Abstract
Seroadaptive behaviors help reduce HIV risk for some men who have sex with men (MSM), and have been well documented across MSM populations. Advancements in biomedical prevention have changed the contexts in which seroadaptive behaviors occur. We thus sought to estimate and compare the prevalence of four stages of the “seroadaptive cascade” by PrEP use in the recent era: knowledge of own serostatus, knowledge of partner serostatus; serosorting (matching by status), and condomless anal intercourse. Serosorting overall appeared to remain common, especially with casual and one-time partners. Although PrEP use did not impact status discussion, it did impact serosorting and the likelihood of having condomless anal intercourse. For respondents not diagnosed with HIV and not on PrEP, condomless anal intercourse occurred in just over half of relationships with HIV-positive partners who were not on treatment. Biomedical prevention has intertwined with rather than supplanted seroadaptive behaviors, while contexts involving neither persist.
Resumen
Los comportamientos seroadaptivos ayudan a reducir el riesgo de VIH en algunos hombres que tienen sexo con otros hombres (HSH) y han sido bien documentados en varias comunidades de HSH. Los avances en prevención biomédica han cambiado los contextos de los comportamientos seroadaptivos. Por ello buscamos estimar y comparar la prevalencia de cuatro fases de la ‘cascada seroadaptiva’ mediante el uso de PrEP en la era reciente: conocimiento del seroestatus personal, conocimiento del seroestatus del compañero, serosorting (emparejamiento por estatus) y coito anal sin condón. En general, el serosorting parece seguir siendo común especialmente con parejas casuales o de una noche. A pesar de que el uso de PrEP no impactó la discusión sobre el estatus, sí impactó el serosorting y la probabilidad de coito anal sin condón. Los encuestados no diagnosticados con VIH y sin PrEP tuvieron coito anal sin condón en la mitad de las relaciones con parejas VIH-positivo que no estaban bajo tratamiento. La prevención biomédica se ha entremezclado en lugar de suplantar los comportamientos seropositivos, mientras persisten los contextos en los que no aparece ninguno.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
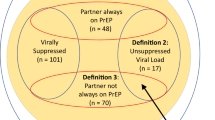
Seroadaptive behaviors represent a longstanding HIV risk reduction strategy practiced by men who have sex with men (MSM) [1,2,3,4,5,6,7,8,9,10,11,12,13]. While selection of sexual partners by serostatus (“serosorting”) is most commonly discussed, seroadaptive behaviors include multiple other types of serostatus-based decisions, e.g. selection of sexual acts (e.g. oral vs. anal), selection of sexual role (“seropositioning”, i.e. insertive vs receptive), and decisions around condom use. Akin to HIV care, these can be framed as a “seroadaptive cascade” (Fig. 1). While seroadaptive behaviors alone are clearly an imperfect strategy for preventing HIV acquisition [14,15,16], some MSM are more successful in adhering to them than to condom use [17], the latter of which has long been on the decline among MSM overall [18, 19]. Two meta-analyses [20, 21] found that men practicing serosorting have lower HIV incidence than those who practice condomless anal intercourse (CLAI) without regard to partner status. This confirms that serosorting, and perhaps other seroadaptive behaviors, play an important role towards HIV harm reduction among MSM. Of course, the effectiveness of seroadaptive behaviors depends on the extent to which men are aware of their status, which requires frequent testing for those not yet diagnosed with HIV. It also depends on accurate and up-to-date sharing of status between prospective and ongoing partners, whether through direct discussion or through other means such as dating and meetup app profiles. Seroadaptive behaviors are typically thought of as a dyadic process (i.e. two people share their status, and decide whether and how to have sex based on the combined information), although it is possible for there to be asymmetry, particularly in the app profile context (i.e. for one person to share status and the other to base individual decisions on this, but not vice versa).
A seroadaptive cascade framework. This provides a schematic of the major elements of seroadaptive behaviors, including the precursor of testing. Steps refer to the components of the analysis in the paper, and do not imply that all of these must occur or, if they do occur, will do so in this exact order. For example, men do not need to know their serostatus to share information (i.e. one can share the fact that one has never tested for HIV), and the decision to have sex can occur without any serostatus discussion at all. In practice, components may also be iterative rather than discretely ordered; for example, a man may change his mind and decide not to have sex if he and a prospective partner cannot agree about sexual type or condom use
Recent developments in biomedical HIV prevention have fundamentally changed the prevention landscape, and thus the contexts shaping the adoption of seroadaptive behaviors. Both pre-exposure prophylaxis (PrEP) and treatment as prevention (TasP, known commonly as “undetectable = untransmittable”, or “U = U”) work to prevent the spread of HIV through the actions of a single individual. That is, a man taking PrEP as recommended might presume that he has high, consistent protection from HIV acquisition, regardless of his partner’s status. A similar situation holds for a man with HIV who is adherent to ART and has exhibited durable HIV viral load suppression, with respect to transmission. This may lead to men in either group deciding that they need not engage in explicit discussion of HIV status, nor adapt behavior based on perceived status concordance or discordance. We might thus imagine that these biomedical tools have influenced seroadaptive behaviors for these men, and possibly even for men who are HIV-negative and not on PrEP as well through broader changes in safer-sex norms. PrEP has a direct effect on testing, as the latter is a requirement for initiating or continuing on PrEP; whether or how men not on PrEP have adjusted their testing in the age of biomedical prevention is less clear. Subsequent steps of seroadaptation appear to have declined overall as PrEP has expanded in San Francisco [22], and subsequent analyses that compared men on PrEP to those off have found some evidence for lower levels of seroadaptive behaviors among the former [23, 24].
