Abstract
Short message service (SMS) text messages have been used to remind and encourage patients to take ART in research studies. However, few studies have assessed the feasibility and acceptability of SMS in routine clinical practice. We report patient perspectives on a weekly SMS adherence support program after implementation into clinical care at an HIV clinic in KwaZulu-Natal, South Africa. We conducted structured interviews with a cross-sectional convenience sample of 100 adult patients who were invited to join the program, 88 of whom had received a program SMS. Of these respondents, 81 (92 %) would recommend the program to a friend. Sixty-eight (77 %) felt the program helped them remember clinic appointments, a response associated with male gender [odds ratio (OR) 5.88, 95 % confidence interval (CI) 1.52–23.26, P = 0.011] and HIV disclosure outside the home [OR 3.40, 95 %CI 1.00–11.60, P = 0.050]. This clinical SMS adherence program was found to have high patient-perceived usefulness.
Resumen
Servicio de mensajes cortos (SMS) mensajes de texto se han utilizado para recordar y alentar a los pacientes a tomar ART en estudios de investigación. Sin embargo, pocos estudios han evaluado la viabilidad y aceptabilidad de los SMS en la práctica clínica habitual. Presentamos las perspectivas del paciente en un programa de apoyo a la adherencia de SMS semanal después de la implementación en la atención clínica en una clínica de VIH en KwaZulu -Natal, Sudáfrica. Hemos llevado a cabo entrevistas estructuradas con una muestra conveniencia transversal de 100 pacientes adultos que fueron invitados a participar en el programa, 88 de los cuales habían recibido un SMS del programa. De estos encuestados, 81 (92 %) recomendarían el programa a un amigo. Sesenta y ocho (77 %) considera el programa ayudó a recordar citas en la clínica, una respuesta asociada con el género masculino [odds ratio (OR) 5,88; intervalo de confianza del 95 % (IC) 1,52 a 23,26; p = 0,011] y la revelación del VIH fuera del casa [OR 3,40; IC del 95 % 1,00 a 11,60; p = 0,050]. Se encontró que este programa de adherencia SMS clínica para tener una alta utilidad percibida por el paciente.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Antiretroviral therapy (ART) can restore health and prevent ongoing transmission among individuals infected with HIV [1, 2]. Viral suppression depends on consistently high adherence to ART and is critical to achieving optimal clinical outcomes, but a systematic review indicated that only 63 % of patients in sub-Saharan Africa demonstrate viral suppression at 2 years after ART initiation [3].
Adherence to ART requires retention in care to access therapy, as well as consistent ingestion of medication. The obstacles to ART adherence are many and complex [4, 5]. Given these multiple challenges, and the growing prevalence of mobile phone usage in the developing world, organizations and researchers have launched pilot projects and studies using text messaging (SMS) and other mobile technologies to support adherence. Such SMS programs generally target forgetfulness [6–9], but may also overcome other adherence barriers such as low self-efficacy [4], low motivation, and poor understanding of intended benefits of ART. Additionally, in a recent evaluation of an SMS program in Uganda, participants reported that the SMS made them feel cared for [10]. This type of support may be especially important in overcoming feelings of shame or reprisal by clinic staff for missed doses or missed appointments, which can contribute to disengagement from care [11].
The impact of SMS programs on adherence has been studied in multiple randomized controlled trials (RCTs), which have generally demonstrated positive results. Two RCTs of weekly SMS programs in Kenya, using local languages for newly-initiating ART patients, demonstrated effectiveness of the SMS programs [12, 13]. An RCT of adherence counseling plus twice-weekly SMS in Nigeria among initially non-adherent subjects found a significant improvement in self-reported adherence [14]. One RCT in Cameroon that examined SMS appointment reminders for caregivers of children living with HIV found that the SMS significantly improved appointment attendance compared to standard of care [15]. Other studies, however, have found no effect. Another RCT in Cameroon, using weekly SMS for ART-experienced patients, found no significant benefit on multiple adherence metrics [16]. An RCT in India found that automated voice calls and pictorial messages had no significant effect on adherence compared to standard of care [17]. Meta-analyses using evidence from some of these and other RCTs have demonstrated that weekly SMS is efficacious at improving self-reported adherence [18–20].
