Abstract
Low-barrier care is one model of a differentiated service delivery approach for people with HIV (PWH) who are not engaged in conventionally-organized HIV care. Although psychiatric and substance use disorders are common among patients in low-barrier clinics, approaches to behavioral health service delivery within this context have not been well-described. We conducted a descriptive analysis using retrospective review of medical records to evaluate substance use and psychiatric comorbidities and receipt of behavioral health services among patients in the Max Clinic in Seattle, Washington. Among 227 patients enrolled from 2015 to mid-2020, most had a history of hazardous substance use (85%), a psychiatric diagnosis (69%) or unstable housing (69%) documented in the medical record. Less than half of patients referred for depression treatment (33%) or for opioid use disorder treatment (40%) completed even one specialty care visit. More effective approaches are needed to engage patients in behavioral health services within the context of low-barrier HIV care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Addressing behavioral health needs in tandem with HIV treatment is important for providing optimal care to people with HIV (PWH) [1,2,3]. For some people with HIV, substance use and psychiatric disorders pose substantial barriers to effective engagement in treatment, especially when compounded by poverty, unstable housing, social isolation, incarceration, and stigma [4,5,6,7]. Even when substance use and mental health services are successfully integrated into HIV clinics, they do not reach a subset of PWH who are incompletely engaged in conventional clinical services. Particularly for people living homeless or unstably housed, it can be difficult to attend regular HIV primary care visits scheduled for a specific date and time in the context of unstable life circumstances and the need to meet basic sustenance needs on a day-to-day basis [7,8,9,10,11]. A differentiated service delivery approach is required to effectively engage high-need, complex PWH who are not reached by existing systems of care.
Low-barrier HIV care is one example of a differentiated service delivery strategy for PWH who have complex medical and social needs [8– [9, 12]–13, 14]. The components that distinguish the low-barrier clinic models from conventionally-organized HIV medical care include provision of comprehensive primary care on a walk-in basis (no scheduled appointments), integrated medical and non-medical case management to address social needs as part of medical care, and provision of tangible incentives (such as gift cards and cash) for visits to the clinic and viral suppression. The Max Clinic in Seattle, Washington [8], the POP-UP Clinic in San Francisco, California [13], and the MAT (Maximally Assisted Therapy) Program in Vancouver, British Columbia, Canada, are examples of this model that have been previously described, but the extent of low-barrier care provision is likely not fully reflected in the peer-reviewed literature. The Max Clinic [8], which is the focus of this analysis, was previously demonstrated to improve viral suppression among PWH with a high prevalence of substance use and psychiatric disorders [13].
Although the Max Clinic was designed to engage PWH with complex barriers to care such as substance use disorders, psychiatric disorders, and unstable housing, the clinic evolved without integrated behavioral health services. This was due to several factors: the clinic initially had a relatively small number of patients enrolled, which did not justify the need for full or part-time mental health services, space and funding constraints, and existing specialty mental health and addiction services located on the same medical campus. However, the first five years of anecdotal experience in the Max Clinic raised concern that despite the geographic proximity to a range of behavioral health services, there appeared to be low levels of patient engagement in specialty mental health and addiction services. Concern that the clinic’s approach was ineffective prompted the development of this study.
To guide development and implementation of behavioral health services in the Max Clinic and to inform the delivery of behavioral healthcare in low-barrier HIV clinics more broadly, we analyzed the substance use and mental health comorbidities and receipt of behavioral health services among Max Clinic patients. This was a descriptive study, and as such, we did not design it to test a hypothesis. This work is broadly relevant because it focuses on high-need PWH who require more intensive support than what is offered through most conventional HIV clinics. To our knowledge, this study is the first to characterize substance use, psychiatric comorbidities, and receipt of specialty care in a low-barrier, clinic-based setting. Although the local context and resources to provide care to this priority population varies substantially throughout the U.S., the issue of addressing behavioral health among high-need PWH is universal. Relatively little is understood about how to best engage high-need PWH in behavioral health services. Using electronic health record (EHR) data, we measured the prevalence of specific psychiatric diagnoses and substance use disorders in Max Clinic as well as service receipt, including medications prescribed in clinic, referrals to specialty care, and completed specialty visits.
