Abstract
To improve outcomes among HIV-positive adolescents, the Malawi Ministry of Health is supporting scale-up of “Teen Clubs,” a facility-based antiretroviral treatment (ART) delivery model. Teen Clubs are monthly ART clinics for adolescents (10–19 years old) that provide clinical services and peer psychosocial support. This paper assesses ART adherence among Teen Club attendees in Malawi. We performed a retrospective analysis of medical records and Teen Club attendance data on 589 HIV-positive adolescents at 16 Partners in Hope (PIH)—Extending Quality Improvement for HIV/AIDS in Malawi (EQUIP) supported facilities across Malawi, from January to June of 2017, who attended at least two Teen Club sessions. Multi-level logistic regression models were used to examine the role of gender and age on optimal ART adherence (≥ 95% based on pill count) among HIV-positive adolescents enrolled in Teen Clubs. The median age of adolescents in this sample was 14 years, and 47% were male. Older adolescent males (15–19 years) were 64% more likely to achieve ≥ 95% ART adherence (aOR 1.64, 95% CI 1.16–2.31, p < 0.01) compared to younger (10–14 years) males. The effect of age on adherence was smaller and not significant among females (aOR 1.36, 95% CI 0.96–1.94, p = 0.08). In the full model including males and females, older adolescence was associated with higher odds of optimal adherence (aOR 1.48, 95% CI 1.16–1.90, p < 0.01). These results reinforce the need for age-specialized programming for adolescents, and future research should evaluate this in achieving optimal ART adherence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malawi is making progress toward the UNAIDS 90-90-90 targets, but significant challenges remain, particularly for HIV-positive adolescents who experience higher rates of virologic failure compared to adults [1]. Adolescents in Malawi represent a growing share of the population living with HIV, and account for nearly 50% of new HIV infections [2]. Older female adolescents (aged 15–19) are particularly vulnerable to poor HIV-related outcomes [3], and may face additional adherence-related social and economic barriers compared to their male counterparts [4, 5].
Several studies have examined factors influencing antiretroviral therapy (ART) adherence among older HIV-positive adults, however research evaluating barriers to adherence among adolescents has been understudied. Additionally, of the few studies that have examined adherence among adolescents, there is conflicting evidence on the association between gender and adherence. While some studies have reported no association [6, 7], others have shown males are more likely to achieve optimal adherence compared to females [8, 9]. There is an urgent need for research on factors that influence adherence among HIV-positive adolescents, and age- and gender-related differences in achieving optimal adherence [10].
To address barriers to adherence and improve overall health outcomes among HIV-positive adolescents, the Ministry of Health in Malawi has supported the scale-up of a facility-based ART delivery model known as “Teen Clubs.” Teen clubs are monthly ART clinics exclusively for HIV-positive adolescents, 10–19 years old, that provide clinical services and peer psychosocial support. Adherence counseling sessions are provided if there is a concern for poor adherence and virologic failure. Partners in Hope (PIH)—Extending Quality Improvements for HIV/AIDS in Malawi (EQUIP) is a PEFPAR-USAID funded HIV care and treatment program that has supported the implementation and expansion of the Teen Club program in Malawi since 2015.
The purpose of this study was to examine the role of gender and age on optimal ART adherence among Teen Club participants in Malawi. Understanding characteristics associated with adherence in this population can inform the design of targeted interventions and identify gaps for program improvement among HIV-positive adolescents.
Methods
Site and Subject Selection
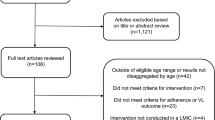
We reviewed medical records and Teen Club attendance data from 16 PIH-EQUIP supported facilities across five districts in Malawi. Adolescents were eligible for inclusion if they were aged 10–19 years and attended at least 2 monthly Teen Club sessions from January 2017 through June 2017 (n = 589). Two or more monthly Teen Club visits was considered a good reflection of attendance and appropriate for evaluating ART adherence among enrolled adolescents given the limited 6-month study period.
