Abstract
There is increasing recognition that some preschool-aged children suffer from mental health conditions, but little is known about the treatment they receive. Using the 2014 MarketScan Commercial Claims and Encounters database (N = 1,987,759) the study finds that only a small proportion of preschool-aged children receive any behavioral interventions, including psychotherapy, in conjunction with having a filled psychiatric prescription. Nearly all of the preschool-aged children who had psychotropic prescriptions filled had no other claims for treatment, and among those children who had prescriptions for psychotropic medication filled, the vast majority did not have a mental health diagnosis on a claim.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past several decades, there has been increasing acceptance that preschool-aged children may experience mental health symptoms; as a consequence, the importance of early identification and treatment of mental and emotional disorders in young children has gained recognition (Carter et al. 2004; Skovgaard 2010; Howell and Teich 2008). The awareness that young children may have unique, sometimes severe, psychiatric problems requiring developmentally-tailored evaluations and intervention has underscored the need for additional therapeutic models as well as the development of skills and expertise on the part of clinicians who work with the age group (Mayes 1999). A 2002 study of infants, toddlers, and families found that 42% of childcare programs had asked families to withdraw their child because the program was unable to handle the child’s social or emotional problems, such as biting, tantrums, hitting, inconsolable crying, and sleep problems (Zero to Three 2016). A substantial body of literature now demonstrates that several discrete Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) depressive and anxiety disorders can be identified in preschool-aged children; however, since these studies are relatively recent, less work has been done on the development and testing of age-appropriate treatments (Luby 2013).
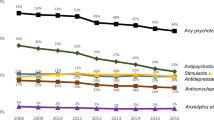
A study of trends in mental health care among children and adolescents (Olfson et al. 2015) found that between 1996 and 2012, the use of psychotropic medications, including stimulants, antidepressants, and antipsychotic agents, almost doubled. Since 2006, antipsychotic medications have increasingly been prescribed to very young children, while provision of assessments and psychosocial interventions for these children remains relatively rare. In one study, less than one-half of young children treated with antipsychotic medication received a mental health assessment (40.8%) or a psychotherapy visit (41.4%), or a visit with a psychiatrist (42.6%) during the year of antipsychotic use (Olfson et al. 2010). Despite growing attention to these issues, national estimates of mental health service utilization by preschool-aged children are limited. Most studies to date have focused on concerns regarding the prescribing of psychotropic medication (Garfield et al. 2015; dosReis et al. 2014; Zito et al. 2000). This issue has important implications because most medications are prescribed without the U.S. Food & Drug Administration (FDA) approval for use with this age group (Vitiello and Jensen 1997). While this practice is common in clinical settings, there are concerns about the safety and effectiveness of using certain psychiatric medications with young children (Zito et al. 2007; Harris 2006).
Recent literature estimates that even though only one-quarter of severely impaired children receive some psychotherapy, the utilization rate of psychotherapy has grown (Olfson et al. 2015). The increase in the utilization of psychotherapy may represent a growing recognition that such interventions are a first-line of treatment for a variety of common mental health conditions, such as disruptive behavior disorders, depression, and anxiety, especially for young children (Olfson et al. 2015; Comer et al. 2013). A meta-analysis of thirty-six controlled trials that empirically evaluated the overall effect of psychosocial treatments on early disruptive behavior problems, as well as potential moderators of treatment response, found that psychosocial treatments, such as Parent Child Interaction Therapy (PCIT) and Triple P (Positive Parenting Program), demonstrated a large and sustained effect on early disruptive behavior problems (Comer et al. 2013). In addition, several small randomized controlled trials of psychotherapeutic treatments for preschool anxiety and depression concluded that age-adjusted psychotherapies be tried as the first line of treatment for preschoolers, although the lack of availability of trained clinicians to provide these psychotherapeutic treatments presents a major challenge (Olfson et al. 2015).
