Abstract
This study assessed the prevalence of exchanging sex for money or drugs among men who have sex with men (MSM) in the 2011 US National HIV Behavioral Surveillance system. Prevalence of HIV, being HIV-positive but unaware (HIV-positive–unaware), risk behaviors and use of services were compared between MSM who did and did not receive money or drugs from one or more casual male partners in exchange for oral or anal sex in the past 12 months. Among 8411 MSM, 7.0 % exchanged sex. MSM who exchanged sex were more likely to be non-Hispanic black, live in poverty, have injected drugs, have multiple condomless anal sex partners, be HIV-positive and be HIV-positive–unaware. In multivariable analysis, exchange sex was associated with being HIV-positive–unaware (aPR 1.34, 95 % CI 1.05–1.69) after adjusting for race/ethnicity, age, education, poverty, and injecting drugs. MSM who exchange sex represent an important group to reach with HIV prevention, testing, and care services as they were more likely to report behavioral risk factors that put them at risk of HIV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Male to male sexual contact accounted for 66 % of the 44,784 estimated new HIV diagnoses in the United States in 2014 [1]. The number of newly diagnosed HIV infections annually attributed to male-to-male sexual contact increased between 2010 and 2014 in contrast to the trends observed in diagnoses attributed to injection drug use, male-to-male sexual contact and injection drug use, or heterosexual contact, which declined [1]. In 2011, 18 % of men who have sex with men (MSM) sampled in the United States National HIV Behavioral Surveillance (NHBS) system tested positive for HIV, 44 % of whom were unaware of their infection (HIV-positive–unaware) [2].
Exchange sex–sex in exchange for money or drugs—has been shown to play a key role in HIV transmission among heterosexual populations in many countries [3]. Among MSM, a recent systematic review documented that an association between exchange sex and higher risk of HIV infection has been reported in several parts of the world [4]. There are several factors associated with exchange sex that increase the risk for HIV acquisition, such as large numbers of partners and sex without a condom, as shown by studies on male sex workers [4–6]. Condom use may be difficult to negotiate if offered additional money to not use a condom when men are in a position of drug dependency or economic hardship [4, 7]. Sexually transmitted diseases (STDs) are prevalent among those who exchange sex [4, 8], and may increase the risk for HIV transmission and acquisition [9]. Furthermore, several studies in the US and Australia have shown both injection and non-injection drug use to be more common among MSM who exchange sex compared to those who do not [5, 6, 10, 11], behaviors that are associated with sexual disinhibition and an increased risk of HIV acquisition [12, 13]. Several socioeconomic factors that are associated with a higher risk of HIV infection are also more common among MSM who sell sex, such as poverty, unemployment, having less than a high school education, being homeless, and having unstable housing [6, 11, 14–16]. Finally, MSM who exchange sex may face stigma and marginalization associated both with being a man who has sex with other men, and engaging in an illegal activity. Such stigma may prevent them from accessing HIV prevention and other services [4].
Studies on MSM who exchange sex in Canada are more recent and not limited to high-risk MSM, compared to those in the US: Among MSM recruited using venue-based sampling in Ontario, Canada, 7 % reported receiving money and 5 % reported receiving drugs and non-monetary items in exchange for sex in the past 12 months, and exchange sex was associated with an increased prevalence of HIV infection [17]. A prospective cohort study of young MSM 18–30 years of age in Vancouver found that 16 % of MSM exchanged sex, and that both HIV prevalence at baseline as well as HIV incidence were significantly higher among those who exchanged sex (7.3 vs. 1.1 % for prevalence and 4.7/100 vs. 0.9/100 person-years for incidence) [6].
Data on exchange sex among MSM in the US are mostly limited to local studies in high-risk sub-populations such as drug using, homeless and marginally housed, and unemployed MSM, which limits their generalizability. Newman et al., recruiting MSM through street based outreach, snowball sampling and flyers at social service agencies in Long Beach, California, found that 63 % had exchanged sex for money, drugs or shelter/food in the past 30 days [11]. Robertson et al., using a probability sample of men from shelters, meal programs and low cost hotels found that 50 % had a lifetime history of sex in exchange for money or drugs [16]. The gender of the exchange partners was not specified in either of these two studies. Another study, using peer outreach in high-risk neighborhoods in San Francisco, found that 68 % of MSM had a lifetime history of exchange sex for money or drugs with a male partner [18], and a study using respondent driven sampling, largely of men of low income, who used drugs, were unemployed, homeless, and with a history of incarceration, found that 18–34 % received money or drugs in exchange for sex with one of three recent male partners [19]. Among single and non-monogamous sexually active MSM recruited at community events in New York City, 37 % had a lifetime history of having been paid for sex, and 27 % had both paid and been paid for sex [20]. These studies were all cross sectional.
