Abstract
To assess whether HIV-negative men who have sex with men (MSM) have realistic views of the current implications of living with HIV, we compared data of 950 tested HIV-negative and 122 never-tested MSM on anticipated consequences of an HIV-infection to the actual experiences of 438 MSM living with HIV. Data were collected with a self-reported, web-based survey conducted between May–June 2019 in the Netherlands. Results indicated that, compared to HIV-positive MSM, HIV-negative MSM significantly overestimated 95% (37/39) of items assessing HIV-related burden. Never-tested participants overestimated 85% (33/39) of items. Overestimation in never-tested MSM was modified with increasing age and having HIV-positive friends/relatives. The high level of overestimation suggests the ongoing need to correct for misperceptions, as this could help reduce stigma towards those living with HIV and diminish fear of an HIV-diagnosis. The latter might be important to improve testing uptake in older never-tested MSM with outdated views on HIV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In most high-income countries, the majority of individuals diagnosed with HIV receive antiretroviral therapy and are virally suppressed [1]. In the Netherlands, for example, 21,969 individuals had been diagnosed with HIV and were in care in 2019, of whom 93% had started antiretroviral therapy and 89% were virally suppressed [2]. Due to availability of effective therapy, the impact of living with HIV subsequently changed from a life-threatening experience to managing a chronic, treatable condition [3,4,5,6]. It has been shown, however, that despite recent developments, such as early initiation of well-tolerated antiretroviral therapy (ART) and awareness of the Undetectable = Untransmittable (U = U) message, several burdensome aspects persist among individuals living with HIV, which predominantly relate to HIV-status disclosure, stigma and sexual and social life [7].
For both HIV stigma reduction and HIV prevention strategies, it is important knowing to what extent individuals at increased risk for HIV, such as HIV-negative men who have sex with men (MSM), over- or underestimate the implications of living with HIV. Overestimating the impact of HIV might propagate stigmatization and discrimination towards those living with HIV, and might additionally result in fear of being stigmatized if becoming HIV-positive. Previous studies among MSM have linked anticipated fear of rejection or discrimination to lower uptake of HIV testing and delayed entry into health care [8, 9]. Furthermore, other studies have shown that when HIV-negative MSM underestimate or are unaware of the implications of HIV as a chronic illness, they are less motivated to get tested or engage in HIV-protective behaviors [10, 11]. This is in line with several theoretical models, including the Health Belief Model [12] and the Common-Sense Model of Self-Regulation [13], which highlight the importance of individuals’ perceptions about the seriousness and potential consequences of an illness as close determinants of relevant health-protecting behaviors.
In the Netherlands, it has been shown that 25% of MSM living with HIV experienced discrimination because of having HIV and 44% experienced rejection by new (sex) partners due to being HIV-positive [7]. Furthermore, it has been estimated that 8% of all people living with HIV in 2018 are undiagnosed and 40% of MSM diagnosed with HIV in 2016 or later had late-stage HIV-infection [14]. As these numbers indicate the need to reduce HIV stigma and increase HIV-testing among MSM, it seems important to determine whether MSM in general have realistic views of living with HIV, and if not, the reasons why. There is a lack of contemporary studies assessing whether HIV-negative MSM understand the full range of consequences that are identified today as burdensome by individuals living with HIV. Previous studies have focused on specific aspects of living with HIV, such as HIV stigma and its association with HIV testing [8, 9, 15,16,17,18]. However, these studies did not compare the anticipated beliefs of HIV negative individuals with the actual experiences of HIV-positive MSM today. The latter would be useful to correct any misperceptions from HIV negative MSM. Several reviews have reported that information-based interventions can contribute to stigma reduction and assist in a more comprehensive understanding of HIV and its impact within the broader community [19,20,21].
The objective of this study was to determine how the burden of living with HIV is perceived among HIV-negative and never-tested MSM, and to compare the anticipated burden among these men to the actual experienced burden among HIV-positive MSM. We furthermore explored socio-demographic factors in HIV-negative or never-tested MSM that were associated with not having a realistic view of the burden of living with HIV.
Methods
Study Design and Population
We conducted a cross-sectional study in which the anticipated and actual experienced consequences of living with HIV were investigated via an online, self-reported, web-based survey among individuals currently residing in the Netherlands. The development of the survey has been described elsewhere [7]. Briefly, experiences of living with HIV among MSM in the Netherlands were identified via in-depth interviews with 18 MSM diagnosed with HIV between 2014 and 2018. Findings from these interviews were used to generate 39 questionnaire items to quantify the qualitative findings with a larger sample of MSM who were either negative, positive or never tested for HIV (Supplement 1). For HIV-positive participants, questionnaire items measured the actual experiences of living with HIV. For HIV-negative participants, or those never tested for HIV, the same questionnaire items were adapted to explore anticipated consequences of living with HIV. Between April and July 2019, the survey was distributed online on gay dating sites and apps (Grindr, Planet Romeo), via the Instagram page of a young social media influencer engaged with MSM (@meijt), and via the Facebook and Instagram pages of an organization involved in sexually transmitted infections (Soa Aids Nederland).