Many parents and caregivers are concerned about their children’s use of strong psychotropic medications and may prefer less invasive interventions, such as psychotherapeutic approaches (dosReis and Myers 2008; Carey 2006). However, although some psychosocial interventions for certain psychiatric diagnoses have been demonstrated to be effective with this age group and are considered by physicians to be a first line of treatment, the extent to which young children receive these treatments either alone or in conjunction with psychotropic medications remains unclear. The purpose of the current study is to extend what is known about mental health treatment for very young children by analyzing recent data drawn from an extensive database of private insurance claims in order to describe the frequency with which various types of mental health services, including both psychotropic medication and psychosocial interventions, are currently utilized by preschool-aged children. Although these young children represent only a very small proportion of the population receiving mental health services in the U.S., understanding the extent of their service use is nevertheless an important concern that has wide-ranging implications for access to mental health care.
Materials and Methods
Data
This study utilizes the 2014 MarketScan Commercial Claims and Encounters database, which includes approximately 43 million commercially insured employees, retirees, and their dependents annually. The database captures approximately 30% of the population in the U.S. with private health insurance. It contains detailed patient-level claims data provided directly by employers and health plans; only preschool-aged children (aged 0–5 in 2014) with full calendar year enrollment were included in this analysis (N = 1,987,759).
The dependent variable is categorical with four mutually exclusive treatment categories: psychotropic prescription filled only, psychotherapy only, both psychotropic prescription filled and psychotherapy, and no mental health treatment. Psychotropic medication use was defined as one or more psychotropic drug prescriptions filled during the year using the pharmacy claims file, which contains the therapeutic class of the medication. The following therapeutic classes, which are commonly used to treat behavioral health disorders, were included to indicate usage of psychotropic medication: antidepressants, antipsychotics, anticonvulsants, antimanic agents, antiparkinsonian agents, anxiolytics/sedatives, hypnotics, benzodiazepines, barbiturates, central nervous system agents-miscellaneous (CNS miscellaneous), and stimulants (see Online Appendix 1 for detailed list). Other mental health services, such as psychotherapy and assessment, were measured by whether the children received any of the following psychotherapy Current Procedural Terminology (CPT) codes: 90804–90819, 90821–90824, 90826–90829, 90845–90847, 90849, 90849, 90853, 90857, 90875, 90876, 90862, 99605 or mental health assessment CPT codes: 90801, 90802, 96101, 96102, 96103, 96105, 96111, 96115, 96118, 96119, 96120, 96150. If the children in the sample had no claims for either any psychotropic medication use or other mental health services (i.e., psychotherapy, assessment) they were categorized as receiving no mental health treatment. These CPT codes, as well as the International Classification of Diseases, Ninth Revision (ICD-9) codes for mental disorders selected for this study, followed the analytic approach established by other researchers (Olfson et al. 2010).
One of the primary independent variables of interest in the empirical model is the mental health diagnosis that was received by the preschool-aged children in the study sample. This variable was measured by whether the children had any of the following diagnoses (ICD-9 codes: 290–319): adjustment disorder; attention deficit/hyperactivity disorder; anxiety disorder; bipolar disorder; communication and learning disorders; depression or mood disorder, not otherwise specified; disruptive behavior disorder; pervasive developmental disorder or mental retardation; schizophrenia and other psychoses; and other mental disorders. (See Appendix Table 5 for the full list of ICD-9 codes.) The analysis also includes indicators for mental health service settings measured by whether the child had any outpatient visit with a mental health diagnosis, any inpatient stay with a mental health diagnosis, and/or any emergency department (ED) visit with a mental health diagnosis. Indicators for mental health service providers were also included in the analysis and were measured by whether the child was seen by either a psychiatrist, psychologist or a psychiatric nurse; therapist; primary care provider (such as pediatrician, family practice, internal medicine, primary care medical doctor, nurse practitioner, or physician assistant) and had a mental health diagnosis; and whether they had been to a mental health facility. The multivariate model controlled for patient age and gender. Descriptive statistics on the study sample and the variables used in the analysis are provided in Table 1.
Methods
Multinomial logistic regression is utilized in the study because the dependent variable is a categorical variable of more than two unordered mutually exclusive outcomes. Of the four treatment categories noted previously, the fourth category, no psychotropic medication or therapy, was used as the reference group for the calculations of the relative risk ratios (RRRs). For each independent variable, this analytic approach produces three RRRs; for example, in the case of an ED visit with a mental health diagnosis, this approach estimates the association of the ED visit with treatment utilization by comparing three logit models simultaneously—(i) psychotropic medication fill only compared to no psychotropic medication or other mental health services (i.e., psychotherapy, assessment); (ii) other mental health services (i.e., psychotherapy, assessment) only compared to no psychotropic medication or psychotherapy/assessment, and (iii) psychotropic medication fill and other mental health services (i.e., psychotherapy, assessment) compared to no psychotropic medication or psychotherapy/assessment.