Some of these studies found that HIV prevalence was higher among men who reported exchanging sex [16, 18], although in one study this was only the case for MSM with more than ten lifetime exchange partners [18]. These, and two other studies which only include MSM who exchange sex without a comparison group, reported an HIV prevalence among those who exchanged sex between 14 and 41 % [7, 16, 18, 21]. Studies that look beyond high-risk sub-populations of MSM in the US are outdated: in a 1998 cross-sectional study recruiting MSM from venues in Denver, Colorado and Long Beach, California, nine percent reported exchange of sex for money or drugs in the past 6 months [5].
People who are HIV-positive–unaware have been shown to be more likely to engage in behaviors that put their sexual partners at risk of acquiring HIV, compared to those aware of being HIV-positive [22]. However, there are very few data on the prevalence of being HIV-positive–unaware among MSM who exchange sex and on how prevalent exchange sex is among MSM.
Mathematical modeling in other settings has shown that female sex workers play a key role in driving heterosexual epidemics [23–26]. In Vietnam, it was estimated that annual HIV testing and immediate treatment of female sex workers would prevent 31 % of new infections over 40 years [27]. Similar modeling studies on male sex workers are rare as data on this population is also scarce [3], but a study from Peru estimated that by providing pre-exposure prophylaxis (PrEP) to 20 % of male sex workers, 3.4 % of infections over 10 years in the MSM population could be averted [28]. MSM who exchange sex may also play a key role in transmission in the United States, but the lack of data on MSM who exchange sex limits our potential to explore this further.
NHBS monitors HIV prevalence and associated HIV risk behaviors in 20 US cities by conducting surveys and HIV testing in populations at high risk of HIV infection, including MSM [29]. We used data from the 2011 NHBS cycle among MSM to determine the prevalence of exchange sex, describe the characteristics of MSM who exchange sex including risk behaviors and HIV testing frequency, and determine whether exchange sex is associated with two different outcomes: HIV prevalence and prevalence of being HIV-positive–unaware.
Methods
Study Population and Data Collection
In 2011, NHBS staff in 20 US metropolitan statistical areas (MSAs) recruited MSM using venue-based sampling (VBS) for interviews and HIV testing. The VBS procedures used in NHBS have previously been described [30, 31]. Briefly, NHBS staff first identified venues where MSM congregate and socialize (e.g., bars, social organizations, and sex venues) and where at least 50 % of the attending men were eligible to participate in NHBS. Men were eligible to participate if they had not previously participated in 2011, were at least 18 years of age, reported having ever had oral or anal sex with another man, were residents of the MSA, were able to complete the survey in English or Spanish, and were able to provide informed consent. Venues and corresponding day/time periods were chosen randomly each month for recruitment events. Trained interviewers conducted anonymous face-to-face interviews using a standardized questionnaire covering demographics, HIV-associated behaviors, and use of prevention and testing services. HIV testing was performed by collecting blood or oral specimens for either rapid testing in the field or laboratory-based testing. Both rapid and laboratory based screening tests were followed by confirmatory laboratory testing (e.g., Western blot, immunofluorescence assay, or nucleic acid amplification test) [32–34]. Participants received incentives for participating in the interview (typically $25) and for taking an HIV test (typically $25). The incentive format (cash or gift card) and amount varied by city based on formative assessment and local policy.
Measures
We examined two main outcomes: HIV prevalence and being HIV-positive–unaware. A nonreactive rapid test was considered a definitive negative result. MSM were considered to be HIV-positive if they had a laboratory-confirmed positive HIV test result. HIV-positive MSM who did not report having previously tested positive for HIV were considered to be HIV-positive–unaware.
Engaging in exchange sex was the main explanatory variable of interest. Participants who reported one or more male oral or anal casual sex partner(s) in the past 12 months from whom they received ‘things like money or drugs in exchange for sex’ were defined as engaging in exchange sex. A casual partner was defined during the interview as ‘a man you have sex with but do not feel committed to or don’t know very well’. A main partner was defined during the interview as ‘a man you have sex with and who you feel committed to above anyone else. This is a partner you would call your boyfriend, husband, significant other, or life partner’.