The study was reviewed by the ethics board of the Academic Medical Centre, Amsterdam, the Netherlands and we received an exemption from further extended protocol review. Questionnaire participation was voluntary and anonymous.
Measurements
Socio-Demographics and Sexual Risk Behavior
The socio-demographic variables that were assessed consisted of gender, age, country of birth, first two numbers of participant’s postal code, highest education level, having a chronic disease other than HIV, relationship status and gender of sex partner(s). Participants were asked about their current HIV-status based on the result of their last HIV-test (i.e., HIV-positive, HIV-negative, and never-tested). PrEP use was measured among HIV-negative and never-tested MSM, in which we distinguished between current, past and never use of PrEP. As a proxy for insight into living with HIV, we asked whether participants had friends or relatives who are diagnosed with HIV. Among HIV-negative and never-tested participants, we examined sexual risk behavior in the past 6 months. Sexual risk behavior was defined as condomless anal sex (CAS) with a casual partner who was HIV-positive with a detectable HIV VL or whose HIV-status was unknown. If current PrEP use was reported, or CAS was reported within a steady relationship, with a causal partner with a self-reported HIV-negative status, or with an HIV-positive partner with an undetectable VL, sexual behavior was not considered risky.
Experienced and Anticipated Consequences of Living with HIV
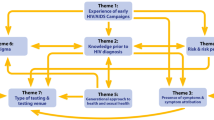
Questionnaire items were categorized into the following HIV-burden related themes: general impact, health, psychosocial, disclosure, sex and relationships, and practical consequences. The items and themes all emerged from the in-depth interviews with HIV-positive MSM [7]. All developed items were measured on a 7-point Likert scale in which 1 represented no/low burden or positive consequences and 7 high burden or negative consequences (Supplement 1). Items within themes were combined using the average Likert scale score if the Cronbach’s alpha (α) for internal consistency was ≥ 0.8.
General impact was evaluated by items on the general perceived severity of living with HIV, acceptance of being HIV-positive, and the change in quality of life due to HIV.
Health-related consequences were measured using questions on the burden of taking ART daily (4 items), ART side-effects (1 item) and hospital-visits (3 items). Additionally, three items explored perceptions on the physical consequences of HIV.
Psychosocial consequences were assessed by measuring the frequency of the following emotions or psychological states: pre-occupation with HIV, living more consciously, inferiority, loneliness, insecurity about the future, fear, sadness, unattractiveness, shame, stress, anger/frustration, relief and confidence. Furthermore, we explored changes in the bond with family/friends and fear of infecting family/friends/colleagues.
Disclosure-related consequences included questions on the level of burden when disclosing HIV status to family, friends, colleagues/work-related people, fellow students, new or existing steady partners, and new or existing casual sex partners. The level of burden when not disclosing HIV-positive status to members of social groups was measured separately. We also explored changes in disclosure-related burden over time.
Sex and relationship related consequences were assessed by asking to what extent participants agreed with the following statements (for steady partners and casual partners, separately): “Having HIV results/resulted in… (1) decreased sexual well-being; (2) decreased sexual pleasure; (3) increased fear/stress around sex; (4) more freedom in condom use; (5) a wilder sex life”. The effect of HIV on relationship quality was explored among participants who reported being in a steady relationship. In addition, the survey assessed the level of trust in the U = U message, fear of sexually transmitting HIV, difficulty in finding a sex partner, and perceived chance or actual frequency of being left by a steady partner or being rejected by a casual sex partner due to their positive HIV status.
Social and practical consequences included the frequency of being discriminated against and getting fired or not hired. We also asked whether problems were expected to be encountered with mortgage providers, the healthcare system (pharmacy, health insurance, dentist and non-HIV health care providers), and traveling.
Statistical Analysis
Socio-demographic variables were compared between HIV-positive, HIV-negative and never-tested participants using Pearson’s χ2 test for categorical variables and rank sum test for continuous variables. For items on consequences of HIV, we generated dichotomous outcomes based on anticipating (for HIV-negative or never tested participants) or experiencing (for HIV-positive participants) low versus high burden. This distinction was determined from the median of the overall study population for each outcome, separately, in which response options equal to or higher than the median represented high burden and those lower than the median represented low burden. Analyzing dichotomized items was chosen over continuous items since the outcome variables were not normally distributed. Odds ratios (OR) and their 95% confidence intervals (95%CI) were estimated using logistic regression to compare the odds of anticipating high burden among HIV-negative and never-tested MSM versus the odds of experiencing high burden among HIV-positive MSM. Models were adjusted for age, being born in the Netherlands, residing in one of the four largest cities in the Netherlands, and having a steady partner, medical comorbidity, and HIV-positive friends/relatives. Here, we define an adjusted OR (aOR) > 1 as overestimation (i.e. more likely to anticipate high burden compared to burden experienced by HIV-positive participants) and an aOR < 1 as underestimation (i.e. more likely to anticipate low burden compared to burden experienced by HIV-positive participants). Eight participants diagnosed in 2019 were excluded from the analyses, as interviews suggested that experiences during the first few months post diagnosis strongly differ from experiences thereafter [7].
