Abstract
The Centers for Disease Control and Prevention recommends annual HIV tests for men who have sex with men (MSM), yet some have never tested. We analyzed data from the MSM Testing Initiative. Of 68,185 HIV tests, 8% were with MSM who never previously tested (“first-time testers”). Among tests with first-time testers, 70.7% were with MSM from racial or ethnic minorities; 66.5% were with MSM younger than 30 years. Tests with MSM who reported female partners only during the past year (compared to male partners only) or were recruited for at-home testing (compared to venue-based recruitment) were 4 times (prevalence ratio [PR] 3.62, 95% CI 3.15–4.15) and 5 times as likely (PR 4.69, 95% CI 4.22–5.21) to be associated with first-time testing. At-home testing and focusing on MSM who have sex with women may be effective methods for reaching MSM who are first-time testers.
Resumen
Los Centros para el Control y la Prevención de Enfermedades (CDC) recomiendan que hombres que tienen sexo con hombres (HSH) se hagan la prueba del VIH una vez al año, sin embargo, algunos nunca se la han hecho. Analizamos los datos de la iniciativa para promover la prueba del VIH entre HSH. De las 68,185 pruebas de VIH hechas, 8% fueron en HSH que nunca antes se habían hecho la prueba del VIH. De las pruebas del VIH hechas a HSH que se hicieron la prueba por primera vez, el 70,7% pertenecían a HSH de minorías raciales o étnicas; 66.5% eran HSH menores de 30 años. Las pruebas de VIH que fueron hechas a HSH que reportaron tener exclusivamente parejas sexuales femeninas durante los últimos 12 meses (comparado con pruebas hechas a hombres con parejas sexuales masculinas) o que fueron pruebas del VIH hechas en casa (comparado con pruebas hechas en hombres reclutados en lugares públicos) tienen 4 veces (razón de prevalencia [PR, por sus siglas en inglés] = 3.62, con un intervalo de coeficiencia (IC) del 95%: 3.15 – 4.15) y 5 veces (PR = 4.69, IC del 95%: 4.22 – 5.21) más probabilidad de haber sido la primera prueba de VIH hecha en estos hombres. Hacerse la prueba del VIH en casa y centrarse en los HSH que tienen relaciones sexuales con mujeres, pueden ser métodos eficaces para alcanzar a aquellos que nunca se han hecho la prueba del VIH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Men who have sex with men (MSM) continue to be disproportionately affected by HIV. Compared to heterosexuals and persons who inject drugs, MSM have the highest lifetime risk for HIV diagnosis (1 in 6) and continue to account for the majority of new diagnoses [1, 2]. During 2016, among adults and adolescents in the United States, 70% of newly diagnosed HIV infections were attributable to male-to-male sexual contact or male-to-male sexual contact and injection drug use [2]. At the end of 2015, 17% of the 632,300 MSM living with HIV infection were estimated to be undiagnosed and therefore had a greater likelihood of transmitting HIV to sexual or injection partners [3, 4]. HIV testing is a key component in the Centers for Disease Control and Prevention (CDC) approach toward increasing awareness of HIV status among MSM and ultimately reducing the number of undiagnosed HIV infections in the United States.
Despite the CDC recommendation for MSM to test annually for HIV, some have never tested [5, 6]. Numerous studies have reported the prevalence of never testing among MSM, with results that vary widely depending upon the sampling and recruitment methodology that was used [7,8,9,10,11,12,13,14]. Data from the National Survey of Family Growth, a nationally representative sample of persons aged 15–44 years, indicate that during 2011–2015, 29% of MSM reported never testing [7]. Pooled, multi-jurisdiction data for 2014 and 2015 from the Behavioral Risk Factor Surveillance System (BRFSS) yielded similar results, indicating that 34% of MSM had never tested [8]. Data from the CDC’s National HIV Behavioral Surveillance system, which recruits respondents from venues frequented by MSM in urban areas with high HIV prevalence or diagnosis rates, indicate that during 2014, 6% of MSM reported never previously testing for HIV [9]. According to a meta-analysis of studies published during 2005 through 2013 that examined HIV testing among internet-using MSM, an average of 15% of MSM had never tested [10]. Recent publications on results from national web-based surveys have found similar percentages (16% to 17%) for never testing among MSM [11,12,13].