Exchange sex was used as a dichotomous variable in the analysis. The focus of this analysis was on MSM who received money or drugs from casual partners in exchange for sex, thus participants who reported receiving money or drugs in exchange for sex only from main partners were considered as not having exchanged sex in the past 12 months (n = 95) and were included in the reference category. Finally, those who only reported giving things like money or drugs in exchange for sex with casual partners (n = 249) were also categorized as not having exchanged sex for the purposes of this analysis and were included in the reference category, as the aim of our analysis was to examine the HIV risk among those who sell sex to casual partners, relative to all other MSM. Prevalence of STDs were measured by asking participants whether in the past 12 months a health care provider had told them that they had gonorrhea, chlamydia, syphilis or some other STD (except HIV).
Analysis of Prevalence and Correlates of Exchange Sex
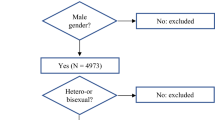
Analyses were limited to data from participants who completed the interview, reported at least one male sex partner in the past 12 months, and had a positive or negative HIV test result. First, we determined the prevalence of exchange sex in the sample, and compared the prevalence of exchange sex by different sociodemographic characteristics. Second, we compared the prevalence of substance abuse, sexual risk behaviors, and use of services between participants who reported exchange sex in the past 12 months and those who did not. Chi square analysis was used to determine statistically significant differences (p < 0.05) between categorical variables. Fisher’s exact test was used for small cell sizes. For continuous variables we used a Poisson model with robust standard error to test for differences in means and a nonparametric exact test for differences in medians. When determining the prevalence of HIV testing within the past year, we excluded MSM who self-reported being HIV-positive during the interview, unless they had their first positive HIV test within the last 12 months.
Analysis of Association Between Exchange Sex and HIV Prevalence
We examined the bivariable and multivariable associations between different variables, including exchange sex, and HIV prevalence as the outcome. Race/ethnicity and lifetime history of injection drug use were considered a priori as confounders based on previous research and included in the multivariable model.
Analysis of Association Between Exchange Sex and HIV-Positive–Unaware
Excluding self-reported HIV-positive participants (n = 1031), we examined the bivariable and multivariable associations between different variables, including exchange sex, and being HIV-positive but unaware of one’s infection. Age, race/ethnicity and lifetime history of injection drug use were considered a priori as confounders and included in the multivariable model. We included additional variables that were significant in bivariable analysis, but removed those with a p value of ≥0.05 in multivariable analysis. To account for income we kept poverty in the final model [4]. We also tested for two-way interactions between exchange sex and each of the covariates in the final model but as these were not significant (all had p > 0.1) they were not included in the final model. In further analyses, to evaluate if there was an association between exchange sex and being HIV-positive–unaware that could not be explained by a larger number of casual partners, we introduced total number of condomless casual anal sex partners in the past 12 months as a continuous variable in the model. We conducted sensitivity analysis to evaluate if excluding men who only paid for sex (gave money or drugs in exchange for sex to casual partners) from the reference category changed the model results.
All analyses were done in SAS v9.2. To account for some of the methodological complexities associated with VBS sampling across multiple cities, in calculating both adjusted and unadjusted prevalence ratios we used generalized estimating equations (GEE), using a Poisson model with a robust standard error in PROC GENMOD [35], clustered on recruitment event (the lowest level of clustering in our data) to account for the general dependence in observations. In addition, we adjusted for the multi-city nature of the study by including an indicator variable for city in multivariable modeling. Unadjusted and adjusted prevalence ratios (PR and aPR) and 95 % confidence intervals (CI) are reported. PRs were chosen because they are a direct measure of risk compared to odds ratios that measure an increase in odds. This allows for ease in interpretation.
Ethics
Verbal informed consent was obtained from all participants. Activities for NHBS were approved by local institutional review boards (IRB) for each of the 20 participating cities. NHBS activities were determined to be research in which the Centers for Disease Control and Prevention (CDC) was not directly engaged and, therefore, did not require review by CDC IRB.
Results
In total, 8460 eligible, consenting MSM completed the survey, had a positive or negative HIV test result and reported oral or anal sex with another man in the past 12 months. We excluded 49 participants who had missing data on exchange sex, or who self-reported being HIV-positive but who tested negative.
