Abstract
Internalized HIV-related stigma negatively impacts the mental and physical health of women living with HIV/AIDS (WLWHA). Yet, some women can successfully confront stigma. The present work uses qualitative methods to investigate the successful stigma coping strategies displayed by 19 WLWHA who reported the least internalized stigma possible on the Internalized AIDS-Related Stigma Scale out of a larger pool of 233 WLWHA in San Felipe de Puerto Plata, Dominican Republic. Such strategies included, HIV disclosure control; preemptive disclosure of HIV-status; educating oneself/others about HIV; viewing HIV as a manageable condition; and looking to family, friends and partners for support. Our findings add to current knowledge about how WLWHA successfully manage internalized stigma, particularly in the context of the Dominican Republic. Clinicians should work closely with WLWHA to counsel them about the stigma coping strategies that best fit their life context.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Stigma is an important obstacle affecting access to health services, [1–3] particularly for people who are living with HIV/AIDS [4]. It is well documented that stigma impedes access to HIV treatment and care [4] and reduces ART adherence [5] for HIV-positive persons. Additionally, stigma is an important predictor of risky sex behaviors, including having multiple sex partners [6]; having receptive vaginal or anal intercourse without a condom [6–8]; drinking before having sex; or exchanging sex for money, alcohol, drugs, or a place to stay [7]. Researchers and public health officials widely recognize stigma as a key barrier to formulating meaningful programmatic responses that address the global HIV epidemic [3]. Most scientific work about stigma focuses on its challenges, rather than on pinpointing strategies to overcome it, which could have a more tangible impact for people living with HIV. Therefore, research that identifies tactics to prevent or reduce HIV-related stigma, using qualitative methods to explore this topic with HIV-positive individuals who are effectively coping with it, is timely and important.
Stigma is “an attribute that is deeply discrediting” [9] and exists in multiple forms, including enacted, perceived, internalized, and “project” typologies. Enacted stigma refers to actual experiences of stigmatization, while perceived stigmas are felt or imagined devaluations from other people and/or institutions [2]. Internalized stigma is characterized by a sense of shame or blame based upon stigmatizing attributes [10]. Less attention has been given to the fourth type of stigma: “stigma projects”. “Stigma projects” are intentional strategies employed by stigmatized individuals to reduce internalized stigma [10], and may be more clearly summarized with the term, “stigma coping strategies.” Combating internalized stigma is extremely important from a clinical perspective, since existing evidence shows that internalized stigma is associated with gaps in medical care, antiretroviral (ART) non-adherence, poorer affective health [11], and depression [12, 13] for HIV-positive individuals. Subsequently, the present paper will focus on stigma coping strategies that can lessen the negative consequences of internalized stigma.
Increasing our understanding of how people living with HIV combat internalized stigma will provide a framework for clinicians and public health organizations to develop more effective stigma prevention and/or reduction strategies for individuals recently diagnosed with HIV. Additionally, reducing internalized stigma could help to lessen the frequency of risky sex behaviors, improve access to HIV-related treatment programs, and increase antiretroviral adherence, [14] thereby impeding the transmission of HIV in high-risk groups [4, 15]. This project aims to document the stigma coping strategies used by women living with HIV/AIDS (WLWHA) in the Dominican Republic. Women are the focus of this work, since gender differentially affects HIV-positive individuals’ experiences with stigma [16]. Gender-based socioeconomic inequalities amplify and worsen the negative impact of HIV-related stigma on women [17]. This is particularly true for women in countries with high rates of female poverty, such as the Dominican Republic [18], the country with the most documented HIV cases in the Caribbean apart from Haiti [19].
In the Dominican Republic, there are 32,000 WLWHA, with a general HIV prevalence of 0.9% [20]. Here, stigma has been identified as a key driver of the HIV epidemic [21], making this a high-priority area for study. Although there are laws and regulations protecting people living with HIV against discrimination, WLWHA report internalized-stigma, including feeling ashamed (41%) or guilty (27%), having low self-esteem (38%), and blaming oneself (29%) or others (49%) [20]. WLWHA also perceive HIV-related discrimination such as gossip (62%), verbal aggression (30%), harassment and verbal or physical threats (27%; 14%), or exclusion from family activities (11%) [20]. These stigma experiences may lead to decisions not to attend social gatherings, not to get married, and not to have children [22]. Nevertheless, over two-thirds of WLWHA report knowing of support groups for people living with HIV and over one quarter report being involved in a program providing assistance to people living with HIV [20]. Given that HIV-related stigma is a critical issue among WLWHA in the Dominican Republic, our study sought to explore their coping strategies in order to promote resilience.
Methods
Research Setting
This research took place in Puerto Plata, a province on the North coast of the Dominican Republic. Puerto Plata was initially selected as the research location because it is a major hub for sex tourism in the Western Hemisphere, which was important for the larger study in which this paper is situated. Specifically, the larger study examined the impact of mothers’ experiences of stigma on the mental and physical health outcomes of their children on two marginalized groups: female sex workers (FSW) and WLWHA. Child health outcomes from these groups were compared with those from a control group of HIV-negative women who were not sex workers.
