Abstract
The aim of this exploratory cross-sectional study was to investigate the characteristics of cortical activity and stress coping in migraine patients, meditation experienced subjects, and healthy controls. 45 meditation experienced subjects, 46 migraine patients, and 46 healthy controls took part in the study. Cortical activity was measured with the contingent negative variation (CNV), a slow cortical event-related potential. Stress coping was examined with the standardized Stress Coping Questionnaire SVF-78. A one-way analysis of variance was used to investigate possible differences between the groups. CNV-amplitude was significantly higher in migraineurs than in controls. The meditators showed significantly lowest amplitudes. Migraine patients used negative stress-coping strategies significantly more often than meditators and healthy controls. Especially the application of the strategy “rumination” was most frequent in migraine patients and least frequent in meditators. Moreover, frequent rumination was significantly correlated with high CNV-amplitudes. Cortical and stress processing in people with meditation experience was improved compared to migraine patients and healthy controls.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Migraine is a neurological disease characterized by altered cortical activity. Migraineurs show decreased habituation to non-painful stimuli as well as increased cortical activation (Ambrosini and Schoenen 2003; Gerber and Kropp 1993; Gerber et al. 1996; Kropp and Gerber 1993a, b, 2005; Kropp et al. 1999, 2005; Schoenen et al. 1985). Cortical activation can be measured by the “contingent negative variation” (CNV), a slow cortical event-related potential (Walter et al. 1964). The CNV occurs between two stimuli, a warning stimulus (S1) and an imperative stimulus (S2) which requires a reaction by the subject. The interstimulus interval (ISI) usually varies between 1 and 3 s. The CNV is a negative potential where the mean amplitude between S1 and S2 is called the overall CNV (oCNV). There are several components of the oCNV which can be differentiated. The early component of the CNV, namely the initial CNV (iCNV), has its maximum between 550 and 750 ms after S1. The late component is called the terminal CNV (tCNV) which is calculated as the mean amplitude of the interval within the 200 ms before the onset of S2. Decreasing amplitudes over the course of a recording are interpreted as habituation while increasing amplitudes reflect dishabituation (Schoenen and Timsit-Berthier 1993). Several studies revealed increased CNV amplitudes and reduced habituation of the CNV in migraineurs than in healthy controls (Gerber et al. 1996; Schoenen et al. 1985; Maertens de Noordhout et al. 1986). Especially the oCNV and the iCNV showed increased amplitudes in migraine patients (Siniatchkin et al. 1998).
One of the most common triggers for migraine is stress (Göbel 2014; Neut et al. 2012; Sauro and Becker 2009). A number of studies have shown that clinical treatment with mindfulness based interventions can positively influence stress disorders (Kabat-Zinn et al. 1985; Kabat-Zinn 2006; Davidson et al. 2003; Shapiro and Walsh 2003; Carlson et al. 2003; 2004), stress (De Vibe et al. 2012; Khoury et al. 2013) and stress coping (Chiesa and Serretti 2009). Other studies revealed positive effects of meditation on migraine symptoms (Day et al. 2014; Rosenzweig et al. 2010; Tonelli and Wachholtz 2014). However, the effect of meditation on CNV amplitude is still unclear. Studies have shown that meditation can increase (Hansenne and Ansseau 2001; Travis et al. 2002) but also decrease (Chatterjee et al. 2012; Paty et al. 1978) CNV amplitude.
Finally, the study results as presented are standing for their own not allowing in doing any final conclusions about the specific mechanisms of meditation in the treatment or prophylaxis of migraine. Nevertheless, the studies imply that there are positive effects of meditation on migraine symptoms. The main goal of this study was to investigate if there are any differences in cortical activity and stress coping between migraine patients, meditators, and healthy controls to shed some light on the question: Does meditation influence migraine by altering cortical activity and stress coping?
Methods
Design
The study was conducted within an exploratory cross-sectional design, and approved by the Ethics Committee of the Medical Faculty of the University of Rostock in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All participants gave informed consent.