Methods
Setting
Individuals enrolled in care at the Max Clinic are primarily identified through referrals from clinicians, case managers, and the health department as PWH who are not engaged in care and are not virally suppressed. The Max Clinic uses a walk-in, incentivized care model with the goal of re-engaging and retaining these patients in care. This model includes walk-in primary care, financial incentives for laboratory testing and suppression of viral load, intensive case management from social work and health department staff (including provision of vouchers for transportation, clothing, food, and other necessities) and care coordination with other agencies the patients encounter, such as day support programs, jail, supportive housing, opioid treatment programs, community mental health agencies, and inpatient hospitals [8]. The staff includes HIV physicians, social workers, and health department disease intervention specialists. At the time of this analysis, only two of five Max Clinic physicians prescribed buprenorphine.
Study Population
The study included patients who enrolled in the Max Clinic between January 01, 2015, and June 30, 2020, excluding those enrolled for less than one month prior to death, transfer of care, or the end of the analysis period.
Data Collection
We used the clinic administrative database to determine the date of initial enrollment for each participant, defined as the date of the first visit with a medical provider in the clinic. Information on patient demographic characteristics was extracted from the EHR (Epic Systems, Verona, WI) and the Ryan White services database. Race/ethnicity, sex at birth, and gender are patient-reported measures collected during the clinic registration process. All other variables used in this analysis were collected through review of individual EHRs. One investigator collected the data using a structured form and focused her review on the problem list, clinical notes from social workers and medical providers, medication list, referrals, and laboratory results. This process included both manual review and free text searches for key words and diagnoses within the EHR. A second reviewer re-reviewed charts to capture additional detail on housing status. A third reviewer performed additional chart review to resolve questions that arose during the primary review. We matched data on housing from the chart review with records in a housing database maintained by the Max Clinic social workers. Data were entered into a Research Electronic Data Capture database (REDCap, Nashville, TN).
Variable Definitions
Substance Use
Substance use and injection drug use were defined as documented in the EHR for the year prior to the enrollment date, and separately, as ascertained after the time of enrollment. We chose the timeframe of one year prior to focus on the patients most likely to have active substance use at the time of clinic entry. Documentation in the chart included ICD-10 codes related to general substance use, the use of specific substances, and substance use disorders in the problem list, mention of substance use in the visit diagnoses, and any report of substance use in the free text of the note. We analyzed all documented use of non-prescribed substances, regardless of whether the patient was diagnosed with a substance use disorder. This was because it was rarely explicitly stated in the EHR whether diagnostic criteria for a substance use disorder was met, despite clear documentation of substance use. We categorized substance-specific use including heroin, methamphetamine or cocaine/crack cocaine (combined into the category of psychostimulants for the analysis), hazardous alcohol use, marijuana, non-prescribed opioids (e.g. oxycodone), non-prescribed benzodiazepines, or “none of the above.” This list of substances was determined by researchers prior to initiation of the study. In addition to the chart elements described above, this variable included urine drug test results positive for the above substances. Of note, we use the term “heroin” use because this was the term typically used in medical records documentation, although local data demonstrate that the use of fentanyl was rapidly increasing during the period of this analysis [15]. Hazardous alcohol use was defined by the problem list and authors of clinical notes. We categorized patients as having hazardous alcohol use if “heavy” or “binge” drinking were noted or a diagnosis of alcohol use disorder was documented. For patients with polysubstance use, each substance was recorded individually.