The incidence of new HIV infections is relatively low in Puerto Plata, despite the substantial concentration of key risk populations, particularly female sex workers [23]. This may be in part due to the efforts of local, progressive, HIV-focused nongovernmental organizations in Puerto Plata. One such organization, El Centro De Promoción y Solidaridad Humana (CEPROSH) has worked in the province since 1987 to design and execute programs to prevent the transmission of HIV and other STIs [24]. CEPROSH has since expanded its mission and efforts now include providing high-quality mental and physical health care to people living with HIV/AIDS, HIV prevention education, efforts to reduce HIV-related stigma, HIV testing initiatives for high-risk populations, and programs to build community capacity, among others [24]. Despite this work, HIV and HIV-related stigma remain persistent problems.
Participating study sites were [1] CEPROSH (Puerto Plata), and [2] a public hospital-based HIV clinic in Puerto Plata that has a close relationship with CEPROSH. Both locations provide comprehensive treatment, care, and support services for people living with HIV/AIDS. Physicians, nurses, psychologists, peer counselors, case managers, and pharmacists provide mental and physical health services to HIV-positive men, women, and children. The clinics serve the largest city in the Puerto Plata province, San Felipe de Puerto Plata, and its municipalities. Participants were patients of the clinics and received at least one psychiatric counseling session as a part of their routine care and have the option to complete others if desired. Additionally, they are managed by peer case managers, many of whom are HIV-positive themselves. Peer case managers help patients to understand treatment options and overcome obstacles to adherence, among other things. Thus, participants in this study may represent a more mobilized and empowered demographic of WLWHA than is typical of the general population of WLWHA. The influence of participation in these programs will be discussed in greater detail in the discussion section.
Participants
This study was a qualitative secondary examination of a mixed-methods, cross-sectional study about motherhood, the health of stigmatized women, and their children. Eligible participants were at least 18 years old, HIV-positive, and not pregnant at the time data were collected. Because the larger study aimed to examine the relationship between mothers’ experiences of stigma and child health outcomes, all participants had to have at least one biological or adopted child age 15 or younger. Specific criteria for inclusion in the qualitative study will be defined in the procedures section.
Procedures
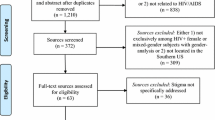
Since this paper focuses exclusively on WLWHA, we will discuss only the study procedures specific to this group. Recruitment took place from May to December 2014 and the overall study took a mixed-methods approach. That is, all participants first completed quantitative surveys, from which eligible qualitative interviewees were identified. All participants were recruited from the waiting rooms of the clinics described in the research setting. In order to recruit participants in this way, a peer research assistant called the clinic administrators the day before the appointed recruitment dates to ensure that: [1] a sufficient number of appointments had been made to warrant recruitment efforts, and [2] clinic staff were aware that the research team was coming. Then, the primary investigator and peer interviewer went to the clinic on the appointed day and explained the study objective and procedures to all individuals in the waiting room at the same time. Interested women were screened for eligibility on-site in private, quiet locations away from the waiting room.
Individuals who met eligibility criteria were verbally administered a quantitative, tablet-based survey in Spanish by a trained interviewer. WLWHA were enrolled into the study until the sampling goal of N = 225 participants was exceeded (actual sample: N = 233). Surveys assessed participant demographics, perceived HIV-related stigma, internalized HIV-related stigma, depression, and physical and mental health outcomes of participants’ children. Since the intent of this paper was to document the stigma coping strategies WLWHA used to reduce internalized HIV-related stigma, participants who had the least amount of stigma possible on the Internalized AIDS-Related Stigma Scale (IA-RSS) [25] were selected for qualitative interviews. Only N = 19 WLWHA (out of a total sample of N = 233 quantitative respondents) reported experiencing no internalized stigma on the IA-RSS. Therefore, 19 participants completed qualitative interviews. Qualitative interviewees completed short, semi-structured open-ended interviews about stigma coping strategies in Spanish. Interviews were conducted immediately after the quantitative surveys and were facilitated by the same interviewer who administered surveys.
All surveys and interviews were conducted privately to ensure participant confidentiality. The Colorado Multiple Institutional Review Board (COMIRB), Consejo Nacional de Bióetica en Salud (CONABIOS) and CEPROSH granted ethical approval for this study. Participation was voluntary and informed written consent was obtained from all participants before enrollment. All WLWHA who participated in the surveys received DOP$150 (US$3.30) for their time. Participants who were selected for qualitative interviews received an additional DOP$150 on top of the money they received for the surveys.
Measures
Semi-structured open-ended interviews were intended to gather information about HIV-related stigma coping strategies. An interview guide focused on participants’ responses and emotional reactions to previous experiences of HIV-related stigma. Interviewees were asked about their reactions to stigmatization from family members, friends, neighbors, and other community members. Additionally, participants were questioned about how stigmatizing events made them feel, if and how they were able to manage stigma on immediate and ongoing bases, how often they experienced stigma and by whom, and potential reasons for why some people might stigmatize WLWHA.
