Abstract
Iran is facing unprecedented dual drug use and HIV epidemics. We conducted a cross-sectional survey to obtain HIV prevalence and risk behavior data from injection drug users (IDU) in Tehran. We used respondent-driven sampling (RDS) to recruit IDU through successive waves starting with 24 “seeds,” conducted anonymous face-to-face interviews and HIV testing and counseling, and used RDSAT to adjust data. During 44 weeks, 1,726 study referral coupons resulted in 645 (37 %) IDU referrals, of whom 548 (85 %) were enrolled. From those enrolled, 84 % were incarcerated, 47 % employed, 55 % single, 27 % under 30 years of age, and 26 % homeless. The adjusted HIV prevalence was 26.6 % (95 % confidence interval 21.3–32.1), and was higher among certain IDU subgroups (e.g., those who sharing injection paraphernalia). Our estimates of HIV prevalence were higher than some other estimates; however, repeated surveys using similar methodology are needed to monitor the trend of HIV epidemic over time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Iranian Ministry of Health and Medical Education estimates that there are at least 125,000 individuals living with HIV in Iran [1], the large majority of whom are injection drug users (IDU). Traditionally, data on HIV prevalence and incidence, risk behaviors, and the size of the IDU population are based on drug treatment program attendees or prisoners [2–7]. Such data usually are not representative of the larger population of IDU [8]. In a review of studies conducted between 1999 and 2002, HIV sero-prevalence ranged between 1.2 and 24 % among IDU who were incarcerated or attending mandatory drug rehabilitation [9]. Outside of such settings, 23 % of 213 active injectors in a convenience sample in Tehran in 2004 were HIV-infected [10]. A 2003 study in the same geographic area found that the prevalence of HIV infection was 15 % among 170 IDU recruited at three drug treatment centers or through outreach in neighboring areas [6]. Variation in HIV prevalence can be due to type of setting, sampling method, and change in HIV incidence rate among underlying IDU sub-populations across time.
According to the United Nations Office of Drug Control, when all modes of substance use are included, Iran has nearly two million individuals with substance abuse problems [11]. In 2006, the year when this study was implemented, there were approximately 200,000 IDU in Iran [2, 12] half of whom resided in Tehran with population of 9 million inhabitants [13]. The most commonly injected substances are heroin and opium derivatives. Afghanistan, the leading producer of opium and heroin worldwide, lies on Iran’s eastern border, across which hundreds of tons of opium-based drugs are smuggled each year [11, 14]. In recent years, a derivation of heroin in the form of white powder kerack has been commonly used in Iran. Kerack is easier to prepare for injection and may cause withdrawal symptoms in shorter time intervals, meaning that kerack users tend to inject more frequently [15]. IDU in Iran also share needles, hand-made injecting instruments, and other drug paraphernalia in drug shooting venues and inside prisons [10, 12, 15–17]. As a result, the conjunction of the twin epidemics of injecting drug use and HIV in Iran could prove devastating.
To respond to the HIV epidemic, Iran has launched large-scale harm reduction programs promoting opioid substitution treatment (OST), needle exchange program (NEP), outreach, and prison-based programs since 2002 [18–20]. Also, as a result of change in drug policy, several community-based drop-in centers (DIC) were established as points of access for harm reduction services [18] and obtaining clean syringes through pharmacies for drug users was legalized [21]. Between 2006 and 2007, concurrent with the time of data collection for this study, 16 DICs distributed a total of 2,754,000 clean needles or syringes in Tehran (nationally 5,826,00), constituting an annual average of 331 per client per year, and a total of 9,675 clients received outpatient drug treatment services in Tehran through government funded clinics [22].