Analysis of Prevalence and Correlates of Exchange Sex
Of 8411 MSM included in this analysis, 585 (7.0 %) reported exchange sex in the past 12 months (Table 1), with city-specific sample estimates ranging from 1.5 % in San Juan to 20.8 % in Baltimore. Among MSM who exchanged sex, 187 (32.0 %) had one exchange partner and 109 (18.6 %) had ten or more exchange partners in the previous 12 months. Exchange sex was more common among MSM who were black (11.0 %) compared to white (5.1 %) and Hispanic (6.2 %) (p < 0.001, Table 1). Education level was associated with exchange sex with 25.3 % of those with less than a high school education reporting exchange sex, compared to 2.3 % of MSM with college or postgraduate education. Exchange sex was also more common among MSM who were not employed (13.0 vs. 4.4 % for those employed), homeless (31.3 vs. 4.8 % for those not homeless), lived in poverty (15.0 vs. 4.9 % among those not living in poverty), had a lifetime history of incarceration (19.1 vs. 3.5 % for those never incarcerated), and who identified as heterosexual or bisexual (16.3 vs. 4.9 % among those identifying as homosexual).
Compared to those who did not exchange sex, MSM who exchanged sex had a higher number of male and female oral, anal or vaginal partners (mean of 19.4 vs. 8.6, p < 0.001) as well as male condomless anal sex partners (main and casual) in the past 12 months (mean of 4.3 vs. 1.8, p < 0.001) (Table 2). MSM who exchanged sex were more likely to report unprotected vaginal or anal sex with both main and casual female partners in the past 12 months (13.5 vs. 3.5 %, p < 0.001 for main; 19.0 vs. 3.6 % for casual, p < 0.001). Among men who exchanged, 30 % said their last female partner was a main partner, 54 % a casual partner and 15 % an exchange partner.
Among MSM who exchanged sex, the most recent male partner appeared to be riskier than the most recent partner of MSM who did not exchange sex; they were more likely to be of unknown HIV status (60.7 vs. 37.5 %, p < 0.001), and ‘definitely’ or ‘probably’ had ever injected drugs according to the participant (19.7 vs. 7.4 %, p < 0.001). Drug use was more common among MSM who exchanged sex, including a lifetime history of injection drug use (22.6 vs. 5.4 %, p < 0.001), and use of non-injection crack cocaine (26.7 vs. 3.2 %, p < 0.001), and methamphetamine (24.2 vs. 5.3 %, p < 0.001) in the past 12 months. There was no difference in the proportion that had had an HIV test in the past 12 months between MSM who did and did not exchange sex (65.6 vs. 66.9 %, p = 0.54). A total of 20.5 % of MSM who exchanged sex had heard about PrEP or post-exposure prophylaxis (PEP) compared to 26.1 % among those who do not exchange (p = 0.006).
Analysis of Association Between Exchange Sex and HIV Prevalence
In total, 29.1 % of men who exchanged sex tested positive for HIV, compared to 17.7 % of men who did not exchange sex in the past 12 months (p < 0.001, Table 2). This association did not remain statistically significant when controlling for race/ethnicity, having ever injected drugs and city of interview (aPR 1.13, 95 % CI 0.98–1.31, p = 0.090).
Analysis of Association Between Exchange Sex and HIV-Positive–Unaware
Among MSM who exchanged sex, 13.2 % were HIV-positive–unaware, compared to 5.6 % among men who did not report exchange sex (Table 2). During bivariable and multivariable analysis, participants who were HIV-positive and aware of their status were excluded. In bivariable analysis, exchange sex was associated with being HIV-positive–unaware (PR 2.16, 95 % CI 1.68–2.77) (Table 3). In multivariable analysis controlling for age, race/ethnicity, education, poverty, lifetime injection drug use and city of interview (Table 3), exchange sex remained associated with being HIV-positive–unaware (aPR 1.34, 95 % CI 1.05–1.69). When the number of casual male condomless anal sex partners in the past 12 months was added to the final model, the association between exchange sex and being HIV-positive–unaware remained statistically significant (aPR 1.30 95 % CI 1.03–1.65, data not shown in tables). In sensitivity analysis we found that excluding those who only gave money or drugs in exchange for sex to casual partners from the reference group did not change the model results.
Discussion
Using data from NHBS, the largest existing study of MSM in the United States with more than 8000 MSM from 20 cities, we found that 7.0 % reported receiving things like money or drugs in exchange for sex with casual partners in the previous 12 months, although the prevalence of exchange sex did vary substantially between cities (range 1.5 % in San Juan to 20.8 % in Baltimore). This prevalence is similar to what was found in a sample recruited through venue-based sampling in Canada [17]. A key finding of this analysis is the high HIV prevalence among MSM who exchange sex (29.1 %) and the high proportion who were HIV-positive and unaware of their HIV infection (13.2 %). Exchange sex was associated with a greater than 30 % increase in the risk of being HIV-positive–unaware in multivariable analysis.
