Abstract
There is little data on the burden of HIV and other infections that affect male sex workers (MSW) in Vietnam. We conducted behavioral and biological sexual health surveys with 300 MSW in Ho Chi Minh City. Generalized estimating equation models were built to assess factors associated with HIV, hepatitis C, and other sexually transmitted infections (STI). Of 300 MSW, 19 (6.3 %) were diagnosed seropositive for HIV, 11 (3.7 %) had hepatitis C, and 26 (8.7 %) had at least one prevalent STI. In a multivariable model, opiate use was significantly associated with HIV infection (aOR 6.46, 95 % CI 1.28–32.7) and hepatitis C (aOR = 19.6, 95 % CI 2.35–163.6). Alcohol dependency was associated with increased odds of hepatitis C (aOR = 4.79, 95 % CI 1.02–22.5) and decreased odds of other STI (aOR = 0.30, 95 % CI 0.10–0.97). These findings suggest that MSW in Vietnam would benefit from regular HIV and STI testing, as well as linkage to care and substance use rehabilitation services.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Men who exchange sex for money, drugs, goods, or other items of value (male sex workers; MSW) are at heightened risk of HIV infection globally compared to men in the general population [1]. In Vietnam, the HIV epidemic is concentrated in key populations including people who inject drugs (PWID) female sex workers (FSW), and men who have sex with men (MSM), including MSW [2, 3]. Individual-level [4], interpersonal (such as stigma [5] and sex work), and structural-level (such as the legal and social environments [6] ) factors influence HIV risk among Vietnamese MSW. In Ho Chi Minh City, MSW are a marginalized population who may not have access to HIV prevention education and interventions. Previous work with this population has demonstrated suboptimal HIV testing practices and inaccurate self-perception of HIV risk [7, 8], demonstrating a need for a better education and HIV prevention programming for this high-risk group.
National surveillance reports have documented an increase in HIV prevalence among MSM and MSW between 2006 and 2009 in Ho Chi Minh City [2, 3]. However, few studies have described factors associated with HIV infection in MSW and little data exist on seroprevalence of HIV in this population outside of national surveillance efforts. MSW may also be at high risk of sexually transmitted infections (STI), which may further predispose individuals to acquiring HIV infection. In addition, the HIV epidemic in Vietnam is highly concentrated among PWID [3], and it is possible that MSW who also inject drugs may have further elevated HIV risk, as well as risk for hepatitis C infection or HIV/hepatitis C co-infection. Furthermore, these risks may cluster within networks of MSW. For example, in other contexts substance use and condom use behaviors have been shown to cluster according to the venues in which MSW meet their clients (i.e., street-based versus indoor sex work) [9–11].
In order to design effective HIV prevention interventions for MSW, it is essential to have a better understanding of the current state of risk behavior and epidemiology, including prevalence of STI and co-infection with hepatitis C. Identifying factors associated with HIV, hepatitis C, and other STI, and how prevalence of these infections varies by client-meeting networks, could help to inform the development of HIV prevention interventions that are specific to these risk environments. The purpose of this study was to assess the prevalence of HIV, hepatitis C, and STI in a diverse population of MSW in Ho Chi Minh City and to determine factors associated with these infections.
Methods
Participants and Procedures
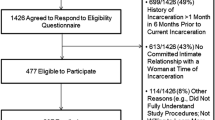
In December 2010, a cross-sectional survey was conducted with 300 MSW in Ho Chi Minh City (HCMC). Inclusion criteria for the study were: (1) 15 years of age or older at the time of the study; (2) born biologically male (regardless of current gender expression); (3) Vietnamese citizen, and (4) exchanged sex for money at least once in the previous month. The survey included structured questions on demographic information, sexual risk behaviors, experience with sex work, and psychosocial factors. Complete methods for the study have been previously reported [4]. In brief, participants were recruited for the survey via peer health educators from the Life Centre using venue-based sampling stratified by five groups based on how MSW in HCMC primarily met clients, including sauna/massage parlors, brothels, street/parks, bicycle massage (i.e., men who travel the streets via bicycle offering massage and sexual services), and callboys. Callboys are MSW who not have physical locations in which they meet partners, but contact clients through the telephone, the Internet, or third-party intermediaries. They were recruited using intermediary mama-sans or mamis. Bicycle massage MSW travel the city streets on bicycle at night to offer massage and sexual services to clients in their home; they were recruited on public streets where they were known to congregate. MSM outreach workers made initial contact in the field, or by telephone for callboys, and provided information about the study goals and procedures.