Subjects
46 migraine patients, 45 meditators, and 46 healthy controls were recruited by postings and flyers in medical practices, meditation centers, newspaper announcements, and a press release directed to the staff of the medical department of the University of Rostock. All participants were informed about the purpose, conception, procedure, measurements, risks, and side effects of the study by a participant information sheet. A book about neuroscience and meditation was given to all meditators who took part in the study. The migraine patients and the controls were allowed to choose between a relaxation course and money for their participation in the study. The sample size was chosen according to the effect size of the iCNV amplitude comparing migraine patients and healthy controls which is ɛ = 0.98 for n = 15 subjects per group (Kropp et al. 2002). The larger group size can be explained by a possible drop out caused by subject’s physical or mental health problems, no complete data sets, to large artifacts on the EEG band or a migraine attack immediately before the CNV recording and the explorative character of this study. The inclusion criterion for all participants was age between 18 and 65 years; exclusion criteria were pregnancy, chronic psychiatric disorder, drug use, alcohol abuse. The migraine patients were diagnosed according to the criteria of the International Headache Society (IHS 2004). Further inclusion criteria for them were no prophylactic treatment for 3 months before the start of the study, at least 1 year duration of migraine, less than 15 days of migraine per month. The CNV recordings of the migraineurs took place in a migraine-free interval, at least 3 days after or before a migraine attack. The latter was verified by a telephone call. An additional inclusion criterion of the meditation group was at least 1 year experience in a kind of meditation which includes the practice of mindfulness. The forms of meditation practiced by the participants at least twice a week were Yoga (n = 12), Zen (n = 11), Vipassana (n = 7), Qigong/Tai Chi (n = 5), and other mindfulness-based techniques (n = 10). Neither migraine patients nor healthy controls were allowed to practice any kind of meditation. Table 1 shows the characteristics of the sample.
Procedure
The subjects were seated in a comfortable arm chair. They were asked to relax and focus on a dot at the wall during the recording to avoid any artifacts caused by eye movements or muscle contractions. The CNV recording consisted of 32 GO-trials comprising a warning stimulus (S1) lasting 100 ms with a frequency of 1000 Hz and an intensity of 75 dB. After an ISI of 3 s an imperative stimulus (S2) was presented with duration of maximum 2500 ms, a frequency of 2500 Hz and an intensity of 75 dB. The subject was asked to immediately respond to S2 with a button press to deactivate the target stimulus. To avoid fluctuation in vigilance 8 NO-GO-trials were presented randomly with a frequency of 200 Hz as a control condition where no response was required. An imperative stimulus (S2) was not presented in the NO-GO-condition. Recordings of each trial (6 s) started 1 s before the onset of S1 and ended 2 s after the onset of S 2. For baseline calculation the periods between recording onset and S1 were used. The intertrial interval (ITI) randomly varied between 6 and 10 s. EEG recording was conducted with electrodes placed according to the international 10–20-System over Cz with linked mastoids as reference. Ag/AgCl ring electrodes were used with impedances of approximately 6 kOhm. The EEG-filters were set as follows: high-pass: 0.03 Hz, low-pass: 35 Hz, notch: 50 Hz. The sampling rate of the EEG-signal was 100 Hz for each channel. Additionally a vertical electrooculogram (EOG) was recorded. The mean was calculated by averaging the 32 GO-trials while the NO-GO trials were not analyzed. Trials with eye blinks and large artifacts were discarded.
The oCNV was the mean amplitude between S1 and S2. The iCNV was calculated as the maximum amplitude between 550 and 750 ms after the onset of S1 with an individual window of ±100 ms around the maximum (Böcker et al. 1990). CNV sessions of all subjects were grand averaged. CNV habituation was calculated by dividing the GO trials into 8 trial blocks. Each of them was averaged and used for calculating the habituation coefficient by regression analysis (Kropp and Gerber 1995) indicating habituation for a positive slope and dishabituation for a negative slope.
The CNV recording was realized by a Brain Vision amplifier (BrainAmp) and the program Brain Vision Recorder 1.20 (Brain Products 2007). Data analysis was conducted by Brain Vision Analyzer 1.05 (Brain Products 2007). Stimuli presentation was controlled by the program E-Prime 2.0 (E-Prime 2002).