Since over- and underestimation could be modified by other factors than HIV-status alone, we performed post-hoc analyses to identify specific groups with specific over- or underestimation profiles. We ran two separate models comparing HIV-negative and never-tested participants to HIV-positive participants while including (i) an interaction term with age as a continuous variable and HIV status, and (ii) an interaction term with having HIV-positive friends/relatives vs. not having HIV-positive friends/relatives (as a proxy for HIV insight) and HIV status. These models were adjusted for the demographic characteristics listed above. Differences in OR were determined by a Wald χ2 test of the interaction term. Stratum-specific estimates were directly calculated from these models using the ‘contrast’ command for the interaction term between having HIV-positive friends/relatives vs not having HIV-positive friends/relatives and HIV status. All statistical analyses were carried out using Stata IC version 15.0.
Results
A total of 2,608 individuals started the survey, of whom 1510 (58%) completed the questionnaire and were included in the analysis. Of these, 950 (63%) were HIV-negative, 438 (29%) were HIV-positive and diagnosed before 2019, and 122 (8%) were never tested for HIV. Median age of HIV-positive participants was significantly higher than that of HIV-negative and never-tested participants (Kruskal–Wallis H(2) = 89.91, p < 0.001, Table 1). HIV-positive participants more often had a medical comorbidity (Pearson χ2 (2, N = 1,510) = 18.13, p < 0.001) and HIV-positive acquaintances (Pearson χ2 (2, N = 1,510) = 119.12, p < 0.001) than HIV-negative and never-tested participants. Never-tested participants less frequently reported living in a large urban area (Pearson χ2 (2, N = 1,510) = 23.85, p < 0.001) and had a lower level of education (Pearson χ2 (2, N = 1,510) = 31.18, p < 0.001) than HIV-positive and HIV-negative participants. Sexual risk behavior in the preceding 6 months was reported by 16% (154/950) of HIV-negative and 20% (24/122) of never-tested MSM, which was not statistically different (Pearson χ2 (1, N = 1,072) = 0.94, p = 0.333). One fifth of HIV-negative MSM (20%, 191/950) reported current PrEP use compared to none of the never-tested MSM (Pearson χ2 (1, N = 1,072) = 32.97, p < 0.001). Almost all HIV-positive participants used ART (429/438, 98%) and reported an undetectable HIV viral load (VL) (430/438, 98%). Their median time since HIV diagnosis was 8 [interquartile range (IQR) = 4–13] years.
General Impact
In total, 95% (37/39) of items on the consequences of living with HIV were significantly overestimated by HIV-negative participants (Table 2). Never-tested participants overestimated 85% (33/39) of the items. HIV-negative and never-tested participants were more likely to anticipate a deterioration in quality of life (aOR = 3.16, 95%CI = 2.45–4.05; aOR = 2.28, 95%CI = 1.46–3.56; respectively) and had a higher perceived severity of living with HIV (aOR = 6.41, 95%CI = 4.94–8.33; aOR = 6.64, 95%CI = 3.88–11.36; respectively) compared to actual experiences of HIV-positive participants. In addition, they were less likely to accept having HIV (aOR = 4.08; 95%CI = 3.16–5.25; aOR = 3.85, 95%CI = 2.38–6.22; respectively) (Table 2; Supplement 2).
Health-Related Consequences
HIV-positive participants reported low burden of health-related consequences, as most reported habituation to ART-taking (338/438, 79%) and frequent hospital visits (314/438, 72%) (Supplement 2). HIV-negative and never-tested participants, however, were more likely to expect not getting used to these aspects (HIV-negative MSM: respectively, aOR = 5.60, 95%CI = 4.33–7.24; aOR = 5.33, 95%CI = 4.12–6.89; never-tested participants: respectively, aOR = 5.98, 95%CI = 3.53–10.09; aOR = 5.30, 95%CI = 3.25–8.64) (Table 2). Moreover, HIV-negative participants overestimated the burden of taking ART in presence of others (aOR = 1.90, 95%CI = 1.49–2.42). A small proportion of HIV-negative (10%, 95/950) and never-tested (12%, 15/122) participants anticipated that HIV would not change health awareness (Supplement 2), which did not differ from the actual experiences of HIV-positive participants (HIV-negative participants: aOR = 1.04, 95%CI = 0.81–1.34; never-tested participants: aOR = 0.81, 95%CI = 0.52–1.26; Table 2). The burden of ART side-effects was underestimated by both HIV-negative and never-tested participants (aOR = 0.64, 95%CI = 0.47–0.89; aOR = 0.52, 95%CI = 0.32–0.85; respectively).