In practice, not all men on PrEP or ART maintain perfect adherence [25,26,27] or full self-awareness of their adherence level [28, 29], and cases of acquisition by those adherent to PrEP, although rare, do exist [30]. Since individuals may vary in their conceptualizations of risk and the confidence they place in any individual strategy, some proportion may continue to engage in seroadaptive behaviors in conjunction with biomedical strategies. These types of decisions likely play out differently by type of relationships (e.g. main, casual, or one-time) [13], given differences in level of trust around accurate disclosure [31, 32], or in trade-offs between prevention and intimacy [33, 34]. Given all of the considerations, detailed assessments of current seroadaptive behaviors for MSM across serostatuses or biomedical prevention engagement in multiple settings can provide insight about the current contexts for continued potential HIV transmissions.
Measuring seroadaptive behaviors is complicated by multiple factors. For one, observed behavioral patterns may emerge from other causes besides explicit intentionality [17, 35,36,37]. For instance, a preponderance of seroconcordant partners could stem from assortative mixing not on serostatus but on attributes that correlate with it, such as age and race/ethnicity; however, some of the effects on epidemiology may be similar regardless of the actual drivers of partner selection. Another issue is endogenous transmission—i.e. that partners match in HIV status not because of selection but because initially serodiscordant relationships transition to seroconcordant-positive via transmission within the relationship. Finally, knowledge of both self and partner serostatus is generally imperfect and time-varying (until someone is diagnosed with HIV and discloses this). Nevertheless, when considering how knowledge of status impacts behavior, that knowledge itself is a relevant measure, regardless of whether it matches true serostatus.
In this paper, we measure the state of seroadaptive behaviors among MSM during the era of PrEP and U = U. We interrogate four steps in the seroadaptive cascade: HIV testing, disclosure, partner selection, and sexual act/condom use selection. We focus in particular on comparing negative men who are on PrEP with those who are not on PrEP, hypothesizing that the former will show less seroadaptation at each step of the cascade after testing. We predict that overall seroadaptation rates will vary by relationship types (being strongest for one-time partners), but that differences between men on and not on PrEP will persist across types. A secondary hypothesis is that men on PrEP will exhibit a probability of CLAI that is lower than that seen within concordant HIV-positive dyads, reflecting the idea that some men on PrEP are still developing a sense of trust in its effectiveness. (Both groups need to contend with the potential transmission of other sexually transmitted infections). Finally, we predict that men who report not knowing their own HIV status at all will exhibit the lowest levels of seroadaptation, reflecting a low level of engagement with HIV prevention overall. By considering each stage and the relational types in which they occur, we aim for our work to provide the evidence needed to parametrize further quantitative analyses, such as mathematical modeling or the development of individual or relational risk scores, that can help to assess and thus intervene upon the contexts in which probable transmission events continue to occur in the biomedical prevention era.
Methods
We used data from the ARTnet study, a web-based sexual network survey of United States MSM conducted in conjunction with the American Men’s Internet Survey (AMIS) in 2017 and 2018. Detailed methods are published for both ARTnet [38] and AMIS [39,40,41,42]. AMIS was in its fifth and sixth cycles in 2017 and 2018, respectively. Recruitment occurred through banner ads on websites and social network applications popular with MSM. Although AMIS is primarily a repeat cross-sectional survey, participants from the prior year who consented to be recontacted were recruited as well. However, in recent years these only comprise about 10% of the next year’s final sample [40, 42]). AMIS eligibility criteria include age ≥ 15 years old, United States residence with valid ZIP code, cisgender male identity, and reporting ever having sex with a man or (for those under 18) identifying as gay or bisexual. Sample sizes were 10,049 and 10,129 for these two rounds, respectively, and included men from every state plus DC and Puerto Rico. Participants were asked extensive questions on demographics; HIV status; sexual behavior; history of HIV testing, prevention and treatment usage; alcohol and drug use; and sexually transmitted infection (STI) histories.
Respondents who completed AMIS were immediately requested to participate in ARTnet, which included additional questions on sexual networks and behaviors with male partners. Additional eligibility criteria for ARTnet included ages 65 or less, and any lifetime sexual activity with another man. Participants did not have to complete ARTnet immediately, but were given periodic reminders to do so; as a result, some questions from AMIS were repeated to ensure up-to-date information. Of those eligible, 53% opted to enroll in ARTnet; the population enrolling had slightly higher representation of White non-Hispanic men than AMIS overall (71.8% vs 69.2%, respectively), but was also less biased towards younger participants [38]. The final ARTnet dataset combines both years of data collection; participants who appeared twice had only their second survey included to ensure each entry represented a unique person.
Most of our outcomes of interest used relationships as the unit of analysis. Respondents were asked summary questions about their relationship history and detailed questions about their most recent male partners (up to 5) within the last year. Relationships were categorized into three types: main (“someone that you feel committed to above all others, someone you might call your boyfriend, significant other, life partner or husband”), casual (anyone else a respondent had had sex with more than once); and one-time.
Respondents were categorized by self-reported knowledge of HIV status: HIV-positive (those who had ever had a positive HIV test); HIV-negative (those who had tested but never with a positive result); and HIV-unknown (those who had never tested, never received their results, or reported not knowing their results). Partners were similarly categorized by respondent’s reported knowledge of their serostatus; here, HIV-unknown included cases where respondent said their partner had never been tested, their partner did not know his status, or that they did not know their partner’s status.
