Abstract
Learning to take safe and effective action in complex settings rife with uncertainty is essential for patient safety and quality care. Doing so is not easy for trainees, as they often consider certainty to be a necessary precursor for action and subsequently struggle in these settings. Understanding how skillful clinicians work comfortably when uncertain, therefore, offers an important opportunity to facilitate trainees’ clinical reasoning development. This critical review aims to define and elaborate the concept of ‘comfort with uncertainty’ in clinical settings by juxtaposing a variety of frameworks and theories in ways that generate more deliberate ways of thinking about, and researching, this phenomenon. We used Google Scholar to identify theoretical concepts and findings relevant to the topics of ‘uncertainty,’ ‘ambiguity,’ ‘comfort,’ and ‘confidence,’ and then used preliminary findings to pursue parallel searches within the social cognition, cognition, sociology, sociocultural, philosophy of medicine, and medical education literatures. We treat uncertainty as representing the lived experience of individuals, reflecting the lack of confidence one feels that he/she has an incomplete mental representation of a particular problem. Comfort, in contrast, references confidence in one’s capabilities to act (or not act) in a safe and effective manner given the situation. Clinicians’ ‘comfort with uncertainty’ is informed by a variety of perceptual, emotional, and situational cues, and is enabled through a combination of self-monitoring and forward planning. Potential implications of using ‘comfort with uncertainty’ as a framework for educational and research programs are explored.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Authentic clinical reasoning requires practitioners to collect and interpret imperfect data in real time. Learning how to take safe and effective action in these complex and ambiguous settings is essential for patient safety and high-quality care (Fargason et al. 1997; Hartmann 1998; Luther and Crandall 2011; Simpkin and Schwartzstein 2016). Thus, health professions educators often express concerns that students struggle with ambiguity and uncertainty (Fargason et al. 1997; Luther and Crandall 2011; White and Williams 2017), and instead strive to impose certainty on inherently ambiguous situations (Geller 2013; Lingard et al. 2003; Simpkin and Schwartzstein 2016). As a result, there are ongoing calls to help learners develop “positive” responses to uncertainty and ambiguity (White and Williams 2017).
To act with confidence while simultaneously remaining uncertain is a paradox that epitomizes expert practice. Thus, understanding how skillful clinicians are able to enact this paradox could offer an important first step toward providing educators with the guidance they need to support trainees’ development of clinical reasoning. In particular, there is little in the medical education literature regarding how physicians manage uncertainty arising from complex, ill-defined problems where “there are conflicting assumptions, evidence, and opinion which may lead to different solutions” (Kitchener 1983, p. 223). Cristancho has argued that these ill-defined problems are characterized by the need for clinicians to continuously reconstruct and redefine their understanding of the problem, even as they are trying to solve it (Cristancho et al. 2017). Yet the processes and mechanisms that enable clinicians to maintain a sense of comfort (or not) when continuing along in these moments of uncertainty in ill-defined problems remains largely unexplored. Thus the question is: how do clinicians become sufficiently comfortable dwelling in these “swampy lowlands of indeterminate practice” (Schön 1983, p. 42), remaining confident that their continued efforts will result in greater diagnostic clarity or resolve their patients’ problems altogether?
The purpose of this critical review, therefore, is to explore what it means to be ‘comfortable’ when working in ill-defined clinical situations while feeling ‘uncertain.’ We will elaborate the concept of ‘comfort with uncertainty’ using a variety of frameworks and theories, examining what is meant by ‘uncertainty’ and ‘ambiguity,’ and what it means to feel ‘comfortable’ in these situations. We will then illustrate how the concept of ‘comfort with uncertainty’ manifests in clinical medicine, provide an analysis of potential mechanisms that might facilitate a feeling of comfort in the face of uncertainty, and conclude with implications of this analysis for medical education practice and future research.
Method
To explore this problem space, we conducted a critical synthesis of relevant literature and theoretical frameworks. Although comprehensiveness is not the goal in critical synthesis (Grant and Booth 2009), we nonetheless sought empiric and theoretical work beyond our a priori knowledge by methodologically searching published literature. We first used Google Scholar to identify theoretical concepts and findings relevant to the topics of ‘uncertainty,’ ‘ambiguity,’ ‘comfort,’ and ‘confidence.’ We then used the search terms identified through this process to pursue parallel searches within the fields of social cognition, cognition, sociology, sociocultural, philosophy of medicine, and medical education, utilizing the following databases: Academic Search Premier, Biomedical Reference Collection: Comprehensive, CINAHL, Dissertation abstracts, ERIC, MEDLINE, PsycINFO, SocINDEX and Web of Science.