Due to the high HIV prevalence in this group, MSM who exchange sex are at high risk for transmitting HIV to their exchange and non-exchange partners. Consistent with other studies, our findings indicate that, compared to MSM who do not exchange sex, MSM who exchange sex are more likely to have multiple partners, including anal sex partners with whom they do not use a condom, as well as female partners [5–7, 10]. The proportion of MSM who exchange sex who reported having been told by a health care provider that they had an STD in the past 12 months was also high in this study (17.3 %) and STDs are known to increase the risk for HIV transmission [36, 37]. For these reasons, MSM who exchange sex may play an important role in the HIV epidemic, in particular in the cities where a high proportion of study participants reported exchanging sex, such as Baltimore where over a fifth of MSM exchanged sex.
MSM who exchange sex are also at high risk for acquiring HIV by having multiple condomless anal sex partners and high prevalence of STDs and drug use. Use of non-injection drugs such as methamphetamine and crack, which have been shown to be associated with HIV seroconversion [38] were commonly reported in this population. Injection drug use was also more prevalent and contributes to the risk of HIV acquisition through sharing of injection equipment; 4.7 % of MSM who exchanged sex reported receptive sharing of syringes. Furthermore, our analyses suggest that exchange sex may increase the risk of HIV not only due to having high numbers of partners, but also due to having higher risk partners. We found that partners of MSM who exchange sex were more likely to be of unknown HIV status and inject drugs, and the association between exchange sex and being HIV-positive–unaware remained significant after controlling for the number of condomless casual anal sex partners in the past 12 months. The combination of these factors (drug use, high number of condomless sex partners, and risky sex partners) could potentially lead to an increased risk for HIV acquisition among MSM who exchange sex.
Although the association between exchange sex and HIV-positive–unaware was significant, we found no association between exchange sex and HIV-prevalence in multivariable analysis. One possible explanation could be that MSM who exchange sex and are diagnosed with HIV cease exchanging sex, consistent with previous data that show people who are aware of being HIV-positive modify their risk behaviors after learning about their status [22]. MSM who recently started exchange sex, may have lower HIV prevalence, and population turnover could lead to an under-estimate of the true burden of HIV among MSM who exchange sex [3]. We are however unable to verify this, as respondents were only asked about exchange sex in the past 12 months. It could also be possible that some participants who were diagnosed with HIV before the interview, misreport their status due to fear of stigma or concerns about negative consequences. This may be more common among MSM who exchange sex because recognizing one’s HIV-positive status may result in having to stop exchanging sex.
As MSM who exchange sex are at risk of both HIV acquisition and transmission, HIV prevention efforts should consider strengthening a variety of interventions in this population. The high prevalence of HIV, in particular HIV-positive–unaware, suggest that this population would benefit from increased access to and frequency of HIV testing in order to initiate early HIV care and treatment [39]. Counseling and partner notification services for MSM who exchange sex should ensure both male and female exchange and non-exchange partners are considered. Current CDC HIV testing guidelines recommend that persons at high risk for HIV infection, which include persons who exchange sex for money or drugs, get tested for HIV every 12 months [39]. But our data show that only two-thirds of MSM who exchange sex follow these recommendations. We found no difference in the proportion of MSM who had tested for HIV in the past 12 months between those who did and did not exchange sex, yet MSM who exchanged sex were more likely to be HIV-positive–unaware. This suggests the importance to all MSM who exchange sex of testing for HIV at least annually. HIV testing in venues where MSM socialize may be one strategy for reaching MSM who exchange sex. Finding ways to reach and offer testing to MSM who sell sex online would also be important, since many men solicit clients online and there are reports of an increased online market for sex [40–42]. Additionally, health care providers can create a trusting and confidential environment for discussing sex, and should ask gay and bisexual men directly about their behaviors and provide recommendations for how they can reduce the risk of getting HIV or transmitting it to others. Linkage to and retention in care are essential for HIV-positive MSM, to address the health needs of those living with HIV and to prevent onward transmission through treatment and viral suppression.
MSM who exchange sex could be offered PrEP, as they are clearly a group at increased risk of HIV infection [4, 43]. A modeling study from Lima, Peru estimated that providing PrEP only to 20 % of male sex workers could avert 3.4 % of new HIV infections over 10 years in the MSM population. Providing PrEP to male sex workers and trans women was found to have higher impact for the same cost compared to providing PrEP to MSM in general [28]. Based on current US federal guidelines [44], people who are at ongoing substantial risk of acquiring HIV should be offered PrEP, including MSM who have had anal sex without a condom or been diagnosed with an STD in the past 6 months. Substance abuse treatment services may also help some MSM [11, 41] since we found a high prevalence of injection and non-injection drug use in our sample.