Respondent’s PrEP use was categorized on a per-partnership basis, i.e. whether they were taking PrEP during none, some, or all of the relationship. For behaviors by PrEP use, we compared cases with PrEP use during all or none of the relationship, since with partial PrEP use we cannot tell which behaviors occurred during the period with and without PrEP. To determine the impact of this decision, we repeated the relevant analysis as any PrEP versus no PrEP during the relationship (see online Supplement). Partner PrEP and ART use were measured similarly, with our analyses also comparing use during all or none of the relationship.
We considered four steps of the seroadaptive cascade (Fig. 1): knowledge of own status (Step 1), knowledge of partner’s status (Step 2), serosorting (Step 3), and selection of sexual acts (CLAI vs others; Step 4). We did not address seropositioning, as previous work found that this was much less common than other seroadaptive behaviors using either behavioral or intentionality definitions, and also had low consistency between those definitions [36].
At all cascade steps, we present our results in terms of the prevalence of each examined behavior by sub-group. We provide frequencies and proportions directly as potential sources for parameterizing mathematical models, and disaggregate these by respondent and partner serostatus, relational type and respondent PrEP status and partner ART status as relevant and feasible given sample sizes. This satisfies one of our goals: to provide a rich set of parameters for those modeling bio-behavioral prevention strategies among MSM in the presence of both PrEP and viral suppression. For HIV testing, we compare across ages given that lifetime history of ever testing should vary greatly on this dimension. To test hypotheses on later steps in the cascade, we calculate relative risks (RR) as relevant, and use exact binomial tests to calculate 95% confidence intervals and Fisher’s exact tests to compare estimates across groups. We use exact tests given that some cell entries are small, and the tests are tractable in all cases, providing a consistent method even for those cases where cells are larger. We use one-sided tests for 2 × 2 comparisons in which our hypothesis predicts a specific direction to the effect, and two-sided tests otherwise. Based on the hypothesis of interest, we test across relational types, respondent and/or partner serostatus, respondent PrEP use and partner ART use, as relevant. Analyses were conducted in R 4.0.2; all code is available at https://github.com/EpiModel/Seroadaptivity_ARTnet.
Results
Our inclusion criteria from the broader ARTnet study yielded 4512 respondents, reporting on 13,800 relationships, or 3.1 relationships per respondent. These were slightly reduced relative to previous published analyses, since we excluded 392 respondents not asked about PrEP use early in the first wave. Table 1 lists descriptive statistics for the samples of both respondents and relationships. Our online convenience sample reported higher education than the adult US population as a whole, perhaps unsurprisingly. The age distribution spanned the full range, being slightly bimodal with a dip among 35–44-year-olds. Black respondents were under-represented relative to the adult US population. Overall, 9.5% of respondents reported being diagnosed with HIV. One-time contacts represented just over half of reported relationships; main and casual relationships, with their longer durations, still reflected most of the relationship time and sexual acts. There were large numbers of relationships in which the respondent reported being HIV-negative and on PrEP (n = 2239) or HIV-negative and not on PrEP (n = 7937) throughout the relationship. However, the relationships reported by men diagnosed with HIV mostly comprised cases where they were on ART throughout (n = 1126) with very few cases of no ART use (n = 69). We thus did not disaggregate any analyses of behaviors of HIV-positive respondents by own suppression status.
Step 1: testing Figure 2 shows multiple measures for respondents’ awareness of their own status. The proportion of respondents who reported ever having an HIV test rose rapidly from less than one in five in the mid-teens to near-universality around age 30, at which point it asymptoted with strong consistency across ages. Including all ages, the proportion with a test ever was 84.0%, but including only respondents 25 + raises this to 92.9%, or for 30 + to 94.4%.
Measures of respondents’ knowledge of their own HIV status, by age. From top to bottom, metrics reflect the proportion at each age who report ever having had an HIV test; the proportion who have had an HIV test in the last 2 years, out of those who have not previously been diagnosed positive and are not on PrEP; and the proportion who have ever tested positive for HIV. Testing in the last two years for men on PrEP is not shown, as it is effectively universal. Dots reflect the mean value for respondents of a given age. Lines represent loess curves with α = 0.5, as implemented with the loess command in R v. 4.0.2
For recent testing, it becomes important to disaggregate men into three types. One is those who are already diagnosed HIV-positive, since they no longer need to test; this sub-group rose steadily with age until about 50, above which 19.9% of respondents reported having an HIV diagnosis. The second is men who are on PrEP, since they are required to test frequently. Indeed, 99.2% (611 of 616) of men currently on PrEP said they had been tested in the last 2 years; we thus do not disaggregate these by age. Third is men who have never tested positive and are not on PrEP. Testing in the last two years for these men followed the same pattern as lifetime testing at young ages—when nearly all testing would be recent. The overall shape suggests three rough phases in testing across the lifecourse for MSM who remain HIV-negative and are not on PrEP, with transition points in the late 20 s and around age 50. Collectively, these findings emphasize that, in subsequent analyses, respondents of “unknown” status largely reflect younger MSM, while those of positive status disproportionately reflect older men.
