Abstract
The role of social desirability bias (SDB) in self-reported HIV risk behaviors continues to be problematic. This study examined whether SDB was associated with self-reported, via audio computer assisted self-interviewing, sexual risk behaviors among people who use drugs. The present study was conducted among 559 participants who reported having a recent sexual partner at their 6-month visit of a longitudinal study. Robust Poisson regression was used to model the association between SDB and five risk behaviors. Analyses were stratified by gender and partner type. Higher scores of SDB were associated with decreased reporting of selling sex and having more than one sexual partner. Higher SDB scores were associated with increased reporting of always using condoms during oral, vaginal, and anal sex. Gender-specific differences were observed. The inclusion of a measure of SDB in data collection, along with other strategies, can be used to both identify and reduce self-report biases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Self-reporting biases, including both acquiescence bias where respondents tend to agree with all questions and respond “yes” when in doubt and social desirability bias where respondents provide information in a manner that they believe will be viewed favorably [1], remain a fundamental concern in HIV prevention and care research. This problem is all too clear when self-reported behaviors do not match other measures of the behaviors [2]. As an example, major discrepancies between self-reports of missed pills and plasma levels of tenofovir as measures of treatment adherence were found in a cohort of women from sub-Saharan Africa [3]. It is often a goal of HIV prevention and care research to change attitudes towards behaviors, such as condom use or medication adherence in order to make the behavior more or less socially desirable and consequently change it. In an effort to change how the behavior is viewed, however, interventions may look effective due to increased reporting of a socially desirable behavior, when in fact, the behavior may not have changed. Alternatively, an increase in socially desirable responding in a comparison condition may mask the impact of effective interventions that significantly changed important HIV prevention and care behaviors.
Many HIV domestic and international intervention and prospective studies have reported declines in HIV risk behaviors after the baseline assessment in all study conditions [4,5,6]. In such studies, it is often difficult to disentangle whether behaviors actually changed, the reporting about the behaviors changed due to social desirability bias, or some combination of both.
Two major components of social desirability bias have been identified: self-deception and impression management. While self-deception has been hypothesized not to be a result of conscious behavior [7], impression management is conceptualized as a conscious effort to portray oneself as having certain characteristics [8], usually, in accordance with social norms of positive health behaviors [9, 10]. In some situations, however, individuals may want to portray themselves as engaging in behaviors that may go against the social norms of one group, but not another. For example, underage drinking may be viewed favorably by peer groups but not by adults. With regard to sexual behaviors, having multiple partners may be viewed as positive among males and negative among females [11]. There is much more evidence to suggest that social desirability bias is due to consciously portraying the self in a positive fashion, rather than unconscious cognitive biases [12].
One of the few studies that have assessed social desirability bias in HIV research found that for individuals who scored lower on a measure of social desirability bias, there was a significantly greater association between self-reported adherence and viral load as compared to those who scored higher [13]. Another study found that social desirability bias was associated with the accuracy of self-reported HIV negative serostatus [14]. A common approach to reducing socially desirable responding has been the use of audio computer assisted self-interviewing (ACASI) rather than face-to-face methods. Yet a systemic review of ACASI compared to face-to-face interviewing found that overall ACASI was not associated with increased reports of sexual risk behaviors; however, among some populations, ACASI use did lead to more frequent reports of some sexual behaviors [15]. It is of great importance to study the presence of socially desirable responding and strategize ways for addressing this bias.
The current study examined whether a measure of social desirability bias was associated with reports of sexual HIV risk behaviors among a sample of people who use drugs and who have high rates of HIV and other STIs in Baltimore City. We were also interested examining gender differences in the associations.
Methods
Study Design and Population
Between July 2009 and July 2013, a longitudinal study was conducted in Baltimore, Maryland to implement and evaluate an intervention of strategies to cope with chronic stress and reduce drug and sexual HIV risk behaviors among heroin and crack users. Neighborhood characteristics, social network factors, and HIV risk behaviors were assessed. In this cross-sectional secondary analysis, data from participants at their 6-month visit were examined, and those participants who reported having no sex partners in the last 90 days were excluded, as these individuals would not be at risk for one of the primary outcomes (n = 98). From the 657 participants with data at the 6-month follow-up visit, 559 were included in this analysis.