Psychiatric Comorbidities
Psychiatric diagnoses were assessed for any time prior to enrollment (i.e., lifetime history), and separately, as new diagnoses after the time of enrollment. Data on psychiatric diagnoses was obtained through review of the EHR, including ICD-10 codes, psychiatric conditions reported in the problem list and/or visit diagnoses, and any documentation of psychiatric diagnoses within the free text of the note. Psychiatric comorbidities were categorized as depressive disorder, anxiety disorder, bipolar disorder, psychosis (including schizophrenia and psychotic disorder not otherwise specified), post-traumatic stress disorder, personality disorder (including borderline personality disorder and obsessive-compulsive personality disorder), and none of the above. The list of included psychiatric comorbidities was determined by the researchers prior to initiation of data collection. For patients with multiple diagnoses, each disorder was recorded individually. For the analysis of comorbid conditions, we examined diagnoses in four specific categories: depressive disorders, anxiety disorders, bipolar and related disorders, and psychoses.
Housing Status
Housing status was defined as of the enrollment date, ascertained in notes on that day or shortly preceding or following that time. We collected the data in detailed categories, which were dichotomized for analysis. “Homelessness/unstable housing” included those who were homeless (staying in a shelter or sleeping outside), couch-surfing or staying temporarily with friends and family, staying in hotels or motels, or in transitional housing (e.g. after release from incarceration or temporary housing provided by an agency). “Stable housing” included those in permanent supportive housing and those living in a private residence.
Treatment at the Time of Enrollment
For patients with documentation of substance use or psychiatric comorbidities at the time of enrollment, we reported treatment started before Max Clinic enrollment, including prescribed psychiatric medications or medications for opioid use disorder (MOUD; methadone, buprenorphine, or naltrexone), involvement with counseling or recovery groups, or establishment with other community agencies providing mental health or substance use recovery services.
Initiation of Pharmacologic Treatment at the Max Clinic
Medications prescribed in the Max Clinic for treatment of substance use disorders or psychiatric diagnoses were ascertained through a combination of the medication lists and medical provider notes, distinguishing the rationale for using a medication specifically to treat these disorders from other indications. Data collected on medications prescribed at the Max Clinic for substance use disorders included buprenorphine for opioid use, naltrexone for alcohol and opioid use, and mirtazapine for methamphetamine use. Medications prescribed for psychiatric conditions included selective serotonin reuptake inhibitors (SSRIs), antipsychotics, and lithium.
Referral to and Receipt of Specialty Care
Among patients with psychiatric comorbidities, we reviewed whether these patients were referred to specialty substance use or mental health care outside of the Max Clinic. For substance use, this included 12-step programs, counseling or other outpatient programs for substance use recovery, residential or inpatient substance use treatment programs or detoxification facility admission. For psychiatric comorbidities, this included referrals to mental health services at both community agencies and several specialty clinics affiliated with Seattle’s primary safety net hospital and located on the same medical campus as the Max Clinic. For the analysis of referrals for substance use treatment, we focused on MOUD (outpatient buprenorphine, naltrexone or methadone).
Among patients who were offered, accepted, and received behavioral health service referrals, we reviewed whether the patient attended 0, 1, or ≥ 2 specialty appointments. We captured patient declinations of referral offers when documented. For specialty services with records inaccessible through the Max Clinic’s EHR, including community counseling agencies and opioid treatment programs, we reviewed Max Clinic provider text notes for documentation of follow-up visits reported by patients. The Max Clinic social workers track completion of referrals.
Analysis
We performed a descriptive analysis of patient characteristics, substance use and mental health comorbidities, housing, and service referrals and receipt. For behavioral health disorders, we calculated the number and proportion of patients with overlapping comorbidities to determine the prevalence and type of polysubstance use and psychiatric comorbidities. To determine the extent that these categories overlapped with housing status, we calculated the proportion with any psychiatric disorder, any substance use disorder, and/or unstable housing and displayed the results in a Venn Diagram.
We described behavioral health treatment, referrals, and completion of specialty visits within each group as the proportion who received pharmacologic treatment in the Max Clinic, were referred for specialty care, completed the initial specialty care appointment, and completed ≥ 2 specialty care appointments (a subset of those who completed the initial appointment). Pharmacologic treatment at the Max Clinic and referrals for specialty care were not mutually exclusive. All analyses were conducted using Stata V.16. The University of Washington IRB approved this analysis.