Data Elements
Data were extracted on study participants’ gender, age, ART regimen type (non-nucleoside reverse transcriptase inhibitor (NNRTI) or protease inhibitor (PI-based), number of Teen Club sessions attended, and ART adherence. Teen Club attendance was determined by assessment of registers containing monthly visit dates at a Teen Club facility. Monthly attendance is included as a continuous measure, ranging from 2 to 6 visits through the 6-month study period. ART adherence was based on a pill count by a clinical provider at a documented visit during the study period, either during a monthly Teen Club session or ART clinic visit; and adherence was classified as optimal (≥ 95%) or suboptimal (< 95%) [11].
Statistical Analyses
Descriptive statistics were performed to summarize demographic variables, ART regimen, Teen Club attendance, and adherence among 589 HIV-positive adolescents. Gender stratified multi-level logistic regression models were used to evaluate characteristics associated with optimal ART adherence. Each multi-level analysis included repeated adherence measures (Level 1), individuals (Level 2) and facilities (Level 3). Potential interaction effects were identified by deriving separate regression models for males and females; significant factors were tested as interaction terms with gender in a model that included both sexes. All analyses were conducted using Stata v14 software (StataCorp 2015). The study protocol was approved by the Institutional Review Board at the University of California, Los Angeles and the National Health Sciences Research Committee in Malawi.
Results
Approximately half of study participants were male (47%). No significant gender differences were found for age, ART regimen, or Teen Club attendance (Table 1). Among study participants, mean ART adherence was 86%, and optimal adherence (≥ 95%) was achieved at least once during the study period by 62%. Approximately 35% of participants achieved optimal adherence at all Teen Club visits.
In fully adjusted models, males aged 15–19 years were 64% more likely to achieve ART adherence (aOR 1.64, 95% CI 1.16–2.31, p < 0.01) compared to younger males (10–14 years) (Table 2). The association between age and adherence was smaller in magnitude and non-significant among females (aOR = 1.36, 95% CI 0.96–1.94, p = 0.08). More frequent attendance at Teen Club was not a significant predictor of adherence among female participants (aOR 1.09 95% CI 0.94–1.27, p = 0.23) or male participants (aOR 0.88, 95% CI 0.76–1.02, p = 0.11).
The association between age and adherence in the combined multi-level model is consistent with estimates from the gender-stratified models (Table 3). In fully adjusted models with both sexes, adolescents 15–19 years old were 48% more likely to achieve adherence, compared to adolescents 10–14 years old (1.48, 95% CI 1.16–1.90, p < 0.01). Females were 14% more likely to achieve optimal adherence, compared to males, however this effect was not significant in the combined model (aOR 1.14, 95% CI 0.91–1.43, p = 0.25). The interaction term between age and gender on adherence was also non-significant (aOR 0.98, 95% CI 0.61–1.55, p = 0.91).
Discussion
In our sample of HIV-positive adolescents attending Teen Clubs in Malawi, older adolescents were more likely to achieve optimal adherence than younger adolescents—particularly older males, who were 64% more likely to achieve optimal adherence compared to younger males. There was a similar trend for female adolescents that was smaller in magnitude and did not reach statistical significance. The finding that Teen Club has a greater impact on adherence among older adolescents suggests that age-specialized programming may be helpful in improving outcomes among younger populations.
Study results are consistent with previous studies from Southern Africa that found higher rates of nonadherence among younger teens and adolescents [12, 13]. Although we did not find a statistically significant association between age and adherence among females, this may be due to the small sample size, which limited statistical power for multi-level analyses.
An unexpected finding was that sustained attendance at monthly Teen Club sessions was not a significant predictor of ART adherence among our study population. These results may indicate that any exposure to Teen Club, regardless of the number of monthly sessions, may facilitate adherence and improve overall outcomes, as these clinics serve as a resource for health education and psychosocial support [14]. ART adherence over the 6-month study period was also higher on average compared to previous studies evaluating adherence among adolescent populations—thus, even a small ‘dose’ of Teen Club programming appears to have a strong response on the outcome of adherence [1, 6].