Results
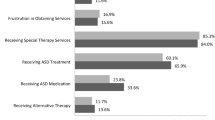
Table 2 displays mental health treatment characteristics of the preschool-aged children who had a diagnosis of any mental health condition. The table shows that 50% of the preschool-aged children with a mental health diagnosis only had a psychotropic prescription filled; approximately 8% of the children received other mental health services only (i.e., psychotherapy or mental health assessment); and 11% of the children received other mental health services and also had a prescription filled for a psychotropic medication. Approximately 31% of them did not receive any psychotherapy/assessment or have a psychotropic prescription filled.
Attention deficit/hyperactivity disorder was the most common mental health diagnosis received by these children (54%). Approximately 98% of the preschool-aged children with any mental health diagnosis had an outpatient visit with a mental health diagnosis. Among psychotropic prescriptions filled, stimulants were the most common medication used (51%); 14% of the children in the sample had a prescription filled for antidepressants, and between 4 and 6% had a prescription filled for antipsychotics, anxiolytics, and benzodiazepines. Approximately 56% of preschool-aged children with any mental health diagnosis were seen by a primary care provider for a mental health related diagnosis; 28% of them had a visit with either a psychiatrist, psychologist or psychiatric nurse; approximately 19% of them were seen by a therapist, and about 1% had an inpatient visit with a mental health diagnosis.
Among the preschool children who had a prescription filled for any psychotropic medication (Table 3), 93% of them received a prescription fill only with no psychotherapy or mental health assessment; approximately 7% received psychotherapy in addition to the medication. Approximately 30% of preschool-aged children with a prescription filled for psychotropic medication had a diagnosis for attention deficit/hyperactivity disorder, and 8% had an anxiety disorder, but the vast majority of them did not have any mental health diagnosis on a claim (62%). About 37% of them had an outpatient visit with a mental health diagnosis. Stimulants were the most common class of psychotropic medication prescriptions filled for them (57%), followed by anxiolytics (28%). While it is known that anxiolytics and benzodiazepines are often used for sedation related to dental procedures, fewer than 1% of these visits were associated with a dental procedure (data not shown); it is also possible that these medications may be used for sedation related to various medical procedures, and for control of epileptic or febrile seizures in very young children. Of the preschool children who had a prescription filled for an anxiolytic, fewer than 2% of them were associated with seizures or epilepsy (data not shown). Approximately 25% of the preschool children with a psychotropic medication filled were seen by a primary care provider, and 12% had a visit with a psychiatrist, psychologist or psychiatric nurse.
Table 4 presents the estimates for the multinomial logistic regression model after accounting for all the variables discussed in the “Data” section. Having a diagnosis of attention deficit/hyperactivity disorder was associated with an increase in the relative risk of only having a psychotropic medication prescription filled by a factor of 2.8, receiving psychotherapy only by a factor of 1.4, and receiving both psychotherapy and psychotropic medication by a factor of 2.9. Diagnosis of pervasive developmental disorder or mental retardation was associated with an increase in the relative risk of having a psychotropic prescription filled only by a factor of 3.4, receiving psychotherapy only by a factor of 1.4, and receiving both psychotherapy and psychotropic medication by a factor of 3.7. Having an outpatient visit with a mental health diagnosis was associated with an increase in the relative risk of only having a psychotropic medication filled by a factor of 1.5, receiving psychotherapy only by a factor of 13, and receiving both psychotherapy and having a psychotropic medication filled by a factor of 8.4. Being seen by a psychologist, psychiatrist or psychiatric nurse was associated with an increase in the relative risk of having only a psychotropic medication filled by a factor of 2.5, whereas the relative risk of receiving psychotherapy only and both psychotherapy and psychotropic medication increased by a factor of 14.8 and 16.3, respectively. Being seen by a primary care provider for a mental health related diagnosis was associated with a reduction in the relative risk of receiving psychotherapy only (relative risk ratio of 0.90).