Step 2: disclosure Figure 3a depicts the proportion of partners for whom the respondent claims knowledge of their partner’s serostatus, regardless of what that status was. Results are divided by respondent serostatus, PrEP status for negative respondents, and relational type. Overall, respondents reported knowing partner status in 68.3% of relationships. As hypothesized, the likelihood of knowing a partner’s status declined with less committed relationship types, regardless of respondents’ serostatus or PrEP status (Fisher’s exact test, p = 1.59 × 10–171 for HIV-negative respondents not on PrEP; p = 2.37 × 10–61 for HIV-negative respondents on PrEP; 1.72 × 10–37 for HIV-positive respondents; and p = 3.53 × 10–8 for HIV-unknown respondents). In contrast, we did not find evidence for our main hypothesis that negative men on PrEP would report lower status communication than negative men not on PrEP for a given relational type (one-tailed Fisher’s exact test, p = 0.89 for main partners; p = 1.00 for casual partners; p = 0.97 for one-time partners). Redoing this comparison between relationships during which the respondent was never on PrEP versus ever (as opposed to always) on PrEP yielded qualitatively similar findings (Figure S1). Finally, men who did not know their own HIV status reported the least knowledge of partner status overall, as predicted; however, we note that even these men reported knowing their one-time partners’ status fully half of the time.
Partner status, by respondent HIV status and relationship type: a Proportion of partners whose HIV status respondents report knowing; b Proportion of partners who respondents report as HIV-positive, among partners of known status. CIs = binomial proportion confidence intervals, selected due to the binary outcome and the small sample sizes in some categories. Relationship types are defined in the text. Note the difference in scale on the y-axis to make visible the differences by relational type in b
Step 3: serosorting The largest distinction in partner serostatus (conditional on it being known) was the considerably higher proportion of HIV-positive partners for HIV-positive respondents over aall other respondents for all partner types (Fig. 3b), consistent with substantial serosorting. As predicted, HIV-negative men on PrEP reported a higher proportion of known HIV-positive partners than did negative men not on PrEP (RR = 2.7 overall, 95% CI 2.2–3.4, Fisher exact test p = 1.0 × 10–17). This association between respondent PrEP status and partner HIV status was particularly strong for main partners, with a RR of 4.2 (95% CI 2.7–6.7, Fisher exact test p = 5.2 × 10–8). Those who reported not knowing their HIV status had responses most similar to HIV-negative men not on PrEP, in contrast to our hypothesis. Again, reanalysis to include PrEP use at any point in the relationship did not change the qualitative results (Fig. S1).
Step 4: act type and condom use Here we focused on disaggregating by partner status rather than partner type, as the former is fundamental to the transmission potential associated with each behavior (Fig. 4). Consistent with our main hypothesis, HIV-negative respondents on PrEP had higher proportions of relationships with any CLAI than did HIV-negative respondents not on PrEP, for all partner serostatuses (one-tailed Fisher’s exact test, p = 3.2 × 10–18 for HIV-negative partners, 3.1 × 10–07 for HIV-positive, and 1.1 × 10–36 for HIV-status-unknown). Indeed, the numbers for respondents on PrEP were similar to those of HIV-positive men (p = 0.39, 0.52, and 0.30 for the same three partner serostatuses, respectively). As with the prior step, responses for unknown-status respondents were most similar to those for HIV-negative men not on PrEP.
Sexual acts and condom use within relationships, by respondent HIV status and PrEP use and partner HIV status. Relationships are categorized by act with highest transmission probability, i.e. a relationship listed as “anal, always w/condom” may also contain oral sex acts, while “any anal without condom” may also contain anal sex with condom and/or oral sex. Pneg = partner HIV-negative; Ppos = partner HIV-positive; Punk = partner HIV status unknown. Bar charts are stacked for easy visual comparison; numbers within sections refer to the proportion in that section
We note a consistent trend that we did not predict; for all types of respondents, regardless of status or PrEP use, CLAI was most likely to occur with known HIV-positive partners. Of course, the implications for this differ for HIV-positive versus HIV-negative men on or off PrEP. More than half of the relationships between HIV-negative respondents not on PrEP and their HIV-positive partners involved some CLAI, and the same was true for serostatus-unknown respondents. Since these types of relationships may entail the greatest transmission opportunity, we further disaggregated them by the respondent’s report of their HIV-positive partner’s use of ART. For HIV-negative respondents not on PrEP, the probability of having CLAI with a given HIV-positive partner on ART was 56.5% (95% exact binomial CI 47.0%–65.7%); for an HIV-positive partner off ART, it was 53.1% (95% exact binomial CI 38.3%–67.5%). These figures were not significantly different (one-tailed Fisher’s exact test, p = 0.72).
Discussion
In this study, we investigated four steps of the seroadaptive cascade in the era of biomedical prevention, comparing behaviors variously by serostatus knowledge, biomedical prevention use, and partnership type. We found that PrEP use does not have a discernible impact on status discussion, but does impact partner selection and the likelihood of having condomless anal intercourse. All groups of respondents were most likely to have CLAI with partners diagnosed with HIV, especially with main or casual partners. For respondents not diagnosed with HIV and not on PrEP, CLAI occurred in just over half of relationships with partners who were not on treatment. The probability that these respondents would have CLAI with one of their partners of unknown status was lower, but such partners were also much more common (n = 2283, or 17.5% of all relationships). This suggests the persistence of sexual activity within known serodiscordant relationships in which men are aware of the absence of any form of prevention of HIV transmission, either biomedical or behavioral, as well as within many relationships where this absence is a reasonable possibility. Both types represent key areas where identification and intervention continue to be needed, and could have substantial impact.
