Abstract
The American Men’s Internet Survey (AMIS) is conducted annually with 10,000 men age 15 + who have sex with men (MSM). Modeling was used with 39,863 AMIS surveys from 4 cycles between December 2013 to February 2017 to identify temporal trends in sexual behavior, substance use, and testing behavior (within 12 months preceding interview) stratified by participants’ self-reported HIV status. HIV-negative/unknown status MSM had significant increases in condomless anal intercourse (CAI), marijuana use, use of other illicit substances, sexually transmitted infection (STI) diagnoses, and HIV or STI testing (testing only increased among MSM age 25 +). HIV-negative/unknown status MSM had significant decrease in CAI with an HIV-positive or unknown status partner. HIV-positive MSM had significant increases in CAI, methamphetamine use, and STI diagnoses/testing. Although encouraging, the few indicators of improvement in HIV/STI sexual health practices are not consistently seen across sub-groups of MSM and may be counteracted by growing proportions of MSM engaging in CAI and acquiring STIs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Men who have sex with men (MSM) are the US population most impacted by HIV infection. MSM account for 59% of those living with HIV infection, 69% of new HIV diagnoses each year, and an estimated 27,000 new infections per year [1, 2]. MSM are also disproportionately impacted by sexually transmitted infections (STI), and are more than 10 times as likely to be diagnosed with gonorrhea and more than 70 times more likely to be diagnosed with syphilis than women or heterosexual men [3, 4]. There is evidence that some groups of MSM, such as African American MSM under the age of 25, continue to see rising annual numbers of persons newly diagnosed with HIV and STIs, while the rest of the nation has experienced flat or declining trends in these indicators [1, 3]. Data from the Centers for Disease Control and Prevention’s National HIV Behavioral Surveillance System (NHBS) show significant increases in the proportion of MSM who report sexual risk behaviors during the past decade [5, 6]. NHBS has also shown some encouraging trends, such as increased proportions of MSM who have been tested for HIV in the past 12 months [7].
Although NHBS provides a valuable source of information about trends in the behaviors of MSM who live in the 20 largest US cities, it is only conducted among MSM every 3 years, and trend data have not been updated since the 2011 collection [5, 8, 9]. At the same time, there has been substantial progress made in conducting large ongoing behavioral surveys of MSM using Internet-based behavioral surveillance methods [10, 11]. Online approaches to sampling of MSM are also aligned with the changing context of social interactions, whereby there are rapidly growing numbers of men who use social networking websites and apps for meeting sexual partners [12,13,14,15]. Although most online behavioral surveillance methods typically use convenience sampling rather than probability sampling, it can allow researchers to reach populations on a national scale with more frequent data collection at substantially reduced costs when compared to traditional approaches such as venue-time–space sampling used by surveys such as NHBS [16]. While there will likely always be a need for the collection of behavioral data using more methodologically stringent sampling, approaches such as online surveys that use convenience sampling should be seen as providing complementary data that contributes to an overall approach to effectively monitoring key sexual risk behaviors among MSM that is more responsive to emerging public health issues than traditional surveys.
The largest ongoing behavioral survey of this type for MSM in the US is the American Men’s Internet Survey (AMIS). This survey has been conducted among approximately 10,000 MSM participants each year since 2013 [16,17,18]. Data collected through AMIS are similar to those collected through NHBS and allow monitoring of behaviors that are critical to understanding population-level trends in sexual risk behaviors and prevention practices for HIV and STIs among MSM. In this study we utilize AMIS data to determine whether there are significant temporal trends in key behaviors related to risk or prevention of HIV or STI infection among national samples of MSM recruited online. To allow understanding of data from different behavioral surveillance systems, we also sought to determine whether any trends in behaviors observed in AMIS data (condomless anal intercourse, substance use, STI testing and diagnosis, and HIV testing) differed by self-reported HIV status or residence in one of the major US cities targeted by NHBS.
Methods
Study Population
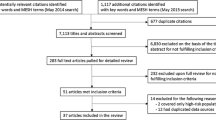
AMIS is conducted in annual cycles with a goal of at least 10,000 complete surveys from eligible MSM each year. The methods have been previously reported in detail [16,17,18]. Briefly, participants were recruited through convenience sampling from a variety of websites using banner ads and email blasts to website members (hereafter referred to as “ads”). Men who clicked on ads were taken directly to the survey website hosted on a secure server administered by SurveyGizmo (Boulder, CO, USA). The survey was self-administered, could be taken on a computer or mobile device and was comprised of questions on demographics, sexual behaviors, substance use, HIV and STI testing and diagnosis, and use of HIV prevention services (see online supplemental material for full AMIS-2016 survey). To date, AMIS has completed four annual data collection cycles: December 2013–May 2014 (AMIS-2013), October 2014–April 2015 (AMIS-2014), September 2015–April 2016 (AMIS-2015), and September 2016–February 2017 (AMIS-2016). For the AMIS-2015 and AMIS-2016 cycles, participants were also recruited by emailing participants from the previous cycles of AMIS (2014 and 2015) who consented to be re-contacted for future studies.