Data Analysis
Audiotapes of interviews were translated into English and transcribed. Data were hand coded and codes were identified through a multilayered coding strategy. The first author and two coders from the University of Colorado-Denver, trained in qualitative research methods, examined the interview transcripts to identify recurring themes. An inductive approach [26] was used for the analysis, where the coders independently reviewed the data and developed a list of emerging themes. Themes were intended to represent the presumed meanings underlying the respondents’ answers. Put another way, the themes identified by coders represented commonalities across participants and items, through which the meaning of participants’ responses could be reasonably interpreted [27].
To ensure that themes represented the data in a reasonable and realistic way, the first author and both coders worked individually to derive them. Then, to encourage consensus among coders, comparisons of codes were made after the first pass through the data and discrepancies were discussed until agreement was reached. The themes were examined alongside examples of data they were intended to represent by the coders. The coders reexamined the data for an all-inclusive assessment of possible themes and met again to discuss the codes, ensure consensus, and verify that the selected quotes illustrated the intended themes. Code constructions for participants’ responses originated from verbal cues. Since interviews were audio recorded, non-verbal cues did not play a role in the creation of codes.
Results
Of the statistically representative sample of N = 233 quantitative participants, a total of 19 WLWHA met the qualitative eligibility criteria (e.g., reporting no internalized HIV-related stigma on the IA-RSS) and participated in semi-structured open-ended interviews. Several themes about stigma coping strategies emerged. Table 1 summarizes the demographic characteristics of participants included in the interviews.
Stigma coping strategies identified in this study are summarized in Table 2 and are discussed below.
HIV Disclosure Control
When asked who knew about their HIV diagnosis, WLWHA explained that only certain people, if anybody, could be trusted with this information. Most participants (N = 14) explained that because the negative consequences of the wrong person finding out about their HIV-positive status are so high, they are extremely strategic about disclosure. Making calculated decisions about who to tell and who to withhold this information from is a stigma coping strategy we termed, “HIV disclosure control.” HIV disclosure control allows WLWHA to selectively share their HIV status with people they believe will be supportive and avoid others they suspect will reject or gossip about them. All women in this study were acutely aware of the negative social consequences, such as community ostracism and employment discrimination, of openly living with HIV in the Dominican Republic. Participants were especially sensitive to the potential for negative changes in their relationships with family members and the anticipated severity of this outcome varied between participants. For instance, some respondents feared complete rejection for living with HIV. One woman had actually experienced this, and revealed that her sister had stopped having a relationship with her after learning that she lives with HIV.
Well, one of my sisters kind of rejected me at first. She told somebody else that she wouldn’t leave her kids with me because I might give them AIDS. And that she wouldn’t live where I live because I have a disease that I can give to other people… I thought that everybody was just going to leave me to die when my sister threw it in my face that I’m sick with HIV (QI010: Participant living with HIV for 11 years).
Other participants did not anticipate outright disownment for living with HIV, but feared they would be looked at less favorably. One woman lamented that she could not tell her father she lives with HIV because, although she suspected he would not reject her, he would likely treat her differently.
I would not tell my dad that I have HIV. My dad always has conversations about… based on the things he says I don’t think he suspects that I have HIV… But he says things about how people with AIDS can infect whoever and so… maybe he wouldn’t reject me but… he says things that are really hard on people who live with this condition. Other family members know and they support me but my mom says to me, “It’s not necessary for your father to know.” My dad is from the country and I’ve always lived apart from him. I’m scared because maybe he won’t reject me but it might change his feelings about me and I would suffer… (QI002: Participant living with HIV for 15 years)
Another participant explained that she would not tell her friend she lives with HIV because she feared this friend would not accept her.
Ok but for example… I have a (female) friend and I go over to her house a lot and I really like her.
But I have… I don’t tell her that I have HIV because there’s people who reject some things… and I don’t know… For example, some people think you can get HIV from using a cup after somebody with HIV has used it. Or from an HIV-positive person using your bathroom. So yeah… I haven’t told her. She doesn’t know… (QI003; Participant living with HIV for 6 years)
Other participants withheld information about their HIV-positive status from people they suspected would tell other people. One woman revealed that she could not disclose her HIV infection to her alcoholic father, since she did not trust him to keep it a secret.
[I would not tell my father that I live with HIV] …Because my dad is a man who likes his alcohol. He drinks a lot. And so when he drinks alcohol, he can’t keep anything to himself… Well, and he’d feel bad. He doesn’t have the awareness to not tell people. (QI014; Participant living with HIV for 5 years)
Alternatively, respondents reported disclosing their HIV status to supportive friends or family members. To participants, “support” meant that targets of disclosure accepted their HIV diagnosis without judgment and did not tell other people about it. One woman explained that she only informs people she suspects will not gossip about her HIV diagnosis.