While overall positive, these inconsistent results raise questions about how best to conduct an effective SMS program [21]. Several feasibility surveys have been done with ART patients to inquire about a proposed SMS program. In these, patients have expressed an interest in such a program, so long as it did not explicitly mention HIV or antiretrovirals [8, 9, 22, 23]. One study that included focus groups of young people aged 15–24 in Uganda found that the youths preferred that any messages not even mention drugs or pills [24]. Post hoc evaluations of SMS programs in India [25], Kenya [12], and Botswana [26] have reported an overall positive impression tempered by concerns about privacy. In contrast, the Cameroon RCT with non-significant results [16, 27] found that 35 % of SMS recipients did not want the program to continue after 6 months. Notably, all of these SMS programs were conducted in the context of randomized controlled trials and experience may be different in “real world” settings. To our knowledge, no study has been published of patient experiences with an SMS adherence program operating in routine clinical practice in the KwaZulu-Natal Province of South Africa.
In this paper, we examine patient-reported experiences with a clinical program of weekly SMS adherence reminders at a clinic near Durban, South Africa. Our primary objectives were to determine the patient-reported acceptability and perceptions of the SMS program. Secondary objectives included identifying areas for improvement and factors associated with perceived usefulness of the SMS program.
Methods
Ethical Approval
Ethical approval for the study was obtained from the Durban University of Technology Institutional Research Ethics Committee and the Partners Human Research Committee. Permission was obtained from the KwaZulu-Natal Department of Health, Office of Health Research and Knowledge Management.
Study Population
The study was conducted at the Ethembeni HIV Clinic, located approximately 40 km from Durban, South Africa. Ethembeni is a government-run antiretroviral clinic with an on-site pharmacy, which provides ART free of charge to more than 3000 patients in care. Nearly all adult patients at Ethembeni speak isiZulu as their first language.
SMS Program
In September 2013, the clinic launched an SMS-based ART adherence support program. The program was developed by clinic staff in collaboration with Sawubona Health (Malden, MA), a US-based non-governmental organization. The clinic SMS program is based on a weekly SMS program found to be effective in the Kenyan RCT noted above [13] and modified for the clinic’s purposes. The program consists of a clinic computer that hosts the local database of patient names and their phone numbers. A secure server, hosted by Sawubona Health, synchronizes with the local database. Each week, the server uses PHP scripts (commonly used for web development) to automatically generate the messages and pass them and the corresponding phone numbers to a BulkSMS service provider (Celerity Systems LTD, South Africa) for distribution. The cost of the program, $1 USD per patient per year, is covered by Sawubona Health; the clinic itself bears no cost. There is also no cost to patients to receive the messages or participate in the program, and patients are able to opt-out at any time. For the first 4 months, the opt-out process was sending a free “Please Call Me” message to a dedicated clinic cell phone. The method was thereafter changed to sending a reply SMS of “yima” (isiZulu for “end”) or “end” in English, subject to standard SMS charges. Throughout, the patient can also opt-out by informing a clinic staff member.
Clinic staff and Sawubona Health volunteers manually entered mobile phone numbers from the charts of adult patients active in care into the SMS program database in 2012 and 2013. Due to resource constraints, patients enrolling at the clinic after the data collection periods were not added to the SMS program database. Prior to launch, explanatory posters were placed in the clinic. The first SMS sent to patients also explains the program and how to opt-out. Enrolled patients receive SMS messages in isiZulu every Monday afternoon stating:
Hi (First name), this is your clinic. Remember to take your pills on schedule in order to (One of: be strong or live a long life or feel well; in rotating order). Thank you.