Psychosocial Consequences
All psychosocial consequences of living with HIV were overestimated by HIV-negative and never-tested participants in comparison to HIV-positive participants, with the exception of the impact of HIV on the bond with family/friends among never-tested participants (aOR = 1.22, 95%CI = 0.72–2.08). 18% (80/438) of HIV-positive participants reported to often experience emotional burden from HIV, while this was anticipated by 51% (488/950) of HIV-negative (aOR = 4.43, 95%CI = 3.39–5.79) and 56% (68/122) never-tested participants (aOR = 4.08, 95%CI = 2.55–6.51). HIV-negative and never-tested participants were also more likely to expect being pre-occupied with HIV than was reported by HIV-positive participants (aOR = 7.75, 95%CI = 5.92–10.15; aOR = 9.49, 95%CI = 5.49–16.41, respectively). Fear of infecting family, friends and colleagues was anticipated by 23% (215/950) of HIV-negative participants and 24% (29/122) of never-tested participants, which was higher than the experienced fear among HIV-positive participants (8%, 36/438; aOR = 3.57, 95%CI = 2.77–4.62; aOR = 4.73, 95%CI = 2.86–7.83, respectively). HIV-negative participants more often expected HIV to negatively impact their bond with family/friends (aOR = 1.95, 95%CI = 1.46–2.61) than HIV-positive participants.
Burden of Disclosure
The burden of disclosure and non-disclosure were both overestimated among HIV-negative participants (aOR = 1.46, 95%CI = 1.14–1.86; aOR = 1.95, 95%CI = 1.52–2.52, respectively) and never-tested participants (aOR = 1.77, 95%CI = 1.11–2.84; aOR = 2.04, 95%CI = 1.30–3.22, respectively) (Table 2). However, never-tested participants expected that the difficulty of HIV-status disclosure would remain unchanged over time, which was in line with the experiences of HIV-positive participants (Supplement 2). HIV-negative MSM were, however, significantly more likely to expect that disclosure would become more difficult over time (aOR = 2.11, 95%CI = 1.62–2.75) (Supplement 2).
Sex and Relationship Related Consequences
HIV-negative and never-tested participants were more likely than HIV-positive participants to anticipate deteriorating quality of their relationship as a result of an HIV diagnosis (aOR = 4.29, 95%CI = 2.90–6.35; aOR = 2.93, 95%CI = 1.49–5.75, respectively). With regard to sex with steady partners, HIV-negative and never-tested participants more often expected a decrease in sexual pleasure (aOR = 2.85, 95%CI = 2.01–4.04; aOR = 3.01, 95%CI = 1.53–5.93, respectively) and more often anticipated fear/stress during sex (aOR = 4.47, 95%CI = 3.10–6.43; aOR = 5.55, 95%CI = 2.69–11.45). Both groups substantially overestimated the probability of being left by a steady partner (aOR = 116.02, 95%CI = 67.52–199.35; aOR = 222.25, 95%CI = 96.91–509.73, respectively) and getting rejected by a potential new partner (aOR = 25.35, 95%CI = 18.34–35.04; aOR = 43.46, 95%CI = 20.36–92.79, respectively). A high proportion of HIV-positive participants reported difficulties getting into a steady relationship due to living with HIV (41%, 85/207), which was expected to be even higher among HIV-negative and never-tested participants (aOR = 1.43, 95%CI = 1.02–2.02; aOR = 1.74, 95%CI = 1.05–2.90, respectively). Never-tested participants reported no differently than HIV-positive participants about the ease of finding new sex partners (aOR = 0.66, 95%CI = 0.42–1.03), while HIV-negative participants expected that it would be more difficult to find new sex partners compared to HIV-positive participants (aOR = 0.63, 95%CI = 0.49–0.82).
Similarly, both HIV-negative and never-tested groups overestimated the negative effect of HIV on the perceived sexual well-being (aOR = 6.12, 95%CI = 4.63–8.10; aOR = 5.98, 95%CI = 3.58–9.98, respectively), sexual pleasure (aOR = 5.71, 95%CI = 4.28–7.61; aOR = 4.64, 95%CI = 2.85–7.56, respectively) and fear/stress (aOR = 5.99, 95%CI = 4.39–8.16; aOR = 4.98, 95%CI = 2.88–8.60, respectively) when having sex with casual partners.