Stress coping was investigated by using the short version of Janke and Erdmanns Coping Questionnaire SVF-78 (Erdmann and Janke 2008). It consists of 78 items which are summarized in 13 subscales of seven positive (stress-reducing) and six negative (stress-enhancing) coping strategies. Positive coping strategies include underestimation, denial of guilt, distraction, substitute gratification, situation control, reaction control, positive self-instructions, and need for social support. Negative coping strategies include avoidance, escape tendency, rumination, resignation, and self-blame. The SFV-78 contains a 5-point response scale (0–4). High values for positive coping strategies indicate an enhanced coping ability to reduce stress. High values for negative coping strategies imply a high degree of strategies which tend to trigger stress. The internal consistencies (Cronbach alpha) of the subscales range between α = .66 and α = .92. The reliabilities after 4 weeks range between rtt = .69 and rtt = .86. Normal values of coping strategies range between a T-score of 40 and 60 points (Erdmann and Janke 2008). The validity of the SVF-78 has been proved by correlation and factorial analysis (Ising et al. 2001).
Statistical Analyses
The program SPSS 21 (Statistical Package of Social Sciences) was used for statistical analysis. Comparability of the groups regarding sex and age was proved with the Chi2-Test. Normal distribution of the variables was tested with the Kolmogorov–Smirnov-Test. The Levene-Test was applied to test variance homogeneity. Differences between groups were calculated with a one-way analysis of variance (ANOVA) and pairwise Scheffé post hoc tests with a criterion for significance of 5 %. Relationships between neurophysiological and psychological measures were investigated using Pearson’s product-moment correlations.
Results
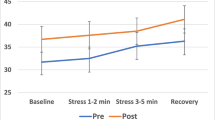
The ANOVA revealed significant differences of oCNV [F(2,135) = 21.18; p = 0.001] and iCNV [F(2,135) = 17.77; p = 0.001] between the groups. There were no significant differences of habituation [F(2,135) = 0.48; p = 0.622] and reaction time [F(2,135) = 1.00; p = 0.37] between the groups. Table 2 and Fig. 1 show that the amplitudes of oCNV and iCNV were significantly higher in the migraine group than in the meditation group and the control group. The meditation group showed significantly lower amplitudes of iCNV and oCNV than the controls. No differences in habituation and reaction time were found between the groups. Although the migraine patients showed lowest habituation and slowest reaction times, they did not differ significantly from the other groups.
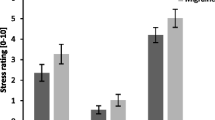
Regarding the SFV-78, no differences were found in the application of positive stress- reducing strategies between all groups. The scale “negative stress-enhancing strategies” showed significant differences between the groups [F(2,135) = 7.52; p = 0.001]. The differences were found on the subscales “rumination” [F(2,135) = 13.801; p = 0.001], “avoidance” [F(2,135) = 6.575; p = 0.002], “resignation” [F(2,135) = 7.125; p = 0.001], and “self-accusation” [F(2,135) = 7.514; p = 0.001]. Table 3 shows that the application of the negative stress coping strategy “rumination” was significantly lower in the meditation group than in the migraine and control group. Migraineurs and controls did not differ in using this strategy. Migraine patients and meditators also differed in using the strategy “avoidance”. Meditation experienced subjects used this strategy significantly less often than migraineurs. No differences were observed between migraineurs and controls as well as controls and meditators in applying this strategy. Meanwhile, differences have been observed with regard to the strategies “resignation” and “self-accusation” showing that the application of both negative stress-enhancing strategies was significantly less frequent in the meditation group than in the migraine group. Migraineurs used these strategies significantly more often than controls while the control and meditation groups showed no significant differences in using these strategies.
Correlational analyses have been conducted for a better understanding of the relationship between the use of coping strategies and the CNV. There were significant correlations between the negative coping strategy “rumination”, and the amplitudes of oCNV (r = 0.206, p = 0.017) and iCNV (r = 0.207, p = 0.017), respectively, across all participants. This means that a frequent use of this strategy was correlated with high CNV-amplitudes. The correlations did not differ between the groups. Further analyses revealed a non-significant correlation trend between the strategy “resignation”, and the amplitudes of oCNV (r = 0.159, p = 0.066) and iCNV (r = 0.152, p = 0.081), respectively.