For the first few months of the program, patients who were more than 30 days late for a scheduled appointment were sent the following message, if such lateness was captured to the SMS program by clinic staff:
Hello (First name), this is your clinic. We are concerned about you. Remember that visiting your clinic on schedule helps keep you healthy.
These late appointment SMS were not maintained due to staffing limitations. Delivery status reports are available for most SMS messages. The program pauses the SMS sending for 3 weeks before trying again for patients from whom it receives 10 consecutive delivery failure reports.
Study Design
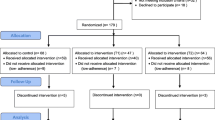
We assessed the acceptability of the SMS program with structured interviews among a cross-sectional convenience sample of patients who had been invited to join the SMS program at Ethembeni Clinic. Patients were eligible to participate if they were HIV-infected, 18 years or older, had a mobile phone number recorded in their chart at the start of the SMS program, and had been on ART at Ethembeni Clinic for at least 6 months prior to the start of the SMS program.
Eligible patients were recruited via a convenience sampling process. A sample size of 100 participants was based on the resources available for this exploratory study. We aimed to achieve balance between genders and age groups (older and younger than 35) because males have been found to differ from females in terms of engagement with care [28–30] and mobile phone use [22], and experience with technology may differ by age. If a patient presenting to clinic for scheduled care was eligible, a clinic nurse directed them to a private room where the research assistant obtained informed consent. The age and gender balancing was achieved by temporarily not offering invitations to patients in the demographic groups with greatest representation in the sample. Consenting participants were then interviewed in their preferred language (English or isiZulu) using a standardized questionnaire. A single research assistant, who was not on the clinic staff, conducted all interviews. Up to 10 interviews could be conducted per day. The survey was based on questions used in assessing feasibility of a similar SMS program in Uganda [31]. We assessed educational attainment, socioeconomic status, cell phone usage, and experience with and perceptions of the SMS program. Demographic and clinic data, including age, most recent CD4 count, and date of ART initiation were extracted from the participant’s medical records. Participants were given 100 Rand (~$9 USD at the time of the study) for their participation.
All data was entered into an online RedCap database [32]. All statistical analyses were performed with SAS University Edition (SAS Institute, Cary, NC). Using univariable logistic regression, we tested for associations between participant characteristics and interview responses. Our outcomes of interest were participant reports (yes or no) of the following: (1) receiving at least one SMS from the program; (2) finding that the SMS program helped with remembering clinic appointments; (3) being late to an appointment in the past year; (4) finding that the SMS program helped with adherence. Because nearly all participants reported that the SMS program helped with adherence, regression analysis was not pursued for outcome 4. For each of the other outcomes, we ran separate univariable regression analyses using gender and age because prior studies have demonstrated their effects on engagement with care [28–30], mobile phone use [22], and experience with clinical SMS [33]. Additional predictors were selected based on hypothesized relationships or prior studies suggesting relevance, as follows:
-
1.
SMS receipt (outcome 1): whether a phone had been replaced due to theft, ownership of an unshared mobile phone, SMS use frequency (more than once per month), and literacy (dichotomized at ability to read complete sentence) [33]
-
2.
Whether the SMS program helped remind patients about appointments (outcome 2): ART duration (per year) [12, 16], HIV disclosure outside the home [34], educational attainment (dichotomized at primary school), and SMS use frequency (more than once per month) [33]
-
3.
Being late to an appointment in the past year (outcome 3): ART duration (per year) [12, 16], HIV disclosure outside the home [34], employment (dichotomized at part-time), and transport method to clinic (dichotomized as public transport vs. other) [35].
For each outcome, we then ran multivariable logistic regression analyses including those variables found to have a P < 0.20 on univariable analysis [36]. Goodness of fit was indirectly assessed by the significance of the estimated parameters. Results with P ≤ 0.05 were considered statistically significant. All individuals missing data in a regression were excluded. This manuscript reflects guidance from the STROBE statement [37].
