Abstract
Given the popularity of geosocial networking applications (“apps”) among gay, bisexual, and other men who have sex with men (GBMSM), this study sought to examine GBMSM’s willingness to use sexual health and behavior tracking features if integrated within apps they are already using to meet sexual partners. Most GBMSM (91%) recruited on a popular app reported interest in one or more sexual health app features, including features to find LGBT-friendly providers (83%), receive lab results (68%), schedule appointment reminders (67%), chat with a healthcare provider (59%), and receive medication reminder alerts (42%). Fewer GBMSM were interested in tracking and receiving feedback on their sexual behavior (35%) and substance use (24%). Our data suggest that integrating sexual health and behavior tracking features for GBMSM who use apps could be promising in engaging them in HIV prevention interventions. Further research is needed on GBMSM’s perspectives about potential barriers in using such features.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gay, bisexual, and other men who have sex with men (GBMSM) accounted for an estimated 82% of new HIV diagnoses among males in the United States (US) at the end of 2015, and of all diagnoses among people 13–29 years of age, GBMSM accounted for 90% of new diagnoses [1]. It is estimated that 1 in 6 GBMSM will be diagnosed with HIV in their lifetime if current trends do not change [2]. Given a lack of GBMSM-relevant sexuality education in most schools, many young GBMSM turn to the Internet as a source of sexual health information [3, 4]. With the rapid expansion of mobile smartphone applications (‘apps’) and users worldwide [5], understanding acceptability of potential app-based HIV and STI prevention interventions for GBMSM is warranted in order to harness their potential for HIV prevention [6]. At this time there are few proven HIV prevention programs for young GBMSM [7, 8] and developing app-based prevention could potentially reach at-risk groups widely.
Geosocial networking (GSN) apps show promise for HIV prevention given their popularity among GBMSM [9, 10]. Research on Internet-based HIV prevention methods conducted in a large national sample of men who use the Internet to seek sex with men showed high interest and acceptability of various approaches and topics to engage GBMSM about sexual health [11]. Apps are used by individuals to connect with other users (i.e., share messages, photos, and exact location) based on geographical proximity via their cellphones. GBMSM use these apps for entertainment [12], socializing [9, 10, 12, 13], and finding sex partners [6, 9, 10, 12,13,14,15]. In a study conducted in a metropolitan area of Washington, DC, nearly 64% of GBMSM reported using these apps [10]. Comparisons with the general population of GBMSM show app-using GBMSM report more sex partners [16] and reports from GBMSM using GRINDR, a popular app, indicate that they log into sexual networking apps more than 8 times/day and use apps for about 1.3 h/day [9].
GBMSM who report using apps to meet sexual partners seem to be at greater risk for HIV and other STIs than men who do not [6, 17]. Studies have reported increased risk with reports of a greater number of recent sex partners among app-using GBMSM [16] and condomless anal sex (CAS) with a partner met using an app compared to those not using an app to meet sex partners [17]. These data are similar to results from studies on men’s use of the Internet to seek sex partners and increased HIV risk [18], but data do not provide evidence that the Internet leads to higher risk per se [18,19,20]. In a study conducted by our research team comparing daily diaries with retrospective reports of sexual behavior among GBMSM, data show that high-risk GBMSM tend to use the Internet as a tool to meet sexual partners, but daily reports showed that CAS was actually lower with partners met online compared to those met offline [21, 22]. Epidemiological data also add to our understanding of risk profiles of app-using GBMSM and underscore the need for interventions that reach sexual networks more widely. Data from STI clinics provide evidence that app-using GBMSM have higher odds of testing positive for chlamydia and gonorrhea compared to men reporting meeting partners offline [23]. This evidence suggests sexual networks with app-using GBMSM have higher STI network prevalence; thereby, increasing rapid HIV transmission potential given that individuals with bacterial STIs are at two- to fivefold higher risk of HIV [24,25,26].