Results
Patient Characteristics
A total of 227 patients were included in the analyses. Patients had a mean age of 40 years (SD = 10), most were male (72%), and most were either non-Hispanic White (52%) or non-Hispanic Black (28%) (Table 1). Most patients had documented substance use in the year prior to enrollment (85%), most commonly methamphetamine (60%) and/or heroin (30%). 42% of all patients had a chart notation of injection drug use within the past year. 69% of patients had a previously diagnosed psychiatric disorder, most commonly a depressive disorder (51%) or anxiety (26%), followed by psychosis (19%) and bipolar disorder (16%). Most patients (69%) were unstably housed with 41% sleeping outside or in a shelter.
Substance Use and Psychiatric Comorbidities
The overlap between substance use and psychiatric diagnoses is demonstrated in Table 2. Among those who used heroin, most (78%) also used psychostimulants, whereas one-third of people who used psychostimulants also used heroin. Among patients with at least one psychiatric diagnosis (N = 157), 61% had at least one co-occurring psychiatric disorder. Approximately one-fifth of patients with a depressive disorder had a comorbid psychotic disorder.
Substance use and psychiatric disorders commonly co-occurred. Among the 68 patients who used heroin, half had a diagnosed depressive disorder and nearly one-quarter had a diagnosed psychotic disorder. The overlap between psychostimulant use and diagnosed anxiety disorders or psychosis was also common: 82% of patients with an anxiety disorder and 77% of patients with a psychotic disorder used psychostimulants.
Overlap of Substance Use and Psychiatric Diagnosis with Unstable Housing
Almost all (97%) patients had either substance use, psychiatric diagnoses, or unstable housing at the time of enrollment; 42% had all three (Fig. 1). Among patients with either substance use or psychiatric diagnoses, most (71%) were unstably housed, and 99% of patients who were unstably housed (N = 157) had either a psychiatric diagnosis (8%), substance use (30%) or both (61%).
Overlap of substance use, psychiatric diagnoses and unstable housing among Max Clinic patients enrolled 2015-19 (N = 227). Note: Size of the circles is not to scale. Six people do not fit into any circle. a Includes those using at least one of the following at baseline: Methamphetamine, heroin, cocaine/crack cocaine, hazardous alcohol use, marijuana, prescription-type opioids, prescription-type benzodiazepines. b Includes those diagnosed with at least one of the following at baseline: Depressive d/o, bipolar and related d/o, anxiety d/o, trauma and stressor-related d/o, PTSD, schizophrenia spectrum and other psychotic disorders, ADD, personality disorders, feeding and eating disorders. c Includes those sleeping outside, staying in a shelter, in transitional housing, or unstable housing (couch-surfing etc.)
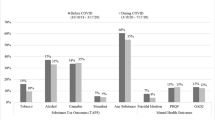
Pharmacologic Treatment, Specialty Care Referral and Completion of Referrals
Among patients who used heroin, 35% received MOUD in the Max Clinic and 63% were referred for specialty care (Table 3). Of those referred, fewer than half (40%) had documentation of attending even one specialty appointment. Although most who completed the initial appointment completed at least one additional appointment, that group comprised only 19% of all patients using heroin. Among patients with methamphetamine use, 26% received pharmacologic treatment in the Max Clinic and 35% were referred for specialty care; of whom 38% completed an initial specialty care appointment and 21% completed at least one follow-up appointment (7% of all patients who were using methamphetamine).
Among patients with depressive disorder diagnoses, 50% received pharmacologic treatment in the Max Clinic and 71% were referred for specialty care. As with substance use treatment referrals, fewer than half (33%) completed even one specialty appointment. The referral and appointment completion patterns were similar for patients with anxiety disorder, with 53% of patients receiving pharmacologic treatment in the Max Clinic, 72% referred to specialty care, and 35% completing the initial specialty appointment. Among the patients with psychiatric diagnoses in other categories, including both psychosis and bipolar disorder, proportionately more received pharmacologic treatment in the Max Clinic (57%), and among those referred (69%), proportionately more completed at least one specialty medical appointment (40%). However, fewer than half of the referred population in any category completed any specialty care appointments.