One barrier to measuring the impact of the current HIV prevention programs, monitoring the trends of the HIV epidemic, and designing more effective prevention programs has been sampling this hard to reach population. HIV infection, HIV-related risk behaviors, and access to prevention programs should be studied among IDU periodically [23–25]. However, obtaining representative samples of IDU and other most at-risk populations (MARP) in Iran is extremely challenging, given that drug use remains illegal, drug users are socially stigmatized [18], and conventional probability-based sampling techniques that require a sampling frame are not a feasible means [8, 26]. As a result, non-probability methods have been the only pragmatic options for sampling MARP [8, 26–29]. In other contexts, respondent-driven sampling (RDS) has been effectively used to sample MARP, including IDU, sex workers, and men who have sex with men for surveys of HIV infection and related risk factors in numerous developing countries [25]. If implemented correctly, RDS can address many of the operational and methodological challenges facing epidemiological surveys of MARP [30–35].
In this paper, we present our findings from the first survey of HIV prevalence and related risk behaviors using RDS among IDU in Tehran. We assess whether RDS was an effective method for recruiting a diverse sample of IDU outside treatment centers, correctional institutions, and social venues. We provide estimates of key demographic characteristics of IDU and the serological prevalence of HIV infection in Tehran.
Methods
Research Setting
The study was conducted between August 2006 and July 2007 in metropolitan Tehran, the capital, economic center, and largest city of Iran. Tehran has approximately 8 million inhabitants [13], is ethnically diverse, and young—nearly half of the population are under 30 years of age. An estimated 100,000 IDU lived in Tehran in that year [12] and are most commonly found in Tehran’s older neighborhoods in the southern, eastern, and central areas of the city [2, 12]. In 2005, we conducted a preliminary study showing that methodological requirements for using RDS in Tehran to study IDU were achievable [15].
Recruitment Sites
We recruited subjects at the Imam Khomeini Medical Center, the largest public general hospital in Tehran, a Tehran University of Medical Sciences (TUMS) affiliate, and a national tertiary care referral center. Our main research site was at the Iranian Research Center for HIV/AIDS (IRCHA), which was in close proximity to an HIV testing and counseling center and the infectious disease ward of the hospital, which serves as the national reference center for HIV/AIDS.
Fourteen weeks after the initial recruitment period, we added three additional recruitment sites in three community-based organization drop-in-centers. These centers provide social support (i.e., a place for socialization, warm meals, and tea) and basic prevention and treatment services to IDU, including methadone maintenance treatment, drug detoxification, HIV counseling (with referral for testing), distribution of free condoms and clean needles, basic medical care (with referral to specialists), and wound care. The centers were located in three geographically disparate parts of the city. All served 150–300 men, women, IDU, and non-injecting drug users daily.
Study Subjects
The target population was active adult IDU in greater Tehran. We defined eligible participants as persons who self-reported injecting any illicit drugs within the prior 30 days, were at least 18 years old at the time of the interview, presented a study referral card (or coupon) at the time of enrollment, reported receiving their coupons in greater Tehran, and provided verbal informed consent for both serological tests and behavioral components of the survey. We excluded individuals who had no signs of injection (e.g., track marks, scars) in visible areas of the body and did not report injecting in genital areas, failed to accurately describe the process of preparing their drug of choice for injection, or were not able to provide informed consent due to mental disorientation or being under the influence of drugs.
Subject Recruitment Procedure
The study participants were sampled using RDS. The methods of RDS have been described in detail elsewhere [36, 37]. We identified seeds through outreach in IDU communities and by recruiting IDU who were attending IRCHA or seeking referrals from the drop-in centers. The study was conducted anonymously. Eligible seeds were enrolled into the study after providing verbal informed consent for both the serological and behavioral components of the survey. The seeds received an initial monetary incentive of 500 Toomans (approximately $0.53), a hygienic package (clean syringes, condoms, cotton, medical alcohol, educational brochure, and the addresses of HIV testing and counseling centers), a laboratory test results card, three study referral coupons, and instructions on how they should use the coupons to refer other IDU to our study. Each coupon had the project name, location, contact information, expiration date (30 days after the issuance date), and a unique ID code that was used to link recruits and recruiters. For each eligible participant who completed the survey, the recruiter would receive a secondary incentive of 1,000 Toomans (approximately $1.07). The incentive was disbursed based on the presentation of their study ID number, which was linked by code to the three referral coupons. We used coupon-management software to keep track of who recruited whom, as needed for statistical adjustments in the RDSAT analysis software [38].
