Abstract
Adverse childhood experiences (ACEs) are associated with numerous risk behaviors and mental health outcomes among youth. This study examines the relationship between the number of types of exposures to ACEs and risk behaviors and mental health outcomes among reservation-based Native Americans. In 2011, data were collected from Native American (N = 288; 15–24 years of age) tribal members from a remote plains reservation using an anonymous web-based questionnaire. We analyzed the relationship between six ACEs, emotional, physical, and sexual abuse, physical and emotional neglect, witness to intimate partner violence, for those <18 years, and included historical loss associated symptoms, and perceived discrimination for those <19 years; and four risk behavior/mental health outcomes: post-traumatic stress disorder (PTSD) symptoms, depression symptoms, poly-drug use, and suicide attempt. Seventy-eight percent of the sample reported at least one ACE and 40 % reported at least two. The cumulative impact of the ACEs were significant (p < .001) for the four outcomes with each additional ACE increasing the odds of suicide attempt (37 %), poly-drug use (51 %), PTSD symptoms (55 %), and depression symptoms (57 %). To address these findings culturally appropriate childhood and adolescent interventions for reservation-based populations must be developed, tested and evaluated longitudinally.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Native Americans have undergone significant traumatic experiences including forced removal from traditional and sacred territories, confinement to reservations, mandatory boarding school experiences, and mass depopulation through starvation, infectious disease, and military action (Duran 2006; Duran et al. 1998). The forced removal of Native children from their families to remote boarding schools, beginning in the late 1800s, has been cited as having the longest lasting harmful effects of all the assimilation and termination policies put forth by the US Government largely due to abuse and neglect experiences that continue to have a negative impact on tribal identity (Brave Heart and DeBruyn 1998). The establishment and maintenance of Indian reservations, which undermine tribal subsistence and thus tribal economies, created areas of concentrated poverty and increased morbidity and mortality. Where one lives is a critical variable in mediating access to quality health care, economic opportunities, social connections, and social capital, all of which determine health status (Diez Roux 2003; Diez Roux et al. 2002; O’Campo et al. 1997; Whitaker et al. 2013). When communities are characterized by persistently low economic status and segregation, higher rates of morbidity and mortality are typical (Chaix et al. 2011; Lawman and Wilson 2012). Reservation segregation has created areas of high poverty resulting in increased social problems, greater exposure to stress and fewer resources with which to cope with these exposures.
An emerging body of research explores the impact historical traumas and discrimination have upon health. Among Native Americans, historical trauma (Brave Heart and DeBruyn 1998) and discrimination (Freedenthal and Stiffman 2004; Whitbeck et al. 2001, 2002, 2004) are hypothesized as being associated with negative health outcomes. Historical trauma (HT) is defined here as the “collective experience of violence perpetrated against Indigenous Peoples in the process of colonizing the Americas resulting in an unresolved humanitarian crisis for reservation communities” (Brockie et al. 2013). There are several ways to operationalize HT including historical loss (Whitbeck et al. 2004); having had a caretaker who attended boarding school (Evans-Campbell et al. 2012); a family history of boarding school (Mota et al. 2012) and direct and indirect residential school exposure (Elias et al. 2012). Instruments have been developed by Whitbeck and colleagues (Whitbeck et al. 2004) to measure historical loss (HL) and historical loss associated symptoms (HLAS). HL and HLAS are measures of the impact of a broad scope of adverse tribal experiences including, among others, loss of land, language, culture, and broken treaties along with the boarding school experience throughout the lifespan. HLAS is utilized here as a measure of stress appraisal in childhood through young adulthood. Among on-reserve First Nations adults in Canada, negative experience in residential school and having a parent or grandparent who attended residential school has been associated with a history of abuse and a history of suicide thoughts and attempts (Elias et al. 2012). One study of adolescents (N = 459; 11–13 years of age) found historical loss had an independent impact on depressive symptoms (Whitbeck et al. 2009) and mediated the impact of discrimination on alcohol abuse (Whitbeck et al. 2004). Discrimination experienced by Native Americans has been associated with anger and aggression among adolescents (Sittner Hartshorn et al. 2012), depression among adults (Whitbeck et al. 2002), suicidal behavior (Freedenthal and Stiffman 2004; Walls et al. 2007) and early substance use among children (Whitbeck et al. 2001). The discrimination experienced by reservation communities, referred to as “border-town racism”, is hypothesized to have a direct affect on identity development (Moore 2006). This discrimination may exacerbate the effects of historical trauma on individuals and thus has important ramifications for child and adolescent development.
In a predominantly white, educated, sample of adults the groundbreaking adverse childhood experiences (ACEs) Center for Disease Control and Prevention (CDC)/Kaiser Permanente Study revealed a strong dose–response relationship between adversity in childhood and increased morbidity and mortality in adulthood (Felitti et al. 1998), such as alcoholism and alcohol abuse, depression, illicit drug use, risk for intimate partner violence (IPV) and suicide attempt (Anda et al. 2002; Dube et al. 2001, 2002, 2002, 2003). Results from the population-based Longitudinal Studies of Child Abuse and Neglect (LONGSCAN) which included primarily white and African American adolescents (N = 933), found a high proportion (90 %) had at least one ACE by 14 years of age and a dose–response relationship was identified between those experiences and poor health (Flaherty et al. 2013). In another study of 136,549 adolescents Duke and colleagues found a lower reported rate of adversity (29 %); however multiple types of childhood adversity were associated with an increased risk for suicide ideation and attempt in adolescents, with significant gender differences noted (Duke et al. 2010). Further, Native American youth in the study by Duke et al. (N = 1975) were more likely to report at least one adverse experience when compared to white youth. In a study of ten ACEs among white, black, and Hispanic high school seniors (N = 1093), most experiences were strongly associated with depressive symptoms, drug use, and antisocial behavior (Schilling et al. 2007).