Given the popularity of apps among GBMSM and the efficient means to meet sexual partners almost immediately, apps represent one of the most promising environments in which to embed HIV prevention. Seventy percent of app-using GBMSM have indicated willingness to engage in app-based HIV prevention programs [6, 27], but no known prior research has explored the types and acceptability of health promotion features among GSN app-using GBMSM. This study sought to examine GBMSM’s willingness to use sexual health and behavior tracking features integrated within GSN apps they are already using to meet sexual partners.
Methods
Participants were recruited via pop-up advertisements and banner ads placed on a geospatial smartphone sexual networking app for GBMSM. The recruitment efforts served the dual purpose of recruiting participants for a randomized controlled trial (RCT; not reported here) and collecting survey data from GBMSM who were ineligible for the RCT [28]. Recruitment advertisements ran from November 2014 through February 2015, throughout the US, and described a university survey seeking input to better understand and serve the health needs of the GBMSM community. Pop-up advertisements were shown five times—the first time a user logged onto the application within each of the scheduled 24-h advertising periods. Supplementing the pop-up advertisements, banner advertisements ran continuously during the period of recruitment. No participation incentives were provided, although depending on responses participants may have been routed to the RCT that provided compensation. This study was approved by the Institutional Review Board of Northwestern University.
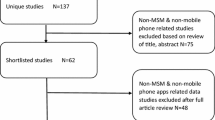
Those who clicked on advertisements were taken to an online eligibility screener. A total of 4783 potential participants clicked the advertisements and of those, 2932 (61.3%) consented and began the screening survey. Of those, 801 (27%) were ineligible due to the following reasons: (1) demographic characteristics (female gender or age under 18 years; n = 30), (2) provisional eligibility for the RCT (age 18–29 years, male sex assigned at birth and male gender identity, not in a serious monogamous relationship lasting more than 6 months, had ever had sex with a male, had CAS in prior 6 months, and HIV negative or unknown status; n = 428), or (3) failure to complete the screening survey (n = 343). During the data cleaning process, 33 surveys were classified as duplicates by matching on 10 demographic characteristics (e.g., age ± 1 year, zip code, etc.) and examination of additional variables (survey date and completion time, survey responses), and were removed from the dataset prior to analysis. The remaining 2098 men were routed to various surveys and of these, 557 GBMSM were asked to report on their interest in a potential mobile phone app to assist in managing their sexual health. Of the 557, 62 participants had incomplete data, resulting in a final analytic sample of 495 GBMSM.
Measures
Demographics and Sexual Behavior
Participants self-reported their demographic characteristics, including age, sexual identity, race/ethnicity, educational achievement, employment status, income, geography (rural, suburban, urban, other), relationship status, HIV-status, and engagement in CAS and group sex activities.
Sexual Health App Use
To assess interest in a potential app features, participants were instructed: “Researchers are interested in developing a mobile app that would be helpful to gay and bisexual men in managing their sexual health. This app could involve a variety of features and we’re interested in knowing which of them you would be willing to use. Choose all that apply.” By design, items asked about sexual health (e.g., receive STI results) and behavior-tracking features (e.g., daily sexual behavior and substance use). Participants had the choice to select nine app features, including a tenth option that stated the participant had no interest in an app to manage their sexual health. Participants who reported interest in one or more app features were then asked about their interest in these features being integrated within already-used apps. Responses were measured using a four-point scale ranging from not at all interested to very interested.
Statistical Analysis
Univariate statistics were reported using frequency measures. Bivariate associations between predictors and app feature interest used χ2, Pearson’s correlation, and one-way analysis of variance, as applicable. We used polychoric principal factor analysis with promax rotation to identify similar features to be included in scale measurement. All predictor variables were then retained for inclusion in the adjusted regression models, which were conducted using logistic regression and ordinary least squares regression for categorical and linear outcome variables, respectively.