Results
Characteristics of Interviewed Participants
From July through September 2014, we conducted 17 interview days in order to recruit and interview 100 patients who met the study inclusion criteria. All participants chose to be interviewed primarily in isiZulu. The characteristics of the participants are summarized in Table 1. The overall adult clinic population is approximately 67 % (~1800/2700) female and has a median age of 37 years old; our sample of 100 participants had a slightly lower proportion of females at 59 % by study design and had a similar median age of 39.5 years. Respondents had a median of 3.3 years of prior ART use and all of them had disclosed their HIV status to at least one other person. Seventy of interviewed patients had achieved at least a secondary education and 56 reported some form of employment. Phone access was high, with 97 participants owning their own mobile phone. Of these, 12 (12.4 %) participants reported that they shared their mobile phone with another person. Phone turnover was also common, with 59 % of the participants having to replace their phone in the past year, most commonly due to theft or damage.
Among the 100 interviewed participants, all of whom had phone numbers recorded in the SMS program database by study design, 88 reported receiving at least one SMS from the program. As shown in Table 2, receiving at least one SMS was negatively associated with a participant having his/her phone stolen in the past year [odds ratio (OR) 0.22, 95 % confidence interval (CI) 0.06–0.85, P = 0.027]. Notably, no significant associations were found with a literacy metric or SMS use frequency.
Acceptability of the SMS Program
The remainder of the results are limited to the 88 participants who reported receiving at least one SMS from the program, and are shown in Table 3. Among them, 81 (92.0 %) said they would recommend the SMS program to a friend and 80 (90.9 %) described the weekly SMS frequency as “just right.” Nine (10.2 %) participants reported that at some point, they did not receive an expected weekly SMS.
Three (3.4 %) respondents reported that an SMS led to an inadvertent disclosure of their HIV status. In all three cases, the respondent explained that they were planning to eventually discuss their status with the individual. Two of these participants reported that they felt the SMS program violated their privacy “a little” and the third one opted out, but all three still stated they would recommend the program to a friend.
Perceptions of the Impact of the SMS Program
Eighty-six (97.7 %) participants reported that the SMS helped them remember their medication and 68 (77.3 %) of the participants agreed that the SMS helped them remember their appointments. As shown in Table 4, male participants [OR 5.88, 95 % CI 1.52–23.26, P = 0.011] and those having disclosed their HIV statuses outside the household [OR 3.40, 95 % CI 1.00–11.60, P = 0.050] were more likely to report that the SMS helped them remember their appointments. Fourteen (15.9 %) participants reported that the SMS were reminders that the clinic cares about them. Without direct prompting, 9 (10.2 %) participants added that they considered the SMS to be encouraging.
Almost 40 % of the participants reported not attending a clinic appointment on its scheduled date (“being late to an appointment”) in the past year, most of which corresponded to time after the SMS program started. Late appointments were rarely (5.9 %) due to forgetting the appointment date, and mostly (52.9 %) due to travel for work. As shown in Table 5, younger respondents were more likely to report being late to an appointment in the past year [OR per 10 years 0.60, 95 % CI 0.37–0.97, P = 0.037]. Among those who were late to a scheduled appointment, the delays had a median of 7 days (IQR 2–7 days), and three participants (8.8 %) did not return within 4 weeks of the scheduled date. Five participants reported receiving a program SMS after their scheduled appointment date but before returning to clinic; all five endorsed that the SMS “encouraged [them] to return.”
Desired Modifications to the SMS Program
Nearly 90 % of the participants expressed a desire to use the SMS as a two-way communication channel with the clinic. These participants stated that they would like to speak with a doctor, counselor, or nurse. Physical concerns, such as illness, were cited as the main reason for seeking to communicate.
In addition, participants generally desired more customizability in terms of SMS delivery time: 40 (45.5 %) preferred to receive the messages at a time other than the afternoon, which is the program’s standard time. In addition, 38 (43.2 %) reported a desire to have greater variety in the message content, among whom 29 (76.3 %) would like more information about HIV medications in the messages.