… If somebody comes to me and I trust them, I would tell them [that I live with HIV]. Because I’m not going to tell somebody that’s going to spread this information into the four winds. To the entire street, the entire neighborhood… A person who is going to tell the entire world. (QI020; Participant living with HIV for 6 years)
Additionally, living with HIV in the Dominican Republic influences individuals’ ability to obtain and hold a job. Although firing or refusing somebody employment because they are HIV-positive is illegal, laws protecting WLWHA against employment discrimination in the Dominican Republic do not always work in practice.
…if you go to look for work. If people know you have HIV it makes it really hard to find a job… (QI003; Participant living with HIV for 6 years)
Moreover, laws to prevent HIV-related employment discrimination do not apply to individuals in the informal economy. Two respondents working in this capacity disclosed feeling pressure to leave their jobs after their respective employers heard rumors about their HIV status. One of these women explained that she quit her job as a domestic worker after her employer started requiring her to wear rubber gloves inside the house and tried to force her to take an HIV test.
…One time I was working as a domestic in the house of a family. And a neighbor of mine was spreading rumors about me because she’s the kind of person who likes to gossip about other people. And she said to my employer, “Did you know that this woman has AIDS? Get rid of her now!” And the next time I saw my employer she said “Put on gloves so you don’t contaminate things… and keep your things separate” … And after like, 20 days my employer came up to me and said, “I’m going to take you to get an HIV test… Because I’ve heard things…” (QI011: Participant living with HIV for 12 years)
Another participant revealed that she was reluctant to disclose her HIV status because it would ruin her reputation in her community, since she would constantly be the subject of others’ conversations.
I wouldn’t tell this neighbor that I have because she’s really gossipy. She likes to run her mouth and she talks a lot… I don’t tell people that I have HIV because sometimes when somebody is doing something controversial, people like to talk about your more (QI014: Participant living with HIV for 5 years)
Preemptive Disclosure of HIV Status
Though participants explained the importance of selecting appropriate targets for HIV disclosure, the timing of disclosure was equally critical. Overwhelmingly, participants preferred to disclose their own HIV status, rather than having it spread in another way. However, when asked about what prompted them to tell others about their HIV status, participants reported instances of “voluntary” and “involuntary” preemptive disclosure (N = 10). With both voluntary and involuntary preemptive disclosure types, participants aimed to tell friends and family members about their HIV diagnosis first, before these people could find out on their own. Voluntary disclosure was characterized by a desire for openness. One woman described how keeping her HIV diagnosis a secret would be more difficult than telling other people.
Pretty much everyone knows… Imagine… It would be harder if somebody came to you and asked if you have HIV, and you told them no. And you wanted to tell them yes, face to face. You know? (QI008: Participant living with HIV for 8 years)
Involuntary disclosure was characterized by participants suspecting that they could not continue to keep their HIV diagnosis a secret. Since they realized that others would find out they were HIV-positive anyway, participants attempted to “get in front of the information” by telling them first. Most often, involuntary disclosure occurred because the respondent became sick with recognizable symptoms of HIV. One participant explained how a severe reaction to her antiretroviral medication led her to tell her family that she is HIV-positive.
Well, it was necessary that I tell my family that I have HIV because I was sick, and they could see that I was sick with HIV… Because I was having stomach problems and I think it was a side effect of the medication. I felt so bad… I was so skinny… (QI003: Participant living with HIV for 6 years)
Educating Oneself and Others About HIV
Participants acknowledged that stigma was the most severe when they were first diagnosed with HIV, but lessened with time. This, one respondent explained, is because few people understand what HIV is, including the recently diagnosed patient.
Now everyone knows I have HIV. I told them because this isn’t a big deal. It’s an illness and nothing more than that. I’ve been taking care of myself with this for two years. My friends and family support me… They have a lot of knowledge about this HIV because I told them…But I felt a lot of stigma when I first got sick. When I first found out, I felt a lot of stigma…When I’d be going around my neighborhood I’d feel stigma because this HIV was an entirely new thing for me…. Everybody in the world started to yell at me and point me out… And gossip about me… Not everybody knows how to treat somebody who has HIV. They’ll start to talk about you behind your back. (QI002; Participant living with HIV for 2 years)
Participants acknowledged that building an understanding of what it means to live with HIV is critical to reducing stigma (N = 9). Learning about how HIV is transmitted was particularly important in this study, since participants reported instances where they were confronted with others’ misconceptions about this theme. Almost all of these misconceptions related to believing you could be exposed to HIV through casual contact, such as sharing eating utensils or food. Participants endorsed the idea that fighting the stigma produced by inaccurate information about HIV transmission occurs in two ways: educating oneself about HIV and educating others. One woman described how she dismissed other people’s incorrect, stigma-promoting ideas about HIV transmission by acknowledging that people who think this simply do not know any better.
Because I live with this condition I have a lot of knowledge about it…When I first tested positive I started gathering information because there’s people who will say, “Ay! You drank out of that glass! I’m not drinking that!” But it’s because these are ignorant people. (QI008: Participant living with HIV for 7 years)
Another woman revealed how educating her family members about HIV transmission has helped them to treat her well.