Our findings are largely consistent with existing data showing that MSM who exchange sex are more likely to be affected by poverty, low educational attainment, homelessness, previous incarceration, and drug use [4, 6, 11]. These observations highlight the importance of understanding how individual-level risks can be influenced by higher-order determinants at different levels [45]. Examples include laws and policies that influence resource allocation, including employment, educational opportunities and provision of services that may affect individual-level HIV risks. Community-level factors such as social norms and values, discrimination or the presence of stigma may also be important as these can act to marginalize MSM who exchange sex and prevent them from accessing HIV prevention and care services [4, 41, 45]. Interventions that only target individual-level risks may therefore have limited impact unless they are delivered as a combination of measures that address the different levels of HIV risk and also target the social determinants of health. Such interventions could range from help with employment readiness, educational attainment, housing and legal assistance, mental health services, and interventions against stigma and discrimination. Services should also not have an exclusive focus on gay men as many MSM who exchange sex identify as bisexual or straight [4, 11]. Prostitution is illegal in most US states and services for male sex workers are likely scant or non-existent [4].
The analysis presented here is subject to several limitations. First, because of the sensitive nature of HIV status, some participants who had been diagnosed with HIV infection before the NHBS interview may not have reported their positive HIV status. This may have resulted in over-estimating the number of MSM who are unaware of their infection, and could result in bias if such under-reporting was associated with exchange sex. Reporting on exchange partners is also a sensitive issue and participants may have chosen to not disclose having had exchange partners, leading us to underestimate the prevalence of exchange sex and potentially biasing the association between exchange sex and HIV towards the null. Second, this analysis is cross-sectional and causality may not be inferred. Third, there may be residual confounding that we were not able to measure and control for, such as social disadvantage that both increases HIV risk and force people to exchange sex, although we did attempt to account for this by including poverty and education in the final model. Other potential confounders could include personality traits such as risk taking and sensation seeking, which may be associated both with exchange sex and HIV risk [46, 47]. Fourth, MSM were recruited in cities with high AIDS burden and results may not be generalizable to all cities or all MSM. In addition, the survey population is limited to MSM who attend venues; MSM who do not attend venues may, or may not, differ from the survey population on key outcomes. Fifth, data are not weighted to account for the complex sampling methodology used to recruit MSM. Point estimates may therefore be biased by over- or under-represented subgroups of the population. (VBS sampling weights are currently under development for future NHBS data collection cycles). Finally, MSM who exchanged only with main partners were included in the reference category, which may have biased our results towards the null.
Conclusion
Seven percent of MSM in this sample from 20 cities across the United States had received money or drugs from a causal partner in exchange for sex in the past 12 months and those who exchanged sex had a higher prevalence of being HIV-positive and unaware of their infection. MSM who exchange sex could be a particularly important group for a variety of HIV prevention efforts in order to help prevent those who sell sex from acquiring HIV, to care for those already infected, and to prevent onward transmission to clients and non-paying male and female partners [4].
References
Centers for Disease Control and Prevention. HIV Surveillance Report, 2014. 2015.
Wejnert C, Le B, Rose CE, Oster AM, Smith AJ, Zhu J, et al. HIV infection and awareness among men who have sex with men-20 cities, United States, 2008 and 2011. PLoS One. 2013;8(10):e76878.
Pruss-Ustun A, Wolf J, Driscoll T, Degenhardt L, Neira M, Calleja JM. HIV due to female sex work: regional and global estimates. PLoS One. 2013;8(5):e63476.
Baral SD, Friedman MR, Geibel S, Rebe K, Bozhinov B, Diouf D, et al. Male sex workers: practices, contexts, and vulnerabilities for HIV acquisition and transmission. Lancet. 2014;385:260–73.
Rietmeijer CA, Wolitski RJ, Fishbein M, Corby NH, Cohn DL. Sex hustling, injection drug use, and non-gay identification by men who have sex with men. Associations with high-risk sexual behaviors and condom use. Sex Transm Dis. 1998;25(7):353–60.
Weber AE, Craib KJ, Chan K, Martindale S, Miller ML, Schechter MT, et al. Sex trade involvement and rates of human immunodeficiency virus positivity among young gay and bisexual men. Int J Epidemiol. 2001;30(6):1449–54.
Mimiaga MJ, Reisner SL, Tinsley JP, Mayer KH, Safren SA. Street workers and internet escorts: contextual and psychosocial factors surrounding HIV risk behavior among men who engage in sex work with other men. J Urban Health. 2009;86(1):54–66.