MSW who were interested in the study were invited to a public HIV testing clinic that also was the site of a publicly funded drop-in center for MSM. Informed consent was provided by study staff in a private room. MSW gave verbal consent as no identifying information was otherwise collected and signatures could potentially create a link to individual participants. Questionnaires were completed by study staff, a physician in the clinic completed the medical and STI examination, and pre-test and post-test HIV counseling was provided by a trained counselor. Following standard procedures for HIV testing in Vietnam at the time, HIV test results were available after 1 week. MSW were given a subject number with which they could receive the HIV and STI test results. All HIV and STI positive results were referred for treatment, which was available in the same public facility.
Participation in the survey was anonymous; no names signatures, or other identifying information was collected. Ethical approval was obtained through the Institutional Review Boards at Beth Israel Deaconess Medical Center and the Ho Chi Minh City Provincial AIDS Committee.
HIV, Hepatitis and STI Testing
Each participant underwent a medical examination to evaluate for physical manifestations of STI. Serum was collected for HIV antibody testing (HIV combi, Roche Diagnostics, Mannheim, Germany) and hepatitis C antibody (Elecsys Anti-HCV, Roche Diagnostics). A rapid plasma reagin (RPR) test (RPR, Biorad, UK) was undertaken for syphilis, Urethral swabs were collected to test for Neisseria gonorrhea by gram stain and microscopy and for Chlamydia trachomatis antigen detection (Hexagon Chlamydia, Human, Wiesbaden, Germany). Samples that tested positive for HIV antibody were sent to the Pasteur Institute for confirmatory testing following Vietnam Ministry of Health regulations. Participants were asked if they had ever previously had an HIV test, if they had collected the results of that test, and what the result of their most recent HIV test was (positive, negative, or unknown).
Measures
Demographic factors included age at the time of the survey, education (coded as completed high school education or above versus did not complete high school education or below), if the participant was born in Ho Chi Minh City or elsewhere, and average monthly income. Gender expression was categorized using the Vietnamese slang terminology commonly used by MSW and their clients at the time: bóng lộ (effeminate), bóng kín (masculine), and trai thẳng (“straight boy”). Sexual orientation was categorized as homosexual, bisexual, heterosexual, or unsure/other. Substance use included alcohol use, stimulant use (ecstasy/crystal methamphetamine), and opiate use. Alcohol dependence was measured using the Alcohol Use Disorders Identification Test (AUDIT), a 10-item validated scale that assesses harmful alcohol use. A score of 8 or greater was coded as suggestive of alcohol dependence. Participants were asked if they had ever used ecstasy/crystal methamphetamine and had ever smoked or injected opiates. Due to the low rate of opiate use in the sample, injecting and smoking were combined into one variable labeled opiate use for data analysis. Sexual behaviors were assessed by asking participants if they had had anal sex with commercial and non-commercial partners in the last month. Condomless anal intercourse (CAI) was defined as answering yes to the question “In the last month did you have anal sex without a condom?” for each partner type and separately for insertive and receptive anal sex.
Statistical Analysis
The prevalence of HIV, hepatitis C, and STIs were calculated for the overall study sample and by venue of recruitment defined by where MSW primarily met their commercial partners. To determine the proportion of participants who were unaware of their HIV serostatus, the number of HIV infected participants who had had a previous HIV test and the results of the most recent HIV test were tabulated. The distributions of demographic and behavioral factors were calculated with proportions for categorical variables and medians and interquartile range (IQR) for continuous variables.