Participants were eligible to participate if they were male sex at birth, resided in the US, and reported oral or anal sex with a man at least once at any time in the past. In AMIS-2013, only participants age 18 years and older were eligible, while for AMIS-2014 onward, eligibility criteria were changed to include participants age 15 years and older. As is standard in behavioral research with MSM, persons who were male at birth but currently identified as female or transgender were excluded from the study. Persons who reported being below the age of eligibility or refused to provide their age were not asked any other screening questions. Participants who met the eligibility criteria and consented to participate in the study started the online survey immediately. No incentive was provided to participants.
Measures
The dependent measures presented in these trend analyses are self-reported behaviors that occurred during the 12 months preceding survey participation. Two sexual behaviors were included in these analyses: condomless anal intercourse (CAI) with any male partner and CAI with any male partner of discordant or unknown HIV status. HIV serostatus discordance was based on the participant’s self-reported HIV status and the status of their male sex partner(s). Discordance was defined as either the participant or partner having unknown status or when one was HIV-negative and the other was HIV-positive. Three substance use behaviors were included in these analyses: use of marijuana (alone or combined with other substances), use of any illicit drug other than marijuana, and use of methamphetamines (alone or combined with other substances). Overall illicit substance use is a standard indicator in HIV behavioral surveillance projects. Marijuana use was included as a separate indicator because it is the most commonly reported illicit substance (under federal law) by our participants. Methamphetamine use was included as a separate indicator because it is the only substance where a plausible direct biologic pathway to increased HIV acquisition risk has been proposed [19]. Problem alcohol consumption was not assessed after AMIS-2013 and could not be used in the trend analyses. Substance use was assessed as the use of any type of drug not prescribed for the participant, by any means of delivery including injection. STI testing behaviors and STI diagnoses included gonorrhea, Chlamydia and syphilis. In AMIS-2013 only a subset of the total sample was asked questions about STI testing and diagnosis. HIV testing in the past 12 months is presented only for participants who reported their HIV status as negative or unknown.
In addition to standard individual demographic characteristics (age and race/ethnicity), we categorized participants based on recruitment source. Banner ads and email blasts contained unique links, which allowed us to determine from which website or app participants entered the survey. We categorized these by target audience and purpose: gay social networking, gay general interest, general social networking and geospatial social networking (i.e., “dating” apps). We do not provide the names of the websites and apps to preserve operator and client privacy. Participants who agreed to be contacted for future studies were emailed links to participate in subsequent rounds of AMIS. This produced participants who completed the survey in more than 1 year; participants recruited from previous AMIS cycles for AMIS-2015 and AMIS-2016 were categorized according to their original recruitment source for analyses of behaviors.
Self-reported HIV status was determined from responses to questions about having ever had an HIV test, results of the most recent HIV test, and having ever had a positive HIV test. Participants were categorized as HIV-positive, HIV-negative, or unknown status. ZIP codes were used to determine county and state of residence, and residence in a NHBS city.Footnote 1 [9], Residential urbanicity was assessed at the county-level using the National Center for Health Statistics (NCHS) Rural–Urban classification scheme [20]. We further collapsed these categories into a four-level urbanicity variable: urban (central), suburban (fringe), medium/small metropolitan and rural (micropolitan and non-core).
Statistical Analyses
Eligible consenting participants were included in analyses if they were unduplicated by IP address, completed the survey, had sex with a man in the past 12 months, and provided a valid US ZIP code. Methods and results for these recruitment and enrollment analytics have been previously reported [16,17,18]. Overall Chi square tests were used to assess whether participant characteristics differed significantly among annual recruitment cycles. Poisson models using Generalized Estimating Equations (GEE) were used to test for a linear trend between AMIS-2013, AMIS-2014, AMIS-2015 and AMIS-2016 for each of the outcomes, stratified by self-reported HIV-status (positive and negative/unknown). Results are presented for both the total sample and a subset of MSM reporting residence in an NHBS city to allow for direct comparisons with other NHBS reports. It was not the purpose of the study to conduct statistical comparisons of trends between participants that resided in NHBS cities or elsewhere. For individual AMIS cycles, those data comparisons have been previously published [16,17,18]. All models included AMIS cycle, age, race/ethnicity, recruitment source and urbanicity (all categories for entire sample and sub-urban/urban for NHBS residents). AMIS cycle and age were treated as continuous variables. Models included interaction terms for AMIS cycle by age if significant (p < 0.05). For models where the age by AMIS cycle interaction term was significant, model findings stratified by age group are presented. No significant interaction with race/ethnicity was found (data not presented).