Recruitment was conducted using a range of different methods, including street-based outreach, word-of-mouth, flyers, advertisements in local papers, and referrals from community agencies. Participants were screened for eligibility by research staff via telephone or at the research center. Inclusion criteria for enrollment into the study were: (1) aged 18–55; (2) willingness to attend group sessions, and (3) at least one drug related HIV risk behavior defined as (a) self-report injection drug use three or more times in the past week, or (b) crack use in the prior 6 months; and (4) at least one sexual risk behavior, defined as (a) two or more sex partners in the past 90 days or (b) having a sex partner who injected drugs or smoked crack or (c) sex partner is HIV positive. All participants completed written informed consent at the baseline visit. Follow-up visits occurred at 6 and 12 months. Details of full study procedures have been described elsewhere [16]. Ethical approval for the study was obtained from the Institutional Review Board at the Johns Hopkins School of Public Health in Baltimore, Maryland.
Outcomes
In the present analysis, there were five main sexual HIV risk behaviors of interest: (1) participant sold sex for drugs or money in the last 3 months, (2) participant had more than one sexual partner in the past 6 months, and condom use during (3) oral sex, (4) vaginal sex, and (5) anal sex (always versus less than always). Analyses of condom use were stratified by partner type, either main or other partner. It was hypothesized that attitudes and reporting of condom use would differ by partner type. All five main outcome variables were collected via ACASI.
Sensitivity analyses were conducted using variables hypothesized not to be associated with social desirability bias: participant had moved in the last 6 months and having taken part in any study (other than the current one) in the last 6 months.
Covariates
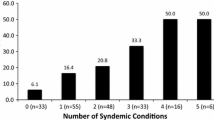
A measure of social desirability bias was the primary covariate. A 10-item scale was used to assess social desirability bias in participants and was developed based on the 33-item Marlow-Crowne Social Desirability Scale [17]. Items were chosen based on a review of all items by staff members who were from the community and then piloted with participants. Participants were asked if ten items were either “true” or “false.” Items included questions like “I have never intensely disliked anyone,” which are highly unlikely to be true but portray the respondent in a positive light. The social desirability scale had a Cronbach’s alpha of 0.68. Based on their responses to all ten questions, participants received a score of 0–10, with higher scores implying higher levels of social desirability bias (Answers that implied greater bias were coded as 1 and answers that implied lower bias were coded as 0). Scores were standardized, using the sample mean (5.34) and standard deviation (2.23) for ease of interpretation. Items defining the social desirability bias scale were collected via ACASI.
Other covariates included drug use in the last 6 months, age, education, employment status, presence of a main sexual partner, HIV status, homelessness, and total monthly income. All covariates were also measured at the 6-month follow-up visit and were categorized based on exploratory analyses and hypothesized relationship to the outcomes. Gender was treated as a potential effect measure modifier. All covariates, with the exception of the presence of a main sexual partner and HIV status which were collected via ACASI, were collected via interviewer-administered questionnaire.
Statistical Analyses
Participants were excluded from analyses if they reported having no sexual partners in the last 90 days. These individuals were excluded because they would not have been at risk for one of the primary outcomes. Demographic characteristics, all of which were dichotomous or categorical, were compared by gender using Pearson’s χ2 tests for proportions. Poisson regression with robust variance estimation was used to assess both crude and adjusted associations of a measure of social desirability bias with each of the sexual HIV risk behaviors, along with whether or not the participant had moved in the past 6 months and whether or not the participant had been a part of a study in the recent past. All analyses were stratified by gender.
Robust Poisson regression was used to model prevalence ratios and 95% confidence intervals because the prevalence of each of the sexual HIV risk behaviors was greater than 10%. Variables were included in the final model based on statistical significance (p < 0.05) in univariate models (not shown) and a priori hypothesized relationships with the outcome. Analyses were conducted with all participants and then restricted to men only and women only. Complete case analysis was performed, as all included variables had less than 3% missing data.
Results
Among those included in this secondary analysis (n = 559), the median age was 45 (interquartile range 41–49), and 48% (268/559) reported being female. Nearly three-quarters of participants had used either heroin or cocaine in the past 6 months (388/559). HIV prevalence was just under 11%, with 39 men and 34 women living with HIV. The median score received on the social desirability scale was a 5 (IQR 4–7).
About half (263/559) reported making less than $500 in the last month, and 53% reported having completed less than high school (298/559). Over one quarter (143/559) of participants reported being homeless in the previous 6 months. Employment status and reporting of a main sexual partner differed significantly by gender, with women being less likely to be employed and more likely to have a main partner compared to men (Table 1).
