the first to use a randomized controlled trial to examine the impact of SMHP on implementation and intervention outcomes—namely, adoption of an essential aspect of SMHP (i.e., addressing mental health needs of supervisees with SMI), mental health treatment engagement, and probation violations. Results were consistent with the existing literature noting increased mental health engagement but no effect or a negative effect on probation violations. Probation agencies should consider SMHP a viable option for addressing mental health treatment engagement among this population. However, given the dearth of research on SMHP and mixed findings regarding the impact of SMHP on criminal justice outcomes, additional large-scale studies, which include standardized fidelity assessments, are needed.
Data Availability
Data from this study will be made available by the Principal Investigator (PI) as freely as possible while safeguarding the confidentiality of the data and privacy of participants. Researchers with a convincing scientific interest in the data can contact the study PI and establish a data sharing agreement.
References
Bonta, J., Blais, J., & Wilson, H. (2014). A theoretically informed meta-analysis of the risk for general and violent recidivism for mentally disordered offenders. Aggression and Violent Behavior, 19, 278–287. https://doi.org/10.1016/j.avb.2014.04.014
Bonta, J., Law, M., & Hanson, K. (1998). The prediction of criminal and violent recidivism among mentally disordered offenders: A meta-analysis. Psychological Bulletin, 123(2), 123–142. https://doi.org/10.1037/0033-2909.123.2.123
Compton, M. T., Bahora, M., Watson, A. C., & Oliva, J. R. (2008). A comprehensive review of extant research on crisis intervention team (CIT) programs. Journal of the American Academy of Psychiatry and the Law Online, 36(1), 47–55.
Council of State Governments. (2002). Criminal justice/mental health consensus project. Council of State Governments.
Curran, G. M., Bauer, M., Mittman, B., Pynt, J., & Stetler, C. (2012). Effectiveness-implementation hybrid designs: Combining elements of clinical effectiveness and implementation research to enhance public health impact. Medical Care, 50(3), 217–226. https://doi.org/10.1097/mlr.0b013e3182408812
Eno Louden, J., Skeem, J. L., Camp, J., Vidal, S., & Peterson, J. (2012). Supervision practices in specialty mental health probation: What happens in officer–probationer meetings? Law and Human Behavior, 36(2), 109. https://doi.org/10.1037/h0093961
Epperson, M. W., Wolff, N., Morgan, R. D., Fisher, W. H., Frueh, B. C., & Huening, J. (2014). Envisioning the next generation of behavioral health and criminal justice interventions. International Journal of Law and Psychiatry, 37(5), 427–438. https://doi.org/10.1016/j.ijlp.2014.02.015
Gottfried, E. D., & Christopher, S. C. (2017). Mental disorders among criminal offenders: A review of the literature. Journal of Correctional Health Care, 23(3), 336–346. https://doi.org/10.1177/1078345817716180
Hsieh, M.-L., Hafoka, M., Woo, Y., van Wormer, J., Stohr, M. K., & Hemmens, C. (2015). Probation officer roles: A statutory analysis. Federal Probation, 79(3), 20–37. https://doi.org/10.1177/0093854814562642
Manchak, S. M., Skeem, J. L., Kennealy, P. J., & Eno Louden, J. (2014). High-fidelity specialty mental health probation improves officer practices, treatment access, and rule compliance. Law and Human Behavior, 38(5), 450. https://doi.org/10.1037/lhb0000076
Maruschak, L. M., & Minton, T. D. (2020, August). Correctional populations in the United States, 2017–2018. U.S. Department of Justice. Retrieved from https://www.bjs.gov/content/pub/pdf/cpus1718.pdf
Munetz, M. R., & Griffin, P. A. (2006). Use of the sequential intercept model as an approach to decriminalization of people with serious mental illness. Psychiatric Services, 57(4), 544–549. https://doi.org/10.1176/ps.2006.57.4.544
Prins, S. J. (2014). Prevalence of mental illnesses in US state prisons: A systematic review. Psychiatric Services, 65(7), 862–872. https://doi.org/10.1176/ps.2006.57.4.544
Proctor, E., Silmere, H., Raghavan, R., Hovmand, P., Aarons, G., Bunger, A., … Hensley, M. (2011). Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Administration and Policy in Mental Health and Mental Health Services Research, 38(2), 65–76.https://doi.org/10.1007/s10488-010-0319-7
Ritsher, J. B., Otilingam, P. G., & Grajales, M. (2003). Internalized stigma of mental illness: Psychometric properties of a new measure. Psychiatry Research, 121(1), 31–49. https://doi.org/10.1016/j.psychres.2003.08.008
Rosen, C., Drescher, K. D., Moos, R. D., Finney, J. W., Murphy, R. T., & Gusman, F. (2000). Six and ten item indices of psychological distress based on the Symptom Checklist-90. Assessment, 7(2), 103–111. https://doi.org/10.1177/107319110000700201
Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., ... & Dunbar, G. C. (1998). The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59, 22–33.