The majority of HIV-positive participants trusted the U = U message (71%, 309/438) and did not fear infecting sex partners (72%, 299/438) (Table 1). Compared to HIV-positive participants, HIV-negative participants and never-tested participants were significantly more likely to fear infecting sex partners (aOR = 7.88, 95%CI = 5.88–10.55; aOR = 9.37, 95%CI = 5.51–15.92, respectively) and distrust the U = U message (aOR = 3.12, 95%CI = 2.42–4.02; aOR = 6.33, 95%CI = 3.85–10.40, respectively).
Practical Consequences
Situations related to HIV-stigma, such as expecting discrimination and getting fired or not hired, were overestimated to a large extent by both HIV-negative (aOR = 41.88, 95%CI = 27.96–62.71; aOR = 177.81, 95%CI = 101.97–310.07, respectively) and never-tested participants (aOR = 30.19, 95%CI = 16.92–53.87; aOR = 256.04, 95%CI = 115.43–567.93, respectively) (Table 2). Only a small proportion of HIV-positive participants reported frequent occurrence of these situations (3%, 12/438 and < 1%, 2/438; respectively) (Supplement 2). Problems with mortgage, traveling or the health system were also reported to be rare among HIV-positive participants (9, 8, 4%; respectively) (Supplement 2), while HIV-negative participants and never-tested participants overestimated the occurrence of these events (Table 2).
Expected HIV-Related Burden and Interactions With Age and Having HIV-Positive Friends/Relatives
Among HIV-negative and never-tested participants, the degree of expected burden (i.e. aOR) of respectively 5 and 6 out of the 39 items differed according to age (Supplement 3). Items for which the degree of anticipated burden statistically increased with age among HIV-negative MSM included burden of disclosure over time (Wald χ2 (1, 1,367) = 6.28, p = 0.012), difficulty finding casual sex partners (Wald χ2 (1, N = 1,327) = 9.87, p = 0.002), and difficulty with obtaining mortgage (Wald χ2 (1, N = 1,388) = 23.90, p < 0.001). On the other hand, the degree of anticipating a decreasing quality of steady relationships (Wald χ2 (1, N = 1,181) = 3.96, p = 0.047) and distrust in the U = U message (Wald χ2 (1, N = 1,388) = 4.02, p = 0.045) decreased with age among HIV-negative participants. Among never-tested participants, the degree of anticipated burden related to emotional aspects (Wald χ2 (1, N = 560) = 7.93, p = 0.005), difficulty of disclosure over time (Wald χ2 (1, N = 539) = 10.17, p = 0.001), difficulty finding casual sex partners (Wald χ2 (1, N = 499) = 6.07, p = 0.014), getting fired or not hired (Wald χ2 (1, N = 560) = 4.89, p = 0.027), problems with the health care system (Wald χ2 (1, N = 560) = 5.83, p = 0.016) or with obtaining mortgage (Wald χ2 (1, N = 560) = 15.34, p < 0.001) all increased with age.
The expected burden differed according to having HIV-positive friends/relatives in 4/39 items among HIV-negative participants and in 11/39 items among never-tested participants (Supplement 4). Among HIV-negative participants, the anticipated burden related to difficulty of disclosure over time (Wald χ2 (1, N = 1,367) = 10.65, p = 0.001) and travel-related problems (Wald χ2 (1, N = 1,388) = 5.35, p = 0.021) were higher among those with HIV-positive relatives or close friends, but the anticipated burden related to non-disclosure (Wald χ2 (1, N = 1,337) = 4.17, p = 0.041) and getting rejected by a new sex partner (Wald χ2 (1, N = 1,388) = 9.29, p = 0.004) was higher among those without HIV-positive acquaintances. Surprisingly, among never-tested participants, having HIV-positive relatives or close friends only increased anticipated burden of certain items. For instance, it was associated with not becoming habituated to ART taking (Wald χ2 (1, N = 551) = 3.90, p = 0.048), fear for hospital visits (Wald χ2 (1, N = 560) = 4.23, p = 0.040), not becoming habituated to frequent hospital visits (Wald χ2 (1, N = 560) = 6.09, p = 0.014), general emotional burden (Wald χ2 (1, N = 560) = 6.19, p = 0.013), difficulty of disclosure over time (Wald χ2 (1, N = 539) = 5.51, p = 0.019), decreasing sexual pleasure with casual partners (Wald χ2 (1, N = 499) = 5.32, p = 0.021), increased fear/stress during sex with casual partners (Wald χ2 (1, N = 499) = 4.05, p = 0.044), fear of sexual HIV transmission (Wald χ2 (1, N = 539) = 4.38, p = 0.036), and problems with the health care system (Wald χ2 (1, N = 560) = 5.56, p = 0.018), obtaining mortgage (Wald χ2 (1, N = 560) = 4.76, p = 0.029) and traveling (Wald χ2 (1, N = 560) = 5.48, p = 0.019).