Selling Sex for Drugs or Money
In the univariate analysis, social desirability bias was negatively associated with selling sex for drugs or money in the last 3 months [prevalence ratio: 0.78, 95% CI 0.67–0.92]. This association remained significant after adjusting for drug use, age, employment status, presence of a main sex partner, HIV status, and homelessness [adjusted prevalence ratio: 0.79, 95% CI 0.68–0.92]. When stratified by gender, the negative association between social desirability bias and selling sex for drugs or money was significant only among women in both the unadjusted and adjusted analyses (Table 2).
Having More than One Sexual Partner
Social desirability bias was negatively associated with reporting more than one sexual partner, but this result was not significant overall in either the unadjusted or adjusted models. When stratified by gender, however, this association was marginally significant among women but not in men in both unadjusted [prevalence ratio: 0.90, 95% CI 0.80–1.00] and adjusted analyses [adjusted prevalence ratio: 0.89, 95% CI 0.80–1.00] (Table 3).
Always Using a Condom During Oral Sex
In both unadjusted [prevalence ratio: 1.62, 95% CI 1.13–2.32] and adjusted [adjusted prevalence ratio: 1.54, 95% CI 1.04–2.29] analyses, social desirability bias was significantly positively associated with always using a condom during oral sex with a main partner. When stratifying by gender, this positive association was no longer significant for either women or men.
When examining the variable of oral sex with other, non-main partners, the measure of social desirability bias was significantly positively associated with always using a condom in both unadjusted [prevalence ratio: 2.50, 95% CI 1.85–3.39] and adjusted [adjusted prevalence ratio: 2.65, 95% CI 1.94–3.61] analyses. This positive association remained significant when stratified by gender for both men and women (Table 4).
Always Using a Condom During Vaginal Sex
In both unadjusted [prevalence ratio: 1.38, 95% CI 1.05–1.81] and adjusted [adjusted prevalence ratio: 1.38, 95% CI 1.08–1.78] analyses, the measure of social desirability bias was significantly positively associated with always using a condom during vaginal sex with a main partner. When stratified by gender, this association was no longer significant for either women or men.
Social desirability bias was significantly positively associated with always using a condom with non-main partners in both unadjusted [prevalence ratio: 1.30, 95% CI 1.07–1.58] and adjusted [adjusted prevalence ratio: 1.28, 95% CI 1.05–1.57] analyses. In the stratified analysis, this positive association remained significant only in men (Table 5).
Always Using a Condom During Anal Sex (Results Not Shown)
In the unadjusted analysis, social desirability bias was positively associated with always using a condom during anal sex with a main partner [prevalence ratio: 1.73, 95% CI 1.14–2.62]. This association did not remain statistically significant after adjusting for drug use, age, employment status, presence of main sex partner, HIV status, and homelessness. Due to a small sample size, it was not possible to assess the association of the measure of social desirability bias with always using a condom during anal sex with non-main partners due to insufficient power.
Sensitivity Analysis
In sensitivity analyses, adjusting for the same variables used in the primary multivariable analyses, there were no significant associations between the measure of social desirability bias and either having taken part in any study (other than the current one) in the last 6 months [prevalence ratio: 1.01, 95% CI 0.82–1.25] or in having moved in the last 6 months [prevalence ratio: 0.98, 95% CI 0.89–1.09].
Discussion
In this study of individuals who use drugs and have high rates of HIV and other STIs, higher social desirability scores were associated with decreased reporting of sexual risk behaviors: selling sex for drugs or money and having more than one sexual partner. We also found that higher scores on social desirability were significantly associated with an increased reporting of protective behaviors, such as always using a condom during oral sex with both main and non-main partners, vaginal sex with both main and other partners, and anal sex with main partners, when compared with lower scores.
Gender-specific differences in associations were also observed. It is possible therefore that there are variations in the perceived desirability of behaviors by gender. For example, women who had higher scores compared to lower scores were significantly less likely to report selling sex for money or drugs or having more than one sex partner; however, this association was not observed in men. Women may perceive selling sex and perceived promiscuity as less socially desirable compared to their male counterparts. Men, on the other hand, were significantly more likely to report using a condom during vaginal sex with other partners with higher scores compared to lower scores, but women were not. It is possible that men felt that using a condom with non-main partners during vaginal sex was a more socially desirable way to respond compared to their female counterparts. These findings suggest some potential effect measure modification by gender and fit into what has been previously observed. Discrepancies between men and women in terms of reporting of sexual partners have been previously reported [18, 19].