Sirdifield, C. (2012). The prevalence of mental health disorders amongst offenders on probation: A literature review. Journal of Mental Health, 21(5), 485–498. https://doi.org/10.3109/09638237.2012.664305
Skeem, J. L., Emke-Francis, P., & Louden, J. E. (2006). Probation, mental health, and mandated treatment a national survey. Criminal Justice and Behavior, 33(2), 158–184. https://doi.org/10.1177/0093854805284420
Skeem, J. L., & Eno Louden, J. (2006). Toward evidence-based practice for probationers and parolees mandated to mental health treatment. Psychiatric Services, 57(3), 333–342. https://doi.org/10.1176/appi.ps.57.3.333
Skeem, J. L., Eno Louden, J. E., Polaschek, D., & Camp, J. (2007). Assessing relationship quality in mandated community treatment: Blending care with control. Psychological Assessment, 19(4), 397–410. https://doi.org/10.1037/1040-3590.19.4.397
Skeem, J. L., Manchak, S., & Montoya, L. (2017). Comparing public safety outcomes for traditional probation vs specialty mental health probation. JAMA Psychiatry, 74(9), 942–948. https://doi.org/10.1001/jamapsychiatry.2017.1384
Stata Corp. (2019). Stata statistical software: Release 16. StataCorp LLC.
Van Deinse, T. B., Crable, E. L., Dunn, C., Weis, J., & Cuddeback, G. (2020). Probation officers’ and supervisors’ perspectives on critical resources for implementing specialty mental health probation. Administration and Policy in Mental Health and Mental Health Services Research. https://doi.org/10.1007/s10488-020-01081-8
Van Deinse, T. B., Cuddeback, G. S., Wilson, A. B., Lambert, M., & Edwards, D. (2018). Using statewide administrative data and brief mental health screening to estimate the prevalence of mental illness among probationers. Probation Journal, 66(2), 236–247. https://doi.org/10.1177/0264550518808369
Wolff, N., Epperson, M., Shi, J., Huening, J., Schumann, B. E., & Sullivan, I. R. (2014). Mental health specialized probation caseloads: Are they effective? International Journal of Law and Psychiatry, 37, 464–472. https://doi.org/10.1016/j.ijlp.2014.02.019
Acknowledgements
The authors would also like to acknowledge Stacey Burgin for project coordination and the NC Department of Public Safety for their leadership and implementation efforts.
Funding
This study was funded by the North Carolina Governor’s Crime Commission. In addition, the first author is supported by the Lifespan/Brown Criminal Justice Research Training Program (National Institute of Drug Abuse [NIDA], R25DA037190).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by TBVD, AG, and GC. The first draft of the manuscript was written by TBVD and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Consent to Participate
Informed consent was obtained from all individual participants included in the study. The informed consent form also indicated that data would be de-identified and shared in aggregate in any future publications.
Ethical Approval
Approval was obtained from the Institutional Review Board at the University of North Carolina at Chapel Hill (8/19/2014; #14-0492).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Dr. Cuddeback was the principal investigator on this study.
Rights and permissions
About this article
Cite this article
Van Deinse, T.B., Givens, A., Cowell, M. et al. A Randomized Trial of Specialty Mental Health Probation: Measuring Implementation and Effectiveness Outcomes. Adm Policy Ment Health 49, 415–428 (2022). https://doi.org/10.1007/s10488-021-01172-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10488-021-01172-0