Discussion
In this analysis of substance use and mental health comorbidities and service receipt among patients enrolled in a low-barrier HIV clinic, complex comorbidities were common but successful completion of referrals to specialty behavioral health services were relatively rare. Overall, 96% of patients had either a psychiatric disorder or substance use, and 42% had concurrent psychiatric diagnoses, substance use, and unstable housing. Less than half of patients referred for depression treatment (33%) or for opioid use disorder treatment (40%) completed even one specialty care visit. Furthermore, even among the minority of Max Clinic patients who attended at least one specialty visit, few were retained in care as measured by completion of at least two specialty visits. These findings quantify the complexity of substance use and mental health comorbidities among a population enrolled in low-barrier HIV care, confirm the Max Clinic team’s experience that referrals to external clinics were not working well for patients, and highlight the need for healthcare system changes to more effectively engage low-barrier clinic patients in behavioral health services.
One strategy to address low completion of specialty referrals would be to integrate behavioral health care into the Max Clinic. The effectiveness of integrated behavioral care models and comprehensive, on-site services is well-documented. The HIV Translating Initiatives for Depression Into Effective Solutions (HITIDES) Study [16] and the Strategies to Link Antidepressant and Antiretroviral Management (SLAM DUNC) Study [17], both randomized controlled trials, supported integrated HIV and depression treatment as an effective strategy to improve mental health treatment response among PWH. A controlled trial of integrated buprenorphine/naloxone and HIV clinical care by Sullivan et al. showed similar promise with integrated HIV and opioid use disorder treatment, with significant reductions in opioid use and stable or improving HIV markers among participants [18]. These studies provided insight into the value of integrating HIV and behavioral health care, but exclusion of patients with psychosis and/or bipolar disorder [16, 17]; concurrent use of cocaine, benzodiazepines, alcohol, or sedatives [18]; and without access to a telephone [16] limits the applicability of these studies to low-barrier clinics and, more generally, to populations of PWH who have complex needs. Integrating behavioral health services into the low-barrier care model has specific challenges distinct from standard clinics, particularly the need to provide all services on a walk-in basis [9]. Expanding Max Clinic services to include walk-in access to substance use and mental health treatment would provide the same flexibility with which patients access their other care and would eliminate the requirement to make appointments to access behavioral health services. Optimizing the ability of existing Max Clinic providers to meet these needs could help address the problem – with training and support to prescribe MOUD and psychiatric medications, for example – but additional strategies will almost certainly be needed to meaningfully improve engagement in behavioral health treatment. Evidence-based models to integrate behavioral health services into low-barrier HIV clinics are needed.
Beyond the inflexibility of pre-scheduled appointments, additional factors probably contribute to the low rate of specialty referral completion in the Max Clinic, which may not be addressed with integrated care. Patients may not think their mental health or substance use is a problem, may not be interested in behavioral health care, or may be reluctant to engage in mental health or substance use treatment based on past experience or perceptions about such treatment. Lack of access to transportation can be a barrier to completing health care appointments, but this is unlikely to be a primary explanation for the low engagement in behavioral health services we observed. All Max Clinic patients are offered unrestricted, no-cost public transportation passes (which can be used for the public bus, light rail system, and regional railway) as well as individualized transportation assistance to medical appointments for patients who have difficulty navigating the public transportation system. Additionally, when needed, Max Clinic team members directly transport patients to the hospital for specialty appointments. Bringing behavioral health services closer to where patients live or stay through mobile services could maximize the convenience of services [19], but whether this would be acceptable to patients is uncertain. Telehealth visits with behavioral health providers were not available during most of the analysis period, which might have improved patient completion of appointments had they been an option. Understanding the perspective of Max Clinic patients is key to developing solutions, and ongoing research in this area includes a qualitative study of patient perceptions.