Trends in behavioral outcomes by participant HIV status were plotted for each AMIS cycle. Because previous AMIS analyses have identified consistent statistically significant associations between behaviors and recruitment source, the prevalence of each outcome is adjusted for recruitment source, using AMIS-2016 as the standard population [16,17,18]. Multi-variable standardization (recruitment type in combination with age, race/ethnicity, or urbanicity) was considered but was not feasible due to sample sizes of participants living with HIV infection, a stratification that was deemed more critical to present in this part of the analysis. Compared to recruitment source, there was also less evidence from previous AMIS analyses for associations between these factors and key behaviors. Standardization of prevalence estimates by recruitment type does not allow for additional multivariable modeling of trend analyses. Rather we chose a complementary approach to examine trends in standardized prevalence estimates using estimated annual percentage change (EAPC) with 95% confidence intervals (CI). This approach has been previously used to examine trends in behavioral surveillance indicators and provides an estimate of the magnitude of the annual trend in these indicators [21]. Statistical significance for all analyses was denoted at alpha = 0.05.
Results
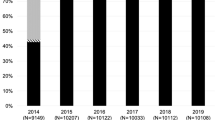
There were 39,863 analyses-eligible MSM participants in 4 annual cycles of AMIS that were conducted from December 2013 through February 2017 (Table 1). Most participants in all cycles were age 30 years or older, non-Hispanic white, and were recruited from general social networking sites. Participants were recruited from all US states and the most common region of residence was the South. Approximately 40% of participants in each AMIS cycle resided in an NHBS city. Most participants resided in an urban or suburban county. Approximately 1 in 10 participants in each AMIS cycle were HIV-positive. All participant characteristics varied significantly by AMIS cycle.
Trends in Condomless Anal Intercourse
Among the HIV-negative or unknown status MSM residing in all regions, the proportion who had engaged in CAI in the past 12 months increased from 61.2% in AMIS-2013 to 65.9% in AMIS-2016 (Table 2a; p < 0.001). There was a significant interaction noted between age and AMIS cycle for trends in any CAI among MSM from all regions. Only MSM who were age 25-29 years or 40 + years had a significant increase in CAI. The proportion of MSM who engaged in CAI with a partner of discordant or unknown HIV status decreased over time from 18.9 to 16.1% (p < 0.001). The decreasing trend in this behavior was noted for all partner pairings: unknown status participants with unknown status partners (18.2 to 14.3%, p = 0.001); negative status participants with unknown status partners (17.0 to 14.3%, p < 0.001); and negative status participants with positive status partners (5.6 to 4.7%, p < 0.001). MSM residing in NHBS cities had similar trends to those residing in all regions—increasing proportions engaged in CAI and decreasing proportions engaged in CAI with a discordant or unknown status partner (Table 2b).
The proportion of HIV-positive status MSM who had engaged in CAI increased from 72.1% in AMIS-2013 to 75.8% in AMIS-2016 for those who resided in all regions (Table 3a; p = 0.001). Though the proportion who engaged in these behaviors were similar for HIV-positive MSM who resided in NHBS cities, there were no significant trends in these behaviors (Table 3b). Neither residency group had significant trends in CAI with a negative/unknown status partner which was similar across both residency groups and ranged from 33 to 40% of participants who reported this behavior in each AMIS cycle (Table 3a and b).
In the analyses that adjusted for recruitment source variations between AMIS cycles, there were no significant trends in CAI in any group (Fig. 1a and b). Additional analyses that attempted to adjust for age group and race/ethnicity in addition to recruitment source also found the same lack of trend in CAI (data not presented). The recruitment-adjusted analyses did show that the proportion of HIV-negative or unknown status MSM who engaged in CAI with a discordant or unknown HIV status partner did decrease significantly over the AMIS cycles for MSM in both residency groups. In all AMIS cycles and residency groups, the proportion of MSM who engaged in any CAI and CAI with a discordant/unknown status male partner was higher among HIV-positive MSM compared to HIV-negative/unknown status MSM.