Our primary finding is broadly consistent with two recent studies that also disaggregated disclosure and partner status by respondent PrEP use. In an analysis that combined national and New York City samples, Grov et al. [23] found that HIV-negative men on PrEP had a higher proportion of positive casual partners than those off PrEP did (roughly 17% and 11% of their partners of known status, estimated from numbers in their Table 3). Wang et al. [24] found similar numbers (17.1% vs 9.3% of all partners with known status, respectively) in a Montreal-based sample. While the pattern of less serosorting by men on PrEP was consistent across all studies, our numbers suggest overall higher serosorting by HIV-negative men than these previous studies did (8.7% and 3.1% known positive partners for men on or off PrEP in this study when averaged across partnership types, or 7.9% and 2.9% when excluding main partnerships for comparability to Grov et al.) Our sample is younger and more White than the US/NYC study, and more geographically diverse and less urban than the Montreal study, all of which may make HIV prevalence in the partner pool of our respondents lower overall.
Because the previous studies did not disaggregate by relationship type, we cannot compare our findings to them in this regard. Our observation that men on PrEP have high rates of main partners known to be diagnosed with HIV (15.8%) relative to other partner types undoubtedly reflects at least some reverse causality—i.e. an HIV-negative man with a main partner living with HIV is indicated for PrEP if they have anal sex, and would have high motivation to take it. For one-time partners, the number is smaller (6.1%) and more similar to but still significantly above that of HIV-negative men off PrEP (2.6%). All of these numbers are far below the comparable numbers for respondents diagnosed with HIV, or indeed the proportion of MSM diagnosed with HIV in the US population [43]. Whether they reflect explicit serosorting by men on PrEP or partner selection on other attributes that correlate with status, the pattern does present evidence for a sexual network that remains fairly segregated between men who are or are not diagnosed with HIV, even as biomedical prevention has been touted as an option to allow individual MSM to more comfortably “bridge the serodivide” [44].
In contrast to our findings, these same two studies found that men with recent PrEP use were significantly more likely to know their partner’s status than HIV-negative men without recent PrEP use (83% versus 74% for Grov et al.; 69.4% versus 50.5% for Wang et al.) Our comparable numbers, averaging across partner types included by each study, were 71.1% and 66.0% (for Grov et al.) and 74.0% and 70.4% (for Wang et al.) These trended in the same direction but were closer and not significantly different from each other. Regardless, all three studies agree that men on PrEP are not generally considering the protection it affords as a reason to engage in less serodiscussion. While we confirmed the expected trend by relational type, we also found that men on PrEP were more likely than not (60.3%) to report knowing even their one-time partners’ HIV status. While one might imagine that knowledge of a main partner’s serostatus would reflect overall intimacy and not solely concern for HIV transmission risk, this should be less true for casual and most especially one-time partners. The high rates of reported status knowledge by men on PrEP here may reflect multiple phenomena: (1) a continued desire by men on PrEP to assess their HIV risk, perhaps because of concern about their own adherence or other PrEP failures; (2) disclosure in the form of app profiles, which would occur automatically and without need for explicit discussion [45]; and (3) the mutuality of HIV status disclosure, such that men on PrEP are sharing and receiving HIV and biomedical status information for their partner’s benefit [46]. The first of these includes cases where men on PrEP are not only seeking partners who are HIV-negative, but who themselves are on PrEP, to provide yet another layer of protection (“PrEP-sorting”); while we did not investigate this pattern here, both Grov et al. and Wang et al. found evidence for this phenomenon. Evidence for the second and third possibilities may come from our observation that men who report not knowing their own status still reported knowing their one-time partners’ status more than half the time. It also highlights the possibility that some men report their status as negative to potential partners as long as they have never had an HIV-positive test result—even if they have never tested or tested very long ago [47].
We found that the first precursor for seroadaptation—having an HIV test—remains common, as one might expect given that accessing new biomedical prevention modalities still requires HIV screening, and the continued emphasis on testing by public health campaigns targeted at MSM. For MSM aged 25–49 who have not been diagnosed with HIV and are not on PrEP, testing in the last 2 years is very high; for men on PrEP it is of course essentially universal. However, those below age 25 show considerable room for improvements in testing, with only 58.8% aged 15–24 (regardless of status or PrEP use) testing in the last 2 years, or 63.7% of those 18–24. (These numbers change only slightly when limiting to those not on PrEP and never diagnosed, to 56.1% and 61.3%). The proportion for 18–24-year-olds is well below the 78.8% in the same age range who had tested in the last 12 months in the most recent NHBS results [43], despite the latter testing time window being shorter. This may reflect differences in web-based versus venue sampling, and requires further investigation.
We found that men on PrEP were just as likely to have CLAI with their partners diagnosed with HIV (83.2%) as were respondents who themselves were diagnosed with HIV (83.6%). Since men on PrEP appeared to exhibit some level of seroadaptivity in terms of partner selection, we might then also anticipate that they would do so in terms of act selection and condom use; the high probability here and its similarity to the rate for respondents diagnosed with HIV suggests this does not appear to be the case.
Respondents of all serostatus and biomedical prevention status reported that CLAI was most likely with their partners who had diagnosed HIV. This finding for HIV-negative respondents implies that something other than simple seroadaptive behaviors is occurring. One likely explanation is selectivity—where those with the strongest propensity for CLAI acquire HIV at disproportionate rates and continue that propensity with their partners, including HIV-negative ones. Nevertheless, it is notable that this apparent effect is strong enough to reverse any tendency for selective use of condoms by HIV-negative men not on PrEP with their partners diagnosed with HIV.