Results
Participants
A total of 495 GBMSM completed the survey items about their interest in using app features to manage their sexual health. The majority of respondents self-identified as gay and White with a mean age of 38 years old (see Table 1). Most respondents (70%) had a college degree or more; nearly three-quarters of men were employed full- or part-time, and 11% reported full-time enrollment in school. The sample was diverse by income, and more than half (54%) of the respondents reported living in an urban environment. Most men were single (78%) and HIV-negative (77%) or unknown status (11%). About half of the sample reported recent engagement in CAS, and a third of the men reported engaging in group sex within the past year.
GSN App Use and Sexual Health Feature Interest
GBMSM reported using GSN smartphone apps for a variety of reasons and had a high interest in sexual health app features (see Table 2). Sixteen percent of men used GSN apps for chatting, 13% for hooking up with sex partners, 12% for making friends, and about 5% for general networking. Only 3% of GBMSM or less reported using GSN apps for relationships and dating.
Most GBMSM (91%) reported interest in one or more sexual health features. Men were most interested in an app feature to find LGBT-friendly providers (83%), followed by receiving lab results (68%), scheduling appointment reminders (67%), live chatting with a healthcare provider (59%), and receiving medication reminder alerts (42%). A little over one-third (35%) were interested in tracking and receiving feedback on their sexual behavior, and only 24% were interested in tracking and receiving feedback on their alcohol and drug use patterns. Of the 495 respondents, 450 were asked about their interest in integrating features into existing apps already being used (1 did not respond). Mean interest in integrating these features into existing apps already used was modest (M = 2.42, SD = 0.94); however 84% of respondents were at least “somewhat interested” in integrating these sexual health app features into existing mobile applications (Table 2).
In an effort to identify sexual health features with similar preferences by users, we conducted an exploratory factor analysis of app feature preferences; results are presented in Table 3. The LR test of the factor analysis was significant [χ2 (21) = 2342.5, p < 0.001], and two factors emerged from observation of eigenvalues and scree plot [eigenvalues: factor 1 = 3.8 (81% of variance) and factor 2 = 0.9 (20% of variance)]. The two factors that emerged were described as (1) sexual health-related app features and (2) behavior tracking and feedback; however, the eigenvalue < 1 and scree plot were used to distinguish the two items in factor two from factor one. Thus, we retained the items in factor one for scale measurement and analyzed the two items in the second factor separately. A five-item scale based on a count of the number of features endorsed was used to measure sexual health app feature preferences (α = 0.74). On average, GBMSM were interested in 3.2 health-related app features (SD = 1.6). Although the items were correlated and formed a factor in the factor analysis, we analyzed sexual behavior and alcohol and drug use behavior tracking/feedback items separately because of the limitations of a two-item scale. Interests in tracking sexual behavior and alcohol and drug use are likely different based on variables of risky sexual behaviors (e.g., CAS and group sex); combining these measures was anticipated to reduce their effect size and thus, we chose to test these items separately.
Feature Preferences by Demographics and Sexual Behavior
In bivariate analyses (Table 1), while no significant differences in interest in tracking and receiving feedback on sexual behavior were found by race, education, income, relationship status, HIV-status, or engagement in CAS, interest in this feature differed significantly by age, employment status, living environment, and engagement in group sex. Younger men were more interested in the sexual behavior tracking feature compared to older men. GBMSM who were students were most interested in this feature (49%), as were unemployed men (47%). Individuals who reported “other” employment had the lowest percentage of men interested in this feature (19%). Men who lived in rural environment also had the most interest in tracking and receiving feedback on sexual behavior (54%). GBMSM who engaged in group sex in the past year were significantly more likely to be interested in this tracking and feedback feature compared to men who did not report group sex.
Interest in tracking and receiving feedback on alcohol and drug use was significantly different by age, employment status, and income. Younger men were more interested in the alcohol and drug use feature compared to older men. GBMSM who were students were most interested in this feature (40%), followed by those unemployed (32%), employed (22%), and reporting “other” employment (11%). A dose–response gradient by income on interest in tracking and receiving feedback on alcohol and drug use was observed, where those with the lowest income (less than $25,000 annually) were most interested (34%) and those with the highest income or preferred not to disclose were least interested (18 and 12%, respectively). No significant differences in alcohol and drug-related app feature interest were found by race, education, living environment, HIV-status, or engagement in CAS or group sex.