To account for potential clustering by venue of recruitment, logistic generalized estimating equation (GEE) models were used to assess factors associated with prevalent HIV, hepatitis C, and STI. First, bivariate models were built assessing the association between sociodemographic variables and HIV risk-related factors and each dependent variable, including HIV, hepatitis C, and STI. Second, due to the relatively small prevalence of each outcome, a multivariable model for each outcome was built by including all variables with P ≤ 0.20 in the bivariate analyses. A P value of <0.05 was considered statistically significant and all tests were two-sided. All analyses were conducted in Stata 13.1 (StataCorp, College Station, TX).
Results
A total of 19 (6.3 %) of the 300 participants had a positive HIV test result in the study. None of these participants were previously aware of their HIV infection. Of the 19 participants with positive serostatus, 9 (47.4 %) had never previously had an HIV test. Of the ten who had been tested before, 8 (80 %) previously tested negative and 2 (20 %) never returned to the clinic to receive the results of their prior tests. The prevalence of HIV differed significantly across venue of recruitment, with the highest prevalence among callboys (11.5 %, Table 1). Eleven (3.7 %) tested positive for hepatitis C, and the prevalence of hepatitis C did not vary by venue of recruitment. The prevalence of other STIs was 8.7 % (n = 26) for any STI, including 2.0 % (n = 6) for chlamydia, 2.7 % (n = 8) for gonorrhea, and 4.0 % (n = 12) for syphilis. Five participants (45.5 % of participants with hepatitis C and 26.3 % of participants with HIV) had HIV/hepatitis C co-infection.
Characteristics by HIV status as well as the overall sample population are reported in Table 2. The median age was 21 years (IQR 19–24), and HIV infected participants tended to be older (median 24 years, IQR 21–27 years). Fewer participants who were HIV infected had completed a high school education compared to those who were not HIV infected (42.1 % compared to 58.9 %). Substance use was common in the sample. More than one-third (34.5 %) had symptoms compatible with alcohol dependency, 28.4 % had used stimulants (crystal methamphetamine or ecstasy), and 3.4 % had used heroin or opium. Of the 10 participants reporting opiate use, 4 (40 %) had done so in the previous month, 4 (40 %) reported only smoking opium, and 6 (60 %) reported injecting heroin. HIV prevalence was not statistically different in opiate smokers (1/4, 25 %) than in injectors (2/6, 33 %) (P = 1.0). More than half of the participants reporting stimulant use had used in the past month (n = 43, 52.4 %).
Gender identity and sexual orientation were not associated with HIV infection (Table 2). Although 30 % of the sample described their gender as trai thẳng or “straight boy,” only 16 % self-identified as heterosexual. About half (44/90) of the trai thẳng identified as heterosexual, 37.8 % (34/90) as bisexual, and 7.8 % (7/90) as homosexual. Anal sex with male partners was reported by 86.7 % of homosexuals, 72.3 % of bisexuals, and 54.2 % of heterosexuals (P < 0.001). Heterosexual MSW did have a lower HIV prevalence (2.1 %) than homosexuals (6.7 %) and bisexuals (8.5 %), but the difference was not significant (P = 0.45). Regardless of gender identity and sexual orientation, almost all of the MSW reported sex with male clients: 86.6 % had only male clients, 12.4 % had both male and female clients, and 1 % reported solely female clients. Gender of clients was not associated with HIV infection (data not shown).
In a multivariable model, older age (aOR 1.09 per year, 95 % CI 1.01–1.18) and a history of opiate use (aOR 6.46, 95 % CI 1.28–32.7) were the only factors independently associated with HIV infection (Table 2).
Bivariate and multivariable models were used to assess factors associated with a diagnosis of hepatitis C infection and other STI, including chlamydia, gonorrhea, and/or syphilis (Table 3). In a multivariable model, factors associated with hepatitis C infection included alcohol dependency (aOR 4.79, 95 % CI 1.02–22.5) and opiate use (aOR 19.6, 95 % CI 2.35–163.6). Use of stimulants was associated with a trend towards decreased odds of hepatitis C (aOR 0.09, 95 % CI 0.008–1.08), and older age was associated with a trend towards increased odds of hepatitis C (aOR 1.10 per year, 95 % CI 0.99–1.22). In a multivariable model, alcohol dependency was associated with decreased odds of STI (aOR 0.30, 95 % CI 0.10–0.97). Higher income was associated with a trend towards increased odds of STI (aOR 1.01 per 100,000 increase in VND, 95 % CI 1.00–1.02).