Elements of the seroadaptive cascade undoubtedly vary by numerous key sociodemographic predictors (race/ethnicity, age, income, education, geography), and some of these differences may help to contribute to persistent disparities in HIV incidence and prevalence [48,49,50,51,52]. We did not look at these predictors here (except for age in the context of testing) given the complexities already introduced by our focus on multiple steps in the seroadaptive cascade and our exploration of respondents’ PrEP status and on relational type as key determinants of them. With a clearer understanding of how PrEP users do (and in some cases do not) differ from non-PrEP users in their seroadaptive behaviors, we now plan follow-up work that will consider the prevalence of behaviors with the greatest HIV transmission potential (e.g. HIV negative men not on PrEP having CLAI with unknown HIV-status partners) by sociodemographic attributes, and determine predictors for these behaviors separately within different racial/ethnic communities.
Limitations
Our study relies on a convenience sample, as do all national surveys of MSM to some extent. Non-Hispanic White men were over-represented, relative to the adult US male population, as were younger men and those with a college degree. Nevertheless, a previous analysis of this data set found that, after accounting for unknown responses, HIV prevalence in the sample was in line with national estimates [38], and our median age matched that in the previous similar studies to which we compared our results [23, 24]. All questions were self-reported, and could not be tested for reliability. It remains challenging to know how different respondents may interpret questions such as knowledge of partners’ status—e.g., where some may assume a one-time partner’s HIV-negative disclosure as truth while others report it as unknown. Again, however, it is presumably respondents’ own perception of partner’s status that most directly influences potential seroadaptive behavior. Answers to our questions were not necessarily the same way respondents would describe their status to a partner, especially for those whose last negative test was long ago. As with most serosorting studies, we do not have information on partnerships that did not occur specifically because of serodiscordance. Source studies did not ask about type of PrEP (e.g. daily vs. on demand), although the latter is not included in CDC guidelines and appears to have been uncommon at the time of this study [53], with efforts to promote its use only taking off as this study was completing [54]. Our inclusion of multiple hypothesis tests increases the overall Type 1 error rate and may yield false positives; we note, however, that all significant differences had p-values orders of magnitude below our significance level, and would thus hold up under a multiple comparison correction.
Conclusions
This study provides substantial new information on the recent magnitude of testing, disclosure, serosorting, sexual act selection, and use of condoms among US MSM, and in particular how men on PrEP and those not differ in these behaviors. Our future work will incorporate this information into mechanistic transmission models, along with measures of imperfect adherence to PrEP and ART, to obtain estimates of the attributable fraction of transmissions among MSM occurring in different contexts, i.e. by relationship type and by the biomedical prevention methods used by the men in these relationships. Such work would be relevant for HIV as well as for other major reportable STIs (e.g., syphilis), which circulate on the same sexual network as HIV. With more than 25,000 new HIV diagnoses among US MSM each year still, such models are critical to identify the conditions where prevention efforts—biomedical and behavioral—remain insufficient, as we work towards the goal of ending the HIV epidemic.
References
Cairns G. New directions in HIV prevention: serosorting and universal testing. IAPAC Mon. 2006;12(2):42–5.
Cassels S, Menza TW, Goodreau SM, Golden MR. HIV serosorting as a harm reduction strategy: evidence from Seattle, Washington. AIDS. 2009;23(18):2497–506.
Chen YH, Snowden JM, McFarland W, Raymond HF. Pre-exposure prophylaxis (PrEP) use, seroadaptation, and sexual behavior among men who have sex with men, San Francisco, 2004–2014. AIDS Behav. 2016;20(12):2791–7.
Grov C, Rendina HJ, Moody RL, Ventuneac A, Parsons JT. HIV serosorting, status disclosure, and strategic positioning among highly sexually active gay and bisexual men. AIDS Pat Care STDS. 2015;29(10):559–68.
Halkitis PN, Moeller RW, Pollock JA. Sexual practices of gay, bisexual, and other nonidentified MSM attending New York City gyms: patterns of serosorting, strategic positioning, and context selection. J Sex Res. 2008;45(3):253–61.
Khosropour CM, Dombrowski JC, Swanson F, et al. Trends in serosorting and the association With HIV/STI risk over time among men who have sex with men. J Acquir Immune Defic Syndr. 2016;72(2):189–97.
Kurtz SP, Buttram ME, Surratt HL, Stall RD. Resilience, syndemic factors, and serosorting behaviors among HIV-positive and HIV-negative substance-using MSM. AIDS Educ Prev. 2012;24(3):193–205.
LeVasseur MT, Goldstein ND, Tabb LP, Olivieri-Mui BL, Welles SL. The effect of PrEP on HIV incidence among men who have sex with men in the context of condom use, treatment as prevention, and seroadaptive practices. J Acquir Immune Defic Syndr. 2018;77(1):31–40.
McFarland W, Chen YH, Raymond HF, et al. HIV seroadaptation among individuals, within sexual dyads, and by sexual episodes, men who have sex with men, San Francisco, 2008. AIDS Care. 2011;23(3):261–8.
Parsons JT, Schrimshaw EW, Wolitski RJ, et al. Sexual harm reduction practices of HIV-seropositive gay and bisexual men: serosorting, strategic positioning, and withdrawal before ejaculation. AIDS. 2005;19(Suppl 1):S13-25.