A brief measure of social desirability bias, along with knowledge on gender differences in what is considered socially desirable, may help identify individuals who tend to report fewer sexual risk behaviors that are associated with HIV transmission. These data can be used to identify individuals who may respond in a socially desirable manner. Flagging these individuals may allow for identification of responses we need to interpret with caution or the development of statistical adjustment strategies for reported outcomes, potentially improving the accuracy of estimates of risk behaviors and models of transmission dynamics.
Social desirability scales can also provide us with an indication of survey questions that have a high social desirability bias associated with them. Future research could explore whether the bias is due to the wording of questions or the subject matter. One potential method to reduce social desirability is to present the risk behaviors as more normative. This can be accomplished by prefaces to the questions, which may suggest that many people engage in the behavior or that there is a socially acceptable reason for engaging in the behavior, e.g., “many people don’t use condoms always because of their relationship with their partner, not having them at the time, or because of the way they feel,” then asking the question of frequency of condom use [20, 21]. Another method to reduce socially desirable responding may be to ask questions using multiple approaches, using, for example, both an interviewer-administered approach and ACASI approach to ask the same question and comparing responses. Still another method to increase reporting of risk is to alter the response categories [22, 23] If the categories are skewed to the high frequency end, then individuals may perceived that the behavior is more normative and be more comfortable in reporting greater frequency of the behavior [24] For example, if the highest response category for unprotected sex can be changed from “several times a week” to “several times a day”. This approach, however, can result in over-reporting. Even a subtle change in questions, such as “how often do you use a condom” to “how seldom do you use a condom” may alter responses.
It should be noted that even individuals at the low end of the scale of social desirability may still alter their responses to respond in a socially desirable manner. It is also possible that some people are actually engaging in behaviors described in the scale, such as never getting mad, are also actually more likely to use condoms. This interpretation is unlikely however as most of the scale items were extreme, reflecting highly unlikely behavior. Moreover, in a sensitivity analysis, we found that scale scores were not associated with behaviors that we perceived not to have a substantial component of social desirability. This indicates that the scale was unlikely measuring other biases such as acquiescence bias.
One of the drawbacks with assessing social desirability response bias as a scale is that it tends to measure a trait attribute rather than a state [25]. Future research should also focus on state or situational factors that may reduce socially desirable responding, such as interviewer selection and wording of questions. An additional limitation of this analysis was low sample size in stratified analyses. When stratifying by gender and partner type, sample size was diminished and the power to detect significant differences decreased sharply. Another weakness of the study was that due to the low HIV incidence levels in this population we were unable to model how adjusting for social desirability bias may potentially alter the magnitude of the association between risk factors and HIV seroconversion. The ability to generalize from this sample is limited by the specific study population and selection criteria.
Our results are consistent with other studies that highlight the importance of developing methods to improve self-report measures [2, 26] systematically. Efforts to improve self-report measures either require separate validity and reliability studies or the embedding of such studies in ongoing research projects. Although large amounts of resources and time are spent improving and validating laboratory assays, relatively little is spent on enhancing self-report measures in the field of HIV research. If just a few survey items were devoted to improving validity and reliability, it is likely that our measures would be much improved.
Social desirability bias in the reporting of sexual HIV risk behaviors continues to confound our interpretation and understanding of effective prevention and treatment interventions. A measure of social desirability bias along with other strategies to reduce bias should be utilized in order to improve interpretability of findings.
References
Phillips DL, Clancy KJ. Some effects of “social desirability” in survey studies. Am J Sociol. 1972;77(5):921–40.
Weinhardt L, Forsyth A, Carey M, Jaworski B, Durant L. Reliability and validity of self-report measures of HIV-related sexual behavior. Arch Sex Behav. 1998;27(2):155–80.
Agot K, Taylor D, Corneli A, Wang M, Ambia J, Kashuba A, et al. Accuracy of self-report and pill-count measures of adherence in the FEM-PrEP Clinical Trial: implications for future HIV-prevention trials. AIDS Behav. 2015;19(5):743–51.
NIMH. Results of the NIMH collaborative HIV/sexually transmitted disease prevention trial of a community popular opinion leader intervention. J Acquir Immune Defic Syndr. 2010;54(2):204–14.
Koblin B, Chesney M, Coates T. Effects of a behavioural intervention to reduce acquisition of HIV infection among men who have sex with men: the EXPLORE randomised controlled study. Lancet. 2004;364(9428):41–50.
Lippman S, Neilands T, MacPhail C, Peacock D, Maman S, Rebombo D, et al. Community mobilization for HIV testing uptake: results from a community randomized trial of a theory-based intervention in rural South Africa. J Acquir Immune Defic Syndr. 2017;74(Suppl 1):S44–51.