During the initial phase of the survey (the first 14 weeks) we recruited 14 seeds at the IRCHA site, but they referred only five eligible subjects. During week 15, we increased the amount of the primary incentive to 2,000 Tooman (approximately $2.14), expanded interviewing to the three drop-in centers, and recruited 10 new seeds from those centers.
Referred participants (recruits) were asked to recruit other members of their networks using the same system of coupons and incentives. Given that participation was anonymous, we used several methods to limit repeat participation. First, once a participant was referred to the recruitment site, we checked the validity of his or her coupon, date of birth, and used a series of questions to create a 12-digit code composed of four characters (initials of the first name, last name, mother’s maiden name, and the city of birth. We also collected a series of biological measures including length of the right arm, height, weight, and circumference of the left wrist, hair color, and presence of body tattooing. We stored these data in a searchable database that enabled us to screen potential repeat participants. Additionally, we used one staff member to conduct the initial screenings for the majority of the participants, so that she would be able to spot repeat participants.
Data Collection Tool
The behavioral survey was conducted face-to-face using four interviewers (three men, all of whom were ex-IDU and two of whom were HIV-infected, and one woman, who was a social worker serving female sex workers and drug users). All staff members and interviewers received intensive training about the basic concepts of the study, neutral and non-judgmental techniques to increase validity of answers, methods to build appropriate interpersonal relationships, and ethical codes with emphasis on anonymity and confidentiality of the participants’ information. Our questionnaire was modeled on two pre-existing questionnaires: the IDU module of the Family Health International Behavioral Surveillance Survey [39] and a previously used local survey implemented among IDU at drug treatment facilities by Zamani et al. [6]. Survey topics included: demographic characteristics, network information, drug use, needle and equipment sharing behaviors, detention history, sexual history, sexually transmitted disease history, condom use, use and assessment of HIV and substance use services, experiences of stigma and discrimination, and HIV/AIDS knowledge, attitudes, beliefs and practices.
HIV Counseling and Testing
A counselor/phlebotomist conducted a 10-min HIV pre-test counseling session and drew 8 ml of venous blood. Serological screening was done for HIV by EIA (Anti-HIV Tetra ELISA, Biotest, Germany) per the manufacturer’s directions. HIV results were confirmed by Western blot (MP Diagnostics, Geno labs Diagnostics, Germany & Singapore). After HIV testing, trained physicians disclosed results and provided counseling. Subjects were offered multiple opportunities to obtain their test results. Persons who tested HIV positive and returned to receive their test results were referred to HIV care services at Imam Khomeini Medical Center for further follow-up.
Data Management and Analysis
Our initial calculated sample size was 762 based on detecting HIV prevalence of 10 % among IDU in Tehran, considering a design effect of 2.0, a two-sided alpha of 0.05, and a 3 % margin of error. We entered data into a Microsoft Access database and crosschecked for validity. We exported the data into the RDSAT software version 5.6 for univariate analysis to calculate adjusted point prevalence estimates with 95 % confidence intervals. We used the “enhanced data smoothing” option and set the bootstrapping re-sampling to 15,000. We imputed the median network size for five participants whose data were missing based on their demographic variables, and excluded all seeds from final data analysis.
Results
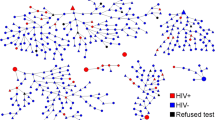
From 24 total seeds, nine (37.5 %) referred at least one eligible IDU. The maximum referral wave generated by a seed was 34. Over the course of the 44 weeks of fieldwork, we distributed a total of 1,726 coupons, from which 645 (37 %) individuals volunteered to participate in our study. From these 645 participants, 97 became ineligible, most of whom (90 %) were non-injecting drug users and the rest did not have study referral coupons. In the end, 548 (85 %) non-duplicated subjects met the eligibility criteria and were consented and enrolled. Figure 1 demonstrates recruitment pattern by HIV sero-status. While 14 seeds did not recruit any new participants, a large portion of IDU were recruited by three initial seeds. Cross HIV status recruitment (HIV positive IDU recruiting HIV negative IDU and visa versa) was common. Our sample reached equilibrium on multiple demographic characteristics; that is, the composition of the sample stabilized on certain key variables including age, education, and employment. Our sample was predominantly male (99.8 %) and ranged in age from 20 to 60 years, with a quarter of the sample being less than 30 years of age (Table 1). Forty-five percent had never been married, and 47 % reported being employed at the time of interview. Two female seeds did not recruit any other participants, and only two female IDU were referred to our study and completed survey.