Discussion
This study demonstrated a relatively high prevalence of previously undiagnosed HIV infection among MSW in Ho Chi Minh City, Vietnam. Previous estimates of HIV prevalence among men who engage in transactional sex in this region have ranged from 3.6 % (Indonesia) to 17.5 % (Thailand) [1]. Importantly, none of the participants who received a positive HIV test result were previously aware of their infection and nearly half of participants with HIV infection had never been tested for HIV before. Given the recent increase in HIV prevalence among MSM in surveillance reports [2, 3], undiagnosed HIV infection among MSW may represent a facilitator of HIV transmission in networks of Vietnamese MSM. Initiation of antiretroviral therapy at higher CD4 counts has been shown to decrease HIV transmission among serodiscordant heterosexual couples [12]. If the majority of MSW in Vietnam are living with HIV infection are undiagnosed and therefore not necessarily virally suppressed, HIV may be transmitted more readily. CD4 and viral load testing was not done as part of this study, and therefore it is not known how progressed participants’ disease was at the time of testing positive. However, these results underscore that further work needs to be done to better characterize the HIV epidemic in terms of the HIV treatment cascade among MSW in Vietnam specifically, and to identify opportunities for primary and secondary HIV prevention interventions.
In this study, HIV and gonorrhea prevalence differed significantly by venue of recruitment. Although there is likely some fluidity in venues in which participants meet their clients, these venues may represent specific and perhaps isolated networks, and disease transmission may vary between these networks. Among PWID, risk environments, which include both social-environmental (i.e., physical location of injecting, homelessness), economic (i.e., reliance on sex work for income), and political (i.e., laws providing syringe access and exchange), have been shown to be an important social determinant in HIV transmission [13, 14]. Although to date few studies have considered the risk environment among MSW, among female sex workers (FSW), client-meeting venue are considered a component of the risk environment [9–11]. In southern Vietnam street-based FSW have been found to have twice the prevalence of HIV compared to establishment-based FSW [15]. The organized structure of a brothel may provide more safety compared to outdoor or venue-less MSW [16–18]. Callboys had the highest prevalence of HIV, and bicycle massage MSW had the highest rates of gonorrhea. Call boys typically arranged client meetings via mobile phone, while bicycle massage MSW meet clients in the street. These situations may attract a specific type of clientele or have risk factors (e.g., less access to condom) that are not as prominent in other venues.
About one-sixth of the MSW in the study reported their sexual orientation as heterosexual, and 30 % identified themselves using a Vietnamese slang term meaning “straight boy.” However, 99 % of the MSW reported male clients and HIV infection was not associated with client type, sexual orientation, or gender identity. The heterosexual MSW may have engaged in sex with men only for money, although it is also possible that there was under-reporting of homosexual and bisexual orientation because of stigmatization against sexual minorities in Vietnam. Conversely, the fact that over half of the heterosexuals had anal sex with male partners indicates that sexual roles among men in Vietnam may be less constrained by sexual orientation and sexual identity than in western and other Asian societies.
In the current study, overall use of opiates were low, but was strongly associated with prevalent HIV infection. In Vietnam, the HIV epidemic is heavily concentrated in PWID [3, 19, 20]. Surveillance estimates in HCMC suggest that 46 % of PWID in the city are living with HIV [3]. Previous work in Hanoi has shown complex interrelations between male sex work and injection drug use, with high levels of sexual risk among MSW who also used heroin [21]. Since this study was cross-sectional, it is unknown when participants used opiates with respect to becoming HIV infected. However, these results suggest that consideration should be given to both drug use and sexual behavior as modalities of HIV transmission among MSW in Ho Chi Minh City.