Tomaka K, Blasovich J, Kelsey R. Effects of self-deception, social desirability, and repressive coping on psychophysiological reactivity to stress. Pers Soc Psychol Bull. 1992;18(5):616–24.
Kuentzel JG, Henderson MJ, Melville CL. The impact of social desirability biases on on self-report among college student and problem gamblers. J Gambl Stud. 2008;24(3):307–19.
Beyer H, Liebe U. Three experimental approaches to measure the social context dependence of prejudice communication and discriminatory behavior. Soc Sci Res. 2015;49:343–55.
Schroder KEE, Carvey MP, Vanable PA. Methodological challenges in research on sexual risk behavior: II. Accuracy of self-reports. Ann Behav Med. 2003;26(2):104–23.
Kelly CA, Soler-Hampejsek E, Mensch BS, Hewett PC. Social desirability bias in sexual behavior reporting: evidence from an interview mode experiment in rural Malawi. Int Perspect Sex Reprod Health. 2013;39(1):14–21.
Tourangeau R, Yan T. Sensitive questions in surveys. Psychol Bull. 2007;133(5):859–83.
Nieuwkerk PT, De Boer-Van der Kolk IM, Prins JM, Locadia M, Sprangers MA. Self-reported adherence in more predictive of virological treatment response among patients with a lower tendency towards socially desirable responding. Antiviral Therapy. 2010;15(6):913–6.
Latkin C, Vlahov D. Socially desirable response tendency as a correlate of accuracy of self-reported HIV serostatus for HIV seropositive injection drug users. Addiction. 1998;93(8):1191–7.
Phillips AE, Gomez GB, Boily MC, Garnett GP. A systematic review and meta-analysis of quantitative interviewing tools to investigate self-reported HIV and STI associated behaviours in low- and middle-income countries. Int J Epidemiol. 2010;39(6):1541–55.
Latkin C, Murray LI, Clegg Smith K, Cohen JE, Knowlton AR. The prevalence and correlates of single cigarettes selling among urban disadvantaged drug users in Baltimore, Maryland. Drug Alcohol Depend. 2013;132(3):466–70.
Crowne D, Marlow D. A new scale of social desirability independent of psychopathology. J Consult Psychol. 1960;24(4):349–54.
Smith TW. Discrepancies between men and women in reporting number of sexual partners: a summary from four countries. Soc Biol. 1992;39(3–4):203–11.
Finer LB, Darroch JE, Singh S. Sexual partnership patterns as a behavioral risk factor for sexually transmitted diseases. Fam Plan Perspect. 1999;31(5):228–36.
Sudman S, Bradburn N. Asking questions: a practical guide to questionnaire design. San Francisco: Jossey-Bass; 1982.
Catania JA, Binson D, Canchola J, Pollack LM, Hauck W, Coates TJ. Effects of interviewer gender, interviewer choice, and item wording on responses to questions concerning sexual behavior. Public Opin Q. 1996;60:345–75.
Schaeffer N, Presser S. The science of asking questions. Ann Rev Sociol. 2003;29:65–88.
Payne SL. The art of asking questions. Princeton: Princeton University Press; 1951.
Tourangeau R, Smith TW. Asking sensitive questions: the impact of data collection mode, question format, and question context. Public Opin Q. 1996;60:275–304.
Schmitt MJ, Steyer R. A latent state-trait model (not only) for social desirability. Personal Individ Differ. 1993;14(4):519–29.
Catania JA, Gibson DR, Chitwood DD, Coates T. Methodological problems in AIDS behavioral research: influences on measurement error and participation bias in studies of sexual behavior. Psychol Bull. 1990;108:339–62.
Acknowledgements
We would like to thank the National Institute on Drug Abuse, who provided funding for this study (DA032217, DA022961). We would also like to thank all of the study participants for their time and efforts.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no potential conflicts of interest.
Informed consent
All participants completed written informed consent at the baseline visit of this study
Rights and permissions
About this article
Cite this article
Rao, A., Tobin, K., Davey-Rothwell, M. et al. Social Desirability Bias and Prevalence of Sexual HIV Risk Behaviors Among People Who Use Drugs in Baltimore, Maryland: Implications for Identifying Individuals Prone to Underreporting Sexual Risk Behaviors. AIDS Behav 21, 2207–2214 (2017). https://doi.org/10.1007/s10461-017-1792-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-017-1792-8