Discussion
Earlier studies showed that the CNV amplitude of migraine patients is increased compared to healthy controls (Gerber and Kropp 1993; Schoenen et al. 1985; Maertens de Noordhout et al. 1986; Siniatchkin et al. 1998; Coppola et al. 2013). Our study confirms these findings (Table 2; Fig. 1). The amplitudes of iCNV and oCNV were significantly higher in the migraine group than in the control group. The literature suggests that high CNV amplitudes in migraineurs are caused by a lower cortical preactivation level (Kropp et al. 2015; Coppola et al. 2013). The ceiling theory was seen as a theoretical explanation for the reduced cortical preactivation in migraine patients (Schoenen 1990). According to this theory, increased CNV amplitudes in migraineurs are caused by reduced habituation, because the ceiling which triggers a habituation response would be reached later than in healthy people.
The influence of meditation on cortical activation is unclear. Studies showed that meditation can both increase (Hansenne and Ansseau 2001; Travis et al. 2002) and decrease (Chatterjee et al. 2012; Paty et al. 1978) CNV amplitude. Results of our study confirm the latter findings revealing that the iCNV and oCNV were significantly lower in the meditation group than in the migraine and control group. Davidson (2004a) emphasized that the main effects of meditation can be achieved by long time practice. Thus, it may be suggested that regular practice of meditation can reduce the CNV amplitude. Other studies have observed that specific EEG-based biofeedback training for the self-regulation of brain potentials, namely neurofeedback, can specifically decrease the CNV-amplitude and have a positive effect on the migraine symptomatic (Kropp et al. 2002; Siniatchkin et al. 2000). These results are relevant for the current study suggesting that attention training can regulate specific physiological processes. Lutz et al. (2008) accentuated that meditators are more effective in discriminating between important and unimportant stimuli of the environment than non-meditators. Thus, we support the idea that meditation can prevent a sensory overload which might lead to a dysfunction of cortical processing. The low CNV amplitudes of the meditators indicate a relaxed state of expectancy and orientation during the stimuli presentation of the CNV measurement while the high CNV amplitudes in migraine patients indicate a more stressful response behavior.
As shown in other studies, habituation was reduced in migraine patients (Gerber et al. 1996; Schoenen et al. 1985; Maertens de Noordhout et al. 1986; Kropp et al. 2012, 2015; Magis et al. 2013). However, in the current study, they did not differ significantly from the other groups. It is conceivable that subgroups of migraineurs with different durations of disease could explain the missing significance. Also it might be possible that habituation is not as robust as postulated. There is a study in which habituation was observed in migraine patients (Omland et al. 2013).
We have hypothesized that stress coping is reduced in migraine patients. Our results confirm studies revealing that migraineurs use significantly more often negative stress-enhancing strategies than healthy controls (Huber and Henrich 2003; Trimmel and Gmeier 2001).
Based on the results of several meta-studies that indicate a positive effect of meditation on stress (Khoury et al. 2013; Chiesa and Serretti 2010; Goyal et al. 2014) and stress coping (Chiesa and Serretti 2009) we assumed that meditators show better performance in stress coping than migraine patients and healthy controls. Our work is in line with these results revealing that meditators use negative stress-enhancing strategies significantly less frequently than migraineurs. Meditators also showed a better ability to cope with stress than healthy controls. However, this difference was not significant.
Analysis of subscales of negative stress increasing strategies unveiled significantly higher values for “resignation” and “self-accusation” and non-significantly higher values for “avoidance” and “rumination” in the migraine group than in the control group (Table 3). These results confirm the findings of earlier studies (Huber and Henrich 2003; Trimmel and Gmeier 2001) supporting the hypothesis that the application of these strategies may increase cortical activity and confines stimulus processing in migraine patients. Compared to the meditation group the migraine group showed significantly higher values for all strategies as mentioned above.
Largest differences between the meditation group and both the migraine and control group were observed for the stress-enhancing strategy “rumination” (Table 3). Meditators used this strategy least often confirming the main practice of meditation which is not to follow thoughts but rather to observe them. Further analysis revealed that frequent rumination was significantly correlated with high CNV-amplitudes. We assume that rumination overly occupies cognitive capacities leading to increased cortical activity which is in line with an earlier study showing that cortical activity of the subjects increased as soon as they started to follow thoughts instead of observing them (Ott et al. 2010).
In summary, the current study shows that cortical activity and the application of negative stress coping strategies are significantly increased in migraine patients compared to healthy controls and meditation experienced subjects. Meditation experienced participants showed lowest cortical activity and best results in stress coping.