Ronn M, White PJ, Hughes G, Ward H. Developing a conceptual framework of seroadaptive behaviors in HIV-diagnosed men who have sex with men. J Infect Dis. 2014;210:S586-593.
Vallabhaneni S, Li X, Vittinghoff E, Donnell D, Pilcher CD, Buchbinder SP. Seroadaptive practices: association with HIV acquisition among HIV-negative men who have sex with men. PLoS ONE. 2012;7(10):e45718.
van den Boom W, Stolte I, Sandfort T, Davidovich U. Serosorting and sexual risk behaviour according to different casual partnership types among MSM: the study of one-night stands and sex buddies. AIDS Care. 2012;24(2):167–73.
Eaton LA, Kalichman SC, Cain DN, et al. Serosorting sexual partners and risk for HIV among men who have sex with men. Am J Prev Med. 2007;33(6):479–85.
Golden MR, Stekler J, Hughes JP, Wood RW. HIV serosorting in men who have sex with men: is it safe? J Acquir Immune Defic Syndr. 2008;49(2):212–8.
Zablotska IB, Imrie J, Prestage G, et al. Gay men’s current practice of HIV seroconcordant unprotected anal intercourse: serosorting or seroguessing? AIDS Care. 2009;21(4):501–10.
McFarland W, Chen YH, Nguyen B, et al. Behavior, intention or chance? A longitudinal study of HIV seroadaptive behaviors, abstinence and condom use. AIDS Behav. 2012;16(1):121–31.
Paz-Bailey G, Mendoza MC, Finlayson T, et al. Trends in condom use among MSM in the United States: the role of antiretroviral therapy and seroadaptive strategies. AIDS. 2016;30(12):1985–90.
Sanchez TH, Zlotorzynska M, Sineath RC, Kahle E, Tregear S, Sullivan PS. National trends in sexual behavior, substance use and HIV testing among United States men who have sex with men recruited online, 2013 through 2017. AIDS Behav. 2018;22(8):2413–25.
Kennedy CE, Bernard LJ, Muessig KE, et al. Serosorting and HIV/STI infection among HIV-negative MSM and transgender people: a systematic review and meta-analysis to inform WHO Guidelines. J Sex Trans Dis. 2013;2013:583627.
Purcell DW, Higa D, Mizuno Y, Lyles C. Quantifying the harms and benefits from serosorting among HIV-negative gay and bisexual men: a systematic review and meta-analysis. AIDS Behav. 2017;21(10):2835–43.
Chen YH, Guigayoma J, McFarland W, Snowden JM, Raymond HF. Increases in pre-exposure prophylaxis use and decreases in condom use: behavioral patterns among HIV-negative San Francisco men who have sex with men, 2004–2017. AIDS Behav. 2019;23(7):1841–5.
Grov C, Jonathan Rendina H, Patel VV, Kelvin E, Anastos K, Parsons JT. Prevalence of and factors associated with the use of HIV serosorting and other biomedical prevention strategies among men who have sex with men in a US Nationwide Survey. AIDS Behav. 2018;22(8):2743–55.
Wang L, Moqueet N, Lambert G, et al. Population-level sexual mixing according to HIV status and preexposure prophylaxis use among men who have sex with men in Montreal, Canada: implications for HIV prevention. Am J Epidemiol. 2020;189(1):44–54.
Liu AY, Cohen SE, Vittinghoff E, et al. Preexposure prophylaxis for HIV infection integrated with municipal- and community-based sexual health services. JAMA Intern Med. 2016;176(1):75–84.
Kelley CF, Kahle E, Siegler A, et al. Applying a PrEP continuum of care for men who have sex with men in Atlanta, Georgia. Clin Infect Dis. 2015;61(10):1590–7.
Maxwell S, Gafos M, Shahmanesh M. Pre-exposure prophylaxis use and medication adherence among men who have sex with men: a systematic review of the literature. J Assoc Nurs AIDS Care. 2019;30(4):e38–61.
Mustanski B, Ryan DT, Remble TA, D’Aquila RT, Newcomb ME, Morgan E. Discordance of self-report and laboratory measures of HIV viral load among young men who have sex with men and transgender women in chicago: implications for epidemiology, care, and prevention. AIDS Behav. 2018;22(7):2360–7.
Stephenson R, Bratcher A, Mimiaga MJ, et al. Brief report: accuracy in self-report of viral suppression among HIV-positive men with HIV-negative male partners. J Acquir Immune Defic Syndr. 2020;83(3):210–4.
To KW, Lee SS. A review of reported cases of HIV pre-exposure prophylaxis failure with resultant breakthrough HIV infections. HIV Med. 2020;22:75–82.
Hoff C. Negotiated safety agreements: do they protect and how they protect. Focus. 2005;20(2):1–5.
Hoff CC, Beougher SC. Sexual agreements among gay male couples. Arch Sex Behav. 2010;39(3):774–87.
Starks TJ, Payton G, Golub SA, Weinberger CL, Parsons JT. Contextualizing condom use: intimacy interference, stigma, and unprotected sex. J Health Psychol. 2014;19(6):711–20.
Golub SA, Starks TJ, Payton G, Parsons JT. The critical role of intimacy in the sexual risk behaviors of gay and bisexual men. AIDS Behav. 2012;16(3):626–32.
Cassels S, Katz DA. Seroadaptation among men who have sex with men: emerging research themes. Curr HIV/AIDS Rep. 2013;10(4):305–13.