Proportion of AMIS participants reporting condomless anal intercourse (CAI) and CAI with a partner of discordant or unknown HIV status, in the past 12 months, by participant HIV status and AMIS cycle, for participants in a United States; and b NHBS cities. Estimated annual percentage change (EAPC) and 95% confidence intervals (95% CI) presented
Trends in Substance Use
Use of marijuana in the past 12 months increased from 22.4% in AMIS-2013 to 25.0% in AMIS-2016 among HIV-negative or unknown status MSM residing in all regions (Table 2a; p = 0.005), and from 24.3% in AMIS-2013 to 28.0% in AMIS-2016 among MSM residing in NHBS cities (Table 2b; p = 0.005). Illicit substance use other than marijuana increased for MSM residing in all regions from 16.6% in AMIS-2013 to 18.5% in AMIS-2016 (p = 0.020) but not for those residing in NHBS cities, in which illicit substance use was approximately 20% in each cycle of AMIS. The proportion of HIV-negative or unknown status MSM who used methamphetamine in the past 12 months was generally low (< 3%) for MSM residing in all regions or in NHBS cities and there were no significant trends in the use of this substance.
Approximately 20–30% of HIV-positive MSM used marijuana in the past 12 months, but use did not change significantly across AMIS cycles. There was no significant trend in the proportions of HIV-positive MSM who used illicit substances other than marijuana with the exception of methamphetamine. The use of methamphetamines varied significantly among HIV-positive MSM residing in all areas (Table 3a; p = 0.016) with a low of 10.4% in AMIS-2014 and a high of 12.9% in AMIS-2015. No similar annual variation in methamphetamine use was noted for HIV-positive MSM who resided in NHBS cities.
In the analyses that adjusted for recruitment source variations between AMIS cycles, we only identified a significant increased trend in the use of illicit substances other than marijuana among HIV-negative or unknown status MSM residing in all regions (Fig. 2a and b). Despite this increasing trend, the proportion of MSM who used illicit substances other than marijuana was higher among HIV-positive MSM compared to HIV negative or unknown status MSM across all AMIS cycles. Marijuana use did not significantly increase or decrease for any group and the patterns of marijuana use trends among MSM groups by HIV status and residency are mixed.
Trends in Sexually Transmitted Infection Diagnosis and Testing
The CDC recommends STI screening at least annually for sexually active MSM [22]. The proportion of HIV-negative or unknown status MSM who had an STI diagnosis in the past 12 months increased significantly between AMIS-2013 and AMIS-2016 for MSM residing in all regions (Table 2a; 5.0–9.0%, p < 0.001) and those residing in NHBS cities (Table 2b; 6.6–12.0%, p < 0.001). Gonorrhea, chlamydia and syphilis diagnoses all increased for those MSM in the national sample, but only gonorrhea and chlamydia increased significantly for MSM residing in NHBS cities. The proportion who had an STI test in the past 12 months increased significantly from 38.0% in AMIS-2013 to 48.2% in AMIS-2016 only among MSM residing in NHBS cities (Table 2b, p = 0.024). There was also a significant AMIS cycle and age interaction with STI testing. Among MSM residing in all regions, only those aged 25 or older had a significant increase in STI testing in the past 12 months (Table 2a, p < 0.001). Among MSM residing in NHBS cities, STI testing increased significantly only among those aged 40 years or older (Table 2b, p < 0.001).
The proportion of HIV-positive MSM who had any STI diagnosis in the past 12 months increased significantly from 20.0% in AMIS-2013 to 24.0% in AMIS-2016 for MSM residing in all regions (Table 3a, p < 0.001) and from 22.2 to 29.2% for MSM residing in NHBS cities (Table 3b; p = 0.021). There were significant increases in STI diagnoses noted for gonorrhea, chlamydia and syphilis for MSM in both residency groups. The proportion of HIV-positive MSM who had any STI testing in the past 12 months also increased from 60.8% in AMIS-2013 to 70.9% in AMIS-2016 for MSM residing in all areas (Table 3a, p < 0.001) and from 68.5 to 75.0% for those residing in NHBS cities (Table 3b; p = 0.021).
In the analyses that adjusted for recruitment source variations between AMIS cycles, we found significantly increased proportions of MSM who had STI diagnoses and testing for all groups, except for STI diagnosis among HIV-positive MSM who resided in NHBS cities which showed no change (Figs. 3a and b). The greatest EAPC increases were noted in STI diagnoses (range 15.8–19.7% EAPC) among HIV negative and unknown status MSM in all residency groups and HIV-positive MSM who resided in all regions. In all AMIS cycles and residency groups, the proportion of participants who had STI testing or diagnosis was higher among HIV-positive MSM than HIV-negative or unknown status MSM.