This study was limited by its retrospective approach and our reliance on the EHR for data collection. The prevalence of comorbidities we report is almost certainly underestimated, and systematic screening would give a more accurate measure. Care providers do not always inquire about or document substance use, and patients may be unwilling to fully disclose this information. Some terms used in the EHR, like “hazardous alcohol use,” can be subjective and poorly defined, which may have led to inconsistencies in diagnosis across the patient population. Since care provision is fragmented across systems, we may have missed psychiatric diagnoses or completed specialty visits, although the intensive case management that is part of Max Clinic makes this less likely. This study did not assess the quality of care received, such as the dose and duration of medication prescription. Additionally, our low threshold for defining retention in behavioral health care based on the completion of only two visits probably did not reflect meaningful engagement in services. However, none of these limitations would change our primary conclusions that complex comorbidities are common in the Max Clinic population and behavioral health treatment is an unmet need.
In summary, we found that substance use and psychiatric comorbidities were extremely common among PWH enrolled in a low-barrier HIV clinic. These comorbidities were often compounded by homelessness or unstable housing, and attempts to link patients to specialty behavioral health services outside the clinic were usually unsuccessful. To successfully engage this patient population in behavioral health services, services need to address complex overlapping comorbidities and social factors common in this population, and provided services need to be more accessible, convenient, and acceptable to the patients. New approaches to behavioral health service delivery are needed to advance the quality of care for especially vulnerable and marginalized PWH in low-barrier care.
Data Availability
De-identified data may be available upon request.
Code Availability
SAS code available upon request.
References
Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet. 2010;376(9738):367–87.
Oldfield BJ, Munoz N, McGovern MP, et al. Integration of care for HIV and opioid use disorder. AIDS. 2019;33(5):873–84.
Chuah FLH, Haldane VE, Cervero-Liceras F, et al. Interventions and approaches to integrating HIV and mental health services: a systematic review. Health Policy Plan. 2017;32(suppl4):iv27–iv47.
Moher M, Erickson M, Black P, et al. Improving Post-Release Care Engagement for People living with HIV involved in the criminal justice system: a systematic review. AIDS Behav. 2022. https://doi.org/10.1007/s10461-021-03513-4.
Holtzman CW, Shea JA, Glanz K Mapping patient-identified barriers and facilitators to retention in HIV care and antiretroviral therapy adherence to Andersen’s Behavioral Model. AIDS Care., Hartzler B, Dombrowski JC, Crane HM et al. Prevalence and Predictors of Substance Use Disorders Among HIV Care Enrollees in the United States. AIDS Behav. 2017; https://doi.org/10.1007/s10461-016-1584-6.
Hartzler B, Dombrowski JC, Crane HM, et al. Prevalence and Predictors of Substance Use Disorders Among HIV Care Enrollees in the United States. AIDS Behav. 2017; https://doi.org/10.1007/s10461-016-1584-6
Yehia BR, Stewart L, Momplaisir F, et al. Barriers and facilitators to patient retention in HIV care. BMC Infect Dis. 2015. https://doi.org/10.1186/s12879-015-0990-0.
Dombrowski JC, Ramchandani M, Dhanireddy S, Harrington RD, Moore A, Golden MR. The Max Clinic: Medical Care designed to engage the hardest-to-Reach Persons living with HIV in Seattle and King County, Washington. AIDS Patient Care STDS. 2018;32(4):149–56.
Hickey MD, Imbert E, Appa A, et al. HIV Treatment Outcomes in POP-UP: Drop-in HIV Primary Care Model for People experiencing homelessness. J Infect Dis. 2022. https://doi.org/10.1093/infdis/jiac267.
Palar K, Wong MD, Cunningham WE. Competing subsistence needs are associated with retention in care and detectable viral load among people living with HIV. J HIV AIDS Soc Serv. 2018. https://doi.org/10.1080/15381501.2017.1407732.
Wong MD, Sarkisian CA, Davis C, Kinsler J, Cunningham WE. The association between life chaos, health care use, and health status among HIV-infected persons. J Gen Intern Med. 2007. https://doi.org/10.1007/s11606-007-0265-6.
Barker B, Adams E, Wood E, et al. Engagement in maximally-assisted therapy and adherence to antiretroviral therapy among a cohort of indigenous people who use illicit drugs. AIDS Behav. 2019;23:1258–66.