Sociodemographic and other factors have been associated with never testing for HIV. Data from national phone or web-based surveys have shown differences by age group, with younger MSM having the highest percentages of never testing [8,9,10,11,12, 14]. A study involving national data from the Youth Risk Behavior Surveillance System (YRBS) and BRFSS indicated a high prevalence of never testing among both sexually active high school students (average percentage from YRBS, 2005–2013 = 78%) and young adults aged 18–24 years (average percentage from BRFSS, 2011–2013 = 67%) [15]. Data from phone, computer-assisted, or web-based surveys have identified other factors such as bisexual or heterosexual identity, lower prevalence of reported HIV risk behaviors (e.g., lower number of sexual partners, never injecting drugs), low perceived HIV risk, and fear of learning about being infected with HIV as self-reported reasons for not testing [14, 16,17,18].
For this study, we analyzed data from a large-scale HIV testing initiative to describe the characteristics of MSM who were recruited for the project and to explore factors that may be associated with never previously testing for HIV among MSM. Findings may help to inform HIV prevention and testing programs and assist with efforts to reach previously untested MSM.
Methods
MTI Project
The CDC funded Abt Associates to implement the project “Scaling Up HIV Testing among African American and Hispanic Men Who Have Sex with Other Men: The MSM Testing Initiative (MTI)” as programmatic activities. The primary goals of this project were to identify at least 3000 MSM with previously undiagnosed HIV infection, at least 50% of whom were black/African American or Hispanic or Latino and to link at least 85% of all newly diagnosed MSM to HIV-related medical care. We defined MSM as persons who were assigned a male sex at birth and had reported lifetime oral or anal sex with a male. MSM were eligible for the MTI project if they had not been previously diagnosed with HIV. Staff of 36 organizations (academic research centers, community-based organizations, AIDS service organizations, and clinical organizations) located in 25 cities in the United States performed HIV testing in clinical and non-clinical settings. Non-clinical settings included HIV testing facilities, community settings (e.g., bars, clubs, or adult entertainment venues), public areas (e.g., parks), and large-scale venue-based testing events for MSM (e.g., circuit parties, house balls, or gay pride events).
The MTI recruitment strategies have been described elsewhere and included venue-based testing (VBT), at-home testing, couples voluntary counseling and testing (CVCT), large-scale testing events (testing events across America, or TEAA), and social network strategy (SNS) [19,20,21,22]. For at-home testing, MSM who were recruited via the internet from a social media or music streaming website or following the completion of a web-based survey on sexual behaviors received a free specimen collection kit.
Data Collection
Staff used a standardized form to collect data on HIV testing encounters with MSM, including information on self-reported date of birth, assigned sex at birth, current gender identity, ethnicity, race, previous HIV test, HIV status, sexual risk behaviors during the past 12 months, and methods used for recruitment and HIV testing. For sexual risk behaviors during the past 12 months, staff also collected information on condom use and if known, the gender (male, female, or transgender), use of injection drugs, needle-sharing, and HIV status for sex partners.
HIV Testing
During 2012 through 2015, staff performed testing in clinical and non-clinical settings using rapid HIV-1/HIV-2 tests with oral or blood specimens. Preliminary positive test results were confirmed using an HIV-1 Western blot test with oral, plasma/serum, or dried blood spot specimens or a nucleic acid test with plasma/serum specimens. For at-home testing, MSM used specimen collection kits for the HIV-1 Test System (Home Access Health Corporation, Hoffman Estates, IL) to collect a dried blood spot specimen, which was shipped to the Home Access laboratory for testing. Test results were returned to the individual through an FDA-approved medical call center. MSM with positive test results were connected with a Linkage-to-Care Coordinator.
Inclusion Criteria
In our analysis, we included HIV tests for persons who reported a male sex at birth and a value of ‘male’ or ‘missing’ for current gender identity and excluded 58 HIV tests for persons who declined to report current gender identity. Staff also performed 2191 HIV tests with transgender women (reported male sex at birth and a current gender identity of ‘transgender male-to-female’); results for this subset of participants will be reported and published separately.