Mor Z, Shohat T, Goor Y, Dan M. Risk behaviors and sexually transmitted diseases in gay and heterosexual men attending an STD clinic in Tel Aviv, Israel: a cross-sectional study. Isr Med Assoc J. 2012;14(3):147–51.
Ward H, Ronn M. Contribution of sexually transmitted infections to the sexual transmission of HIV. Curr Opin HIV AIDS. 2010;5(4):305–10.
Estcourt CS, Marks C, Rohrsheim R, Johnson AM, Donovan B, Mindel A. HIV, sexually transmitted infections, and risk behaviours in male commercial sex workers in Sydney. Sex Transm Infect. 2000;76(4):294–8.
Newman PA, Rhodes F, Weiss RE. Correlates of sex trading among drug-using men who have sex with men. Am J Public Health. 2004;94(11):1998–2003.
Mathers BM, Degenhardt L, Phillips B, Wiessing L, Hickman M, Strathdee SA, et al. Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. Lancet. 2008;372(9651):1733–45.
Melendez-Torres G, Bourne A. Illicit drug use and its association with sexual risk behaviour among MSM: more questions than answers? Curr Opin Infect Dis. 2016;29(1):58–63.
Datta SD, Sternberg M, Johnson RE, Berman S, Papp JR, McQuillan G, et al. Gonorrhea and chlamydia in the United States among persons 14 to 39 years of age, 1999 to 2002. Ann Intern Med. 2007;147(2):89–96.
Buot ML, Docena JP, Ratemo BK, Bittner MJ, Burlew JT, Nuritdinov AR, et al. Beyond race and place: distal sociological determinants of HIV disparities. PLoS One. 2014;9(4):e91711.
Robertson MJ, Clark RA, Charlebois ED, Tulsky J, Long HL, Bangsberg DR, et al. HIV seroprevalence among homeless and marginally housed adults in San Francisco. Am J Public Health. 2004;94(7):1207–17.
Myers T, Allman D, Xu K, Remis RS, Aguinaldo J, Burchell A, et al. The prevalence and correlates of hepatitis C virus (HCV) infection and HCV-HIV co-infection in a community sample of gay and bisexual men. Int J Infect Dis. 2009;13(6):730–9.
Bacon O, Lum P, Hahn J, Evans J, Davidson P, Moss A, et al. Commercial sex work and risk of HIV infection among young drug-injecting men who have sex with men in San Francisco. Sex Transm Dis. 2006;33(4):228–34.
Gorbach PM, Murphy R, Weiss RE, Hucks-Ortiz C, Shoptaw S. Bridging sexual boundaries: men who have sex with men and women in a street-based sample in Los Angeles. J Urban Health. 2009;86(Suppl 1):63–76.
Koken JA, Parsons JT, Severino J, Bimbi DS. Exploring commercial sex encounters in an urban community sample of gay and bisexual men: a preliminary report. J Psychol Human Sex. 2005;17(1–2):197–213.
Elifson KW, Boles J, Sweat M. Risk factors associated with HIV infection among male prostitutes. Am J Public Health. 1993;83(1):79–83.
Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: implications for HIV prevention programs. J Acquir Immune Defic Syndr. 2005;39(4):446–53.
Boily M-C, Shubber Z. Modelling in concentrated epidemics: informing epidemic trajectories and assessing prevention approaches. Curr Opin HIV AIDS. 2014;9(2):134–49.
Boily M, Lowndes C, Alary M. The impact of HIV epidemic phases on the effectiveness of core group interventions: insights from mathematical models. Sex Transm Infect. 2002;78(Suppl 1):i78–90.
Vickerman P, Foss AM, Pickles M, Deering K, Verma S, Demers E, et al. To what extent is the HIV epidemic in southern India driven by commercial sex? A Model Anal AIDS. 2010;24(16):2563–72.
Boily M-C, Pickles M, Alary M, Baral S, Blanchard J, Moses S, et al. What really is a concentrated HIV epidemic and what does it mean for West and Central Africa? Insights from mathematical modeling. J Acquir Immun Defic Syndr. 2015;68:S74–82.
Kato M, Granich R, Bui DD, Tran HV, Nadol P, Jacka D, et al. The potential impact of expanding antiretroviral therapy and combination prevention in Vietnam: towards elimination of HIV transmission. J Acquir Immun Defic Syndr. 2013;63(5):e142–9.