Results
Defining comfort with uncertainty
In exploring the phrase ‘comfort with uncertainty,’ we found a lack of specificity in how the terms ‘uncertainty’ and ‘comfort’ are used in published literature. Thus, in this section we will discuss and clarify each of these terms individually, and then propose an operational definition of what clinicians mean when they say ‘comfort with uncertainty.’
The term ‘uncertainty,’ as applied to ill-defined problems in medicine, is frequently used in ways that do not sufficiently distinguish between the properties of the situation and the ‘lived experience’Footnote 1 of the individual (Atkinson 1984; Babrow et al. 1998; Djulbegovic et al. 2011; Fox 1957; Lazarus 1991; Lazarus and Folkman 1984; Light 1979; Lipshitz and Strauss 1997; Mishel 1988, 1990; Schraw et al. 1995; Schwartz and Griffin 1986; Simpkin and Schwartzstein 2016; Simpson et al. 1986). In fact, the term ‘uncertainty’ is often used interchangeably with the term ‘ambiguity’ (Geller 2013; White and Williams 2017). To draw this important distinction between the situation and the lived experience more explicitly, we propose using ‘ambiguity’ to represent the properties of the situation and ‘uncertainty’ to represent the lived experience of an individual. Thus, we will consider some thing, be it an image, a sound, or a constellation of clinical findings, to be inherently ambiguous if it can be interpreted in two or more distinct ways by different individuals, or by the same individual at different moments in time (Dogra et al. 2007; Levine 1985; Rensink et al. 1997; Simons and Chabris 1999). For example, a heart sound that might or might not indicate a murmur is ‘ambiguous.’ In contrast, we will preserve the term ‘certainty’ to reference the lived experience of the individual, describing the extent to which one feels confident in one’s representation of the underlying cause of a particular problem or situation (e.g., the pathology causing a patient’s illness). Certainty is expressed whenever a clinician says things like “this patient’s symptoms are from granulomatosis with polyangiitis” or “this patient’s otitis media will get better without antibiotics.” In contrast, ‘uncertainty’ represents a state of tentativeness with regard to one’s conception of the underlying causes of a patient’s symptoms. This can arise from recognizing that a situation is ambiguous (Babrow et al. 1998; Lazarus and Folkman 1984), from perceived limitations in one’s own knowledge (Fox 1957), or from recognition that one has incomplete information (Light 1979).
If ‘certainty’ represents one’s confidence in interpreting a clinical situation, ‘comfort’ references the confidence one feels in being capable of acting (or deciding to wait and watch) safely and effectively in a given situation (Barbalet 1993; Eva and Regehr 2005). Thus, for example, comfort is expressed when a clinician confidently chooses to write a prescription, enact a particular procedure, or withhold action while observing a patient. In each case, the individual is exhibiting a willingness to ‘manage a problem,’ at least through its most imminent stages. By contrast, ‘discomfort’ is likely to arise because one is concerned that the demands of the situation outstrip one’s capacity to deal with it (LeBlanc 2009; LeBlanc et al. 2015). This can occur, for example, because a clinician has not dealt with a particular problem before (or for a long period of time), or because a clinician feels that something needs to be done while simultaneously believing the appropriateness of a particular management plan is dependent on knowing the yet unknown root cause of the issue (Light 1979).
In short, for the purposes of this analysis, we will define ‘certainty’ as the confidence in one’s interpretation of a clinical situation and we will define ‘comfort’ as the confidence in one’s ability to act (or choose to continue monitoring the situation without direct action). Accordingly, ‘comfort with uncertainty,’ can be operationally defined as the phenomenological lived experience of having the confidence to act on a problem (or wait and observe) in the absence of full confidence in one’s understanding of the underlying cause of the issue. Parenthetically, we note that this also would allow us to acknowledge the state of being ‘certain but uncomfortable’ in which one perceives a clear understanding of the problem and realizes that one is not capable of managing it.
Circumstances that embody comfort with uncertainty
Having developed a definition of ‘comfort with uncertainty’ in the context of ill-defined problems, we next sought to use the literature to explore various manifestations of this construct in clinical practice. We identified two broad categories that could be considered manifestations of ‘comfort with uncertainty’ that are framed around the source of uncertainty: uncertainty regarding the diagnosis and uncertainty regarding the treatment plan. Each is elaborated below, although we note that the current literature does not allow us to make claims regarding the prevalence, variety of manifestations, or degree of risk associated with either.
Letting go of the need to know
The first form of ‘comfort with uncertainty’ organizes around comfort with a management plan in the face of uncertainty regarding the diagnosis. In some cases, this involves accepting the ongoing possibility of a less common or rare diagnosis that could only be excluded through expensive or risky diagnostic tests. Although these less likely diagnoses are theoretically possible, seriously considering them would likely take clinicians down paths that are neither feasible nor in patients’ best interests (Jha 2014). Skillful clinicians thus comfortably adopt the position of conscious inaction toward these rare diagnoses (Jha 2014; Smith and Paauw 2000). They hone their management plans towards a more probable and limited subset of diagnoses while remaining alert to changes (or lack thereof) in patients’ clinical status that would suggest the need to more seriously consider improbable diagnoses.