Studies that have explored these concepts among Native American adults found a high proportion of ACEs (De Ravello et al. 2008; Koss et al. 2003). In a study among seven tribes (N = 1660), Koss and colleagues found that 74–100 % of men and 83–93 % of women were exposed to ACEs, and physical abuse, sexual abuse, and boarding school attendance were strongly associated with alcohol dependence (Koss et al. 2003). Significant tribal differences were found for ACEs and alcohol dependence and dose–response relationships were observed for men and women. In a small study of incarcerated Native American women, De Ravello et al. found that 75 % of participants were exposed to ACEs with 83 % reporting attempted suicide in their lifetime. Women with high ACE scores (4–5 ACEs) were seven times more likely to attempt suicide than those with lower ACE scores (0–3 ACEs; De Ravello et al. 2008).
Despite the high rates of suicide, depression, trauma exposure, and substance use found among Native American adolescents and young adults and the important research connecting childhood experiences to risk behavior and mental health outcomes, few studies have examined ACEs among this group and none have focused specifically on the unique stressful and traumatic experiences of reservation-based adolescents and young adults. The transition into adulthood is a tumultuous period for some adolescents and young adults, and this transition could be made more challenging by ACEs. We lack research for this specific population that (1) explains the persistently high rates of suicide, depression, substance use, and PTSD found among some tribes, (2) explores the relationship between adversity in childhood and risk behaviors and multiple mental health outcomes, and (3) examines culturally specific variables. Current assessments of adverse childhood experiences may not address the broader scope of adversity to which reservation-based Native American children are exposed, including discrimination and historical loss. The purpose of this study was to examine the relationship between the number of types of exposures to ACEs and risk behaviors and mental health outcomes among a sample of reservation-based Native American adolescents and young adults. In addition to variables common to other ACE studies and the ACE screening instrument items being used by primary care providers and mental health specialists, we also examined how two culturally specific variables, historical loss associated symptoms and perceived discrimination, are related to risk behaviors and mental health outcomes. To achieve this we first compared the relationship of six ACEs among those <18 years of age to depression symptoms, PTSD symptoms, poly-drug use and suicide attempt, we then added the two culturally specific variables and examined the relationship among the subset of those <19 years of age.
Materials and Methods
Setting
To protect community anonymity the reservation and tribes will not be identified.
The plains reservation is home to more than one distinct tribe, each comprised of numerous bands and divisions and having their own history, culture, language, and traditions. On the reservation there are six communities—two larger (A = 3698; B = 2663) and four smaller (C = 472; D = 362; E = 204; F = 71). Tribal enrollment totals over 10,000 members, with 52 % living on or near the reservation, including 1219 of the estimated 2221 members between the ages of 15–24 years. The reservation lies within a county considered one of the 100 poorest in America, (US Census 2010), and morbidity and mortality factors qualify the area as one of the least healthy counties in the United States (University of Wisconsin Population Health Institute 2010). The persistently high rate of suicide in this reservation community was intensified in 2010 when a clustering of suicides and suicide attempts occurred over a 5-month period, including 6 suicides and 20 attempts that resulted in the tribal leadership declaring a state of emergency.
Participants
Of the total sample (N = 288), a larger portion were in the 15–19 year age group (59 %; mean = 19.25 years, SD = 2.9), while comparable numbers were female (51 %) and attending high school or college (48 %).
Participants were required to be 15–24 year old tribal members, have parental/guardian consent if <18 years of age, and live within 1 h of the Indian Health Service (IHS) Unit to ensure eligibility for healthcare service if referrals were deemed necessary. An introduction to the study and consent form was read verbatim; parents and participants were provided an opportunity to ask questions. Verbal parental consent was obtained for participants 15–17 years of age either in person (n = 46) or via telephone (n = 36) and verbal assent (n = 86) for those 15–17 years, or verbal consent (n = 198) for those 18–24 years of age was obtained and recorded. Once enrolled, participants completed the survey and were compensated twenty dollars.
Recruitment occurred through word of mouth and by a flyer that indicated the study was about suicidality. The team exceeded the pre-established goal to recruit at least 60 participants from each of the two larger communities, but did not meet the goal of at least 30 from each of the four smaller communities. Of the total sample, 140 participants were from community A; 111 from B; 18 from C; 12 from D; 3 from E, and 0 from F. Four participants did not identify a community and community was classified as missing data for these four individuals.
Study Design and Approval
A cross-sectional design was used with self-report data. In fall 2011, an all Native American research team utilized an anonymous, self-administered web-based questionnaire to collect data. Enrollment and data collection took place in select educational institutions with computer labs located within the reservation. Members of the research team guided participants through the process of enrollment, survey completion, debrief and check-out. Privacy was provided by seating participants in every other workstation and alternating seated rows. Participants were instructed to direct any questions to research staff present in the computer lab. Cell phone use was not permitted. Participants logged on to a secure website to enter their survey responses from their individual workstation computer. As each participant finished, research staff verified survey completion before directing each participant to the debrief station. Research staff monitored the lab to provide assistance as needed and to ensure that each participant was fully logged out before seating another participant at workstations. A formal tribal resolution provided permission to conduct the study, and the tribe or a designee reviewed and approved all research documents. The proposal (Protocol # NA_00039213) received approval from the Johns Hopkins University School of Medicine Institutional Review Board (IRB).