References
Ambrosini, A., & Schoenen, J. (2003). The electrophysiology of migraine. Current Opinion in Neurology, 16(3), 327–331.
Böcker, K. B. E., Timsit-Berthier, M., Schoenen, J., & Brunia, C. H. M. (1990). Contingent negative variation in migraine. Headache, 30(9), 604–609.
Brain Products. (2007). Brain Vision Recorder version 1.20, Software for EEG-recording. Brain Vision Analyzer version 1.05, Software for EEG-analysis. Gilching: Brain Products GmbH.
Carlson, L. E., Speca, M., Patel, K. D., & Goodey, E. (2003). Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosomatic Medicine, 65, 571–581.
Carlson, L. E., Speca, M., Patel, K. D., & Goodey, E. (2004). Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology, 29, 448–474.
Chatterjee, A., Ray, K., Panjwani, U., Thakur, L., & Anand, J. P. (2012). Meditation as an intervention for cognitive disturbances following total sleep deprivation. Indian Journal of Medical Research, 136(6), 1031–1038.
Chiesa, A., & Serretti, A. (2009). Mindfulness-based stress reduction for stress management in healthy people: A review and meta-analysis. Journal of Alternative and Complementary Medicine, 15(5), 593–600.
Chiesa, A., & Serretti, A. (2010). A systematic review of neurobiological and clinical features of mindfulness meditations. Psychological Medicine, 40(8), 1239–1252.
Coppola, G., Di Lorenzo, C., Schoenen, J., & Pierelli, F. (2013). Habituation and sensitization in primary headaches. The Journal of Headache and Pain, 14(65), 1–13.
Davidson, R. J. (2004a). Presentation at “Mind and Life Summer Research Institute 2004”. Garrison Institute, Garrison, New York, July 21–26, 2004, Talk # 19. (DVD video recording).
Davidson, R. J., Kabat-Zinn, J., Schumacher, J., et al. (2003). Alterations in brain and immune function produced by mindfulness meditation. Psychosomatic Medicine, 65, 564–570.
Day, M. A., Thorn, B. E., & Rubin, N. J. (2014). Mindfulness-based cognitive therapy for the treatment of headache pain: A mixed-methods analysis comparing treatment responders and treatment non-responders. Complementary Therapies in Medicine, 22(2), 278–285.
De Vibe, M., Bjørndal, A., Tipton, E., Hammerstrøm, K. T., & Kowalski, K. (2012). Mindfulness based stress reduction (MBSR) for improving health, quality of life and social functioning in adults. Campbell Systematic Reviews, 3, 1–127.
E-Prime. (2002). Software for stimulus presentation. Psychology Software Tools, Inc.: Pittsburgh.
Erdmann, G., & Janke, W. (2008). Stressverarbeitungsfragebogen (SVF). Handbuch: Stress, Stressverarbeitung und ihre Erfassung durch ein mehrdimensionales Testsystem. [Stress coping questionnaire (SVF). Handbook: Stress, stress coping and its acquisition in a multidimensional test system.]. Göttingen: Hogrefe.
Gerber, W.-D., & Kropp, P. (1993). Migräne als Reizverarbeitungsstörung? Empirische Untersuchungen zur Contingenten Negativen Variation bei Migränepatienten. [Migraine as stimulus processing disorder? Empirically investigations of the contingent negative variation in migraine patients]. Der Schmerz, 7(4), 280–286.
Gerber, W.-D., Kropp, P., Schoenen, J., & Siniatchkin, M. S. (1996). “Born to be wild oder doch gelernt?” Neue verhaltensmedizinische Erkenntnisse zur Ätiopathogenese der Migräne. [“Born to be wild or still learned?” New medical behavioral findings about the etiopathogenesis of migraine]. Verhaltenstherapie, 6, 210–220.
Göbel, H. (2014). Erfolgreich gegen Kopfschmerzen und Migräne. Ursachen beseitigen, gezielt vorbeugen, Strategien zur Selbsthilfe. [Successful treatment of headache and migraine. Cause elimination, specific prevention, strategies for self-help.] (7th ed.). Berlin: Springer.