Finally, interest in sexual health-related app features was highest among younger men and men with lower incomes. In a linear relationship by age, younger men reported interest in more features. A similar dose–response trend was observed, where men with lowest incomes were most interested (M = 3.6) and men with higher incomes were less interested (M ≤ 3.2, see Table 1). No significant differences in sexual health-related app feature interest were found by race, education, employment, living environment, HIV-status, or engagement in CAS or group sex in bivariate analyses.
In fully-adjusted regression models (Table 4), age, income, living environment, HIV-status, and engagement in group sex were significantly associated with app feature interest. GBMSM who lived in rural environments had significantly higher interest in tracking and receiving feedback on sexual behavior compared to men in urban environments. Men who reported group sex in the past year were significantly more interested in tracking their sexual behavior and receiving feedback. Younger men were significantly more interested in tracking and receiving feedback on their alcohol and drug use behaviors, as well as in sexual health-related app features. Men with the lowest incomes were interested in significantly more health-related app features compared to men with higher incomes (or chose not to report). Finally, GBMSM living with HIV were significantly less interested in health-related app features.
In further evaluation of bivariate statistics of GBMSM living with HIV, we explored interest in specific health-related app features because of their priority for connection to services as part of treatment as prevention (i.e., TasP) [29] and facilitating health care engagement. Significant omnibus χ2 differences were observed by interest in receiving scheduling alerts [χ2(2) = 8.4, p < 0.05] and receiving lab test results [χ2(2) = 8.2, p < 0.05]. Only 50% of GBMSM living with HIV were interested in receiving scheduling alerts for health care (e.g., HIV/STI testing, annual physicals) compared to 69% of HIV-negative and 66% of unknown status men. Similarly, only 52% of GBMSM with HIV were interested in receiving lab test results through a mobile app compared to 71% of HIV-negative and 66% of unknown status men.
Discussion
In this study, we sought to examine willingness to use sexual health and behavior tracking features among GBMSM. Given research conducted to understand preferences in the development of stand-alone mobile HIV prevention apps [30, 31], we were particularly interested in exploring whether GBMSM would find these features acceptable if they were integrated within GSN apps they are already using to meet sexual partners. We found most GBMSM who use GSN apps are interested in using sexual-health features, but fewer GBMSM are interested in the behavior tracking features. One of the most endorsed features was the capability to make connections with LGBT-friendly providers. Other sexual health features endorsed by the respondents seem to indicate an interest in accessing health information and alerts, including receiving lab results, medication reminder alerts and appointment reminders, as well as to be able to chat in real-time with a healthcare provider. Most were at least somewhat interested in having these features integrated into existing GSN apps, about one in three respondents were interested in features to track and receive feedback about their sexual behavior, and nearly a quarter expressed interest in tracking and receiving feedback on their alcohol and drug use.
These data provide support for the integration of sexual health features into existing dating/meeting apps that are popular among GBMSM. Our findings are consistent with other studies that have found interest among GBMSM about various types of technologies, social media, and online resources for LGBT advocacy and sexual health [4, 6, 11, 32, 33]. Research early in the HIV epidemic has documented the willingness of GBMSM to participate in HIV prevention online [11, 34], and our results indicate GSN app-using GBMSM are willing to engage with HIV prevention and treatment efforts through this medium extension. Furthermore, there is promising evidence that eHealth interventions are efficacious in reducing HIV risk [35]. Understanding GBMSM’s interest in app features will enable the development of tailored programs that can be incorporated into smartphone apps that are already being used by GBMSM.