Univariate and Bivariate Analyses
To examine characteristics associated with never previously testing (i.e., first-time testing) among MSM, we calculated row percentages for first-time testing by race/ethnicity, age group, recruitment method, high-risk sexual behaviors (i.e., sex with a person known to inject drugs, share needles, or have HIV infection), condom use, gender of sex partners during the past year, and HIV test results (negative or confirmed positive). We categorized MSM by the self-reported gender of their past-year sex partners as MSM who had not been sexually active, MSM who had sex with men only, MSM who had sex with women only, MSM who had sex with men and women, and MSM who had sex with transgender persons (either solely or in addition to cisgender men or women). To examine factors associated with first-time testing for HIV among MSM, we calculated prevalence ratios derived from a binomial regression model. An individual may have tested more than once during the course of this project. To examine the frequency of repeat HIV testing, we characterized HIV tests that matched on both date of birth and the HIV test site as repeat tests (i.e., belonging to the same individual). MSM should only be able to identify once as a first-time tester. Thus, as expected, we found a much higher percentage of potential repeat testing in the previously tested group (“previous testers”) compared to the first-time testers (50.0% compared to 6.5%; see Supplemental Material). Because of this difference in percentages, we controlled for clustering of results in the bivariate analyses based on date of birth and test site for persons who tested repeatedly (see Supplemental Material). As this was an exploratory analysis designed to examine individual factors that may be associated with first-time testing for HIV, we did not calculate adjusted prevalence ratios using regression models [23].
Results
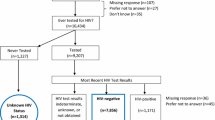
MTI project staff performed 68,826 HIV tests with MSM. We restricted the remainder of our analysis to HIV tests with MSM who provided information on previous HIV testing (99.1%; 68 185/68,826). Less than 10% (8.0%; 5474/68,185) of HIV tests occurred with MSM who reported never previously testing. Over two-thirds (70.7%) of the HIV tests with MSM who had never previously tested were among MSM belonging to racial or ethnic minorities—29.8% (1604/5383) were among non-Hispanic black/African American MSM, 34.0% (1831/5383) were among Hispanic or Latino MSM, and 6.9% (372/5383) were among MSM of other race/ethnicity (American Indian/Alaska Native, Asian, or Native Hawaiian/Pacific Islander) (Table 1). Over half (66.5%) of HIV tests with first-time testers were among MSM younger than 30 years (less than 18 years: 3.3% [178/5442]; 18–24 years: 44.4% [2418/5442]; 25–29 years: 18.8% [1023/5442]). Most HIV tests with first-time testers were among MSM recruited through venue-based testing (90.1%; 4934/5474), and most were among MSM who did not report any past-year sex with a partner who injected drugs/shared needles or was living with HIV (92.6%; 5033/5436). Three-quarters of HIV tests with first-time testers were among MSM who reported past-year sex without using a condom (75.7%; 4128/5452). Most HIV tests with first-time testers were among MSM who reported having male sex partners only during the past year (76.6%; 4133/5399). The remaining HIV tests with first-time testers were among MSM who reported having male and female sex partners (14.7%; 795/5399), MSM who reported not being sexually active (3.4%; 186/5399), MSM who reported having transgender sex partners (either solely or in addition to male or female sex partners) (2.3%; 124/5399), and MSM who reported having female sex partners only (3.0%; 161/5399). Among HIV tests with first-time testers, 3.9% (212/5474) had confirmed positive HIV test results.