Khosropour CM, Dombrowski JC, Hughes JP, Manhart LE, Simoni JM, Golden MR. Operationalizing the measurement of seroadaptive behaviors: a comparison of reported sexual behaviors and purposely-adopted behaviors among men who have sex with men (MSM) in Seattle. AIDS Behav. 2017;21(10):2935–44.
Siegler AJ, Sullivan PS, Khosropour CM, Rosenberg ES. The role of intent in serosorting behaviors among men who have sex with men sexual partnerships. J Acquir Immune Defic Syndr. 2013;64(3):307–14.
Weiss KM, Goodreau SM, Morris M, et al. Egocentric sexual networks of men who have sex with men in the United States: results from the ARTnet study. Epidemics. 2020;30:100386.
Sanchez TH, Sineath RC, Kahle EM, Tregear SJ, Sullivan PS. The Annual American Men’s Internet Survey of behaviors of men who have sex with men in the United States: protocol and key indicators Report 2013. JMIR Publ Health Surveill. 2015;1(1):e3.
Zlotorzynska M, Cantu C, Rai R, Sullivan P, Sanchez T. The annual American Men’s Internet Survey of behaviors of men who have sex with men in the United States: 2017 Key Indicators Report. JMIR Public Health Surveill. 2020;6(2):e16847.
Zlotorzynska M, Sullivan P, Sanchez T. The Annual American Men’s Internet Survey of Behaviors of men who have sex with men in the United States: 2015 key indicators report. JMIR Publ Health Surveill. 2017;3(1):e13.
Zlotorzynska M, Sullivan P, Sanchez T. The annual American Men’s Internet Survey of Behaviors of men who have sex with men in the United States: 2016 key indicators report. JMIR Public Health Surveill. 2019;5(1):e11313.
Centers for Disease Control and Prevention. HIV Infection Risk, Prevention, and Testing Behaviors Among Men Who Have Sex With Men—National HIV Behavioral Surveillance, 23 U.S. Cities, 2017. HIV Surveillance Special Report 22. https://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published February 2019. Accessed Sep 21, 2020
Koester KA, Erguera XA, Kang Dufour MS, et al. “Losing the Phobia:” understanding how HIV pre-exposure prophylaxis facilitates bridging the serodivide among men who have sex with men. Front Public Health. 2018;6:250.
Medina MM, Crowley C, Montgomery MC, et al. Disclosure of HIV serostatus and pre-exposure prophylaxis use on internet hookup sites among men who have sex with men. AIDS Behav. 2019;23(7):1681–8.
Holt M, Rawstorne P, Worth H, Bittman M, Wilkinson J, Kippax S. Predictors of HIV disclosure among untested, HIV-negative and HIV-positive Australian men who had anal intercourse with their most recent casual male sex partner. AIDS Behav. 2011;15(6):1128–39.
Grov C, Rendina HJ, Parsons JT. How different are men who do not know their HIV status from those who do? Results from an US online study of gay and bisexual men. AIDS Behav. 2016;20(9):1989–99.
Crosby RA, Mena L, Geter A. Favourable attitudes towards serosorting are associated with overall less frequent condom use among young Black men having sex men. Sex Health. 2016;13(1):91–2.
Marks G, Millett GA, Bingham T, Lauby J, Murrill CS, Stueve A. Prevalence and protective value of serosorting and strategic positioning among Black and Latino men who have sex with men. Sex Transm Dis. 2010;37(5):325–7.
Wilton L, Koblin B, Nandi V, et al. Correlates of seroadaptation strategies among black men who have sex with men (MSM) in 4 US cities. AIDS Behav. 2015;19(12):2333–46.
Golden MR, Dombrowski JC, Kerani RP, Stekler JD. Failure of serosorting to protect African American men who have sex with men from HIV infection. Sex Transm Dis. 2012;39(9):659–64.
Goodreau SM, Rosenberg ES, Jenness SM, et al. Sources of racial disparities in HIV prevalence in men who have sex with men in Atlanta, GA, USA: a modelling study. Lancet HIV. 2017;4(7):e311–20.
Sewell WC, Powell VE, Mayer KH, Ochoa A, Krakower DS, Marcus JL. Nondaily use of HIV preexposure prophylaxis in a large online survey of primarily men who have sex with men in the United States. J Acquir Immune Defic Syndr. 2020;84(2):182–8.
Hojilla JC, Marcus JL, Silverberg MJ, et al. Early adopters of event-driven human immunodeficiency virus pre-exposure prophylaxis in a large healthcare system in San Francisco. Clin Infect Dis. 2020;71:2710–2.
Acknowledgements
The authors would like to thank the study participants, the full AMIS and ARTnet research teams, and the Network Modeling Group at the University of Washington. Special thanks to Ana Dobao and Marcos Llobera.
Funding
This work was supported by National Institutes of Health Grant Nos. R21 MH112449 and R01 AI138783. Partial support for this research came from a Eunice Kennedy Shriver National Institute of Child Health and Human Development research infrastructure Grant, P2C HD042828, to the Center for Studies in Demography and Ecology at the University of Washington.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethical approval
This study was approved by the Emory University Institutional Review Board. It was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Goodreau, S.M., Maloney, K.M., Sanchez, T.H. et al. A Behavioral Cascade of HIV Seroadaptation Among US Men Who Have Sex with Men in the Era of PrEP and U = U. AIDS Behav 25, 3933–3943 (2021). https://doi.org/10.1007/s10461-021-03266-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-021-03266-0