My family is super informed about HIV. You don’t get HIV from sharing household items – you get it from sexual contact. I’ve explained this a bunch of times because I’ve had a lot of informational meetings with outreach workers….Everybody treats me well… (QI007: Participant living with HIV for 7 years)
Viewing HIV as a Chronic and Manageable Condition
Participants (N = 12) explained that viewing HIV as a chronic and manageable condition is particularly important for overcoming stigma. WLWHA in this study endorsed the idea that living with HIV is not different than living with other chronic diseases.
…This isn’t…HIV isn’t a big deal… It’s an illness and nothing more than that. I’ve been taking care of myself with this disease for 2 years now… (QI006: Participant living with HIV for 2 years)
Participants credited the hopeful prognosis for persons diagnosed with HIV to the development of effective antiretroviral medications. One respondent described how clinical advances in HIV treatment have transitioned HIV from being a death sentence to an illness that is controllable over a long-term basis.
Well now I think things are better because at least now when a person gets sick, they get a lot of support. They can get medication. I remember that before… Like 18 years before… At that time I was living with my mom, and we knew two people who died of HIV. But at the time, I didn’t know they had died of HIV. And I said to my mom, “What is this? What did they die of?” And she told me, “They died of something that has no cure.” But now science is very advanced and there are a lot of things out there for you if you have HIV. (QI011: Participant living with HIV for 12 years)
However, WLWHA in this study explained that in order for HIV-positive people to see HIV as something manageable, they must learn about treatment options and other forms of self-care (e.g., adherence to medication regimens, getting adequate rest, and eating a proper diet). One participant revealed how she was able to overcome a bout of depression once she began an effective care regimen.
You can get depressed… but right now my health is completely fine like anybody else’s. Because if you rest and if you take your medication like you’re supposed to you can be stable. But you have to take care of yourself… at first when this all started I was thinking that this was a really difficult situation. Because maybe I’d stay sick… But then I saw that this wasn’t the case… I saw that I could feel normal. (QI003: Participant living with HIV for 6 years)
Looking to Family, Friends, or Partners for Support
Nearly all women in this sample felt that they had adequate social support for living with HIV. While participants were careful to keep their HIV diagnosis a secret from some people, almost everyone (N = 15) reported that they had built up a network of supportive friends and family. One woman, who tested positive for HIV during her most recent pregnancy, described how her friends and family rallied around her after the birth of her daughter.
But I’m honestly not ashamed to have HIV… I have a daughter who is about to turn 12… she was the last child that I had because I got HIV… And after I gave birth, there were so many people at my house to bring me pills…bringing me teas… And I prayed for God to make my little girl healthy… and thanks be to God that my daughter was born HIV-negative. (QI011: Participant living with HIV for 12 years)
When asked to characterize the social support they received, participants revealed that acceptance of their HIV diagnosis, inclusion in social activities, being treated the same as before they were diagnosed, and feeling loved by people they care about, were important.
…My family has never rejected me. If you have enough love you can get through this. (QI001: Participant living with HIV for 10 years)
Normal. Everything is normal. Mami… My dad died 11 years ago and I didn’t have HIV. But my mom kept treating me the way she did before (QI008: Participant living with HIV for 7 years)
Everyone sends for me and brings me around… Well… when I was sick they supported me… Yeah. Everybody treats me well. They love me a lot. (QI007: Participant living with HIV for 7 years)
Discussion
All WLWHA interviewed as a part of this study successfully used stigma coping strategies. Overall, participants indicated that HIV-related stigma was the most severe when they found out about their HIV infection and lessened with time. This may be because over time, participants became more adept at deploying stigma coping strategies to reduce the effect of stigma. This is particularly significant from a clinical standpoint. Specifically, if mental health providers could help WLWHA execute stigma coping strategies sooner by helping them to understand what has worked for others, we could potentially lessen stigma and consequently, its negative behavioral and mental health effects. Little research exists about stigma coping strategies. However, findings from this study support existing knowledge about this topic and introduce new strategies. For instance, work with men and women living with HIV in sub-Saharan Africa found that stigma coping strategies include educating others about this disease, acquiring knowledge and understanding about HIV, improving social support networks, and putting their faith in God [28]. Additionally, other studies in sub-Saharan Africa [29], show that access to health services and HIV treatment play an important role in mitigating stigma.
In this study, stigma coping strategies included disclosure control; preemptive disclosure of HIV status; educating oneself and others about HIV; viewing HIV as a chronic and manageable condition; and looking to family, friends, or partners for support. Taken together, stigma coping strategies identified in this research show that improved participant control over various aspects of HIV disease effectively reduces internalized stigma. That is, when WLWHA are able to take charge of specific social and/or clinical domains of HIV such as disclosure, education, treatment, or support seeking, they are less likely to internalize negative narratives about themselves. For instance, some participants engaged in HIV disclosure control, which allowed them to monitor the spread of information about their HIV status. For the most part, these WLWHA were able to contain this knowledge to an accepting group of friends and family, and to avoid others who would react poorly. By doing this, respondents drastically limited the inflow of negative feedback about their HIV diagnosis, which likely helped to reduce internalized stigma. A positive relationship exists between perceived and internalized stigma [30], possibly explaining this result. That is, the more a person believes that others stigmatize him/her, the more likely that person is to agree with these stigmatizing messages. Through limiting the stigmatizing narratives from outsiders by disclosing only to supportive others, WLWHA were able to control the information they heard about people living with HIV.