Results from the gender-stratified analysis showed that higher monthly attendance at Teen Club was positively associated with increased odds of ART adherence among females; however, among males, increased attendance was associated with worse adherence. Although these findings were non-significant, the disparity in the gender-stratified models may reflect potential differences in gender-based behaviors and responses to Teen Club adherence counseling and education. Research has shown that gender-responsive HIV programming can be effective in promoting adherence and overall outcomes, as these programs are tailored to address gender-specific barriers to ART adherence [15]. For example, females may face additional competing priorities that can influence ART adherence, including the stress of domestic and caregiving responsibilities, and other structural barriers, such as gender-based violence [16, 17]. Further research is needed to better understand the mechanisms by which exposure to Teen Club influences adherence, and whether the factors and processes that facilitate adherence in HIV-positive adolescents may be different for males than for females and younger versus older participants.
There are additional limitations to consider in this study. First, due to data restrictions, we were unable to control for other potential confounding factors, such as duration on ART or in the Teen Club program. We also did not have information on viral load as a measure of adherence. At the time data were collected for this study, up-to-date viral load measurements were relatively unavailable for adolescents and adults in Malawi. Pill counts are considered an appropriate method to assess medication adherence, and have been found to be a reliable measure of adherence in resource-limited settings [18, 19]. Selection bias may exist based on adolescents who chose to enroll and attend Teen Club over the 6-month study period, compared to non-enrolled adolescents; this bias may be reflected in the high level of adherence reported in this study. Additionally, these findings may not generalize to other populations or settings; in particular, those who participate in Teen Club are required to know and have disclosed their HIV status, so they may be systematically different from other adolescents for whom disclosure has not occurred.
Conclusion
We found that HIV-positive adolescents aged 15–19 years who were enrolled in Teen Club in Malawi were more likely to achieve optimal adherence compared to younger Teen Club participants (aged 10–14 years), and this finding was particularly robust for males. Future research should evaluate age-specific adolescent programming as strategies for achieving optimal adherence. Future studies should also consider use of viral load measures for evaluating factors associated with adherence in this vulnerable population.
References
Kim S-H, Gerver SM, Fidler S, Ward H. Adherence to antiretroviral therapy in adolescents living with HIV: systematic review and meta-analysis. AIDS. 2014;28(13):1945–56.
Kiprono Ruttoh S, Tobias M, Kipngeno Ruttoh B. The status of human immuno-deficiency virus (HIV) infection among youth aged 15–24 years in Malawi and Kenya. 2017.
Dellar RC, Dlamini S, Karim QA. Adolescent girls and young women: key populations for HIV epidemic control. J Int AIDS Soc. 2015;18:19408.
Harrison A, Colvin CJ, Kuo C, Swartz A, Lurie M. Sustained high HIV incidence in young women in Southern Africa: social, behavioral, and structural factors and emerging intervention approaches. Curr HIV/AIDS Rep. 2015;12(2):207–15.
Holstad MM, Spangler S, Higgins M, Dalmida SG, Sharma S. Psychosocial characteristics associated with both antiretroviral therapy adherence and risk behaviors in women living with HIV. AIDS Behav. 2016;20(5):1084–96.
Kim MH, Mazenga AC, Yu X, Ahmed S, Paul ME, Kazembe PN, et al. High self-reported non-adherence to antiretroviral therapy amongst adolescents living with HIV in Malawi: barriers and associated factors. J. Int. AIDS Soc. 2017;20(1):21437.