Preferences by subgroup were also considered to identify whether app features were preferred differentially by sociodemographic characteristics and sexual behavior. We found that younger GBMSM were more willing than older GBMSM to use features to track and receive feedback about their sexual behavior and substance use. Online diaries have been used successfully to track sexual behavior and substance use among young [36, 37] and adult GBMSM [38], and researchers are exploring the impact of coupling tailored feedback on behavioral patterns with self-monitoring diaries [39,40,41,42]. Thus, efforts to leverage this type of technology for tailored HIV prevention programs for young GBMSM could be key, given that this group of men continues to be at increased risk for HIV [6]. Similarly, given disproportionate rates of HIV in the rural South, our finding that GBMSM who live in rural environments had significantly higher interest in tracking and receiving feedback on sexual behavior compared to men in urban environments is also of relative importance. Additionally, GBMSM who reported group sex in the past year were significantly more interested in tracking their sexual behavior and receiving feedback. We did not ask participants about their reasons for wanting to track or receive feedback about their behavior; however, our data indicate that interventions with a focus on self-monitoring for GBMSM who engage in group sex could be useful in raising awareness about behaviors that may place them at risk of contracting HIV and other STIs and providing strategies to mitigate those risks.
On the other hand, our survey results showed that HIV-positive GBMSM were significantly less interested in using health-related app features compared to HIV-negative and unknown GBMSM. Stigma, negative attitudes and stereotypes have been identified as barriers to engagement in HIV treatment and prevention [43]. Therefore, it is not surprising that fewer HIV-positive men were interested in health app features that would facilitate alerts about scheduled medical appointments and receipt of lab results. While GSN apps could be a convenient approach for improving HIV treatment by providing HIV-positive GBMSM easy access to their patient data and convenient scheduling alerts for health care, potential barriers need to be considered for the development of mobile interventions. Further research is needed on GBMSM’s perspectives and concerns about other potential issues, including unintentional HIV status disclosure, confidentiality, and other unintended consequences of using mobile apps. It is particularly important to gain insight from GBMSM of color, for whom there is a historical context of mistrust of medical and research communities in general [44]. While this is key for both, treatment and care for people with HIV and TasP, it is of equal importance in terms of biomedical prevention efforts, such as pre-exposure prophylaxis (PrEP) that require somewhat similar engagement with the medical community for HIV prevention. Stigma-related barriers to PrEP use are emerging [45] but it is encouraging that two-thirds of the HIV-negative or unknown participants in this study were interested in receiving scheduling alerts and lab results. However, mobile health apps are already developed for an array of public health issues, and embedding HIV-related features into GSN apps GBMSM are using to hook up with other men may not be appropriate for all GBMSM.
Limitations
This study is not without limitations. First, this is a cross sectional survey that was completed by users of one GSN app, therefore the results presented indicate associations, not causality, and could be favorably biased toward app features than if we had a more diverse sample of GBMSM. Second, inclusion criteria for the parent study meant that GSN app members in a serious monogamous relationship (lasting more than 6 months) were not recruited for this study and thus, results could be different with a more diverse sample of GBMSM. Third, although there was ethnic and racial diversity within the sample, most of respondents identified as gay, White, single and HIV-negative and thus, care must be taken in generalizing our findings to GBMSM of color and the larger GBMSM population. However, no statistically significant differences were found among the racial and ethnic groups in their willingness to use the app features described in this study. Furthermore, the study sample was diverse in terms of GSN app use from general networking purposes to seeking relationships and dating, indicating a diverse set of interests. Finally, while GBMSM’s willingness to use sexual health app features is fundamental to integrate sexual health interventions into popular GSN apps, this study did not conduct interviews with app owners or developers to understand their perspectives about adding such features in GSN apps popular among GBMSM and what considerations may be key to successfully incorporate them, such as the level of investment that is needed and perhaps ways to offset costs. Given prior initiatives by GSN app owners to incorporate sexual health information and available resources on their sites through advertising and other means, working in partnership with app developers could help to identify innovative interventions that position sexual health without a primary focus on disease and further stigmatizing sex between men.