Dombrowski JC, Galagan SR, Ramchandani M, et al. HIV Care for patients with Complex needs: a controlled evaluation of a Walk-In, Incentivized Care Model. Open Forum Infect Dis. 2019;6(7):ofz294.
Imbert E, Hickey MD, Clemenzi-Allen A et al. Evaluation of the POP-UP programme: a multicomponent model of care for people living with HIV with homelessness or unstable housing. AIDS. 2021 Jul 1;35(8):1241–1246.
2022 Overdose Death Report. In: King County Fatal Overdose Dashboard. Seattle & King County Public Health. 2022. https://kingcounty.gov/depts/health/overdose-prevention/~/media/depts/health/medical-examiner/documents/2022-overdose-death-report.ashx.
Pyne JM, Fortney JC, Curran GM, et al. Effectiveness of collaborative care for depression in human immunodeficiency virus clinics. Arch Intern Med. 2011;171(1):23–31.
Pence BW, Gaynes BN, Adams JL, et al. The effect of antidepressant treatment on HIV and depression outcomes: results from a randomized trial. AIDS. 2015;29(15):1975–86.
Sullivan LE, Barry D, Moore BA, et al. A trial of integrated buprenorphine/naloxone and HIV clinical care. Clin Infect Dis. 2006;43(Suppl 4):184–90.
Rosecrans A, Harris R, Saxton RE, et al. Mobile low-threshold buprenorphine integrated with infectious disease services. J Subst Abuse Treat. 2022;133:108553.
Acknowledgements
The authors would like to acknowledge the Max Clinic care team and Julie Sako, who performed some chart review for this project. Research reported in this manuscript was supported by the following: the National Institute On Drug Abuse of the National Institutes of Health under Award Number 1R25DA050985; the IDSA Foundation and HIV Medicine Association (HIVMA) Grants for Emerging Researchers/Clinicians Mentorship Program (G.E.R.M.) Grant, the University of Washington Center for AIDS Research (CFAR), an National Institutes of Health funded program [P30AI027757]; and the University of Washington Behavioral Research Center for HIV, a NIMH-funded program (P30 MH123248). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Funding
This research was supported by the National Institute On Drug Abuse of the National Institutes of Health (Award Number 1R25DA050985); the IDSA Foundation and HIV Medicine Association (HIVMA) Grants for Emerging Researchers/Clinicians Mentorship Program (G.E.R.M.) Grant (to EA); the University of Washington Center for AIDS Research (CFAR), an National Institutes of Health funded program([P30AI027757); the University of Washington Behavioral Research Center for HIV, a NIMH-funded program (P30 MH123248). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
Eden E. Altwies: funding acquisition, conceptualization, chart review, data curation and analysis, writing – original draft preparation and revision. Kaitlin A. Zinsli: data curation, data analysis, writing – original draft preparation and revision. Lydia Chwastiak: conceptualization, writing – reviewing and editing. Judith I. Tsui: funding acquisition, conceptualization, writing – reviewing and editing. Elenore P. Bhatraju: conceptualization, writing – reviewing and editing. Meena S. Ramchandani: writing – reviewing and editing. Matthew R. Golden: writing – reviewing and editing. Julia C. Dombrowski: conceptualization, supervision, writing - original draft preparation and revision.
Corresponding author
Ethics declarations
Conflict of interest
Financial interests: JCD has participated in research with materials donated by Hologic, Cepheid and Mayne Pharmaceuticals. MSR is a stockholder at Gilead Sciences and Merck & Co. Non-financial interests: None.
Ethics approval and consent to participate
The University of Washington Human Subjects Division approved this research.
Consent for publication
Not applicable.
Consent to participate
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Altwies, E.E., Zinsli, K.A., Chwastiak, L. et al. Substance Use and Mental Health Comorbidities and Receipt of Specialty Care Among Patients Enrolled in a Low-Barrier HIV Clinic. AIDS Behav 27, 3952–3960 (2023). https://doi.org/10.1007/s10461-023-04110-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-023-04110-3