Gomez GB, Borquez A, Caceres CF, Segura ER, Grant RM, Garnett GP, et al. The potential impact of pre-exposure prophylaxis for HIV prevention among men who have sex with men and transwomen in Lima, Peru: a mathematical modelling study. PLoS Med. 2012;9(10):e1001323.
Gallagher KM, Sullivan PS, Lansky A, Onorato IM. Behavioral surveillance among people at risk for HIV infection in the US: The National HIV Behavioral Surveillance System. Public Health Rep. 2007;122(Suppl 1):32–8.
MacKellar DA, Gallagher KM, Finlayson T, Sanchez T, Lansky A, Sullivan PS. Surveillance of HIV risk and prevention behaviors of men who have sex with men—a national application of venue-based, time-space sampling. Public Health Rep. 2007;122(Suppl 1):39–47.
Finlayson TJ, Le B, Smith A, Bowles K, Cribbin M, Miles I, et al. HIV risk, prevention, and testing behaviors among men who have sex with men—National HIV Behavioral Surveillance System, 21 US cities, United States, 2008. Surveill Summ. 2011;60(14):1–34.
CDC. Notice to readers: protocols for confirmation of reactive rapid HIV tests. Morb Mortal Wkly Rep. 2004;53(10):221–2.
CDC. Update: HIV counseling and testing using rapid tests–United States, 1995. Morb Mortal Wkly Rep. 1998;47(11):211–5.
CDC. Interpretation and use of the western blot assay for serodiagnosis of human immunodeficiency virus type 1 infections. Morb Mortal Wkly Rep. 1989;38(Suppl 7):1–7.
Barros AJ, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003;3:21.
Bernstein KT, Marcus JL, Nieri G, Philip SS, Klausner JD. Rectal gonorrhea and chlamydia reinfection is associated with increased risk of HIV seroconversion. J Acquir Immune Defic Syndr. 2010;53(4):537–43.
Jin F, Prestage GP, Imrie J, Kippax SC, Donovan B, Templeton DJ, et al. Anal sexually transmitted infections and risk of HIV infection in homosexual men. J Acquir Immune Defic Syndr. 2010;53(1):144–9.
Ostrow DG, Plankey MW, Cox C, Li X, Shoptaw S, Jacobson LP, et al. Specific sex drug combinations contribute to the majority of recent HIV seroconversions among MSM in the MACS. J Acquir Immun Defic Syndr. 2009;51(3):349–55.
Workowski KA, Berman SM, Control CfD, Prevention. Sexually transmitted diseases treatment guidelines, 2010: department of Health and Human Services, Centers for Disease Control and Prevention; 2010.
Parsons JT, Koken JA, Bimbi DS. The use of the Internet by gay and bisexual male escorts: sex workers as sex educators. AIDS Care. 2004;16(8):1021–35.
Mosbergen D. The internet’s most desired gay male escorts tell all. Huffpost Gay Voices. 2014.
Döring NM. The Internet’s impact on sexuality: a critical review of 15 years of research. Comput Human Behav. 2009;25(5):1089–101.
Sullivan PS, Carballo-Dieguez A, Coates T, Goodreau SM, McGowan I, Sanders EJ, et al. Successes and challenges of HIV prevention in men who have sex with men. Lancet. 2012;380(9839):388–99.
US Public Health Service. Prexposure prophylaxis for the prevention of HIV infection in the United States-2014. A clinical practice guideline-2014.
Baral S, Logie CH, Grosso A, Wirtz AL, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2013;13:482.
Amaral MLS, Abdo CH, Tavares H. Scanavino MdT. Personality among sexually compulsive men who practice intentional unsafe sex in São Paulo, Brazil. J Sex Med. 2015;12(2):557–66.
Gullette D, Booth BM, Wright PB, Montgomery BE, Stewart KE. Sexual sensation seeking, transactional sex, and rural African American cocaine users. J Assoc Nurses AIDS Care. 2014;25(4):289–96.
Acknowledgments
This research was supported in part by an appointment to the Research Participation Program at the Centers for Disease Control and Prevention administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the US Department of Energy and CDC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Lina M. Nerlander, Kristen L. Hess, Catlainn Sionean, Charles E. Rose, Anna Thorson, Dita Broz and Gabriela Paz-Bailey declares that they have no conflict of interest.
Disclaimer
The findings and conclusions in this paper are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
M. Nerlander, L., Hess, K.L., Sionean, C. et al. Exchange Sex and HIV Infection Among Men Who Have Sex with Men: 20 US Cities, 2011. AIDS Behav 21, 2283–2294 (2017). https://doi.org/10.1007/s10461-016-1450-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-016-1450-6