Discussion
Participant-reported experiences with a clinically-implemented SMS program were overall positive. The program’s technical reliability was high, as evidenced by only 10 % of recipients reporting that they had not received an expected SMS at some point during the study period. The SMS program was also widely accepted and perceived as helpful, based on 92 % of participants reporting that they would recommend it to a friend and that it was commonly reported to help respondents remember their medications (98 %) and appointments (77 %). These findings of patient-reported benefit are consistent with reports on other SMS adherence programs [12, 25, 26] and compare favorably to a weekly SMS trial in Cameroon, where 65 % of participants wanted to continue receiving the SMS [16], versus 97 % in this study. Participants favored the weekly frequency of the messaging program over either greater or lesser frequencies, which is consistent with the finding from a meta-analysis that weekly SMS are better than daily SMS at improving self-reported adherence [19].
The mechanism by which weekly SMS might enhance adherence to a daily schedule of medication is unclear. As reported previously in Uganda [10], participants may have felt “cared for” by the Ethembeni clinic, possibly reflected by the fact that approximately 27 % of respondents said that the SMS encouraged them or that the SMS reminded them that the clinic cares. Further exploration of the meaning of SMS in this and other populations is needed.
We found that males and those who had disclosed their HIV status outside the home were more likely to find the SMS program helpful. Males typically have a lower baseline retention in care [29, 30], whereas there may have been a ceiling effect for female patients. An RCT in Kenya found a non-significant trend of males gaining greater benefit from an SMS program [12]. It is possible that the SMS partially addresses an unmet need in men’s engagement with HIV care. Patients who have already disclosed their status may perceive the SMS program as more helpful because they are less worried about the SMS contributing to inadvertent disclosure.
Privacy concerns must be considered, given that three patients reported that an SMS led to a disclosure of their HIV status. Importantly, all three added that they had been planning on eventually disclosing to the individuals, although we cannot be certain of the precise circumstances. This finding, in addition to the association of HIV status disclosure with helpfulness of the SMS program, suggests that the program is better suited for patients for whom disclosure is less of a concern. It is notable that the messages do not mention “HIV” or “antiretrovirals”, and that many other chronic diseases are treated with long-term medication in South Africa. Even so, the SMS program messages may be too direct. A direct message was found acceptable and helpful for reporting abnormal lab results in Uganda [31, 33]. However, other approaches seem feasible, given that some SMS programs have used coded messages, such as “This is your reminder” [13] or even “ABCDEFG” [33], with good effect when communicating with patients regarding clinical matters. Overall, both direct and coded messages seem to be acceptable, and options may be appealing to individual patients.
Appointment attendance remains challenging, with nearly 40 % of participants reporting being late to an appointment in the past year. Notably, this rate was derived from participants who were attending a clinic visit at the time of interview, so the clinic-wide no-show rate may be higher. This finding is important as prior research has shown that even a single late appointment risks initiating a disengagement from care [11]. Work travel was cited in the majority of cases. Interestingly, younger age, but not employment, was found to be an independent predictor of missing an appointment. The association between younger age and HIV clinic nonattendance has been seen elsewhere [38]. Messages encouraging advance planning, especially for work travel and for young patients, may thus be beneficial to maintaining continuity of care.
The results of this study highlighted other possible targets for optimizing SMS adherence programs. Two further areas of enhancement would not require additional human resources at the clinic: (1) greater customizability in terms of SMS delivery time, and (2) more variety and personalization of the SMS content, including information about new HIV medications and nutrition. In contrast, the following suggestions would require partial reallocation of clinic staff, but the benefits may outweigh the costs. Consistent with previous findings at a nearby HIV clinic [22], phone turnover was high. While a lost phone doesn’t necessarily translate to a changed number, this is a strong indication for frequently updating patient phone numbers. Also, nearly all patients desired two-way communication with the clinic staff via SMS, primarily about physical concerns (such as illness or side effects). Trials in Kenya [12] and Cameroon [27] found two-way communication to be similarly desired and also feasible; a SMS program trial in Kenya used two-way communication with a nurse and found that only 3.3 % of patients per week actually requested follow-up [12].