Discussion
In this study, we explored which aspects of the burden of living with HIV are misperceived by HIV-negative and never-tested MSM in comparison to HIV-positive MSM. We found that both HIV-negative and never-tested MSM largely overestimate the consequences of living with HIV as a chronic illness, although the number of overestimated items was higher among HIV-negative MSM than among never-tested MSM. However, overestimation of some items in never-tested MSM was modified with increasing age and having HIV-positive friends or relatives, whereas these distinct effects were not clearly present in HIV-negative MSM.
Our findings of overestimation fit well with the general affective forecasting literature, which is described as the process of predicting future emotion states following emotional events, such as an HIV diagnosis [22]. It has been demonstrated that there are several errors involved when people predict future feelings. The most prevalent error is impact bias, whereby people frequently overestimate the hypothetical emotional impact of negative events [22]. A major source of impact bias in response to negative events is failure to anticipate how much a person’s coping capabilities will hasten their recovery. The current study was preceded by a qualitative study in which we examined the durability of experienced burden among MSM living with HIV [7]. Results from that study showed that several aspects, such as the clinical management of infection, were initially experienced as burdensome, but were quickly habituated to. It is likely that MSM in our study did not anticipate developing such coping or habituation capabilities, resulting in a predominant overestimation of burden. The experiences of HIV-positive MSM on habituation to their new condition over time can be used in interventions to correct misperceptions on the anticipated burden of living with HIV and create more realistic views.
Correcting overestimation of burden can be useful to counteract stigmatization of individuals living with HIV. In our preceding qualitative study, we showed that approximately one-third of HIV-positive MSM experienced burden of living with HIV, which was mainly linked to interpersonal experiences, such as difficulties with disclosure [7]. Others have also shown that individuals living with HIV frequently deal with HIV-related stigma, resulting in negative affective feelings, such as guilt and depression, and social consequences, such as isolation and discrimination [23,24,25,26]. These effects might be exacerbated to a great extent by negative attitudes and fear from HIV-negative peers, as acceptance of an HIV diagnosis is highly dependent on acceptance of others [3]. Negative attitudes among MSM likely result from existing stereotypes within the MSM community, which in itself has been identified as a main factor driving HIV-related stigma [15, 27]. Several interventions were found to be successful in reducing stigma attitudes among individuals and communities using information-based approaches, but were mostly targeted towards at-risk populations [19,20,21]. Correction of stereotypic perceptions and specific misperceptions on the implications of living with HIV among MSM might therefore also be useful in stigma-reducing campaigns aiming to improve the quality of life of individuals living with HIV.
Besides driving stigmatization of individuals living with HIV, overestimating the implications of an HIV-infection might result in lower uptake of HIV-testing. This claim is substantiated by previous studies showing an association between anticipating negative consequences of HIV and less frequent testing for HIV [8, 9, 15,16,17,18]. Individuals who perceive the consequences of HIV as more burdensome than in actuality might be more afraid of a potential positive HIV test result and therefore postpone or avoid HIV-testing. This effect might be reinforced by HIV-prevention messages implicitly stating that an HIV-infection should be avoided. In our sample, more than 10% never had an HIV test, even though about a fifth of this group had engaged in activities at-risk for HIV in the past 6 months. For some younger never-tested MSM, recent HIV-testing could be less relevant as they might have been less, or only recently became, sexually active and therefore might not yet have had a substantial reason for testing. Interestingly, our data suggest that among never-tested MSM, overestimation of especially health-care and stigma-related perceptions significantly increased with age or knowing others with HIV. Overestimation from this subgroup of MSM might be the result of outdated views on health-related and interpersonal consequences of living with HIV, such as perceptions regarding the negative impact of HIV diagnosis due to experiences dating from the pre-ART period. A recent qualitative study elaborated this concept, demonstrating that the images from the AIDS epidemic during the pre-ART period still impact older MSM today and is associated with late testing and late presentation in care [28]. In addition, we expected that having HIV-positive friends/relatives would have contributed to a more realistic view of the burden of HIV, which was clearly not the case for never-tested MSM. It could be that ‘having acquaintances with HIV’ by itself is not necessarily a proxy for HIV-related insight. If knowing persons with HIV does not involve discussion and exposure to their experiences, it might actually evoke a reaction of fear, rather than acquiring realistic views of burden. Older never-tested MSM might therefore benefit from correction of misperceptions regarding the burden of living with HIV that might improve their testing uptake. Interventions using narrative evidence from those living with HIV or interventions that target affective forecasting might have a positive effect on HIV testing, as these strategies were found to be effective in changing behavior across several health domains [29, 30].