Still, it is important to note that HIV disclosure control was complicated. While some participants reported that disclosing their HIV status to trusted friends, family, and partners resulted in increased social support, others reported that they did not feel stigmatized for living with HIV because nobody knows that they do. WLWHA in this study who did not disclose their HIV status to others, typically made this choice because they anticipated negative social outcomes, such as gossip about their HIV status and/or rejection by family or friends. Though we can only speculate, this particular case may represent a manifestation of internalized stigma, rather than a stigma coping strategy. Specifically, women who elect not to disclose their HIV-positive status to anybody may unconsciously agree with the biases against them, regardless of how they responded on the IA-RSS. This finding highlights the need for HIV clinicians to work closely with WLWHA to fully understand their life circumstances and to create disclosure plans that take into account the unique characteristics of their social and family networks. On a broader level, this finding points to the need to introduce community-level interventions to reduce HIV-related stigma.
Preemptive disclosure was also complex. Specifically, this stigma coping strategy had the capacity to both facilitate and undermine the control WLWHA had over information about their HIV status. This duality was particularly evident among participants who disclosed “involuntarily,” meaning that they disclosed their HIV status because they suspected it would be found out anyway. WLWHA who disclosed involuntarily simultaneously lost and regained control over this information because: [1] they were forced by some event (e.g., being visibly sick with symptoms of HIV) to disclose when they may not have otherwise (lost control), but [2] decided to reassert control by disclosing before other people could find out about their HIV diagnosis on their own (regained control). By disclosing their HIV status preemptively, WLWHA in this study were able to control when, how, and by whom disclosure targets learned about their HIV. Additionally, they were able to control how much information was shared and could respond to others’ questions and concerns. Taking this into account, preemptive disclosure, in the case where it is involuntary, may actually be a unique strategy to regain control over HIV information when WLWHA feel they have lost it because of events beyond their control. Therefore, when designing disclosure plans, it may be useful for clinicians to discuss with patients a contingency plan to prepare for the possibility that information about their HIV diagnosis may become difficult or impossible to contain.
Interviewees emphasized the importance of educating themselves, family members, and the community about HIV. Having an accurate understanding of this disease empowered WLWHA in this study to counter misconceptions about HIV with factual information. This was especially important in the case of myths about transmission. For instance, participants reported instances where they were forced to separate their eating utensils or were forbidden from sharing food with HIV-negative relatives because they believed the virus could be passed in this way. Respondents explained that learning about various aspects of HIV disease, including modes of exposure, lessened their own and others’ anxieties and prejudices. In this way, WLWHA were able to control: [1] the amount of stigma directed towards them by others, and [2] their own likelihood of internalizing shaming and blaming attitudes about people living with HIV.
Educational materials about HIV are widely available in the Dominican Republic, and the scale-up of community HIV education efforts is feasible. Participants reported using written outreach materials from CEPROSH, attending HIV-related education classes held in their neighborhoods, and having one-on-one peer-mentoring sessions with HIV-positive CEPROSH community leaders. WLWHA in this study reported sharing the information they learned with family members. Some participants even attended HIV education classes and/or peer-mentoring sessions with relatives. Expanding the reach of these programs could have the community-wide effect of reducing negative perceptions of people living with HIV and myths about how HIV is spread, thus reducing HIV-related stigma for people affected by this disease.
Understanding the treatment options available to HIV-positive people was a critically important part of HIV-related education. This study and others [29, 31] show that viewing HIV as a chronic and manageable condition, rather than a terminal illness, reduces the impact of HIV-related stigma. This may be because through learning about disease management, people living with HIV are able to take steps to reduce or control their symptoms; there is a strong relationship between experiencing active HIV symptomology and worse internalized stigma [25, 32]. Several interviewees reported feeling severely depressed about their HIV status until they understood that effective treatment is available. This finding has two clinical implications. First, people living with HIV in the Dominican Republic should be educated about treatment options and how to access them upon diagnosis with HIV. Second, community and family education about HIV should include a component that summarizes the available treatment options and emphasizes the possibility of living a long, healthy life with this disease if patients adhere to treatment. CEPROSH and clinics that have a relationship with CEPROSH discuss these themes with newly diagnosed patients already. However, given the fragmented nature of HIV treatment and care in the Dominican Republic, it is highly unlikely that this practice is widespread, particularly in rural areas. Access to antiretroviral (ART) medication is better in the Dominican Republic than in many other places and community-based organizations that serve people living with HIV exist in multiple regions of the country. Therefore, initiatives to improve collaboration between local providers and HIV clinics could drastically expand ART access and subsequently reduce HIV-related stigma.