Variables and Measurement
The Kaiser/CDC ACE study provided a framework for variable selection and served to guide our study (Felitti et al. 1998). Four socio-demographic variables were selected as the most salient covariates for further examination after initial bivariate analysis: gender, age-group, tribal affiliation, and school attendance (high school or college). A 189-item questionnaire was developed from several measures and questionnaires including the Childhood Trauma Questionnaire (CTQ; Bernstein and Fink 1998), Perceived Discrimination (PD) Scale (Whitbeck et al. 2002), HLAS Scale (Whitbeck et al. 2004), Youth Risk Behavior Survey (Centers for Disease Control and Prevention 2012), Short Screen for PTSD (Breslau et al. 1999), and Beck Depression Inventory (BDI-IA; Beck et al. 1996). It also included single-item assessments for exposure to IPV and suicide attempt. All but one of the selected measures, the Short Screen for PTSD (Breslau et al. 1999), have been used and validated in Native American communities. The Short Screen for PTSD has been tested in diverse populations (Bohnert and Breslau 2011; Kimerling et al. 2006).
Adverse Childhood Experiences
Six stressful or traumatic childhood experiences were assessed that were part of the original Kaiser/CDC ACE study: physical abuse, emotional abuse, sexual abuse, emotional neglect, physical neglect, and witnessing violence against mother (IPV exposure). In addition to these six, two experiences unique to this study, historical loss associated symptoms and discrimination were included and assessed for those <19 years.
Five categories of abuse and neglect were measured using the CTQ subscales (Bernstein et al. 2003), which exhibited fair to good internal consistency in the current sample: emotional abuse (α = .89), physical abuse (α = .69), sexual abuse (α = .94), physical neglect (α = .58) and emotional neglect (α = .85). We used the suggested standardized scores that indicate the presence of abuse or neglect—emotional abuse (≥9), physical abuse (≥8), sexual abuse (≥6), emotional neglect (≥10), and physical neglect (≥8; Bernstein and Fink 1998). Witness to IPV was assessed using one item (in your whole life did you ever see your mother get hit, slapped, punched or beaten up?) with a yes/no response option. Historical loss associated symptoms are current thoughts and feelings associated with a historical loss. The twelve-item HLAS Scale (α = .89) measures emotional responses related to historical loss (Whitbeck et al. 2004) including symptoms of sadness, depression, anxiety, shame, as well as loss of self-respect, language, culture, and land (Whitbeck et al. 2004). Discrimination was measured using the ten-item PD Scale (α = .87) modified by Whitbeck et al. (2002). The measure includes questions related to how often the participant was insulted, treated disrespectfully, ignored, suspected of wrong doing, or treated unfairly as a Native American.
Participants were considered exposed to a category if they responded yes to a question in that category or according to pre-established scores, as in the case of the CTQ. Scores from the HLAS and PD scales were dichotomized using a mean cut into low/high or absence/presence. Similar to De Ravello et al. (2008) we stratified stressful or traumatic childhood experiences to study adverse childhood exposure; which ranged from 0 (no exposure) to 6 (exposed to all categories) and 0–8 for those <19 years. We also used the Schilling approach (Schilling et al. 2007) to determine the effect of experiencing at least one ACE (“Any ACE”) and the cumulative effect (“Sum of ACEs”).
Risk Behaviors and Mental Health Outcomes
Two mental health outcomes (depression symptoms, and PTSD symptoms) and two risk behaviors (poly-drug use and suicide attempt) were selected for analysis.
PTSD was assessed using Breslau’s 7-item Short Screening Scale (α = .83) for DSM IV PTSD (Breslau et al. 1999). The pre-established score of four or greater defines positive cases of PTSD symptoms sufficient to qualify for a diagnosis of PTSD (sensitivity = 80 %, specificity = 97 %; Breslau et al. 1999). The 21-item BDI-IA (α = 0.89) was used to determine depression symptoms and a score of 14 or more was the cutoff to distinguish those with and without depression symptoms (Beck et al. 1996). Questions about lifetime substance use, including alcohol, marijuana, inhalants, methamphetamine, and prescription drugs, were adapted from the Youth Risk Behavior Survey (Centers for Disease Control and Prevention 2012). We defined poly-drug use as those with high alcohol use (>100 times) and high marijuana use (>100 times) in addition to at least one of three endorsements of lifetime inhalant, methamphetamine, or prescription drug use. Suicide attempt was defined as an affirmative response to “have you ever attempted suicide?”
Statistical Analysis
Statistical analyses were conducted using SPSS, version 19.0. Descriptive statistics and Pearson’s Chi Square (χ2) test were used to examine the relationship among select variables. Significance was set at (p < .05). Adjusted odds ratios (OR) and 95 % confidence intervals (CI) were calculated using logistic regression to estimate the likelihood of depression symptoms, poly-drug use, PTSD symptoms and ever attempting suicide by the number of types of ACE exposures. Separate logistic regression analyses were conducted for the four mental health/risk behavior outcomes, with the number of types of adverse exposures (0–6) and (0–8) included as a single variable. Mann–Whitney U tests were used to compare demographic differences for the number of types of adverse experiences. The dose–response logistic regression analyses controlled for the effects of age, gender, tribe, and school attendance on the relationship between ACE exposures and mental health/risk behavior outcomes.