This study benefited from representation from a sample with age and gender balance and from interviewing recipients with a median of 10 months of experience with the clinical SMS program. This is an advantage over others in which patients were asked about hypothetical SMS programs [9, 22, 23]. Our analysis was limited by a small sample size (N = 100) that may have been affected by sampling bias. Interviews were conducted on a convenience sample of longstanding patients who were attending their clinic appointments, which may lead to over-estimation of program acceptability. In addition, the program’s patient-reported impact on retention in care may have been influenced by social desirability bias (i.e., patients may have wanted to appear appreciative of the clinic’s services). Furthermore, our questions did not illuminate the mechanisms by which the SMS program’s patient-reported impact was brought about. The generalizability of these results to other clinics, especially those outside of KwaZulu-Natal, is uncertain as patients experience an SMS program in the context of their clinical and social worlds. Importantly, this study is limited to self-reported opinions and does not include objective data on adherence or retention in care. Additionally, the SMS program did not supply any mobile phones, as has been done in some research studies [13, 17], because of cost. Thus, the participants who received SMS had pre-existing access to cell phones, and thus may have been more familiar with the technology than others at the clinic. However, most government-run clinics would face similar economic challenges, and so we do not believe that this significantly limits the generalizability of the results.
In evaluating this clinical program, several lessons were learned. First, scarcity of human resources limited the frequency with which patient phone numbers could be updated, as well as new enrollments into the program. As standard clinical record keeping becomes increasingly electronic, better integration of SMS programs may reduce the human resource requirement. Importantly, the automated nature of the program enabled continued provision of the program to subscribed patients despite human resource limitations.
Conclusions
This cross-sectional structured interview study of an SMS program implemented as part of routine clinical care found high levels of acceptability and positive perceptions of the program. To our knowledge, it is one of the first studies of an SMS program that had been implemented outside of the resource-intensive context of a research study. These findings suggest that a clinical SMS program can offer at least a perceived benefit. Additional evaluation of the objective impact of the program is needed. Given the low cost of the program at $1 USD per patient per year, such programs merit further exploration and consideration for use if proven to be effective.
References
Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505.
Conway B. The role of adherence to antiretroviral therapy in the management of HIV infection. JAIDS J Acquir Immune Defici Syndr. 2007;45:S14–8.
Barth RE, van der Loeff MFS, Schuurman R, Hoepelman AIM, Wensing AMJ. Virological follow-up of adult patients in antiretroviral treatment programmes in Sub-Saharan Africa: a systematic review. Lancet Infect Dis. 2010;10(3):155–66.
Merten S, Kenter E, McKenzie O, Musheke M, Ntalasha H, Martin-Hilber A. Patient-reported barriers and drivers of adherence to antiretrovirals in Sub-Saharan Africa: a meta-ethnography. Trop Med Int Health. 2010;15:16–33.
Chesney M. Adherence to HAART regimens. AIDS Patient Care STDs. 2003;17(4):169–77.
Peltzer K, Friend-du Preez N, Ramlagan S, Anderson J. Antiretroviral treatment adherence among HIV patients in KwaZulu-Natal, South Africa. BMC Public Health. 2010;10(1):111.
Mills EJ, Nachega JB, Buchan I, et al. Adherence to antiretroviral therapy in Sub-Saharan Africa and North America: a meta-analysis. JAMA. 2006;296(6):679–90.
Shet A, Arumugam K, Rodrigues R, et al. Designing a mobile phone-based intervention to promote adherence to antiretroviral therapy in South India. AIDS Behav. 2010;14(3):716–20.