In the regression analysis, we controlled for clustering and treated HIV tests with matching information on date of birth and test site as belonging to the same individual. Compared to HIV tests with white MSM, HIV tests with black/African American MSM (prevalence ratio [PR] 1.36, 95% confidence interval [CI] 1.27–1.46), Hispanic or Latino MSM (PR 1.39, 95% CI 1.30–1.49), and MSM belonging to other racial/ethnic groups (PR 1.23, 95% CI 1.10–1.37) were associated with a higher prevalence of first-time testing (Table 1). Except for HIV tests among MSM aged 40–49 years, HIV tests among MSM of all age groups were associated with a higher prevalence of first-time testing compared to tests with those aged 30–39 years. The highest prevalence of first-time testing was associated with HIV tests among MSM who were younger than 18 years (PR 5.14, 95% CI 4.46–5.92). Compared to HIV tests with MSM who were recruited through venue-based testing, HIV tests among MSM who used at-home HIV testing were associated with the highest prevalence of first-time testing (PR 4.69, 95% CI 4.22–5.21); only HIV tests performed via couples voluntary counseling and testing (PR 0.72, 95% CI 0.55–0.94) was associated with a lower prevalence of first-time testing. HIV tests with MSM who reported past-year high-risk sexual behaviors (i.e., sex with a partner who injects drugs, shares needles, or is living with HIV) were associated with a lower prevalence of first-time testing (PR 0.59, 95% CI 0.54–0.65) compared to HIV tests among MSM who did not report these behaviors. HIV tests with MSM who reported sex without a condom during the past year were associated with a higher prevalence of first-time testing (PR 1.16, 95% CI 1.10–1.24) compared to HIV tests with those who did not report it. Compared to HIV tests with MSM who reported having male sex partners only during the past year, HIV tests with all other groups of MSM were associated with a higher prevalence of first-time testing; the highest prevalence of first-time testing was associated with HIV tests among MSM who reported having female partners only (PR 3.62, 95% CI 3.15–4.15). Compared to HIV tests among MSM who received negative HIV test results, HIV tests among MSM who received confirmed positive HIV test results were associated with a higher prevalence of first-time testing (PR 1.24, 95% CI 1.09–1.42).
Discussion
The MTI project provided data on a large number of HIV tests with MSM who were at risk for HIV infection but had never previously tested for HIV. We examined data from HIV tests that occurred primarily in non-clinical settings and found that 8.0% of HIV tests were among MSM who had never previously tested; 212 of the HIV tests among MSM who had never previously tested resulted in a confirmed positive test result. Similar to other large-scale testing programs or surveillance systems, we found a higher prevalence of first-time testing among MSM belonging to younger age groups [9, 10, 12, 14, 16]. In a recently published report involving data on CDC-funded HIV tests with young people during 2015, CDC identified a need for increased HIV testing among young MSM in non-clinical settings [24]. In our analysis, the prevalence of first-time testing was highest among HIV tests with MSM younger than 25 years, further emphasizing the need to increase HIV testing among this group. We found a lower percentage of confirmed positive HIV test results among MSM younger than 25 years who had never previously tested compared to their older counterparts, although small cell sizes prevented us from assessing whether these differences were significant. Additional analyses are needed to examine potential associations between age group and HIV test results among MSM testing for the first time.
Compared to MSM who reported having male sex partners only during the past year, we found a higher prevalence of first-time testing among MSM who reported having female sex partners only, both female and male sex partners, transgender sex partners (not excluding male and/or female sex partners), and MSM who had not been sexually active during the past year. HIV tests among MSM who reported both male and female sex partners or female sex partners only were 2 times as likely and nearly 4 times as likely (respectively) to have occurred with first-time testers. Previous research has identified factors such as experienced or perceived MSM- or HIV-related stigma, bisexual or heterosexual identity, race/ethnicity, and cultural concepts of masculinity (especially among non-Hispanic black or Hispanic or Latino MSM) that could serve as barriers to seeking HIV testing for MSM who also have sex with women [10, 14, 17, 25,26,27]. In addition to employing behavioral interventions that may address some of these barriers, HIV prevention and testing program staff may employ recruitment methods such as social network strategy and alternate venue testing that have been shown to be successful at reaching men who identify as bisexual and have never tested [28]. Our analysis included data from MSM who reported having both male and female partners or female partners only during the past year; data on sexual orientation were not available. Regardless, these data show that the MTI project, which was implemented primarily in non-clinical settings, was successful at reaching MSM who also have sex with women and have never tested.