Trends in HIV Testing
The proportion of HIV-negative or unknown status MSM who had an HIV test in the past 12 months was between 49 and 64% across AMIS cycles and residency, but there was no significant trend for either residency group (Table 2a and b). There was significant interaction between age and AMIS cycle for HIV testing, in which only MSM age 25 years and older in both residency groups had an increased proportion who had an HIV test in the past 12 months. In the analyses that adjusted for recruitment source variations between AMIS cycles, significant increases in the proportion of MSM in both residency groups who had an HIV test the past 12 months were found (Fig. 4).
Discussion
The ongoing AMIS study has identified multiple significant trends in the behaviors of MSM over an approximately 4 year period (from December 2013 to February 2017) in large samples of MSM from the entire US. One of the most concerning trends is the significant increase in CAI among most sub-groups of our MSM participants. These increases occurred in the context of high proportions of MSM who engaged in CAI in the past 12 months (approximately two-thirds of HIV negative and unknown status MSM and approximately three-quarters of HIV-positive status MSM) and create concerns for potential ongoing HIV and STI transmission risk in this population. Although we did not identify substantial increases in self-reported HIV prevalence in our study, we identified significant increases in STI diagnoses in the past 12 months among all MSM subgroups we examined. The rates of increase in STI diagnoses are also cause for concern: all groups except HIV-positive MSM residing in NHBS cities had more than a 10% per year annual increase in STI prevalence. These increases in CAI and STI diagnoses among MSM have also been reported in NHBS and in national STI surveillance data [3, 5].
The use of non-prescription marijuana and other illicit substances by HIV-negative or unknown status MSM in our study is growing. MSM living with HIV infection had increases in methamphetamine use. There are no previous national studies reporting on trends in recent substance usage among MSM, but our findings are consistent with a previously published NHBS study of MSM living in San Francisco which showed similar increases there [23]. The increases in non-prescription marijuana usage could be related to recent changes in recreational marijuana laws in some states and changing general public sentiment on legalization and usage [24,25,26,27]. The significant increase in marijuana use remained even when we only analyzed data from states that have not legalized marijuana use (data not presented). There are other potentially burgeoning epidemics in methamphetamine and opioid abuse that could also be reflected in the trends observed for MSM in our study [28,29,30]. These increases are concerning not just because of the detrimental health and community effects of the drugs themselves, but also because substance use has been associated with increases in sexual risk behavior among MSM and may reduce effectiveness of behavioral interventions to prevent HIV infection [19, 31,32,33].
Our study also identified several encouraging trends in behaviors of MSM. There was a significant decrease in the proportion of HIV-negative or unknown status MSM who engaged in CAI with a discordant or unknown status partner. This is consistent with the most recent NHBS report of behavioral trends and may indicate that MSM are increasingly taking other steps to reduce their risk of acquiring HIV [5], such as becoming aware of their own HIV status through testing and selecting partners or sexual activities based on their status, also referred to as serosorting or seroadaptive behavior [34,35,36]. Serosorting or seroadaptive behaviors would involve being aware of one’s own HIV status and we found corroborating data in the significantly increased proportions of MSM that reported being tested for HIV or STIs in the past 12 months. Though these increases in HIV and STI testing are encouraging, the overall prevalence of HIV and STI testing in the past 12 months is still suboptimal for MSM given current CDC guidelines [37]. We also did not find that all sub-groups of MSM had these encouraging trends. Those aged 15–24 years did not have significant increases in these testing behaviors and this group makes up nearly 30% of all new HIV infections among MSM each year [2, 38].
Though the purpose of this study was not to directly compare cross-sectional prevalence of key indicators between demographic or HIV status sub-groups, or compare cross-sectional AMIS data to previously published reports, there are multiple previously published AMIS papers that have reported these findings [16,17,18]. Generally, those previous AMIS reports have shown MSM living with HIV infection have higher prevalence of most behavioral risk indicators than MSM who are HIV-negative or unknown HIV status. Some behaviors, but not all, also significantly vary by NHBS-city residency. AMIS participants who reside in NHBS cities also generally exhibit cross-sectional prevalence of risk behaviors comparable to NHBS study participants for most key indicators [39].