Fonsah JY, Njamnshi AK, Kouanfack C, Qiu F, Njamnshi DM, Tagny CT, et al. Adherence to antiretroviral therapy (ART) in yaounde-cameroon: association with opportunistic infections, depression, ART regimen and side effects. PLoS ONE. 2017;12(1):e0170893.
de Fatima Bonolo P, Ceccato MdGB, Rocha GM, de Assis Acúrcio F, Campos LN, Guimarães MDC. Gender differences in non-adherence among Brazilian patients initiating antiretroviral therapy. Clinics. 2013;68(5):612–20.
Lopez EJ, Jones DL, Villar-Loubet OM, Arheart KL, Weiss SM. Violence, coping, and consistent medication adherence in hiv-positive couples. AIDS Educ Prev. 2010;22(1):61–8.
Lall P, Lim SH, Khairuddin N, Kamarulzaman A. Review: An urgent need for research on factors impacting adherence to and retention in care among HIV-positive youth and adolescents from key populations. J Int AIDS Soc. 2015;18(2Suppl 1):19393.
Malawi Ministry of Health and Population. Clinical management of HIV in children and adults. Malawi: Malawi Ministry of Health and Population; 2018.
Mukui IN, Ng’ang’a L, Williamson J, Wamicwe JN, Vakil S, Katana A, et al. Rates and predictors of non-adherence to antiretroviral therapy among HIV-positive individuals in kenya: results from the second Kenya AIDS indicator survey, 2012. PLOS ONE. 2016;11(12):e0167465.
Nachega JB, Hislop M, Nguyen H, Dowdy DW, Chaisson RE, Regensberg L, et al. Antiretroviral therapy adherence, virologic and immunologic outcomes in adolescents compared with adults in southern Africa. J Acquir Immune Defic Syndr. 2009;51(1):65.
MacKenzie RK, van Lettow M, Gondwe C, Nyirongo J, Singano V, Banda V, et al. Greater retention in care among adolescents on antiretroviral treatment accessing “Teen Club” an adolescent-centred differentiated care model compared with standard of care: a nested case-control study at a tertiary referral hospital in Malawi. J Int AIDS Soc. 2017;20(3):e25028.
Remme M, Siapka M, Vassall A, Heise L, Jacobi J, Ahumada C, et al. The cost and cost-effectiveness of gender-responsive interventions for HIV: a systematic review. J Int AIDS Soc. 2014;17(1):19228.
Kahamba J, Massawe F, Nombo C, Jeckoniah J. How gender affects adherence to antiretroviral therapy in Tanzania. Morogoro: Sokoine University of Agriculture; 2017.
Maskew M, Fox MP, Evans D, Govindasamy D, Jamieson L, Malete G, et al. Insights into adherence among a cohort of adolescents aged 12–20 years in South Africa: reported barriers to antiretroviral treatment. AIDS Res Treat. 2016;2016:4161738.
Oyugi JH, Byakika-Tusiime J, Charlebois ED, Kityo C, Mugerwa R, Mugyenyi P, et al. Multiple validated measures of adherence indicate high levels of adherence to generic HIV antiretroviral therapy in a resource-limited setting. JAIDS J Acquir Immune Defic Syndr. 2004;36(5):1100–2.
Lee JK, Grace KA, Foster TG, Crawley MJ, Erowele GI, Sun HJ, et al. How should we measure medication adherence in clinical trials and practice? Ther Clin Risk Manag. 2007;3(4):685–90.
Acknowledgements
We wish to thank the clinical and administrative staff at Partners in Hope-EQUIP for their support of Teen Clubs and their assistance with this evaluation project.
Funding
Funding was funded by U.S. Agency for International Development (USAID) and the President’s Emergency Plan for AIDS Relief (PEPFAR) (Grant No. AID-OAA-A-15-00070).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
McBride, K., Parent, J., Mmanga, K. et al. ART Adherence Among Malawian Youth Enrolled in Teen Clubs: A Retrospective Chart Review. AIDS Behav 23, 2629–2633 (2019). https://doi.org/10.1007/s10461-019-02580-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-019-02580-y