Goyal, M., Singh, S., Sibinga, E. M., Gould, N. F., Rowland-Seymour, A., Sharma, R., et al. (2014). Meditation programs for psychological stress and well-being: A systematic review and meta-analysis. JAMA Internal Medicine, 174(3), 357–368.
Hansenne, M., & Ansseau, M. (2001). Contingent negative variation and personality in depression. Neuropsychobiology, 44(1), 7–12.
Huber, D., & Henrich, G. (2003). Personality traits and stress sensitivity in migraine patients. Behavioral Medicine, 29, 4–13.
International Headache Society (IHS). (2004). The international classification of headache disorders, 2nd edition (ICHD-II). Cephalalgia, 24(Suppl. 1), 1–160.
Ising, M., Weyers, P., Janke, W., & Erdmann, G. (2001). The psychometric properties of the SVF78 by Janke and Erdmann, a short version of the SVF120. PsyJournals, 22, 279–289.
Kabat-Zinn, J. (2006). Gesund durch Meditation: Das große Buch der Selbstheilung. Frankfurt am Main: Fischer. Original title: Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness.
Kabat-Zinn, J., Lipworth, L., & Burney, R. (1985). The Clinical use of mindfulness meditation for the self-regulation of chronic pain. Journal of Behavioral Medicine, 8(2), 163–190.
Khoury, B., Lecomte, T., Fortin, G., Masse, M., Therien, P., Bouchard, V., et al. (2013). Mindfulness-based therapy: A comprehensive meta-analysis. Clinical Psychology Review, 33(6), 763–771.
Kropp, P., Brecht, I. B., Niederberger, U., Kowalski, J., Schröder, D., Thome, J., et al. (2012). Time-dependent post-imperative negative variation indicates adaptation and problem solving in migraine patients. Journal of Neural Transmission, 119(10), 1213–1221.
Kropp, P., & Gerber, W.-D. (1993a). Contingent negative variation: Findings and perspectives in migraine. Cephalagia, 13(1), 33–36.
Kropp, P., & Gerber, W.-D. (1993b). Is increased amplitude of contingent negative variation in migraine due to cortical hyperactivity or reduced habituation? Cephalalgia, 13, 37–41.
Kropp, P., & Gerber, W.-D. (1995). Contingent negative variation during migraine attack and interval: Evidence for normalization of slow cortical potentials during the attack. Cephalalgia, 15, 123–128.
Kropp, P., & Gerber, W.-D. (2005). Slow cortical potential in migraine. Predictive value and possible novel therapeutic strategies to prevent an attack. Functional Neurology, 20(4), 193–197.
Kropp, P., Linstedt, U., & Gerber, W.-D. (2005). Migräne: Die Dauer der Erkrankung beeinflusst Amplitude und Habituation ereigniskorrelierter Potenziale. [Migraine: The duration of the disorder influences amplitude and habituation of event-related potentials]. Der Schmerz, 19, 489–496.
Kropp, P., Siniatchkin, M., & Gerber, W.-D. (2002). On the pathophysiology of migraine: Links for “empirically based treatment” with neurofeedback. Applied Psychophysiology and Biofeedback, 27(3), 203–213.
Kropp, P., Siniatchkin, M., Stephani, U., & Gerber, W. D. (1999). Migraine: Evidence for a disturbance of cerebral maturation in man? Neuroscience Letters, 276, 181–184.
Kropp, P., Wallasch, T. M., Müller, B., Meyer, B., Darabaneanu, S., Bosse, C., et al. (2015). Disease duration of episodic migraine correlates with modified amplitudes and habituation of contingent negative variation. Journal of Neural Transmission, 122(6), 877–885.
Lutz, A., Slagter, H. A., Dunne, J. D., & Davidson, R. J. (2008). Attention regulation and monitoring in meditation. Trends in Cognitive Science, 12(4), 163–169.
Maertens de Noordhout, A., Timsit-Berthier, M., Timsit, M., & Schoenen, M. (1986). Contingent negative variation in headache. Annals of Neurology, 19(1), 78–80.
Magis, D., Vigano, A., Sava, S., d’Elia, T. S., Schoenen, J., & Coppola, G. (2013). Pearls and pitfalls: Electrophysiology for primary headaches. Cephalalgia, 33(8), 526–539.