To check the robustness of the multinomial logit regression, the model was estimated by including mental health assessment as a covariate rather than including it as psychotherapy (part of the dependent variable). The coefficients were very similar to ones reported here. For the purpose of brevity the estimates are not provided but available from the authors upon request.
Discussion
This study found that among privately insured preschool-aged children with a mental health diagnosis on a claim, more than a quarter (31%) received neither assessment/psychotherapy nor psychotropic medications. This finding may be due, in part, to the fact that some state and county government agencies may provide mental health services for children with pervasive developmental disorders, and those encounters would not appear in a commercial claims database (CMS 2016). However, a caregiver’s decision not to treat their young children may also be the result of advice from the child’s physician that “watchful waiting” may be the best course of action (Zeanah 2009). Another interpretation of this result may be that parents were hesitant to place their young children on psychiatric medications, and this treatment modality may be the only treatment provided in the health care setting they accessed (dosReis and Myers 2008).
This paper finds that very few young children with a mental health diagnosis received any behavioral interventions or psychotherapy in tandem with a psychiatric prescription filled (7%). Nearly all of the preschool-aged children who had a prescription for any psychotropic medication filled had no claims for other mental health treatment (93%). Further, among those children for whom a psychotropic medication prescription was filled in 2014, a vast majority of them (62%) did not have a mental health diagnosis on a claim in 2014. This finding, which is consistent with other research (Epstein et al. 2014; Olfson et al. 2010, 2012, 2015), is of concern because some psychiatric medications are used for indications other than those for which the medication was originally approved by the FDA. Although off-label prescribing is common in healthcare, relatively few psychiatric medications are approved for use in young children and their safety and effectiveness with this age group is unknown (Zito et al. 2007).
An analysis of national trends in the office-based treatment of children, adolescents, and adults with antipsychotics, examined the frequency of “FDA-approved visits” (i.e., those visits with a diagnosis for which the prescribed antipsychotic had been approved by the visit year for the age of the patient) and found that for children ages 0–13, there was no approved FDA antipsychotic indication in the overwhelming majority (94%) of visits; however, that study did not include an analysis of the use of psychosocial interventions in addition to psychotropic medications (Olfson et al. 2012). The authors suggest that in light of known safety concerns about certain psychotropic medications and uncertainty over long-term risks and benefits, the increasing use of antipsychotic medications may signal a need to re-evaluate clinical practice patterns and strengthen efforts to educate physicians, especially primary-practice physicians, concerning the known safety and efficacy of these medications.
Even though there are evidence-based psychosocial treatments that are known to physicians (AAP 2016; Kolko and Perrin 2014) and these interventions have been designated as the first line of treatment, caregivers may face challenges with accessing these treatments. The child mental health workforce shortage, as well as staff turnover in mental health clinics, may make it difficult for parents to identify a clinician who could work with their child, let alone one who is qualified to deliver a specific treatment, such as Triple P or PCIT (Dodge and Huang 2008). Training for evidence-based treatments like these can be costly for mental health agencies to implement, and when this factor is combined with high staff turnover in that setting, the cost can escalate because new staff must also be trained (Torrey et al. 2001).
The finding that an outpatient visit with a mental health diagnosis was associated with an increase in relative risk of having only a prescription for psychiatric medication filled by a factor of 1.5 suggests that there is opportunity for improvement in the delivery of pharmacological as well as psychosocial treatments. This is also true for findings of receiving psychotherapy only, and receiving both psychotherapy and having a prescription for psychotropic medication filled, which were associated with an increase by factors of 13 and 8.4, respectively.