Mbuagbaw L, Bonono-Momnougui RC, Thabane L. Considerations in using text messages to improve adherence to highly active antiretroviral therapy: a qualitative study among clients in Yaoundé, Cameroon. HIV/AIDS (Auckland, N.Z.). 2012;4:45–50.
Ware NC, Wyatt MA, Pisarski EE, et al. Meanings of SMS reminders for adherence support among adults taking ART in rural Southwestern Uganda. In: International conference on HIV prevention and treatment adherence. Miami, 2015 [abstract].
Ware NC, Wyatt MA, Geng EH, et al. Toward an understanding of disengagement from HIV Treatment and care in Sub-Saharan Africa: a qualitative study. PLoS Med. 2013;10(1):e1001369.
Lester RT, Ritvo P, Mills EJ, et al. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trial. Lancet. 2010;376(9755):1838–45.
Pop-Eleches C, Thirumurthy H, Habyarimana JP, et al. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: a randomized controlled trial of text message reminders. AIDS. 2011;25(6):825–34.
Maduka O, Tobin-West CI. Adherence counseling and reminder text messages improve uptake of antiretroviral therapy in a tertiary hospital in Nigeria. Niger J Clin Pract. 2013;16(3):302–8.
Bigna JJR, Noubiap JJN, Kouanfack C, Plottel CS, Koulla-Shiro S. Effect of mobile phone reminders on follow-up medical care of children exposed to or infected with HIV in Cameroon (MORE CARE): a multicentre, single-blind, factorial, randomised controlled trial. Lancet Infect Dis. 2014;14(7):600–8.
Mbuagbaw L, Thabane L, Ongolo-Zogo P, et al. The cameroon mobile phone SMS (CAMPS) trial: a randomized trial of text messaging versus usual care for adherence to antiretroviral therapy. PLoS One. 2012;7(12):e46909.
Shet A, Costa AD, Kumarasamy N, et al. Effect of mobile telephone reminders on treatment outcome in HIV: evidence from a randomised controlled trial in India. BMJ. 2014;349:g5978.
Mbuagbaw L, van der Kop ML, Lester RT, et al. Mobile phone text messages for improving adherence to antiretroviral therapy (ART): an individual patient data meta-analysis of randomised trials. BMJ Open. 2013;3(12):e003950.
Mills EJ, Lester R, Thorlund K, et al. Interventions to promote adherence to antiretroviral therapy in Africa: a network meta-analysis. Lancet HIV. 2014;1(3):e104–11.
Finitsis DJ, Pellowski JA, Johnson BT. Text message intervention designs to promote adherence to antiretroviral therapy (ART): a meta-analysis of randomized controlled trials. PLoS One. 2014;9(2):e88166.
Wald DS, Butt S, Bestwick JP. One-way versus two-way text messaging on improving medication adherence: meta-analysis of randomized trials. Am J Med. 2015;128(10):1139.e1131–5.
Crankshaw T, Corless IB, Giddy J, Nicholas PK, Eichbaum Q, Butler LM. Exploring the patterns of use and the feasibility of using cellular phones for clinic appointment reminders and adherence messages in an antiretroviral treatment clinic, Durban, South Africa. AIDS Patient Care STDs. 2010;24(11):729–34.
Curioso WH, Alex Quistberg D, Cabello R, et al. “It’s time for your life”: How should we remind patients to take medicines using short text messages? In: AMIA annual symposium proceedings/AMIA symposium. AMIA symposium. 2009;2009:129–33.
Rana Y, Haberer J, Huang H, et al. Short message service (SMS)-based intervention to improve treatment adherence among HIV-positive youth in Uganda: focus group findings. PLoS One. 2015;10(4):e0125187.
Rodrigues R, Shet A, Antony J, et al. Supporting adherence to antiretroviral therapy with mobile phone reminders: results from a Cohort in South India. PLoS One. 2012;7(8):e40723.