Chain of recruitment in injection drug users participated in our respondent-driven sampling survey in Tehran, Iran 2006–2007 (total n including seeds = 570). Shape of nodes represents the recruitment role of IDU (square seed, circle recruited). Size of shapes reflects self-reported network size. Arrow represents the recruitment pattern. Color represents HIV sero-status (Red HIV positive, Green HIV negative, Yellow indeterminate) (Color figure online)
Of 544 IDU with known HIV results, 127 (23.3 %) were infected. The RDSAT-adjusted HIV sero-prevalence was 26.6 % (21.3–32.1 %). HIV prevalence was higher among participants from south-central region of Tehran (33 %), the illiterate (61 %), and those from the Fars ethnic group (60 %) (Table 2). Prevalence among those who had ever been incarcerated (27 %) was similar to those who had not (25 %). Prevalence was also higher among those who reported that they had been tattooed using shared equipment (42 %) and, in the subsample that had injected in the prior month, those who reported that they “always or most of the time” shared drug paraphernalia (25 %) (Table 3). IDU who reported certain sexual risk behaviors including “ever visiting a sex worker,” “exchanging sex for money or drugs,” “having had sex with other men,” and “had multiple lifetime sexual partners” had HIV infection rates similar to those without these behaviors.
Discussion
We found that 26.6 % of IDU in Tehran were HIV infected. This was the first survey to use RDS to study IDU in Iran, and it has recruited the largest sample of IDU reported in Iran in 2006. We have demonstrated that RDS is a feasible and effective tool to sample IDU in Iran if incentive amounts are carefully set, a trusted community-based organization is involved and—in a large city like Tehran—recruitment sites are decentralized.
Our study population differed somewhat from those in two studies conducted by Zamani et al. [6, 10], which used convenience and venue-based samples. After adjustment, our RDS sample had fewer IDU less than 30 years of age (27 vs. 49 % in 2003 and 36 % in 2004), was more ethnically heterogeneous (only 33 % were Fars in our study as compared with 60–63 %), was less likely to be unemployed, and was less illiterate. Furthermore, our sample, which theoretically is representative of IDU in Tehran, found significantly higher HIV prevalence (15.2 %) than Zamani’s 2003 convenience sample from drug treatment centers and slightly higher prevalence (24 %) than his 2004 venue-based sample. This finding contradicts the expectation that we had when we started the study that a community-based sample would have a lower prevalence because of its ability to reach out to a more diverse sample of IDU.
In Table 4, we compared characteristics of participants in our study with two other HIV bio-behavioral surveys that were also conducted among IDU in Tehran during 2006–2007: (1) Rahimi-Movaghar et al. who sampled from five communities and five clinics [4], and (2) Kheirandish et al. who sampled from mandatory drug rehabilitation center [7, 40]. We observed overall similarities in characteristics of IDU who participated in these three studies with respect to age, sex, education, being resident of Tehran, and history of incarceration. However, HIV prevalence of our study was very close to estimates from Kheirandish (24 %) [7] but significantly higher than Rahimi-Movaghar (10.5 %) [4]. One explanation for this finding can be that both our study and Kheirandish’s study reached sub-populations of IDU with higher risk behaviors and less access to harm reduction services compared to those who participated in Rahimi-Movaghar’s 2010 study.
We found that a history of tattooing with shared equipment and recent (last month) history of sharing drug paraphernalia were associated to a higher HIV prevalence among IDU. However, many other well-known behavioral risk factors (visiting sex workers, exchanging sex for money, lifetime of sharing syringes or needles for injection) were not associated with higher HIV prevalence among IDU, possibly owing to sample size constraints.