Results
Sample Characteristics
The 288 participants were 51 % female, 48 % attending school, primarily members of tribe 1 (66 %), and 15–19 years old (59 %) (M = 19.25 SD = 2.9). Fifty-three (18 %) reported living with both parents, 53 (18 %) with mother, 19 (7 %) with their father, 46 (16 %) with a significant other in their own home, 37 (13 %) with grandparents, and 32 (11 %) with other relatives. In terms of occupation, participants were working full or part time (17 %), unemployed (40 %), attending school (37 %) or attending school and working part time (5 %). Those not attending school were mostly unemployed (n = 102, 89 %). About half of the sample, n = 136 (47 %), reported an annual family income of ≤$2500 (76 % reported ≤$10,000). This amount is consistent with the general public assistance program benefits paid through the Bureau of Indian Affairs for a family size of one; $298 per month if they have their own housing and $223 if not (Bureau of Indian Affairs 2008).
Adverse Childhood Experiences (ACEs)
The overall distribution of ACEs by select sociodemographic characteristics can be found in Table 1. The most prevalent of the six ACEs was emotional abuse (48 %) and the least was sexual abuse (20 %). Across demographics, at least 30 % of participants reported emotional neglect, physical neglect, or witness of violence against their mother, while 40 % reported emotional abuse. Females were more likely than males to report emotional abuse (χ2 (1) = 4.12, p < .05) and sexual abuse (χ2 (1) = 5.26, p < .05) while males were more likely than females to report physical neglect (χ2 (1) = 5.01, p < .05). Those 20–24 years of age had a higher prevalence of physical (χ2 (1) = 4.14, p < .05) and sexual abuse (χ2 (1) = 4.60, p < .05) when compared to those 15–19 years of age. Members of tribe 1 were more likely to report emotional abuse than tribe 2, (χ2 (1) = 4.20, p < .05). Those not attending school were more likely than those attending school to report physical abuse (χ2 (1) = 6.7, p < .05), emotional neglect (χ2 (1) = 5.3, p < .05), and witnessing IPV (χ2 (1) = 5.35, p < .05). The majority (80 %) of those who witnessed violence against their mother (n = 103) indicated that the perpetrator was a partner or ex-partner.
The distributions of ACE score by gender, age, tribal affiliation and school attendance for the full sample are shown in Table 2. Significant differences in adverse experiences were found for age group and school attendance. Older participants (20–24 years) had higher ACE scores than younger participants, and those not attending school had higher ACE scores than those attending school. Overall, 78 % of participants reported at least one ACE and 58.6 % reported at least two. Eleven participants (4 %) reported experiencing all six ACEs; 182 (63 %) had a low ACE score (0–2) and 106 (37 %) had a high ACE score (3–6).
Effect of ACEs on Risk Behavior and Mental Health Outcomes
The mental health and risk behavior outcomes associated with adverse experiences for those <18 years of age are presented in Table 3. Overall, 21 % had depression symptoms, 54 % were classified as a poly-drug user, 21 % had PTSD symptoms, and 30 % reported a lifetime suicide attempt. After controlling for the effects of age, gender, tribal affiliation and school attendance, five of six ACEs were independently, significantly related to depression symptoms (all except sexual abuse) poly-drug use (all except physical neglect), and suicide attempt (all except sexual abuse); and four were related to PTSD symptoms (all except sexual abuse and emotional neglect). Certain ACEs were related more strongly than others to each of the four outcomes. IPV exposure (OR = 2.96, p < .001) most strongly and significantly increased the odds of PTSD symptoms and poly-drug use (OR = 5.3, p < .001) and physical abuse most strongly and significantly increased the odds of depression symptoms (OR = 3.68, p < .001) and suicide attempt (OR = 2.90, p < .001). Three of the six ACEs (emotional abuse, physical abuse, and IPV exposure) were associated with all four mental health and behavioral risk outcomes.
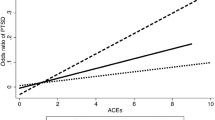
Cumulative Adverse Experiences
The high prevalence of trauma exposures (78 % with at least one ACE) resulted in a very small number of participants with no exposure to adversities as assessed, thus we were unable to determine the effect of individual ACEs. Instead, we categorized the adverse experiences into a variable tapping number of types of ACE exposures: high (3–6 ACEs, n = 106) and low (0–2 ACEs, n = 182), as shown in the bottom row of Table 3 (High ACEs). Those with high ACE scores had more than four and a half times the odds of depression symptoms (p < .05), four times the odds of poly-drug use (p < .001), three times the odds of PTSD symptoms (p < .001) and two times the odds of suicide attempt (p < .001) when compared to those with low ACE scores. Using the Schilling et al. (2007) method, in which the Sum of ACEs variable is continuous, the cumulative effect of the ACEs (shown in the bottom row of Table 3, Sum of ACEs) was highly significant (p < .001) for the four outcomes. The effect of experiencing at least one ACE (Any ACE) and the cumulative effect (Sum of ACEs) are significant with the strength and magnitude of association reflected in ORs ranging from 1.37 to 3.67. After controlling for age, gender, tribal affiliation, and school attendance, each additional ACE increased the odds of depression symptoms 57 %, poly-drug use 51 %, PTSD symptoms 55 %, and lifetime suicide attempt 37 %.