Reid MJA, Dhar SI, Cary M, et al. Opinions and attitudes of participants in a randomized controlled trial examining the efficacy of SMS reminders to enhance antiretroviral adherence: a cross-sectional survey. JAIDS J Acquir Immune Defici Syndr. 2014;65(2):e86–8.
Mbuagbaw L, Thabane L, Ongolo-Zogo P. Opening communication channels with people living with HIV using mobile phone text messaging: insights from the CAMPS trial. BMC Res Notes. 2013;6(1):131.
Bassett IV, Regan S, Chetty S, et al. Who starts antiretroviral therapy in Durban, South Africa?… not everyone who should. AIDS (London, England). 2010;24(Suppl 1):S37.
Mills EJ, Beyrer C, Birungi J, Dybul MR. Engaging men in prevention and care for HIV/AIDS in Africa. PLoS Med. 2012;9(2):e1001167.
Brennan A, Maskew M, Sanne I, Fox M. The importance of clinic attendance in the first six months on antiretroviral treatment: a retrospective analysis at a large public sector HIV clinic in South Africa. J Int AIDS Soc. 2010;13(1):49.
Siedner MJ, Haberer JE, Bwana MB, Ware NC, Bangsberg DR. High acceptability for cell phone text messages to improve communication of laboratory results with HIV-infected patients in rural Uganda: a cross-sectional survey study. BMC Med Inform Decis Mak. 2012;12:56.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Siedner MJ, Santorino D, Haberer JE, Bangsberg DR. Know your audience: predictors of success for a patient-centered texting app to augment linkage to HIV care in rural Uganda. J Med Internet Res. 2015;17(3):e78.
Stirratt M, Remien R, Smith A, Copeland O, Dolezal C, Krieger D. The role of HIV serostatus disclosure in antiretroviral medication adherence. AIDS Behav. 2006;10(5):483–93.
Tuller D, Bangsberg D, Senkungu J, Ware N, Emenyonu N, Weiser S. Transportation costs impede sustained adherence and access to HAART in a clinic population in Southwestern Uganda: a qualitative study. AIDS Behav. 2010;14(4):778–84.
Hosmer DW, Lemeshow S. Multiple logistic regression. Applied logistic regression. New York: Wiley; 2005. p. 31–46.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Prev Med. 2007;45(4):247–51.
Catz SL, McClure JB, Jones GN, Brantley PJ. Predictors of outpatient medical appointment attendance among persons with HIV. AIDS Care. 1999;11(3):361–73.
Acknowledgments
This study received financial support from the Harvard Medical School Scholars in Medicine Program, NIH Grant K23 MH087228, K23 MH099916, T32 AI007433. This work was conducted with support from Harvard Catalyst. The Harvard Clinical and Translational Science Center (NCRR and NCATS, NIH Award UL1 TR001102) and financial contributions from Harvard University and its affiliated academic healthcare centers. The authors would like to thank the staff of Ethembeni clinic for welcoming and assisting the research team, the interview participants for their time and feedback, student volunteers (including Marco Grossi, Grace Hansen-Gilmour, April Kim, and Bessie Zhang) for assistance with data capture, and the leadership staff of Sawubona Health (including Majahonkhe Shabangu, Roy Zhang, Dario Sava, and Antony Bett) for their insights into the SMS program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Nathan Georgette and Stephen Carpenter were involved in the development and implementation of the Ethembeni SMS program. Georgette is the volunteer CEO of the non-profit Sawubona Health, which helped establish and supports the Ethembeni SMS program.
Rights and permissions
About this article
Cite this article
Georgette, N., Siedner, M.J., Zanoni, B. et al. The Acceptability and Perceived Usefulness of a Weekly Clinical SMS Program to Promote HIV Antiretroviral Medication Adherence in KwaZulu-Natal, South Africa. AIDS Behav 20, 2629–2638 (2016). https://doi.org/10.1007/s10461-016-1287-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-016-1287-z