Our study had similar limitations noted in other studies that have used RDS. Some IDU subpopulations may have been underrepresented because they either did not have strong social ties with other IDU or were reluctant to participate. Although there is some evidence that 5 % of IDU in Iran are female, and despite expenditures of extra effort to recruit women, only two female IDU were referred to our study. Additionally, our formative study indicated that we should have found Afghan IDU in Tehran, but none appeared in our sample. More qualitative research is needed to explore the barriers to participations of IDU subpopulations that we did not reach and understand whether or not these populations are actually networked, tease out if the behavior is considered too stigmatized to use RDS in this context, and identify alternative sampling methods to access them. Another limitation of our study is the lack of sufficient statistical power to measure the prevalence of some variables with greater precision. This is most evident among women.
It took 44 weeks to recruit 548 eligible IDU (average 12 IDU/week). There are several explanations for this slow recruitment. First, we started the recruitment process utilizing only a single site in the central part of Tehran to ensure good access for all potential participants. Tehran is considered a megacity with heavy street traffic during daytime hours, causing long travel times from the city’s perimeter to the center. Second, the monetary incentive initially designated for participation was not sufficient to cover the cost of round trip transportation for all participants. To respond to these issues, we recruited 10 new seeds, doubled the amount of initial and secondary incentives, and launched three new and geographically scattered recruitment sites 14 weeks after the initial recruitment. Although these changes significantly increased the pace of the recruitment process, recruitment slowed down again almost 10 weeks after these changes (Week 25) due to antidrug police activists with active checkpoints in main streets and intersections throughout the city.
Nonetheless, we were able to recruit a large sample; the number of participants in our study was the second largest among 65 RDS-based surveys of IDU worldwide in 2006 [30]. Calculating an accurate sample size for RDS-based surveys has remained a challenge, but it is important to note that we inflated our calculated sample size twofold, taking into account a design effect of 2.0 [41]. Among 91 RDS-based surveys that were conducted among MARPs in developing countries, only 34 (38 %) had used a design effect of >1.5 in the sample size calculation [30].
This was the first implementation of the RDS method in the context of IDU in Iran in which we were able to demonstrate the feasibility of RDS in 2006. Our study contributed to the adoption of RDS methods to conduct several other HIV bio-behavioral surveys among MARPs in Iran. In order to incorporate RDS in Iran’s national HIV surveillance program, more data must be gathered on the cost, time, and human resource needs associated with the use of RDS and its operational advantages compared to other methods. Our community-based sample reported the highest level of HIV prevalence among male IDU in Tehran. More research is necessary to verify our observed figures as well as to study HIV prevalence and risk behaviors among Iranian women and ethnic subgroups.
References
MOHME-CDM. The latest statistics of HIV/AIDS in Islamic Republic of Iran. Center for Disease Management, Ministry of Health and Medical Education, Islamic Republic of Iran; 2013.
Razzaghi E, Rahimi-Movaghar A. Rapid assessment and responses: multi-center project on injection drug use in Tehran. Tehran: World Health Organization; 2003.
Rahimi-Movaghar A, Amin-Esmaeili M, Haghdoost AA, Sadeghirad B, Mohraz M. HIV prevalence amongst injecting drug users in Iran: a systematic review of studies conducted during the decade 1998–2007. Int J Drug Policy. 2012;23(4):271–8.
Rahimi-Movaghar A, Razaghi EM, Sahimi-Izadian E, Amin-Esmaeili M. HIV, hepatitis C virus, and hepatitis B virus co-infections among injecting drug users in Tehran, Iran. Int J Infect Dis. 2010;14(1):e28–33.
Zamani S, Farnia M, Torknejad A, et al. Patterns of drug use and HIV-related risk behaviors among incarcerated people in a prison in Iran. J Urban Health. 2010;87(4):603–16.
Zamani S, Kihara M, Gouya MM, et al. Prevalence of and factors associated with HIV-1 infection among drug users visiting treatment centers in Tehran, Iran. AIDS. 2005;19(7):709–16.
Kheirandish P, Seyedalinaghi SA, Hosseini M, et al. Prevalence and correlates of HIV infection among male injection drug users in detention in Tehran, Iran. J Acquir Immune Defic Syndr. 2010;53(2):273–5.