Table 4 includes the effect of all 8 ACEs, including discrimination and historical loss associated symptoms in participants younger than 19 years. The odds of depression symptoms (p < .05), poly-drug use (p < .001) and PTSD symptoms (p < .001) were strongly and significantly higher in those with higher levels of historical loss associated symptoms, while the odds of poly-drug use (p < .001) and PTSD symptoms (p < .05) were higher in those who had greater experiences of discrimination.
Discussion
In this study, we explored ACEs common to other populations, and we included factors which may uniquely contribute to increased likelihood of lifetime depression, poly-drug use, PTSD, and suicide among Native Americans. Discrimination and historical loss associated symptoms are relevant ACE factors for Native American populations. The exploration of these relationships reflects the importance of examining tribal health status partly as a function of collective trauma. We found a high prevalence of adverse experiences, and a significant dose–response relationship between the number of adverse exposures and mental health and risk behavior outcomes. These findings suggest a strong and cumulative impact of the number of types of ACE exposures among this sample of adolescents and young adults. Results of this study also found similar relationships between adversity and outcomes as were reported in the CDC/Kaiser ACE study (Dube et al. 2001, 2002, 2002, 2003; Felitti et al. 1998), even though the demographic characteristics of our sample were quite different. The prevalence of ACEs in this rural, reservation sample is higher than in the ACE study of primarily white, urban adults in San Diego County in which 52 % reported at least one of seven ACEs (psychological, physical or sexual abuse, violence against mother, living with household members who were substance users, mentally ill, suicidal or ever imprisoned; Felitti et al. 1998). There were similar rates of sexual abuse in the CDC/Kaiser ACE study compared to our study (22.0 vs. 20.1 %) but different rates of physical abuse, (10.8 vs. 29.8 %) and witness of IPV (12.5 vs. 40.1 %). The National Comorbidity Study (NCS), a representative sample of participants ages 15–54 years old (N = 8098), found that 74 % of participants reported at least one of twenty-six ACEs (Kessler et al. 1997), none of which were comparable with the eight ACEs we selected. In a study of Native American adults ages 18–70 years old (N = 309) ACEs among a sample from eight reservations, Ehlers et al. found that 94 % reported experiencing at least one of seven types of trauma, with similar rates of sexual abuse as compared to our sample (22.0 vs. 20.1 %; Ehlers et al. 2013). However, caution should be taken when making comparisons between other ACE studies and ours given that estimates of ACEs vary widely depending on sampling, operational definitions of ACEs, and measurement methodology.
Each of the five categories of abuse and neglect (physical, emotional, and sexual abuse; physical and emotional neglect) were significantly associated with depression symptoms, poly-drug use, PTSD symptoms, and suicide attempt, with physical and emotional abuse increasing the odds of all four outcomes. These findings are consistent with other studies linking abuse and neglect to mental health and risk behavior outcomes (Duke et al. 2010; Durant et al. 2000; Schilling et al. 2007). However, we did not find a significant relationship between sexual abuse and suicide attempt as was found in other studies of non-Indigenous populations (Dube et al. 2001; Schilling et al. 2007). The rate of violent victimization (rape, sexual assault, robbery, aggravated assault, and simple assault) is highest among Native Americans in comparison to other ethnic groups at 42.2 violent victimizations per 1000 persons age 12 or older—a rate more than twice that of blacks, 2.5 times that of Hispanics, 3 times that of whites, and 6.5 times that of Asians (Truman et al. 2013). Given that Native American children experience higher rates of maltreatment when compared to other children in the US, our findings contribute importantly to understanding the implications of child abuse and neglect in reservation communities (US Department of Health and Human Services 2010).
We found those who were witness to their mother’s abuse (IPV exposure) had significant increased odds of depressive symptoms, poly-drug use, PTSD symptoms, and suicide attempt. Although males more than females, and the 20–24 year age group more than the 15–19 year age group, were more likely to have witnessed this type of violence, there were no significant demographic differences. Those attending school were less likely to report witness of violence against their mother compared to those not attending school, which is consistent with other studies in the literature that have found witnessing IPV to be associated with poor school performance and not completing high school (Tajima et al. 2011; Thompson and Trice-Black 2012). Children who witness this abuse are at risk of emotional and behavioral problems, aggressive behavior, depressive symptoms, and poorer academic performance (Lepore and Kliewer 2013; Russell et al. 2010; Thompson and Trice-Black 2012; Yates et al. 2003). Native American women were found to be at increased risk of intimate partner violence in the 2010 CDC population based study (Black et al. 2011).
Historical trauma experiences including loss of language, culture, and land that occurred over 100 years ago persist today as expressed in historical loss associated symptoms and discrimination reported by these Native American adolescents and young adults. We found that high rates of historical loss associated symptoms were strongly associated with an increased risk of depression symptoms, poly-drug use, and PTSD symptoms, but not suicide attempt, when compared to those with low historical loss associated symptoms. For those reporting discrimination (80 %), the odds of poly-drug use and PTSD symptoms was greatly increased, compared to those without this exposure. This is one of the first studies that links historical loss associated symptoms and discrimination with the oft noted higher prevalence of child abuse and intimate partner violence among Indigenous Peoples in the US and globally.