Compared to venue-based HIV tests, we found a higher prevalence of first-time testing for MSM who were tested at large-scale testing events, were recruited via social network strategy (i.e., recruited for HIV testing by members of their own social network) and then tested, or were recruited for at-home testing [19]. At-home tests with MSM were nearly 5 times as likely to be associated with first-time testing compared to venue-based tests. For the MTI project, MSM were recruited for at-home testing via web-based promotion. Other studies involving online recruitment of MSM for cross-sectional surveys and/or HIV testing have been effective at identifying groups of MSM who have never previously tested and who may be eligible for at-home testing [11,12,13,14, 29]. For MSM who have never previously tested, at-home testing can address some of the barriers associated with traditional HIV testing, including HIV- or MSM-related stigma, confidentiality, and structural barriers (e.g., transportation, access to HIV testing facilities) [13, 29,30,31]. However, qualitative research with MSM have identified other barriers specific to at-home testing, including concerns pertaining to the comprehension and interpretation of test instructions and results and privacy (when purchasing test kits) [29,30,31,32]. Novel approaches that address these concerns (e.g., cell phone application to detect when at-home test kits are opened, phone-based follow-up) are being developed and could be incorporated into HIV testing and prevention programs to reach MSM who might otherwise be reluctant to test [32]. Such approaches in conjunction with other improvements to at-home tests (e.g., improved sensitivity, capacity to detect HIV infection earlier) could make at-home testing an effective tool for reaching MSM who have never previously tested.
Our analysis of first-time testing for HIV among MSM has several limitations. With the exception of HIV test results, we used self-reported data. In addition, these data represent the number of HIV tests performed during the MTI project as opposed to the number of persons who tested. Results from our assessment of repeat testing based on birthdate and test site suggested that 6.5% of MSM may have tested through MTI more than once and still identified as never previously testing. For HIV tests with MSM who identified as previous testers, half (50.0%) of the tests performed may have represented repeat MTI tests. However, we accounted for this potential limitation in the regression analysis by controlling for clustering based on date of birth and test site. Finally, we did not have information available on specific sexual encounters or partner characteristics and therefore could not examine the frequency of unprotected sexual encounters, encounters with high-risk partners, or partner characteristics (e.g., HIV viral load or medication adherence for partners with diagnosed HIV infection, safe injection practices for partners who inject drugs) for MSM who had never previously tested.
Overall, our results indicated that among a racially and ethnically diverse group of MSM, 8% of HIV tests occurred with MSM who had never previously tested for HIV. Based on national estimates of never testing among MSM (approximately 30%), MTI was not highly effective at reaching first-time testers [7, 8]. However, MTI reached some MSM who had never previously tested for HIV and were identified as having confirmed HIV infection (3.9% of HIV tests with first-time testers). Additionally, results from our analysis suggest that at-home testing and interventions designed to reach MSM who are young or also have sex with women may provide effective methods for HIV prevention and other health care professionals to access groups of MSM who have never previously tested. By reaching and testing MSM who have never previously tested, professionals help to increase awareness of HIV status and ultimately reduce the number of previously undiagnosed infections among MSM in the United States.
References
Hess KL, Hu X, Lansky A, et al. Lifetime risk of a diagnosis of HIV infection in the United States. Ann Epidemiol. 2017;27(4):238–43. https://doi.org/10.1016/j.annepidem.2017.02.003.
Centers for Disease Control and Prevention. HIV Surveillance Report, 2016; vol. 28. http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published November 2017. Accessed 1 Dec 2017.
Singh S, Song R, Johnson AS, et al. HIV incidence, prevalence, and undiagnosed infections in U.S. men who have sex with men. Ann Intern Med. 2018;168:685–94. https://doi.org/10.7326/M17-2082.
Gopalappa C, Farnham PG, Chen Y, Sansom SL. Progression and transmission of HIV/AIDS (PATH 2.0): a new, agent-based model to estimate HIV transmissions in the United States. Med Decis Mak. 2017;37:224–33. https://doi.org/10.1056/NEJMoa1600693.
CDC. Revised recommendations for HV testing of adults, adolescents, and pregnant women in health-care settings. MMWR. 2006;55:1–17.