Magnani R, Sabin K, Saidel T, Heckathorn D. Review of sampling hard-to-reach and hidden populations for HIV surveillance. AIDS. 2005;19(Suppl 2):S67–72.
Feizzadeh A, Nedjat S, Asghari S, et al. Evidence-based approach to HIV/AIDS policy and research prioritization in the Islamic Republic of Iran. East Mediterr Health J. 2010;16(3):259–65.
Zamani S, Kihara M, Gouya MM, et al. High prevalence of HIV infection associated with incarceration among community-based injecting drug users in Tehran, Iran. J Acquir Immune Defic Syndr. 2006;42(3):342–6.
UNODC. Epidemiology of drug use in Iran. 2008. http://www.unodc.org/iran/en/epidemiology.html. Accessed 14 May 2014.
Razzaghi EM, Movaghar AR, Green TC, Khoshnood K. Profiles of risk: a qualitative study of injecting drug users in Tehran, Iran. Harm Reduct J. 2006;3:12.
Tehran-Municipality. 2008. http://www.tehran.ir/Default.aspx?tabid=2213. Accessed Aug 30 2008.
March JC, Oviedo-Joekes E, Romero M, et al. The experimental drug prescription program in Andalusia [PEPSA]: procedure for recruiting participants. Gac Sanit. 2004;18(3):245–7.
Razani N, Mohraz M, Kheirandish P, et al. HIV risk behavior among injection drug users in Tehran, Iran. Addiction. 2007;102(9):1472–82.
Vazirian M, Nassirimanesh B, Zamani S, et al. Needle and syringe sharing practices of injecting drug users participating in an outreach HIV prevention program in Tehran, Iran: a cross-sectional study. Harm Reduct J. 2005;2:19.
Zamani S, Vazirian M, Nassirimanesh B, et al. Needle and syringe sharing practices among injecting drug users in Tehran: a comparison of two neighborhoods, one with and one without a needle and syringe program. AIDS Behav. 2010;14(4):885–90.
Nassirimanesh B, Trace M, Roberts M. The rise of harm reduction in the Islamic Republic of Iran. International Drug Policy. 2005;2006
Malekinejad M, Vazirian M. Transition to injection amongst opioid users in Iran: implications for harm reduction. Int J Drug Policy. 2012;23(4):333–7.
Razzaghi E, Nassirimanesh B, Afshar P, Ohiri K, Claeson M, Power R. HIV/AIDS harm reduction in Iran. Lancet. 2006;368(9534):434–5.
Razzaghi EM, Movaghar AR, Green TC, Khoshnood K. Profiles of risk: a qualitative study of injecting drug users in Tehran, Iran. Harm Reduct J. 2006;3:12.
Noroozi A, Shamshiri A. Geographical distribution of mental, social, and addiction in 2007: substance use version. Tehran, Iran: Iranian Ministry of Health and Medical Education, Office of Mental and Social Health and Addiction. 2007.
UNAIDS/WHO/Working Group on Global HIV/AIDS and STI Surveillance. Second generation surveillance for HIV: the next decade. In: Joint United Nations Programme on HIV/AIDS WHO, ed. Geneva, Switzerland: (WHO/CDS/CSR/EDC/2000.5|UNAIDS/00.03E); 2000.
Rehle T, Lazzari S, Dallabetta G, Asamoah-Odei E. Second-generation HIV surveillance: better data for decision-making. Bull World Health Organ. 2004;82:121–7.
Pisani E, Lazzari S, Walker N, Schwartlander B. HIV surveillance: a global perspective. J Acquir Immune Defic Syndr. 2003;32(Suppl 1):S3–11.
Schwartlander B, Ghys PD, Pisani E, et al. HIV surveillance in hard-to-reach populations. AIDS. 2001;15(Suppl 3):S1–3.
Hoda Z, Kerr T, Li K, Montaner JS, Wood E. Prevalence and correlates of jugular injections among injection drug users. Drug Alcohol Rev. 2008;27(4):442–6.