Several limitations of this study should be noted. AMIS data are not generalizable to all MSM in the US or to all MSM online. The convenience sampling approach, even though conducted with multiple types of websites and social networking applications intended to increase sample diversity, increases the potential for selection or enrollment biases. The online convenience sampling approach also introduces more opportunity for year-to-year variations in who is enrolled in the study, demonstrated by statistically significant differences in all participant demographics between AMIS cycles, and necessitated additional statistical approaches to control for these variations. Although much of this variation was an unintentional product of convenience sampling from online websites producing variations in sample composition, some was purposive as we attempted to improve recruitment of youth and African Americans in our study over time. These improvements were comprised of better ads that appealed to these groups, more specific targeting of ads to these groups on platforms that allowed demographic-based targeting, and increasing ad buys on websites/apps that had previously done better for recruitment of these populations. Despite those improvements in diversity of our samples, African American MSM remain under-represented in AMIS—a problem common to internet research [40]. For this trend analysis, we were not able to include information on other practices, such as taking PrEP or having suppressed HIV vial load, that could reduce HIV transmission risk between discordant sexual partners. That information was not included in earlier AMIS cycles. Lack of condom use, including in discordant sexual partnerships, does not equal entirely unprotected sexual risk during anal intercourse. Finally, the surveys only involved self-report of behaviors and HIV/STI diagnosis. It is possible that less socially desirable responses may be under-reported (e.g., CAI) and more socially desirable responses (e.g., recent HIV testing) may be over-reported. These biases may have resulted in incorrectly identifying improved trends in CAI with discordant partners and HIV/STI testing, but would not explain worsening trends in CAI, drug use and STI diagnoses.
In this large ongoing national study of MSM in the United States, we identified significant and substantial trends in most indicators and among most sub-groups of MSM. Most of these changes are not good news for HIV or STI prevention efforts. CAI and diagnoses of STIs are significantly increasing in the context of an increasing potential prevention barrier—substance use. Although encouraging, the few indicators of improvement may not sufficiently counter these concerns. There were reductions in CAI with a partner who was serodiscordant or of unknown status but perceptions of partner serostatus and decisions about condom use in these situations are fraught with potential for errors [41,42,43]. This concern is supported by the fact that only about half of MSM in our study had been tested for HIV in the past 12 months. Although testing has been increasing over time, the CDC currently recommends that all sexually active MSM be tested at least annually as part of a comprehensive HIV prevention approach [22].
This study has shown that the main purpose of the American Men’s Internet Survey (AMIS), to monitor trends in behavioral indicators that are central to HIV prevention efforts, has been met and we were successfully able to detect trends in multiple behaviors. AMIS extends current CDC-supported behavioral surveillance in MSM conducted in cities, and also reflects the important epidemics occurring outside of urban areas. Unfortunately, the trends observed in this more inclusive survey of MSM mostly highlight the improvements that need to be made to ensure that this population achieves the best prevention outcomes such as annual HIV and STI testing, and consistent condom use for sexually active MSM. Continued monitoring of our progress towards these optimal outcomes, and rapidly generating new data about emerging public health issues among MSM will be a critical role for future cycles of AMIS.
Notes
MSAs included in NHBS are: : Atlanta, GA; Baltimore, MD; Boston, MA; Chicago, IL; Dallas, TX; Denver, CO; Detroit, MI; Houston, TX; Los Angeles, CA; Miami, FL; Nassau-Suffolk, NY; New Orleans, LA, New York City, NY; Newark, NJ; Philadelphia, PA; San Diego, CA; San Francisco, CA; San Juan, PR; Seattle, WA; Washington, DC.
References
Centers for Disease Control and Prevention. Diagnoses of HIV Infection in the United States and Dependent Areas. https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2015-vol-27.pdf (2015). Accessed 23 Oct 2017.
Centers for Disease Control and Prevention. HIV Incidence: Estimated Annual Infections in the U.S., 2008–2014. https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/hiv-incidence-fact-sheet_508.pdf (2015). Accessed 23 Oct 2017.
Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance. https://www.cdc.gov/std/stats15/STD-Surveillance-2015-print.pdf (2015). Accessed 23 Oct 2017.
Purcell DW, Johnson CH, Lansky A, et al. Estimating the population size of men who have sex with men in the United States to obtain HIV and syphilis rates. Open AIDS J. 2012;6:98–107.
HIV testing and risk behaviors among gay. bisexual, and other men who have sex with men—United States. Morb Mortal Wkly Rep. 2013;62(47):958–62.
Paz-Bailey G, Mendoza MC, Finlayson T, et al. Trends in condom use among MSM in the United States: the role of antiretroviral therapy and seroadaptive strategies. AIDS. 2016;30(12):1985–90.