Opiate use was also significantly associated with hepatitis C infection. There were three participants who were infected with hepatitis C and reported injection of opiates. In Vietnam, very high hepatitis C prevalence (31–97 %) has been noted among PWID, as well as high prevalence of HIV [22]. Although a major scale-up of needle and syringe exchange programs started in Vietnam in 2005 [23], and methadone maintenance treatment programs were initiated in 2008 [24], there remains a substantial burden of HIV and hepatitis C among PWID. Attention should be given to ensure that MSW who inject drugs have access to harm reduction interventions as well as HIV and hepatitis C treatment.
Alcohol dependency was not associated not with HIV infection, but was significantly associated with HCV infection and had an inverse association with STIs. It is not clear why alcohol dependency should be protective for STIs, but it may be that increased alcohol use results in less sexual desire and less sex with casual partners outside of commercial encounters, where condom use may be less frequent.
The results of this study must be considered in the context of several limitations. This was a cross-sectional survey, and associations assessed prevalent infections. Temporality cannot be inferred, since it is not known for how long individuals had been infected at the time of testing, or if they had changed behaviors before or after infection. Sexual behavior data were collected via self-report, which could result in social desirability bias. Reporting of previous HIV testing could also be biased by social desirability in that MSW might not want to reveal HIV positive status, which would falsely increase the proportion of HIV positive MSW that were categorized as “newly diagnosed.” STI screening relied on gram stain for diagnosis of gonorrhea and antigen detection for chlamydia. Polymerase chain reaction (PCR) based tests are more sensitive and might have detected a higher proportion of STI, but were not available in Vietnam when the research was conducted.
Due to the low HIV prevalence measured, power was limited in multivariable models to detect significant associations. However, to date few studies have documented HIV, hepatitis C, and STI prevalence and factors associated with these infections among MSW in Vietnam.
The results of this study indicate a relatively high prevalence of HIV among MSW in HCMC, and that a substantial proportion of MSW with HIV are unaware of their infection. Increasing HIV testing, including regular HIV testing, and ensuring that participants with a positive serostatus are linked to care, will be a crucial component in the response to the HIV epidemic in both MSM and MSW. These results have important implications suggesting that both biomedical (HIV testing, ART treatment, and pre-exposure prophylaxis) and behavioral (substance use treatment) interventions may be necessary to adequately address the HIV epidemic in this population.
References
Oldenburg CE, Perez-Brumer AG, Reisner SL, et al. Global burden of HIV among men who engage in transactional sex: a systematic review and meta-analysis. PLoS One. 2014;9:e103549.
Ministry of Health. Results from the HIV/STI integrated biological and behavioral surveillance (IBBS) in Vietnam, 2005–2006. Hanoi: Vietnam Ministry of Health; 2007.
Ministry of Health. Results from the HIV/STI integrated biological and behavioral surveillance (IBBS) in Vietnam - Round II, 2009. Hanoi: Vietnam Ministry of Health; 2011.
Biello KB, Colby D, Closson E, Mimiaga MJ. The syndemic condition of psychosocial problems and HIV risk among male sex workers in Ho Chi Minh City, Vietnam. AIDS Behav. 2014;8(7):1264–71.
Oldenburg C, Biello KB, Colby D, et al. Stigma related to sex work among men who engage in transactional sex with men in Ho Chi Minh City, Vietnam. Int J Public Health. 2014;59(5):833–40.
Colby D, Cao NH. Men who have sex with men and HIV in Vietnam: a review. AIDS Educ Prev. 2004;16(1):45–54.
Mimiaga MJ, Reisner SL, Closson EF, et al. Self-perceived HIV risk and the use of risk reduction strategies among men who engage in transactional sex with other men in Ho Chi Minh City, Vietnam. AIDS Care. 2013;25(8):1039–44.
Oldenburg CE, Biello KB, Colby D, et al. Engagement with peer health educators is associated with willingness to use pre-exposure prophylaxis among male sex workers in Ho Chi Minh City, Vietnam. AIDS Patient Care STDs. 2014;28(3):109–12.