Neut, D., Fily, A., Cuvellier, J.-C., & Vallée, L. (2012). The prevalence of triggers in paediatric migraine: A questionnaire study in 102 children and adolescents. The Journal of Headache and Pain, 13(1), 61–65.
Omland, P. M., Nilsen, K. B., Uglem, M., Gravdahl, G., Linde, M., Hagen, K., & Sand, T. (2013). Visual evoked potentials in interictal migraine: No confirmation of anbormal habituation. Headache, 53, 1071–1086.
Ott, U., Walter, B., Gebhardt, H., Stark, R. & Vaitl, D. (2010). Inhibition of default mode network activity during mindfulness meditation. (Poster) In 16th annual meeting of the organization for human brain mapping. Barcelona, Spanien Juni 6–10, 2010.
Paty, J., Brenot, P., Tignol, J., & Bourgeois, M. (1978). Evoked cerebral activity (contingent negative variation and evoked potentials) and modified states of consciousness (sleeplike relaxation, transcendental meditation). Annales Medico-Psychologiques, 136, 143–169.
Rosenzweig, S., Greeson, J. M., Reibel, D. K., Green, J. S., Jasser, S. A., & Beasley, D. (2010). Mindfulness-based stress reduction for chronic pain conditions: Variation in treatment outcomes and role of home meditation practice. Journal of Psychosomatic Research, 68(1), 29–36.
Sauro, K. M., & Becker, W. J. (2009). The stress and migraine interaction. Headache, 49(9), 1378–1386.
Schoenen, J. (1990). Deficient habituation of evoked cortical potentials in migraine: A link between brain biology, behavior and trigeminovascular activation? Biomedicine and Pharmacotherapy, 50(2), 71–78.
Schoenen, J., Maertens de Noordhout, A., Timsit-Berthier, M., & Timsit, M. (1985). Contingent negative variation (CNV) as a diagnostic and physiopathologic tool in headache patients. In C. Rose (Ed.), Migraine (pp. 17–25). Basel: Karger.
Schoenen, J., & Timsit-Berthier, M. (1993). Contingent negative variation: Methods and potential interest in headache. Cephalalgia, 13(1), 28–32.
Shapiro, S. L., & Walsh, R. (2003). An analysis of recent meditation research and suggestions for future directions. Humanistic Psychologist, 31, 86–114.
Siniatchkin, M., Gerber, W.-D., Kropp, P., & Vein, A. (1998). Contingent negative variation in patients with chronic daily headache. Cephalalgia, 18(8), 565–569.
Siniatchkin, M., Hierundar, A., Kropp, P., Kuhnert, R., & Gerber, W.-D. (2000). Self-regulation of slow cortical potentials in children with migraine: An exploratory study. Applied Psychophysiology and Biofeedback, 25(1), 13–32.
Tonelli, M. E., & Wachholtz, A. B. (2014). Meditation-based treatment yielding immediate relief for meditation-naive migraineurs. Pain Management Nursing, 15(1), 36–40.
Travis, F., Tecce, J., Arenander, A., & Wallace, R. K. (2002). Patterns of EEG coherence, power, and contingent negative variation characterize the integration of transcendental and waking states. Biological Psychology, 61, 293–319.
Trimmel, M., & Gmeier, G. (2001). Partnerschaftliches Interaktionsverhalten und Stressverarbeitung von Migränepatientinnen. [Partnership interaction behavior and stress coping in female migraine patients]. Psychotherapie, Psychosomatik und Medizinische Psychologie, 51, 430–433.
Walter, W. G., Cooper, R., Aldridge, V. J., McCallum, W. C., & Winter, A. L. (1964). Contingent negative variation: An electric sign of sensorimotor association and expectancy in the human brain. Nature, 203, 380–384.
Acknowledgments
This study was supported by the Barbara-Wengeler Foundation. We are grateful for Prof. Dr. Thomas Metzingers’ help.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no competing interests.
Rights and permissions
About this article
Cite this article
Keller, A., Meyer, B., Wöhlbier, HG. et al. Migraine and Meditation: Characteristics of Cortical Activity and Stress Coping in Migraine Patients, Meditators and Healthy Controls—An Exploratory Cross-Sectional Study. Appl Psychophysiol Biofeedback 41, 307–313 (2016). https://doi.org/10.1007/s10484-016-9334-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10484-016-9334-0