Conclusions
Despite these limitations, GBMSM who use GSN apps are interested in using various sexual health related features that could be used for HIV prevention. In fact, these features could reach a wider group of GBMSM more quickly and be cost-effective than in-person programs. As demonstrated through our analysis, subgroup comparisons are key and could provide a more nuanced understanding of app preferences that may lead to tailored efforts targeting at-risk subgroups of GBMSM. We were able to delineate preferences based on various demographic and behavioral characteristics that can be used to tailor HIV prevention interventions for specific subgroups of GBMSM. Future research should engage GBMSM, and particularly men of color, in the development app-based HIV prevention efforts and assessment of their use.
References
CDC. HIV surveillance report. 2017. p. 27. http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Accessed 8 Dec 2017.
Hess K, Hu X, Lansky A, Mermin J, Hall H. Estimating the lifetime risk of a diagnosis of HIV infection in the United States. In: CROI 2016, , Boston, MA, 22–25 February 2016.
Magee JC, Bigelow L, DeHaan S, Mustanski BS. Sexual health information seeking online a mixed-methods study among lesbian, gay, bisexual, and transgender young people. Health Educ Behav. 2012;39(3):276–89.
Mustanski B, Lyons T, Garcia SC. Internet use and sexual health of young men who have sex with men: a mixed-methods study. Arch Sex Behav. 2011;40(2):289–300.
Chaffey D. Mobile marketing statistics compilation: smatinsights.com. 2016 (cited 28 Nov 2016). http://www.smartinsights.com/mobile-marketing/mobile-marketing-analytics/mobile-marketing-statistics/.
Holloway IW, Rice E, Gibbs J, Winetrobe H, Dunlap S, Rhoades H. Acceptability of smartphone application-based HIV prevention among young men who have sex with men. AIDS Behav. 2014;18(2):285–96.
Hergenrather KC, Emmanuel D, Durant S, Rhodes SD. Enhancing HIV prevention among young men who have sex with men: a systematic review of HIV behavioral interventions for young gay and bisexual men. AIDS Educ Prev. 2016;28(3):252–71.
Mustanski BS, Newcomb ME, Du Bois SN, Garcia SC, Grov C. HIV in young men who have sex with men: a review of epidemiology, risk and protective factors, and interventions. J Sex Res. 2011;48(2–3):218–53.
Goedel WC, Duncan DT. Geosocial-networking app usage patterns of gay, bisexual, and other men who have sex with men: survey among users of GRINDR, a mobile dating app. JMIR. 2015. https://doi.org/10.2196/publichealth.4353.
Phillips G, Magnus M, Kuo I, et al. Use of geosocial networking (GSN) mobile phone applications to find men for sex by men who have sex with men (MSM) in Washington, DC. AIDS Behav. 2014;18(9):1630–7.
Hooper S, Rosser BS, Horvath KJ, Oakes JM, Danilenko G. An online needs assessment of a virtual community: what men who use the Internet to seek sex with men want in Internet-based HIV prevention. AIDS Behav. 2008;12(6):867–75.
Rice E, Holloway IW, Winetrobe H, et al. Sex risk among young men who have sex with men who use GRINDR, a smartphone geosocial networking application. J AIDS Clinic Res. 2012. https://doi.org/10.4172/2155-6113.S4-005.
Landovitz RJ, Tseng C-H, Weissman M, et al. Epidemiology, sexual risk behavior, and HIV prevention practices of men who have sex with men using GRINDR in Los Angeles, California. J Urban Health. 2013;90(4):729–39.
Muessig KE, Pike EC, Fowler B, et al. Putting prevention in their pockets: developing mobile phone-based HIV interventions for black men who have sex with men. AIDS Patient Care STDs. 2013;27(4):211–22.
Beymer MR, Weiss RE, Bolan RK, et al. Sex on demand: geosocial networking phone apps and risk of sexually transmitted infections among a cross-sectional sample of men who have sex with men in Los Angeles County. Sex Transm Infect. 2014;90:567–72.