DiNenno EA, Prejean J, Irwin K, et al. Recommendations for HIV screening of gay, bisexual, and other men who have sex with men—United States, 2017. MMWR. 2017;66(31):830–2.
Febo-Vazquez I, Copen CE, Daugherty J. Main reasons for never testing for HIV among women and men aged 15–44 in the United States, 2011–2015. National Health Statistics Reports; no 107. Hyattsville, MD: National Center for Health Statistics. 2018. https://www.cdc.gov/nchs/data/nhsr/nhsr107.pdf.
Pitasi MA, Oraka E, Clark H, et al. HIV testing among transgender women and men—27 states and Guam, 2014–2015. MMWR. 2017;66(33):883–7.
CDC. HIV infection risk, prevention, and testing behaviors among men who have sex with men—National HIV Behavioral Surveillance, 20 U.S. cities, 2014. HIV Surveillance Special Report 15. http://www.cdc.gov/hiv/library/reports/surveillance/#panel2. Published January 2016. Accessed 14 Nov 2017.
Noble M, Jones AM, Bowles K, et al. HIV testing among internet-using MSM in the United States: systematic review. AIDS Behav. 2016;21(2):561–75. https://doi.org/10.1007/s10461-016-1506-7.
CDC. A web-based survey of HIV testing and risk behaviors among gay, bisexual, and other men who have sex with men—United States, 2012. HIV Surveillance Special Report 14. Revised edition. http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published February 2017. Accessed 14 Nov 2017.
Sanchez TH, Sineath C, Kahle EM, et al. The annual American Men’s Internet Survey of behaviors of men who have sex with men in the United States: protocol and key indicators report 2013. JMIR Public Health Surveill. 2015;1(1):e3. https://doi.org/10.2196/publichealth.4314.
Chavez PR, MacGowan RJ, Borkowf CB, et al. Characteristics associated with HIV self-testing reported by internet-recruited MSM in the United States, eSTAMP baseline data, 2015. In: 9th IAS Conference on HIV Science. Paris, France, 2017 [abstract TUPEC0839].
Margolis AD, Joseph H, Belcher L, et al. ‘Never testing for HIV’ among men who have sex with men recruited from a sexual networking website, United States. AIDS Behav. 2012;16:23–9. https://doi.org/10.1007/s10461-011-9883-4.
Van Handel M, Kann L, Olsen EO, Dietz P. HIV testing among US high school students and young adults. Pediatrics. 2016;137:e20152700. https://doi.org/10.1542/peds.2015-2700.
MacKellar DA, Hou S, Whalen CC, et al. Reasons for not HIV testing, testing intentions, and potential use of an over-the-counter rapid HIV test in an internet sample of men who have sex with men who have never tested for HIV. Sex Transm Dis. 2011;38(5):419–28. https://doi.org/10.1097/OLQ.0b013e31820369dd.
Jeffries WL. HIV testing among bisexual men in the United States. AIDS Educ Prev. 2010;22:356–70. https://doi.org/10.1521/aeap.2010.22.4.356.
Ellen JM, Greenberg L, Willard N, et al. Cross-sectional survey comparing HIV risk behaviours of adolescent and young adult men who have sex with men only and men who have sex with men and women in the US and Puerto Rico. Sex Transm Infect. 2015;91:458–61. https://doi.org/10.1136/sextrans-2014-051712.
Zulliger R, Maulsby C, Solomon L, et al. Cost-utility of HIV testing programs among men who have sex with men in the United States. AIDS Behav. 2017;21:619–25. https://doi.org/10.1007/s10461-016-1547-y.
DiNenno EA, Shouse L, Martin T, Nasrullah M, Baytop C, Orr A, Solomon L. The MSM Testing Initiative (MTI): innovative approaches for HIV testing and linkage to medical care. In: National HIV Prevention Conference. Atlanta, 2015 [abstract 1165].
Solomon L, Baytop C, Orr A, Flygare G, Gasper J, Sullivan P, DiNenno EA. Reaching previously untested men who have sex with men: a public health imperative. In: American Public Health Association Annual Meeting and Expo. Chicago, 2015 [abstract 326379].