Dunn J, Ferri CP. Epidemiological methods for research with drug misusers: review of methods for studying prevalence and morbidity. Rev Saude Publica. 1999;33(2):206–15.
Thomas JC, Isler MR, Carter C, Torrone E. An interagency network perspective on HIV prevention. Sex Transm Dis. 2007;34(2):71–5.
Malekinejad M, Johnston LG, Kendall C, Kerr LR, Rifkin MR, Rutherford GW. Using respondent-driven sampling methodology for HIV biological and behavioral surveillance in international settings: a systematic review. AIDS Behav. 2008;12(4 Suppl):S105–30.
Johnston L, Khanam R, Reza M, et al. The effectiveness of respondent driven sampling for recruiting males who have sex with males in Dhaka, Bangladesh. AIDS Behav. 2008;12(2):294–304.
Johnston LG, Sabin K, Mai TH, Pham TH. Assessment of respondent driven sampling for recruiting female sex workers in two Vietnamese cities: reaching the unseen sex worker. J Urban Health. 2006;83(6 Suppl):i16–28.
Stormer A, Tun W, Guli L, et al. An analysis of respondent driven sampling with injection drug users (IDU) in Albania and the Russian Federation. J Urban Health. 2006;83(6 Suppl):i73–82.
Yeka W, Maibani-Michie G, Prybylski D, Colby D. Application of respondent driven sampling to collect baseline data on FSWs and MSM for HIV risk reduction interventions in two urban centres in Papua New Guinea. J Urban Health. 2006;83(6 Suppl):i60–72.
Mohkrie A. Brief overview of the status of drug abuse in Iran. Arch Iran Med. 2003. http://www.ams.ac.ir/. Accessed 30 Aug 2008.
Heckathorn D. Respondent driven sampling: a new approach to the study of hidden population. Soc Probl. 1997;44(2):174–99.
Heckathorn D, Semaan S, Broadhead R, Hughes J. Extensions of respondent-driven sampling: a new approach to the study of injection drug users aged 18–25. AIDS Behav. 2002;6(1):55–67.
Heckathorn DD. Respondent driven sampling. [Website]. 2008. Articles and free software related to RDS. http://www.respondentdrivensampling.org. Accessed 20 Aug 2008.
FHI. Behavioral surveillance surveys: guidelines for repeated behavioral surveys in populations at risk of HIV. 2000. http://www.fhi.org/en/hivaids/pub/guide/bssguidelines.htm. Accessed 30 Sep 2008.
Hosseini M, SeyedAlinaghi S, Kheirandish P, et al. Prevalence and correlates of co-infection with human immunodeficiency virus and hepatitis C virus in male injection drug users in Iran. Arch Iran Med. 2010;13(4):318–23.
Salganik MJ. Variance estimation, design effects, and sample size calculations for respondent-driven sampling. J Urban Health. 2006;83(6 Suppl):i98–112.
Acknowledgments
We would like to thank to the directors of the drop-in centers, Aeen Mehr I, Aeen-Mehr II, and Azadi, the Boo-Ali Triangular Center, and the Persepolis Institute for their collaboration, and the staff of the IRCHA, who provided logistical support throughout the study. We also would like to express our gratitude to Dr. Azarakhsh Mokri and Dr. Mohsen Vazirian at the Iranian National Center for Addiction Studies at TUMS who provided their expertise, and to Dr. Hossein Kayvan who conducted serological tests. This research project was supported by a Grant from the World Health Organization-Eastern Mediterranean Regional Office/Tropical Disease Research Programme small grant (Small Grants AMS Code 1: 43119022 and AMS Code 2: 43119040), TUMS Office of the Deputy of Research (Grant No. 3895-55-02-85); and the John P. Dowdle Endowment and the Russell M. Grossman Medical Research Fund of the School of Public Health, University of California, Berkeley.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Malekinejad, M., Mohraz, M., Razani, N. et al. High HIV Prevalence in a Respondent-Driven Sampling Survey of Injection Drug Users in Tehran, Iran. AIDS Behav 19, 440–449 (2015). https://doi.org/10.1007/s10461-014-0904-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-014-0904-y