Participants discussed the importance of looking to family, friends, or partners for support as a way to cope with HIV-related stigma. This may be an especially important stigma coping strategy for women, since they rely on their relationships with others more than men do in similar situations [33]. This stigma coping strategy is highly related to disclosure control, since in order to gain social support, stigmatized individuals must select accepting others to disclose to. Healthy social support networks buffer stigmatized individuals from the daily stressors and devaluations associated with their stigmatizing identities [34] and may limit the inflow of negative rhetoric about their stigmatizing trait. For this reason, clinicians and public health workers recommend HIV disclosure as a way to reduce HIV-related stigma. However, it is noteworthy that not all WLWHA in this study had friends or relatives that they felt would be supportive. In this case, patients’ relationships with their provider may be especially important and support groups for HIV-positive people could help to fill this void.
Limitations
This study had limitations. First, only women engaged in treatment were included in the sample, potentially biasing results. This is especially true, since women in this sample may represent a more mobilized group than what is typical of WLWHA in the general population. Furthermore, all participants in this study had children. Though we can only speculate, motherhood, in this context, may confer additional social support from other family members or from adult children. This, in turn, may have improved how women in this sample coped with internalized stigma, compared with childless women. No women who reported any degree of internalized stigma on the IA-RSS were interviewed about stigma coping strategies. Therefore, it is impossible to determine if these strategies are unique to women who do not experience internalized stigma, which is a limitation. Lastly, some women in this sample have lived with HIV for a decade or more. In this case, it is possible that stigma coping strategies alone did not account for their lack of self-reported internalized stigma. Advances in HIV care, amount of time living with HIV, and changing public perceptions of HIV may have contributed also to their ability to resist stigma.
Conclusions
More cross-cultural study of the stigma coping strategies employed by WLWHA is needed. Broader inquiry would yield a greater volume of culturally contextualized stigma-reducing strategies to be engaged by HIV-positive women. All stigma reduction strategies in this research facilitated greater control of various domains of respondents’ HIV disease, such as disclosure, education, treatment, and social support seeking. Presenting WLWHA with these strategies early on could potentially help to reduce internalized stigma and the associated mental and behavioral health outcomes by limiting the stigma they perceive from others and building the capacity to reject misconceptions about HIV. However, it is important for providers to contextualize stigma coping strategies to the unique needs of individuals. Individual-level interventions to help WLWHA implement stigma coping strategies are in no way a substitute for large-scale efforts to address HIV-related stigma in the community. Findings from this paper are meant to compliment these larger strategies, not replace them, since widespread prejudice against HIV-positive people remains the primary driver for the challenges this paper aims to address.
References
LaVeist TA, Rolley NC, Chamberlain D. Prevalence and patterns of discrimination among U.S. health care consumers. Int J Health Serv. 2003;33(2):331–44.
Liu SH, Srikrishnan AK, Zelaya CE, Solomon S, Celentano DD, Sherman SG. Measuring perceived stigma in female sex workers in Chennai, India. AIDS Care. 2011;23(5):619–27.
Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc Sci Med. 2003;57(1):13–24.
Sayles JN, Wong MD, Kinsler JJ, Martins D, Cunningham WE. The association of stigma with self-reported access to medical care and antiretroviral therapy adherence in persons living with HIV/AIDS. J Gen Intern Med. 2009;24(10):1101–8.
Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc. 2013;16(3 Suppl 2):18640.
Preston DB, D’Augelli AR, Kassab CD, Cain RE, Schulze FW, Starks MT. The influence of stigma on the sexual risk behavior of rural men who have sex with men. AIDS Educ Prev. 2004;16(4):291–303.
Pitpitan EV, Kalichman SC, Eaton LA, Cain D, Sikkema KJ, Skinner D, et al. AIDS-related stigma, HIV testing, and transmission risk among patrons of informal drinking places in Cape Town, South Africa. Ann Behav Med. 2012;43(3):362–71.
Reid AE, Dovidio JF, Ballester E, Johnson BT. HIV prevention interventions to reduce sexual risk for African Americans: the influence of community-level stigma and psychological processes. Soc Sci Med. 2014;103:118–25.
Goffman E. Stigma: notes on the management of spoiled identity. New York: Simon and Schuster Inc; 1963.
Scambler G, Paoli F. Health work, female sex workers, and HIV/AIDS: Global and local dimensions of stigma and deviance as barriers to effective interventions. Soc Sci Med. 2008;66(8):1848–62.
Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav. 2013;17(5):1785–95.
Li L, Lee SJ, Thammawijaya P, Jiraphongsa C, Rotheram-Borus MJ. Stigma, social support, and depression among people living with HIV in Thailand. AIDS Care. 2009;21(8):1007–13.
Rael CT, Davis A. Depression and key associated factors in female sex workers and women living with HIV/AIDS in the Dominican Republic. Int J STD AIDS. 2016.
Dlamini PS, Wantland D, Makoae LN, Chirwa M, Kohi TW, Greeff M, et al. HIV stigma and missed medications in HIV-positive people in five African countries. AIDS Patient Care STDS. 2009;23(5):377–87.