Morisky DE, Pena M, Tiglao TV, Liu KY. The impact of the work environment on condom use among female bar workers in the Philippines. Health Edu Behav. 2002;29:461–72.
Shannon K, Rusch M, Shoveller J, Alexson D, Gibson K, Tyndall MW. Mapping violence and policing as an environmental-structural berrier to health service and syringe availability among substance-using women in street-level sex work. Int J Drug Policy. 2008;19(2):140–7.
Deering KN, Lyons T, Feng CX, et al. Client demands for unsafe sex: the socioeconomic risk environment for HIV among street and off-street sex workers. J Acquir Immune Defic Syndr. 2013;63(4):522–31.
Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505.
Strathdee SA, Hallett TB, Bobrova N, et al. HIV in people who use drugs 1HIV and risk environment for injecting drug users: the past, present, and future. Lancet. 2010;376:268–84.
Rhodes T. Risk environments and drug harms: A social science for harm reduction approach. Int J Drug Policy. 2009;20(3):193–201.
Tran BX, Nguyen TV, Pham QD, et al. HIV infection, risk factors, and preventive services utilization among female sex workers in the Mekong Delta Region of Vietnam. PLoS One. 2014;9(1):e86267.
Toledo CA, Varangrat A, Wimolsate W, et al. Examining HIV infection among male sex workers in Bangkok, Thailand: a comparison of participants recruited at entertainment and street venues. AIDS Educ Prev. 2010;22(4):299–311.
Mimiaga MJ, Reisner SL, Tinsley JP, Mayer KH, Safren SA. Street workers and internet escorts: contextual and psychosocial factors surrounding HIV risk behavior among men who engage in sex work with other men. J Urban Health. 2008;86(1):54–66.
Fujimoto K, Williams ML, Ross MW. Venue-based affiliation networks and HIV risk-taking behavior among male sex workers. Sex Transm Dis. 2013;40(6):453–8.
Tran BX, Nguyen N, Ohinmaa A, et al. Prevalence and correlates of alcohol use disorders during antiretroviral treatment in injection-driven HIV epidemics in Vietnam. Drug Alcohol Depend. 2013;127(1–3):39–44.
Tran TN, Detels R, Long HT, Lan HP. Drug use among female sex workers in Hanoi, Vietnam. Addiction. 2005;100(5):619–25.
Clatts MC, Gian LM, Goldsamt LA, Yi H. Male sex work and HIV risk among young heroin users in Hanoi, Vietnam. Sex Health. 2007;4(4):261–7.
Sereno L, Mesquita F, Kato M, Jacka D, Nguyen TT, Nguyen TN. Epidemiology, responses, and way forward: The silent epidemic of viral hepatitis and HIV coinfection in Vietnam. J Int Assoc Physicians AIDS Care. 2012;11(5):311–20.
Des Jarlais DC, Feelemyer JP, Modi SN, Abdul-Quader A, Hagan H. High coverage needle/syringe programs for people who inject drugs in low and middle income countries: a systematic review. BMC Public Health. 2013;13:53.
Tran BX, Ohinmaa A, Duong AT, et al. Cost-effectiveness of methadone maintenance treatment for HIV-positive drug users in Vietnam. AIDS Care. 2012;24(3):283–90.
Funding
This study was conducted with the support of a pilot Grant from Harvard Catalyst – the Harvard Clinical and Translational Science Center (PIs: DJC and MJM). CEO is supported by a National Institute of Drug Abuse T32 NRSA Grant (T32 DA0131911; PI: Flanigan) and by a Harvard Global Health Institute Fellowship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Donn J. Colby and Catherine E. Oldenburg have contributed equally to the manuscript.
Rights and permissions
About this article
Cite this article
Colby, D.J., Oldenburg, C.E., Nguyen, T. et al. HIV, Hepatitis C, and Other Sexually Transmitted Infections Among Male Sex Workers in Ho Chi Minh City, Vietnam. AIDS Behav 20, 768–775 (2016). https://doi.org/10.1007/s10461-015-1247-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-015-1247-z