Cooley LA, Oster AM, Rose CE, Wejnert C, Paz-Bailey G. Increases in HIV testing among men who have sex with men–National HIV Behavioral Surveillance System, 20 U.S. Metropolitan Statistical Areas, 2008 and 2011. PLoS ONE. 2014;9(9):e104162.
MacKellar DA, Gallagher KM, Finlayson T, Sanchez T, Lansky A, Sullivan PS. Surveillance of HIV risk and prevention behaviors of men who have sex with men–a national application of venue-based, time-space sampling. Public Health Rep. 2007;122(Suppl 1):39–47.
Centers for Disease Control and Prevention. HIV Infection Risk, Prevention, and Testing Behaviors among Men Who Have Sex with Men National HIV Behavioral Surveillance, 20 U.S. Cities. https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-hssr-nhbs-msm-2014.pdf (2014). Accessed 23 Oct 2017.
Hickson F, Tomlin K, Hargreaves J, Bonell C, Reid D, Weatherburn P. Internet-based cohort study of HIV testing over 1 year among men who have sex with men living in England and exposed to a social marketing intervention promoting testing. Sex Transm Infect. 2014;91:24–30.
The EMIS Network. EMIS 2010: The European Men-Who-Have-Sex-With-Men Internet Survey. Findings from 38 countries. https://ecdc.europa.eu/sites/portal/files/media/en/publications/Publications/EMIS-2010-european-men-who-have-sex-with-men-survey.pdf Accessed 23 Oct 2017.
Pew Research Internet Project. Social Media Update. http://www.pewinternet.org/2016/11/11/social-media-update-2016/ (2016). Accessed 8 Aug 2017.
Bolding G, Davis M, Hart G, Sherr L, Elford J. Where young MSM meet their first sexual partner: the role of the Internet. AIDS Behav. 2007;11(4):522–6.
Grosskopf NA, Harris JK, Wallace BC, Nanin JE. Online sex-seeking behaviors of men who have sex with men in New York City. American Journal of Men’s Health. 2011;5(5):378–85.
Centers for Disease Control and Prevention. 15% of American adults have used online dating sites or mobile dating apps. http://assets.pewresearch.org/wp-content/uploads/sites/14/2016/02/PI_2016.02.11_Online-Dating_FINAL.pdf (2016). Accessed 8 Aug 2017.
Sanchez TH, Sineath RC, Kahle EM, Tregear SJ, Sullivan PS. The Annual American Men’s Internet Survey of Behaviors of Men Who Have Sex With Men in the United States: Protocol and Key Indicators Report 2013. JMIR Public Health and Surveillance. 2015;1(1):e3.
Sanchez T, Zlotorzynska M, Sineath C, Kahle E, Sullivan P. The Annual American Men’s Internet Survey of Behaviors of Men Who have Sex with Men in the United States: 2014 Key Indicators Report. JMIR Publ Health Surveill. 2016;2(1):e23.
Zlotorzynska M, Sullivan P, Sanchez T. The Annual American Men’s Internet Survey of behaviors of men who have sex with men in the United States: 2015 key indicators report. JMIR Publ Health Surveill. 2017;3(1):e13.
Colfax G, Santos GM, Chu P, et al. Amphetamine-group substances and HIV. Lancet. 2010;376(9739):458–74.
Ingram DD, Franco SJ. 2013 NCHS Urban-Rural Classification Scheme for Counties. Vital Health Stat. 2014;166:1–73.
Linley L, An Q, Song R, et al. HIV testing experience before HIV diagnosis among men who have sex with men—21 jurisdictions, United States, 2007–2013. Morb Mortal Wkly Rep. 2016;65(37):999–1003.
DiNenno EA, Prejean JIKDK. Recommendations for HIV screening of gay, bisexual, and other men who have sex with men—United States, 2017. Morb Mor Wkly Rep. 2017;66(31):830–2.
Raymond HF, Chen YH, Ick T, et al. A new trend in the HIV epidemic among men who have sex with men, San Francisco, 2004–2011. J Acquir Immune Defic Syndr. 2013;62(5):584–9.
Marijuana Policy Project. State Marijuana Policies. https://www.mpp.org/states/. Accessed 8 Jul 2017.
Centers for Disease Control and Prevention. Support for marijuana legalization continues to rise. http://www.pewresearch.org/fact-tank/2016/10/12/support-for-marijuana-legalization-continues-to-rise/. Accessed 8 Jul 2017.
Gallup. Support for Legal Marijuana Use Up to 60% in U.S. http://news.gallup.com/poll/196550/support-legal-marijuana.aspx (2016). Accessed 8 Jul 2017.
Gallup. In U.S., 45% Say They Have Tried Marijuana. http://www.gallup.com/poll/214250/say-tried-marijuana.aspx. Accessed 8 Jul 2017.