DeLonga KTH, Kamen C, et al. Loneliness, internalized homophobia, and compulsive internet use: factors associated with sexual risk behavior among a sample of adolescent males seeking services at a community LGBT center. Sex Addict Compulsivity. 2011;18(2):61–74.
Shamos S, Hartwig KA, Zindela N. Men’s and women’s experiences with HIV and stigma in Swaziland. Qual Health Res. 2009;19(12):1678–89.
Castro A, Farmer P. Understanding and addressing AIDS-related stigma: from anthropological theory to clinical practice in Haiti. Am J Public Health. 2005;95(1):53–9.
Lambert V. Gender assessment: USAID/Dominican Republic. USAID; 2009.
USAID. HIV/AIDS health profile: Caribbean. 2011.
Middleton-Lee S, Shepard J. Piecing it together for women and girls: the gender dimensions of HIV-related stigma: evidence from Bangladesh, The Dominican Republic, and Ethiopia. London: Inernational Planned Parenthood Federation; 2011.
Rojas P, Malow R, Ruffin B, Rothe EM, Rosenberg R. The HIV/AIDS Epidemic in the Dominican Republic: key contributing factors. J Int Assoc Physicians AIDS Care (Chic). 2011;10(5):306–15.
Cáceres Ureña FI. República Dominicana: Estigma y discriminación en personas que viven con el VIH. Santo Domingo, República Dominicana: Asociación Dominicana Pro Bienestar de la Familia (Profamilia) y Instituto de Estudios de Población y Desarrollo (IEPD); 2009.
Julian ZBB. Informe nacional sobre los avances en la respuesta al SIDA: Seguimiento a la declaración política de las Naciones Unidas sobre el VIH y el SIDA, 2011. Santo Domingo de Guzmán, Districto Nacional República Dominicana; 2014
Perdomo AH. Centro de Promoción y Solidaridad Humana Puerto Plata, República Dominicana2012 [Available from: ceproshinc.org.
Kalichman SC, Simbayi LC, Cloete A, Mthembu PP, Mkhonta RN, Ginindza T. Measuring AIDS stigmas in people living with HIV/AIDS: the Internalized AIDS-Related Stigma Scale. AIDS Care. 2009;21(1):87–93.
Corbin J, Strauss A. Basics of Qualitative Research. 4th ed. Thousand Oaks: SAGE Publications Ltd; 2015.
Thomas DR. A general inductive approach for analyzing qualitative evaluation data. Am J Eval. 2006;27(2):237–46.
Makoae LN, Greeff M, Phetlhu RD, Uys LR, Naidoo JR, Kohi TW, et al. Coping with HIV-related stigma in five African countries. J Assoc Nurses AIDS Care. 2008;19(2):137–46.
Campbell C, Skovdak M, Madanhire C, Mugurungi O, Gregson S, Nyamukapa C. “We the AIDS people…”: How antiretroviral therapy enables Zimbabweans living with AIDS to cope with stigma. Am J Public Health. 2011;101(6):1004–10.
Rael CT, Hampanda K. Understanding internalized HIV/AIDS-related stigmas in the Dominican Republic: a short report. AIDS Care. 2016;28(3):319–24.
Zuch M, Lurie M. ‘A virus and nothing else’: the effect of ART on HIV related stigma in rural South Africa. AIDS Behav. 2012;16(3):564–70.
Holzemer WL, Uys LR, Chirwa ML, Greeff M, Makoae LN, Kohi TW, et al. Validation of the HIV/AIDS Stigma Instrument–PLWA (HASI-P). AIDS Care. 2007;19(8):1002–12.
Hurdle DE. Social support: a critical factor in women’s health and health promotion. Health Soc Work. 2001;26(2):72–9.
Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–97.
Acknowledgements
Data collection support was provided by Maria del Rosario Martínez-Muñoz and Yasmín Soto. Special thanks to CEPROSH and Grupo Clara, who provided the local infrastructure for outreach and study subject recruitment. Research design and project development was supported by the dissertation committee: Drs. David Tracer, Jean Scandlyn, John Brett, and Richard Miech at the University of Colorado-Denver. Grammatical editing was provided by Tim Frasca.
Funding
This project was supported by a Fulbright Program grant sponsored by the Bureau of Educational and Cultural Affairs of the United States Department of State and administered by the Institute of International Education. All affiliated research was conducted with the University of Colorado-Denver. The first author is now supported by a training grant (T32 MH019139; Principal Investigator, Theodorus Sandfort, Ph.D.) from the National Institute of Mental Health at the HIV Center for Clinical and Behavioral Studies at the NY State Psychiatric Institute and Columbia University (P30-MH43520; Center Principal Investigator: Robert Remien, Ph.D.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical Standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Rael, C.T., Carballo-Diéguez, A., Norton, R. et al. Identifying Strategies to Cope with HIV-Related Stigma in a Group of Women Living with HIV/AIDS in the Dominican Republic: A Qualitative Study. AIDS Behav 21, 2589–2599 (2017). https://doi.org/10.1007/s10461-016-1654-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-016-1654-9