Burrell ER, Pines HA, Robbie E, et al. Use of the location-based social networking application GRINDR as a recruitment tool in rectal microbicide development research. AIDS Behav. 2012;16(7):1816–20.
Holloway IW, Pulsipher CA, Gibbs J, Barman-Adhikari A, Rice E. Network influences on the sexual risk behaviors of gay, bisexual and other men who have sex with men using geosocial networking applications. AIDS Behav. 2015;19(Suppl 2):112–22.
Rosser BS, Miner MH, Bockting WO, et al. HIV risk and the Internet: results of the Men’s INTernet Sex (MINTS) Study. AIDS Behav. 2009;13(4):746–56.
Benotsch EG, Kalichman S, Cage M. Men who have met sex partners via the Internet: prevalence, predictors, and implications for HIV prevention. Arch Sex Behav. 2002;31(2):177–83.
Liau A, Millett G, Marks G. Meta-analytic examination of online sex-seeking and sexual risk behavior among men who have sex with men. Sex Transm Dis. 2006;33(9):576–84.
Mustanski B, Newcomb ME, Clerkin EM. Relationship characteristics and sexual risk-taking in young men who have sex with men. Health Psychol. 2011;30(5):597.
Mustanski BS. Are sexual partners met online associated with HIV/STI risk behaviours? Retrospective and daily diary data in conflict. AIDS Care. 2007;19(6):822–7.
Beymer MR, Weiss RE, Bolan RK, et al. Sex on demand: geosocial networking phone apps and risk of sexually transmitted infections among a cross-sectional sample of men who have sex with men in Los Angeles County. Sex Transm Infect. 2014;90(7):567–72.
CDC. HIV prevention through early detection and treatment of other sexually transmitted diseases—United States. Recommendations of the Advisory Committee for HIV and STD Prevention. MMWR. 1998;47(RR-12):1–24.
Nusbaum MR, Wallace RR, Slatt LM, Kondrad EC. Sexually transmitted infections and increased risk of co-infection with human immunodeficiency virus. J Am Osteopath Assoc. 2004;104(12):527–35.
Wasserheit JN. Epidemiological synergy. Interrelationships between human immunodeficiency virus infection and other sexually transmitted diseases. Sex Transm Dis. 1992;19(2):61–77.
Sun CJ, Stowers J, Miller C, Bachmann LH, Rhodes SD. Acceptability and feasibility of using established geosocial and sexual networking mobile applications to promote HIV and STD testing among men who have sex with men. AIDS Behav. 2015;19(3):543–52.
Macapagal K, Coventry R, Puckett JA, Phillips G 2nd, Mustanski B. Geosocial networking app use among men who have sex with men in serious romantic relationships. Arch Sex Behav. 2016;45(6):1513–24.
Cohen SE, Vittinghoff E, Bacon O, et al. High interest in preexposure prophylaxis among men who have sex with men at risk for HIV infection: baseline data from the US PrEP demonstration project. JAIDS. 2015;68(4):439–48.
Goldenberg T, McDougal S, Sullivan P, Stekler J, Stephenson R. Preferences for a mobile HIV prevention app for men who have sex with men. JMIR mHealth and uHealth. 2014;2(4):e47.
Goldenberg T, McDougal S, Sullivan P, Stekler J, Stephenson R. Building a mobile HIV prevention app for men who have sex with men: an iterative and community-driven process. JMIR Public Health Surveill. 2015;1(2):e18.
Hirshfield S, Chiasson MA, Joseph H, et al. An online randomized controlled trial evaluating HIV prevention digital media interventions for men who have sex with men. PLoS ONE. 2012;7(10):e46252.
Swendeman D, Rotheram-Borus MJ. Innovation in sexually transmitted disease and HIV prevention: Internet and mobile phone delivery vehicles for global diffusion. Curr Opin Psychiatry. 2010;23(2):139.