The ACEs explored in our study, including discrimination and the memory of historical trauma work in tandem to add immeasurably to the inherent difficulties in the development of children who live on reservations. The high prevalence of such childhood experiences among this and other Native American samples, in addition to increased prevalence of other problem outcomes, demonstrate the particular vulnerability of this population. Gender, tribal affiliation, age, and school attendance were factors associated with the ACEs and influenced these outcomes. Prior research on adversity in childhood has focused on proximal and individual factors and has been restricted to one or two outcomes. This narrow perspective has limited our understanding of the full range of factors including collective tribal experiences, historical and contemporary, which affect reservation-based Native American youth. Our study begins to address this knowledge gap.
This study has limitations that should be noted. First, the study was limited to a one reservation, two-tribe convenience sample; therefore, it cannot be generalized to the broader Native American population. At the same time, it should be noted that this reservation is not unlike many isolated, rural reservations with similar socio-economic profiles and historical trauma experiences. Second, the study is cross-sectional and causal relationships cannot be inferred from the identified associations. Third, data were self-reported and thus subject to recall bias; however, the young age of this sample may minimize this concern and research suggests that the false positive disclosures of trauma are unlikely (Hardt and Rutter 2004). Finally, due to multiple comparisons the results should be considered preliminary. When Bonferroni corrections were applied to the final models (Table 3) all variables significant at p < .05 were no longer significant, although, those significant at (p < .001) were still significant. Despite these methodological limitations this study is unique and expands upon what is known about ACEs in its examination of multiple experiences and outcomes among high-risk reservation-based Native American adolescents and young adults.
Conclusions
Our findings indicate that abuse and neglect, witnessing violence against one’s mother, historical loss associated symptoms and discrimination are common and strongly linked to depression symptoms, poly-drug use, PTSD symptoms, and suicide attempt among this sample. Further research is needed to understand the most effective and feasible ways to intervene. Additional research is also needed to understand how the risk behaviors of Native American youth can be addressed at multiple levels, not just through individually focused interventions. Future studies should include prospective longitudinal designs using a diverse Native American sample and strive to develop and test community informed and culturally specific interventions for Native Americans. Investigators could focus on primary prevention such as the early identification and care of the risk factors for ACEs in this population. The American Academy of Pediatrics (AAP) advocates primary care providers (PCP) screen parents for factors that could put their children at increased risk for child abuse and trauma including parental substance abuse, depression, and suicide as well as exposure to IPV and other traumas (Hagan et al. 2008). In addition, Indigenous knowledge and practices aimed at addressing historical trauma, and community efforts to counteract and deconstruct structural racism and unequal treatment for Indigenous Peoples must be encouraged and supported.
References
Anda, R. F., Whitfield, C. L., Felitti, V. J., Chapman, D., Edwards, V. J., Dube, S. R., & Williamson, D. F. (2002). Adverse childhood experiences, alcoholic parents, and later risk of alcoholism and depression. Psychiatric Services, 53(8), 1001–1009.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Manual for the Beck depression inventory-II. San Antonio, TX: Psychological Corporation.
Bernstein, D. P., & Fink, L. (1998). Childhood Trauma Questionnaire: A retrospective self-report. San Antonio, TX: Psychological Corporation.
Bernstein, D. P., Stein, J. A., Newcomb, M. D., Walker, E., Pogge, D., Ahluvalia, T., & Desmond, D. (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse and Neglect, 27(2), 169–190.
Black, M., Basile, K., Breiding, M., Smith, S., Walters, M., Merrick, M., & Stevens, M. (2011). National intimate partner and sexual violence survey: 2010 summary report National Center for Injury Prevention and Control. Atlanta, GA: Centers for Disease Control and Prevention.
Bohnert, K. M., & Breslau, N. (2011). Assessing the performance of the short screening scale for post-traumatic stress disorder in a large nationally-representative survey. International Journal of Methods in Psychiatric Research, 20(1), e1–e5. doi:10.1002/mpr.331.
Brave Heart, M. Y. H., & DeBruyn, L. (1998). The American Indian Holocaust: Healing historical unresolved grief. American Indian Alaska Native Mental Health Research: The Journal of the National Center, 8(2), 60–82.
Breslau, N., Peterson, E., Kessler, R., & Schultz, L. (1999). Short screening scale for DSM-IV posttraumatic stress disorder. American Journal of Psychiatry, 156(6), 908–911.
Brockie, T. N., Heinzelmann, M., & Gill, J. (2013). A framework to examine the role of epigenetics in health disparities among Native Americans. Nursing Research and Practice, 2013, 410395. doi:10.1155/2013/410395.
Bureau of Indian Affairs. (2008). 115-8 Bureau of Indian Affairs General Assistance. Washington, DC. http://dpaweb.hss.state.ak.us/manuals/admin/115/115-8.htm
Centers for Disease Control and Prevention. (2012). 2009 National High School Youth Risk Behavior Survey (YRBS) Questionnaire. Atlanta, GA: US Department of Health and Human Services.
Chaix, B., Jouven, X., Thomas, F., Leal, C., Billaudeau, N., Bean, K., & Danchin, N. (2011). Why socially deprived populations have a faster resting heart rate: Impact of behaviour, life course anthropometry, and biology—The RECORD Cohort Study. Social Science and Medicine, 73(10), 1543–1550. doi:10.1016/j.socscimed.2011.09.009.
De Ravello, L., Abeita, J., & Brown, P. (2008). Breaking the cycle/mending the hoop: Adverse childhood experiences among incarcerated American Indian/Alaska Native women in New Mexico. Health Care for Women International, 29(3), 300–315. doi:10.1080/07399330701738366.