One last intriguing finding in our analysis was the underestimation of burden due to side effects of ART among our HIV-negative and never-tested participants. This finding suggests that perceptions regarding the ease of using current ART regimens have been well adopted by HIV-negative and never tested MSM. The implications of such an underestimation among HIV negative or never tested MSM need to be clarified—it could be that perceptions among some of these individuals can lower the perceived severity of HIV and could therefore form the basis for lower motivation to protect oneself from HIV or to test for HIV. In such cases, efforts to correct underestimation of HIV-related burden must be formulated in a cautious way not to lead to an opposite effect of increasing stigma and testing avoidance.
A limitation of our study was its cross-sectional nature, which limited us from establishing causal inference between overestimation and HIV testing uptake. We recruited an online, convenience sample of respondents, and half did not complete the survey. This sample might therefore not be fully representative for the overall MSM population of the Netherlands or of other countries. Generalizing our results to other settings should therefore be done with caution. Furthermore, over- or underestimation was difficult to establish whenever an item was reported by almost all HIV-positive MSM as burdensome or not burdensome, respectively (as was the case for underestimation with the item “frequency of discrimination”, for example). Furthermore, our risk definition could be limited as we had no data on the use of PrEP during every CAS act, negotiated safety within steady relationships, or information on the validity of the perceived HIV status of casual partners.
In conclusion, our study illustrated that the consequences of living with HIV as a chronic illness are predominantly overestimated among HIV-negative and never tested MSM. The overestimation of almost all items suggests ongoing need for knowledge-based campaigns that correct misperceptions on the realities of living with HIV, which may have the potential to decrease stigmatization towards those living with HIV and might additionally reduce fear of negative consequences of an HIV diagnosis. The latter could be especially relevant for older never-tested MSM to improve their testing uptake, as they may have outdated views of the consequences of living with HIV.
References
UNAIDS. Global HIV & AIDS statistics - 2019 fact sheet. Available online at: https://www.unaids.org/en/resources/fact-sheet. Accessed 21 December 2021.
Stichting HIV Monitoring the Netherlands. Annual Report 2020. Available online at www.hiv-monitoring.nl.
Flowers P, Davis MM, Larkin M, Church S, Marriott C. Understanding the impact of HIV diagnosis amongst gay men in Scotland: an interpretative phenomenological analysis. Psychol Health. 2011;26(10):1378–91.
Moskowitz JT, Wrubel J, Hult JR, Maurer S, Acree M. Illness appraisals and depression in the first year after HIV diagnosis. PLoS ONE. 2013;8(10):e78904.
Rai T, Bruton J, Day S, Ward H. From activism to secrecy: Contemporary experiences of living with HIV in London in people diagnosed from 1986 to 2014. Health Expect. 2018;21(6):1134–41.
Siegel K, Lekas HM. AIDS as a chronic illness: psychosocial implications. AIDS. 2002;16(Suppl 4):S69-76.
Van Bilsen WPH, Zimmermann HML, Boyd A, Davidovich U. Burden of living with HIV among men who have sex with men: a mixed-methods study. Lancet HIV. 2020;7(12):e835–84. https://doi.org/10.1016/S2352-3018(20)30197-1.
Gamarel KE, Nelson KM, Stephenson R, Santiago Rivera OJ, Chiaramonte D, Miller RL, et al. Anticipated HIV stigma and delays in regular HIV testing behaviors among sexually-active young gay, bisexual, and other men who have sex with men and transgender women. AIDS Behav. 2018;22(2):522–30.
Golub SA, Gamarel KE. The impact of anticipated HIV stigma on delays in HIV testing behaviors: findings from a community-based sample of men who have sex with men and transgender women in New York City. AIDS Patient Care STDS. 2013;27(11):621–7.
Fuster-RuizdeApodaca MJ, Laguia A, Molero F, Toledo J, Arrillaga A, Jaen A. Psychosocial determinants of HIV testing across stages of change in Spanish population: a cross-sectional national survey. BMC Public Health. 2017;17(1):234.
Schnall R, Rojas M, Travers J. Understanding HIV testing behaviors of minority adolescents: a health behavior model analysis. J Assoc Nurses AIDS Care. 2015;26(3):246–58.
Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Q. 1988;15(2):175–83.
Leventhal H, Nerenz D, Steele DJ. Illness representations and coping with health threats handbook of psychology and health. 4th ed. Hillsdale: Lawrence Erlbaum Associates; 1984. p. 219–52.
van Sighem AI, Wit FWNM, Boyd A, Smit C, Matser A, Reiss PM, Report, . Human Immunodeficiency Virus (HIV) Infection in the Netherlands. Amsterdam: Stichting HIV Monitoring; 2019. p. 2019.