Baytop C., Solomon L, Gasper J, Orr A., Shouse L, DiNenno EA. Time to linkage to care among newly diagnosed MSM: the MSM Testing Initiative. In: American Public Health Association Annual Meeting and Expo. Chicago, 2015 [abstract 322618].
Westreich D, Greenland S. The table 2 fallacy: presenting and interpreting confounder and modifier coefficients. Am J Epidemiol. 2013;177(4):292–8. https://doi.org/10.1093/aje/kws412.
Stein R, Song W, Marano M, et al. HIV testing, linkage to HIV medical care, and interviews for partner services among youths—61 health department jurisdictions, United States, Puerto Rico, and the U.S. Virgin Islands, 2015. MMWR. 2017;66(24):629–35.
Forenza B, Benoit E. Exploring service provider perceptions of treatment barriers facing black, non-gay-identified MSMW. J Ethn Cult Divers Soc Work. 2016;25(2):114–29. https://doi.org/10.1080/15313204.2015.1071300.
Muñoz-Laboy M, Severson N, Levine E, Martínez O. Latino men who have sex with transgendered women: the influence of heteronormativity, homonegativity and transphobia on gender and sexual scripts. Cult Health Sex. 2017;19(9):964–78. https://doi.org/10.1080/13691058.2016.1276967.
Jeffries WL. Beyond the bisexual bridge. Am J Prev Med. 2014;47(3):320–32. https://doi.org/10.1016/j.amepre.2014.05.002.
Baytop C, Royal S, Hubbard McCree D, et al. Comparison of strategies to increase HIV testing among African-American gay, bisexual, and other men who have sex with men in Washington, DC. AIDS Care. 2014;26(5):608–12. https://doi.org/10.1080/09540121.2013.845280.
Merchant RC, Clark MA, Liu T, et al. Comparison of home-based oral fluid rapid HIV self-testing versus mail-in blood sample collection or medical/community HIV testing by young adult black, Hispanic, and white MSM: results from a randomized trial. AIDS Behav. 2017;22(1):337–46. https://doi.org/10.1007/s10461-017-1802-x.
Medline A, Daniels J, Marlin R, et al. HIV testing preferences among MSM members of an LGBT community organization in Los Angeles. JANAC. 2017;28(3):363–71. https://doi.org/10.1016/j.jana.2017.01.001.
Sharma A, Chavez PR, MacGowan RJ, et al. Willingness to distribute free rapid home HIV test kits and to test with social or sexual network associates among men who have sex with men in the United States. AIDS Care. 2017;29(12):1499–503. https://doi.org/10.1080/09540121.2017.1313386.
Wray T, Chan PA, Simpanen E, Operario D. eTEST: developing a smart home HIV testing kit that enables active, real-time follow-up and referral after testing. JMIR mHealth uHealth. 2017;5(5):e62. https://doi.org/10.2196/mhealth.6491.
Acknowledgements
The authors would like to thank Dr. Liza Solomon, Dr. Chanza Baytop, and Alex Orr, MPH, previously of Abt Associates and Dr. Patrick Sullivan of Emory University. Publication of this manuscript would not have been possible without their dedication towards project implementation and monitoring. The authors thank Dr. Muazzam Nasrullah and Dr. R. Luke Shouse of CDC’s National Center for HIV, Viral Hepatitis, STD, and TB Prevention, Division of HIV/AIDS Prevention and Dr. Eduardo Valverde of CDC’s Center for Global Health, Division of Global HIV and TB for their contributions to the design and implementation of the MTI project. Finally, the authors thank Mr. Emilio German of CDC’s National Center for HIV, Viral Hepatitis, STD, and TB Prevention, Division of HIV/AIDS Prevention for his assistance with Spanish translation.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Clark, H.A., Oraka, E., DiNenno, E.A. et al. Men Who Have Sex with Men (MSM) Who Have Not Previously Tested for HIV: Results from the MSM Testing Initiative, United States (2012–2015). AIDS Behav 23, 359–365 (2019). https://doi.org/10.1007/s10461-018-2266-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-018-2266-3