Despite the rich data set and rigorous empirical methodology used in this study, the results should be interpreted in the light of a few limitations. First, filling a prescription does not necessarily mean that the child actually received the medication. It is, therefore, possible that the rate of psychotropic medication utilization could be lower than what was estimated in the study. Also, MarketScan only captures prescriptions filled. Prescriptions for psychotropic medications that were written but not filled are not captured by the data either. (The same data limitation applies to follow-up appointments and referrals to specialty providers. If providers gave them, but patient caregivers did not use them, they will not be in the data.) Relatedly, given the common practice of off-label drug use (Brauner et al. 2016), it is possible that the psychotropic medication prescribed to preschool-aged children was not mental health related but for other medical purposes. As mentioned in the “Results” section, utilization of dental procedures, sedation, and services for epileptic or febrile seizures (some of the most common non-mental health related reasons for psychotropic medication use) was very low. While we cannot completely rule out the possibility that these medications were prescribed for other medical reasons, our results suggest that the proportion of psychiatric medications prescribed for this purpose is likely to be quite small. However, future studies should examine this issue further. Second, only claims that were paid for by health insurance were captured in the study, and thus it is possible that psychotherapy components were included in the visit to the service providers, but insurance was only billed for psychotropic medication. It is therefore possible that the utilization of psychotherapy is higher than what was found in the study. Third, the analysis was confined to 2014 data. It is possible, for example, that patients who filled a prescription for a psychotropic medication in 2014 and did not have a visit with a provider with a mental health diagnosis in 2014 had such a visit in 2013. Fourth, the analysis in this study was conducted on commercial claims, and the results may not generalize to individuals with different insurance statuses, such as those on Medicaid or the uninsured. In addition, race/ethnicity information was not available in the commercial claims database. Given its importance as a determinant of mental health service use, examining how race/ethnicity influences the utilization of mental health services by preschool-aged children is an important avenue for future studies to consider.
Conclusion
In recent years, there has been growing recognition that preschool-aged children can suffer from a variety of mental health conditions. By analyzing recent data from an extensive database of private insurance claims, the current study describes the frequency with which various types of mental health services, including both psychotropic medication and psychosocial interventions, are utilized by children in this age group. The findings from this study suggest that only a small proportion of young children receive any behavioral interventions or psychotherapy in conjunction with a prescription psychiatric medication. Nearly all of the preschool-aged children who received a prescription for a psychotropic medication received it with no other treatment, and among those children who were prescribed psychotropic medication, the vast majority did not have a mental health diagnosis on a claim. Given the concerns about the safety and effectiveness of psychiatric medications among young children, the study’s findings raise potential concerns about the children’s mental health workforce shortage, implementing evidence-based practices, and the need for a more integrated and comprehensive approach in treating children with mental health conditions.
References
American Academy of Pediatrics. (2016). Mental health initiatives: Evidence-based child and adolescent psychosocial intervention. Retrieved Feb 29, 2016 from https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Mental-Health/Pages/default.aspx.
Brauner, J. V., Johansen, L. M., Roesbjerg, T. M., & Pagsberg, A. K. (2016). Off-label prescription of psychopharmacological drugs in child and adolescent psychiatry. Journal of Clinical Psychopharmacology, 36(5), 500–507.
Carey, B. (2006). Parenting as therapy for child’s mental disorders. New York: New York Times.
Carter, A. S., Briggs-Gowan, M. J., & Davis, N. O. (2004). Assessment of young children’s social-emotional development and psychopathology: Recent advances and recommendations for practice. Journal of Child Psychology and Psychiatry, 45(1), 109–134.
Centers for Medicare and Medicaid Services. (2016). CMCS informational bulletin: Clarification of medicaid coverage of services to children with autism. Baltimore, MD: U.S. Department of Health & Human Services. Retrieved Feb 29, 2016 from https://www.medicaid.gov.
Comer, J. S., Chow, C., Chan, P. T., Cooper-Vince, C., & Wilson, L. A. S. (2013). Psychosocial treatment efficacy for disruptive behavior problems in very young children: A meta-analytic examination. Journal of the American Academy of Child and Adolescent Psychiatry, 52(1), 26–36.
Dodge, J. M., & Huang, L. N. (2008). Workforce implications: Issues and strategies for workforce development. In B. A. Stroul & G. M. Blau (Eds.), The system of care handbook: Transforming mental health services for children, youth, and families (pp. 643–662). Baltimore: Paul H. Brookes Pub. Co.
dosReis, S., & Myers, M. A. (2008). Parental attitudes and involvement in psychopharmacological treatment for ADHD: A conceptual model. International Review of Psychiatry, 20(2), 135–141.
dosReis, S., Tai, M. H., Goffman, D., Lynch, S. E., Reeves, G., & Shaw, T. (2014). Age-related trends in psychotropic medication use among very young children in foster care. Psychiatric Services, 65(12), 1452–1457.