Earnshaw VA, Smith LR, Chaudoir SR, Lee IC, Copenhaver MM. Stereotypes about people living with HIV: implications for perceptions of HIV risk and testing frequency among at-risk populations. AIDS Educ Prev. 2012;24(6):574–81.
Kalichman SC, Simbayi LC. HIV testing attitudes, AIDS stigma, and voluntary HIV counselling and testing in a black township in Cape Town. South Africa Sex Transm Infect. 2003;79(6):442–7.
Li X, Lu H, Ma X, Sun Y, He X, Li C, et al. HIV/AIDS-related stigmatizing and discriminatory attitudes and recent HIV testing among men who have sex with men in Beijing. AIDS Behav. 2012;16(3):499–507.
Herek GM, Mitnick L, Burris S, Chesney M, Devine P, Fullilove MT, et al. Workshop report: AIDS and stigma: a conceptual framework and research agenda. AIDS Public Policy J. 1998;13(1):36–47.
Andersson GZ, Reinius M, Eriksson LE, Svedhem V, Esfahani FM, Deuba K, et al. Stigma reduction interventions in people living with HIV to improve health-related quality of life. Lancet HIV. 2020;7(2):e129–40.
Mahajan AP, Sayles JN, Patel VA, Remien RH, Sawires SR, Ortiz DJ, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS. 2008;22(Suppl 2):S67-79.
Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? J Int AIDS Soc. 2013;16(3 Suppl 2):18734.
Wilson TD, Gilbert DT. Affective Forecasting. Adv Exp. Soc Psychol. 2003;35:345–411.
Nachega JB, Lehman DA, Hlatshwayo D, Mothopeng R, Chaisson RE, Karstaedt AS. HIV/AIDS and antiretroviral treatment knowledge, attitudes, beliefs, and practices in HIV-infected adults in Soweto, South Africa. J Acquir Immune Defic Syndr. 2005;38(2):196–201.
Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc Sci Med. 2003;57(1):13–24.
Wolfe WR, Weiser SD, Bangsberg DR, Thior I, Makhema JM, Dickinson DB, et al. Effects of HIV-related stigma among an early sample of patients receiving antiretroviral therapy in Botswana. AIDS Care. 2006;18(8):931–3.
Logie C, Gadalla TM. Meta-analysis of health and demographic correlates of stigma towards people living with HIV. AIDS Care. 2009;21(6):742–53.
Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13(6):1160–77.
Bedert M. Reasons for late presentation among older MSM in Amsterdam. 12th Netherlands Conference on HIV Pathogenesis, Epidemiology, Prevention and Treatment (NCHIV) Amsterdam 2019.
Ellis EM, Elwyn G, Nelson WL, Scalia P, Kobrin SC, Ferrer RA. Interventions to engage affective forecasting in health-related decision making: a meta-analysis. Ann Behav Med. 2018;52(2):157–74.
de Wit JB, Das E, Vet R. What works best: objective statistics or a personal testimonial? An assessment of the persuasive effects of different types of message evidence on risk perception. Health Psychol. 2008;27(1):110–5.
Acknowledgements
We thank all our participants for filling out the online survey. We further like to thank the following persons for their invaluable support to this study: Wim Zuilhof, Arjan van Bijnen, Tomas Derckx, Renee Finkenflügel, Ertan Ersan, Dominique Loomans, and Fred Verdult. Furthermore, we thank all of those who contributed to the H-TEAM (see Supplement 5).
Funding
This study was funded by the HIV Transmission Elimination Amsterdam Initiative (H-TEAM).
Author information
Authors and Affiliations
Author notes
On behalf of HIV Transmission Elimination Amsterdam Initiative (H-TEAM)
- Udi Davidovich
Consortia
Contributions
HZ, WvB and UD contributed to study concept and design. HZ and WvB performed all data analyses. AB and UD supervised the data analysis. HZ and WvB wrote the first draft of the report. All authors contributed to interpretation of the data and critically revised the manuscript and approved the final version for publication.
Corresponding author
Ethics declarations
Conflict of interest
A.B. reports grants from ANRS and grants from Sidaction, outside the submitted work. UD reports obtaining unrestricted research grants and speaker’s fees from Gilead Sciences, paid to his institute (Public Health Service of Amsterdam). All other authors declare no competing interests.
Ethics Approval
The study was reviewed by the ethics board of the Academic Medical Centre, Amsterdam, the Netherlands and we received an exemption from further extended protocol review. Questionnaire participation was voluntary and anonymous.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zimmermann, H.M.L., van Bilsen, W.P.H., Boyd, A. et al. The Burden of Living With HIV is Mostly Overestimated by HIV-Negative and Never-Tested Men Who Have Sex With Men. AIDS Behav 25, 3804–3813 (2021). https://doi.org/10.1007/s10461-021-03281-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-021-03281-1