Diez Roux, A. V. (2003). Residential environments and cardiovascular risk. Journal of Urban Health, 80(4), 569–589.
Diez Roux, A. V., Jacobs, D. R., & Kiefe, C. I. (2002). Neighborhood characteristics and components of the insulin resistance syndrome in young adults: The coronary artery risk development in young adults (CARDIA) study. Diabetes Care, 25(11), 1976–1982.
Dube, S. R., Anda, R. F., Felitti, V. J., Chapman, D. P., Williamson, D. F., & Giles, W. H. (2001). Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: Findings from the Adverse Childhood Experiences Study. JAMA, 286(24), 3089–3096.
Dube, S. R., Anda, R. F., Felitti, V. J., Edwards, V. J., & Croft, J. B. (2002a). Adverse childhood experiences and personal alcohol abuse as an adult. Addictive Behaviors, 27(5), 713–725.
Dube, S. R., Anda, R. F., Felitti, V. J., Edwards, V. J., & Williamson, D. F. (2002b). Exposure to abuse, neglect, and household dysfunction among adults who witnessed intimate partner violence as children: Implications for health and social services. Violence and Victims, 17(1), 3–17.
Dube, S. R., Felitti, V. J., Dong, M., Chapman, D. P., Giles, W. H., & Anda, R. F. (2003). Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: The adverse childhood experiences study. Pediatrics, 111(3), 564–572.
Duke, N. N., Pettingell, S. L., McMorris, B. J., & Borowsky, I. W. (2010). Adolescent violence perpetration: Associations with multiple types of adverse childhood experiences. Pediatrics, 125(4), e778–e786. doi:10.1542/peds.2009-0597.
Duran, E. (2006). Healing the soul wound: Counseling with American Indians and other native peoples. New York, NY: Teachers College Press.
Duran, E., Duran, B., Brave Heart, M. Y. H., & Yellow Horse-Davis, S. (1998). Healing the American Indian soul wound. In Y. Danieli (Ed.), International handbook of multigenerational legacies of trauma (pp. 341–354). New York: Plenum Press.
Durant, R. H., Altman, D., Wolfson, M., Barkin, S., Kreiter, S., & Krowchuk, D. (2000). Exposure to violence and victimization, depression, substance use, and the use of violence by young adolescents. Journal of Pediatrics, 137(5), 707–713. doi:10.1067/mpd.2000.109146.
Ehlers, C. L., Gizer, I. R., Gilder, D. A., & Yehuda, R. (2013). Lifetime history of traumatic events in an American Indian community sample: Heritability and relation to substance dependence, affective disorder, conduct disorder and PTSD. Journal of Psychiatric Research, 47(2), 155–161. doi:10.1016/j.jpsychires.2012.10.002.
Elias, B., Mignone, J., Hall, M., Hong, S. P., Hart, L., & Sareen, J. (2012). Trauma and suicide behaviour histories among a Canadian indigenous population: An empirical exploration of the potential role of Canada’s residential school system. Social Science and Medicine, 74(10), 1560–1569. doi:10.1016/j.socscimed.2012.01.026.
Evans-Campbell, T., Walters, K. L., Pearson, C. R., & Campbell, C. D. (2012). Indian boarding school experience, substance use, and mental health among urban two-spirit American Indian/Alaska natives. American Journal of Drug and Alcohol Abuse, 38(5), 421–427. doi:10.3109/00952990.2012.701358.
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., & Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258.
Flaherty, E. G., Thompson, R., Dubowitz, H., Harvey, E. M., English, D. J., Proctor, L. J., & Runyan, D. K. (2013). Adverse childhood experiences and child health in early adolescence. JAMA Pediatrics, 167(7), 622–629. doi:10.1001/jamapediatrics.2013.22.
Freedenthal, S., & Stiffman, A. R. (2004). Suicidal behavior in urban American Indian adolescents: A comparison with reservation youth in a southwestern state. Suicide and Life-Threatening Behavior, 34(2), 160–171.
Hagan, J., Shaw, J., & Duncan, P. (2008). Bright futures: Guidelines for health supervision of infants, children, and adolescent (3rd ed.). Elk Grove Village, IL: The American Academy of Pediatrics.
Hamby, S., Finkelhor, D., Turner, H., & Ormrod, R. (2010). The overlap of witnessing partner violence with child maltreatment and other victimizations in a nationally representative survey of youth. Child Abuse and Neglect, 34(10), 734–741. doi:10.1016/j.chiabu.2010.03.001.
Hardt, J., & Rutter, M. (2004). Validity of adult retrospective reports of adverse childhood experiences: Review of the evidence. Journal of Child Psychology and Psychiatry, 45(2), 260–273.
Kessler, R. C., Davis, C. G., & Kendler, K. S. (1997). Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychological Medicine, 27(5), 1101–1119.
Kimerling, R., Ouimette, P., Prins, A., Nisco, P., Lawler, C., Cronkite, R., & Moos, R. H. (2006). Brief report: Utility of a short screening scale for DSM-IV PTSD in primary care. Journal of General Internal Medicine, 21(1), 65–67.
Koss, M. P., Yuan, N. P., Dightman, D., Prince, R. J., Polacca, M., Sanderson, B., & Goldman, D. (2003). Adverse childhood exposures and alcohol dependence among seven Native American tribes. American Journal of Preventive Medicine, 25(3), 238–244.