Epstein, J. N., et al. (2014). Variability in ADHD care in community-based pediatrics. Pediatrics, 134(6), 1136–1143.
Garfield, L. D., Brown, D. S., Allaire, B. T., Ross, R. E., Nicol, G. E., & Raghavan, R. (2015). Psychotropic drug use among preschool children in the medicaid program from 36 states. American Journal of Public Health, 105(3), 524–529.
Harris, G. (2006). Proof is scant on psychiatric drug mix for young. New York.: New York Times.
Howell, M. E., & Teich, J. (2008). Variation in medicaid mental health service use and cost for children. Administration & Policy in Mental Health & Mental Health Services Research, 35, 220–228.
Kolko, D. J., & Perrin, E. (2014). The integration of behavioral health interventions in children’s health care: Services, science, and suggestions. Journal of Clinical Child & Adolescent Psychology, 43(2), 216–228.
Luby, J. L. (2013). Treatment of anxiety and depression in the preschool period. Journal of the American Academy of Child and Adolescent Psychiatry, 52(4), 346–358.
Mayes, L. C. (1999). Addressing mental health needs of infants and young children. Child and Adolescent Psychiatric Clinics of North America, 8(2), 209–224.
Olfson, M., Blanco, C., Lui, S.-M., Wang, S., & Correll, C. U. (2012). National trends in the office-based treatment of chlldren, adolescents, and adults with antipsychotics. JAMA Psychiatry, 69(12), 1247–1256.
Olfson, M., Crystal, S., Huang, C., & Gerhard, T. (2010). Trends in antipsychotic drug use by very young, privately insured children. Journal of the American Academy of Child and Adolescent Psychiatry, 49(1), 13–23.
Olfson, M., Druss, B. G., & Marcus, S. C. (2015). Trends in mental health care among children and adolescents. The New England Journal of Medicine, 372, 2029–2038.
Olfson, M., King, M., & Schoenbaum, M. (2015). Treatment of young people with antipsychotic medications in the United States. JAMA Psychiatry, 72(9), 867–874.
Skovgaard, A. M. (2010). Mental health problems and psychopathology in infancy and early childhood: An epidemiological study. Danish Medical Bulletin, 57(10), B4193.
Torrey, W. C., et al. (2001). Implementing evidence-based practices for persons with severe mental illnesses. Psychiatric Services, 52(1), 45–50.
Vitiello, B., & Jensen, P. S. (1997). Medication development and testing in children and adolescents: Current problems, future directions. Archives of General Psychiatry, 54(9), 871–876.
Zeanah, C. S., Jr. (Ed.). (2009). Handbook of infant mental health (3rd edn.). New York: The Guilford Press.
Zero to Three. (2016). Early childhood mental health. Retrieved Feb 29, 2016 from http://www.zerotothree.org/child-development/early-childhood-mental-health.
Zito, J. M., Safer, D. J., dosReis, S., Gardner, J. F., Boles, M., & Lynch, F. (2000). Trends in the prescribing of psychotropic medications to preschoolers. JAMA: The Journal of the American Medical Association, 283(8), 1025–1030.
Zito, J. M., Safer, D. J., Valluri, S., Gardner, J. F., Korelitz, J. J., & Mattison, D. R. (2007). Psychotherapeutic medication prevalence in Medicaid-insured preschoolers. J Child Adolesc Psychopharmacol, 17(2), 195–203.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no financial relationships with commercial interests and have no conflict of interest relevant to this article to disclose.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Disclaimer The views expressed here are those of the authors and do not necessarily reflect the views of the Substance Abuse and Mental Health Services Administration (SAMHSA) or the U.S. Department of Health and Human Services (DHHS).
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Appendix
Appendix
See Table 5.
Rights and permissions
About this article
Cite this article
Ali, M.M., Teich, J., Lynch, S. et al. Utilization of Mental Health Services by Preschool-Aged Children with Private Insurance Coverage. Adm Policy Ment Health 45, 731–740 (2018). https://doi.org/10.1007/s10488-018-0858-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10488-018-0858-x