Mustanski BS. Getting wired: exploiting the Internet for the collection of valid sexuality data. J Sex Res. 2001;38(4):292–301.
Schnall R, Travers J, Rojas M, Carballo-Diéguez A. eHealth interventions for HIV prevention in high-risk men who have sex with men: a systematic review. J Med Internet Res. 2014. https://doi.org/10.2196/jmir.3393.
Newcomb ME, Mustanski B. Racial differences in same-race partnering and the effects of sexual partnership characteristics on HIV risk in MSM: a prospective sexual diary study. JAIDS. 2013;62(3):329.
Newcomb ME, Swann G, Estabrook R, et al. Patterns and predictors of compliance in a prospective diary study of substance use and sexual behavior in a sample of young men who have sex with men. Assessment. 2016. https://doi.org/10.1177/1073191116667584.
Newcomb ME, Swann G, Mohr D, Mustanski B. Do diary studies cause behavior change? An examination of reactivity in sexual risk and substance use in young men who have sex with men. AIDS Behav. 2018. https://doi.org/10.1007/s10461-018-2027-3.
Grov C, Golub SA, Mustanski B, Parsons JT. Sexual compulsivity, state affect, and sexual risk behavior in a daily diary study of gay and bisexual men. Psychol Addict Behav. 2010;24(3):487.
Mustanski B. Moderating effects of age on the alcohol and sexual risk taking association: an online daily diary study of men who have sex with men. AIDS Behav. 2008;12(1):118–26.
Rendina HJ, Ventuneac A, Mustanski B, Grov C, Parsons JT. Prospective measurement of daily health behaviors: modeling temporal patterns in missing data, sexual behavior, and substance use in an online daily diary study of gay and bisexual men. AIDS Behav. 2016;20(8):1730–43.
Swendeman D, Comulada WS, Ramanathan N, Lazar M, Estrin D. Reliability and validity of daily self-monitoring by smartphone application for health-related quality-of-life, antiretroviral adherence, substance use, and sexual behaviors among people living with HIV. AIDS Behav. 2015;19(2):330–40.
Gamarel K, Nelson K, Stephenson R, Santiago Rivera O, Chiaramonte D, Miller R. Anticipated HIV stigma and delays in regular HIV testing behaviors among sexually-active young gay, bisexual, and other men who have sex with men and transgender women. AIDS Behav. 2018;22(2):522–30.
Underhill K, Morrow K, Colleran C, et al. A qualitative study of medical mistrust, perceived discrimination, and risk behavior disclosure to clinicians by U.S. male sex workers and other men who have sex with men: implications for biomedical HIV prevention. J Urban Health. 2015;92(4):667–86.
Biello K, Oldenburg C, Mitty J. The, “safe sex” conundrum: anticipated stigma from sexual partners as a barrier to PrEP use among substance using MSM engaging in transactional sex. AIDS Behav. 2017;21(1):300–6.
Acknowledgements
Data for this study were collected in concert with online recruitment efforts for the Keep It Up! randomized controlled trial funded by the National Institute on Drug Abuse (R01DA035145, PI: Mustanski). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors would like to give special thanks to Krystal Madkins and Craig Sineath for managing the advertisement campaign, Katie Andrews for survey programming and data management, and Mark Pawson and Ruben Jimenez for their contributions to the project.
Funding
This study was funded by National Institute on Drug Abuse (R01DA035145, PI: Mustanski).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Ana Ventuneac, Steven A. John, Thomas H. F. Whitfield, Brian Mustanski, and Jeffrey T. Parsons declare that they have no conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the Ethical Standards of the Institutional and/or National Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Ventuneac, A., John, S.A., Whitfield, T.H.F. et al. Preferences for Sexual Health Smartphone App Features Among Gay and Bisexual Men. AIDS Behav 22, 3384–3394 (2018). https://doi.org/10.1007/s10461-018-2171-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-018-2171-9