Lawman, H. G., & Wilson, D. K. (2012). A review of family and environmental correlates of health behaviors in high-risk youth. Obesity, 20(6), 1142–1157.
Lepore, S. J., & Kliewer, W. (2013). Violence exposure, sleep disturbance, and poor academic performance in middle school. Journal of Abnormal Child Psychology, 41(8), 1179–1189.
Moore, M. (2006). Conference explores racism in cities near reservations, Missoulian. http://missoulian.com/news/state-and-regional/conference-explores-racism-in-cities-near-reservations/article_95c8c9df-754a-5812-b4c8-a8aaff2f67b1.html.
Mota, N., Elias, B., Tefft, B., Medved, M., Munro, G., & Sareen, J. (2012). Correlates of suicidality: Investigation of a representative sample of Manitoba First Nations adolescents. American Journal of Public Health, 102(7), 1353–1361. doi:10.2105/ajph.2011.300385.
O’Campo, P., Xue, X., Wang, M. C., & Caughy, M. (1997). Neighborhood risk factors for low birthweight in Baltimore: A multilevel analysis. American Journal of Public Health, 87(7), 1113–1118.
Russell, D., Springer, K. W., & Greenfield, E. A. (2010). Witnessing domestic abuse in childhood as an independent risk factor for depressive symptoms in young adulthood. Child Abuse and Neglect, 34(6), 448–453.
Schilling, E., Aseltine, R, Jr, & Gore, S. (2007). Adverse childhood experiences and mental health in young adults: A longitudinal survey. BMC Public Health, 7, 30. doi:10.1186/1471-2458-7-30.
Sittner Hartshorn, K. J., Whitbeck, L. B., & Hoyt, D. R. (2012). Exploring the relationships of perceived discrimination, anger, and aggression among North American indigenous adolescents. Society and Mental Health, 2(1), 53–67.
Tajima, E., Herrenkohl, T., Moylan, C., & Derr, A. (2011). Moderating the effects of childhood exposure to intimate partner violence: The roles of parenting characteristics and adolescent peer support. Journal of Research on Adolescence, 21(2), 376–394.
Thompson, E. H., & Trice-Black, S. (2012). School-based group interventions for children exposed to domestic violence. Journal of Family Violence, 27(3), 233–241. doi:10.1007/s10896-012-9416-6.
Truman, J., Langton, L., & Platy, M. (2013). Criminal victimization, 2012. Washington, DC: Office of Justice Programs.
US Census Bureau. (2010). Small area income and poverty estimates. http://www.census.gov/did/www/saipe/methods/statecounty/2010county.html.
University of Wisconsin Population Health Institute. (2010). County health rankings & roadmaps: A healthier nation, county by county. www.countyhealthrankings.org.
US Department of Health and Human Services. (2010). Child Maltreatment 2009. Washington, DC: Administration on Children, Youth and Families, Children Bureau.
Walls, M., Chapple, C., & BJohnson, K. (2007). Strain, emotion, and suicide among American Indian youth. Deviant Behavior, 28(3), 219–246. doi:10.1080/01639620701233100.
Whitaker, D., Milam, A. J., Graham, C. M., Cooley-Strickland, M., Belcher, H. M., & Furr-Holden, C. D. (2013). Neighborhood environment and urban schoolchildren’s risk for being overweight. American Journal of Health Promotion, 27(6), 410–416.
Whitbeck, L., Adams, G., Hoyt, D., & Chen, X. (2004a). Conceptualizing and measuring historical trauma among American Indian people. American Journal of Community Psychology, 33(3–4), 119–130.
Whitbeck, L., Chen, X., Hoyt, D., & Adams, G. (2004b). Discrimination, historical loss and enculturation: Culturally specific risk and resiliency factors for alcohol abuse among American Indians. Journal of Studies on Alcohol, 65(4), 409–418.
Whitbeck, L., Hoyt, D., McMorris, B., Chen, X., & Stubben, J. (2001). Perceived discrimination and early substance abuse among American Indian children. Journal of Health and Social Behavior, 42, 405–424.
Whitbeck, L., McMorris, B., Hoyt, D., Stubben, J., & Lafromboise, T. (2002). Perceived discrimination, traditional practices, and depressive symptoms among American Indians in the upper Midwest. Journal of Health and Social Behavior, 43(4), 400–418.
Whitbeck, L., Walls, M., Johnson, K., Morrisseau, A., & McDougall, C. (2009). Depressed affect and historical loss among North American indigenous adolescents. American Indian Alaska Native Mental Health Research, 16(3), 16–41.
Yates, T. M., Dodds, M. F., Sroufe, L. A., & Egeland, B. (2003). Exposure to partner violence and child behavior problems: A prospective study controlling for child physical abuse and neglect, child cognitive ability, socioeconomic status, and life stress. Development and Psychopathology, 15(1), 199–218.
Acknowledgments
We gratefully acknowledge Dr. John Umhau, Indian Health Service, for his expertise. This work was supported in part by the intramural research program at the National Institutes of Health Clinical Center and the Johns Hopkins Bloomberg School of Public Health Center for American Indian Health.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brockie, T.N., Dana-Sacco, G., Wallen, G.R. et al. The Relationship of Adverse Childhood Experiences to PTSD, Depression, Poly-Drug Use and Suicide Attempt in Reservation-Based Native American Adolescents and Young Adults. Am J Community Psychol 55, 411–421 (2015). https://doi.org/10.1007/s10464-015-9721-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10464-015-9721-3