National Institute on Drug Abuse. Available at https://www.drugabuse.gov/national-survey-drug-use-health. . Accessed 23 Oct 2017.
Dart RC, Surratt HL, Cicero TJ, et al. Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med. 2015;372(3):241–8.
Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. MMWR Morb Mortal Wkly Rep. 2016;65(50–51):1445–1452.
Santos GM, Coffin PO, Vittinghoff E, et al. Substance use and drinking outcomes in Personalized Cognitive Counseling randomized trial for episodic substance-using men who have sex with men. Drug Alcohol Depend. 2014;138:234–9.
Morgenstern J, Bux DA Jr, Parsons J, Hagman BT, Wainberg M, Irwin T. Randomized trial to reduce club drug use and HIV risk behaviors among men who have sex with men. J Consult Clin Psychol. 2009;77(4):645–56.
Coffin PO, Santos GM, Colfax G, et al. Adapted personalized cognitive counseling for episodic substance-using men who have sex with men: a randomized controlled trial. AIDS Behav. 2014;18(7):1390–400.
Snowden JM, Wei C, McFarland W, Raymond HF. Prevalence, correlates and trends in seroadaptive behaviours among men who have sex with men from serial cross-sectional surveillance in San Francisco, 2004–2011. Sex Transm Infect. 2014;90(6):498–504.
Khosropour CM, Dombrowski JC, Hughes JP, Manhart LE, Simoni JM, Golden MR. Operationalizing the measurement of seroadaptive behaviors: a comparison of reported sexual behaviors and purposely-adopted behaviors among men who have sex with men (MSM) in Seattle. AIDS Behav. 2017;21:2935–44.
Siegler AJ, Sullivan PS, Khosropour CM, Rosenberg ES. The role of intent in serosorting behaviors among men who have sex with men sexual partnerships. J Acqur Immune Def Syndr. 2013;64(3):307–14.
Centers for Disease Control and Prevention. Sexually Transmitted Diseases Treatment Guidelines, 2015. https://www.cdc.gov/std/tg2015/tg-2015-print.pdf (2015). Accessed 8 Oct 2017.
Singh SS, Ruiguang; Satcher-Johnson, Anna; McCray, Eugene; Hall, Irene. HIV incidence, prevalence and undiagnosed infections in men who have sex with men. Conference on Retroviruses and Opportunistic Infections. Seattle, WA (2017).
Centers for Disease Control and Prevention. HIV Infection Risk, Prevention, and Testing Behaviors among Men Who Have Sex with Men National HIV Behavioral Surveillance 20 U.S. Cities, 2014. 1/1/2016.
Sullivan PS, Khosropour CM, Luisi N, et al. Bias in online recruitment and retention of racial and ethnic minority men who have sex with men. J Medl Internet Res. 2011;13(2):e38.
Vallabhaneni S, Li X, Vittinghoff E, Donnell D, Pilcher CD, Buchbinder SP. Seroadaptive practices: association with HIV acquisition among HIV-negative men who have sex with men. PLoS ONE. 2012;7(10):e45718.
Golden MR, Dombrowski JC, Kerani RP, Stekler JD. Failure of serosorting to protect African American men who have sex with men from HIV infection. Sex Transm Dis. 2012;39(9):659–64.
Eaton LA, Kalichman SC, Cain DN, et al. Serosorting sexual partners and risk for HIV among men who have sex with men. Am J Prev Med. 2007;33(6):479–85.
Acknowledgements
The study was funded by a grant from the MAC AIDS Fund and by the National Institutes of Health [P30AI050409]—the Emory Center for AIDS Research.
Author information
Authors and Affiliations
Contributions
TS, CS, ST and PS developed the research questions, designed the study and materials. TS, MZ, CS, EK and ST implemented the study data collection and contributed to dataset creation over the multiple cycles. MZ conducted the data analyses for this manuscript. TS, MZ and PS wrote the manuscript. All authors critically reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Ethical Approval
The study was conducted in compliance with Federal Regulations Governing Protection of Human Subjects and was reviewed and approved by Emory University’s Institutional Review Board.
Informed Consent
Informed consent was obtained from all individual participants in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sanchez, T.H., Zlotorzynska, M., Sineath, R.C. et al. National Trends in Sexual Behavior, Substance Use and HIV Testing Among United States Men Who have Sex with Men Recruited Online, 2013 Through 2017. AIDS Behav 22, 2413–2425 (2018). https://doi.org/10.1007/s10461-018-2168-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-018-2168-4