In other cases that involve ‘comfort with uncertainty’ regarding diagnosis, it is not necessary to tease apart confusable diseases that manifest with similar symptoms because one can comfortably use symptom-focused management strategies that focus on ‘what will work’ without the need for diagnostic precision (Bordage and Lemieux 1991; Bowen 2006). That is, clinicians can comfortably adopt a pragmatic treatment-oriented categorization of illness, grouping a subset of possible diagnoses in ways that allow them to confidently initiate empiric therapies that have a high probability of success while remaining uncertain about the actual diagnosis. In these situations, perfect certainty regarding diagnosis is not a goal because it is not necessary for action. Instead, clinicians monitor their patients’ progress to ensure they are indeed achieving the anticipated outcomes, and pivot towards further evaluation or a change in management if the illness progression deviates from the anticipated path.
Feeling your way through a problem
A second form of ‘comfort with uncertainty’ takes place under circumstances of greater ambiguity, complexity, and acuity where definitive management strategies are less clear. In these situations where multiple conceptualizations of an illness remain possible (Cristancho et al. 2017), multiple management approaches also remain reasonable. Clinicians’ ‘comfort’ in these settings reflects feeling able to take a reasonable next step in managing the situation at hand despite not being certain that it will lead to the desired outcome. Indeed, clinicians might consciously remain uncertain, recognizing that their initial steps in management will likely provide additional data that will enhance their understanding of a situation.
When clinicians act in this way they are engaging in an exercise of “pragmatic empiricism” (Atkinson 1984, p. 954), using symptom evolution and treatment responses as additional data to frame and reframe problems, and shifting management strategies based upon how a patient’s illness evolves under their care (Cristancho et al. 2013a, 2016). For example, an emergency physician may preliminarily classify a patient as having “acute respiratory distress,” lacking certainty whether these symptoms are secondary to a diagnosis of congestive heart failure, pneumonia, or a number of other pulmonary pathologies. Classifying the situation as an ill-defined problem rather than a specific diagnosis provides an initial roadmap for immediate actions (e.g., pulse oximetry, cardiac monitoring) and helps to plan for future potentially-necessary actions (e.g., bringing intubation equipment to the bedside; Zilbert et al. 2015a). It also provides a framework for tentative treatments, the response to which clinicians use to better understand a situation. For example, an effective dose of a diuretic may affirm a clinician’s hypothesis that her patient’s shortness of breath is from congestive heart failure. In contrast, a therapeutically-ineffective dose of this medication is unlikely to cause long-lasting harm and may help her to consider alternative diagnoses.
Engaging with this form of uncertainty is thus akin to walking down a familiar dark path: it involves the recognition that even if a problem definition remains elusive, it is a problem within one’s realm of expertise (Zilbert et al. 2015b). Skillful clinicians therefore assume the risks of engaging with these ill-defined problems, feeling comfortable that even if a multitude of potential problems, risks, and management paths remain possible, their skillset will enable them to manage these complexities safely and effectively in the absence of certainty.
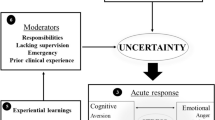
Conditions and processes that facilitate comfort with uncertainty
Having identified several circumstances that embody comfort with uncertainty in the context of ill-defined problems in clinical practice, we turn to the processes that might facilitate such comfort. To frame this discussion, Koriat’s dual-basis view of metacognitive judgments proved particularly generative. This model, developed to explain individuals’ judgments of their own learning (Koriat 1997), suggests that people use cues drawn from both their lived experience in the moment (e.g., their current subjective feelings that manifest when engaging in a task) and their theories about the situation (e.g., their beliefs about how memory works based on assumptions built from the accrual of previous experiences) to make a judgment about whether or not they have learned a set of materials. For Koriat, an “experience-based cue”Footnote 2 might be the ease with which the material is read, with individuals interpreting their reading fluency in the moment of reading as mastery of the material (Koriat 1997; Koriat et al. 2005). A “theory-based cue” might be drawn from the belief that reading the material multiple times enables one to remember it, such that if one has read the material several times, one feels increased confidence that one must know it (Koriat et al. 2005). Our review of the literature around ‘comfort with uncertainty,’ suggests that such experience-based and theory-based cues are likely to be similarly influential when making judgments about one’s comfort when facing uncertainty. We elaborate on these connections below.
Experience-based cues that influence feelings of comfort with uncertainty
Experience-based cues come directly from an individual’s internal lived experience when engaging in a clinical reasoning situation in the moment. For example, as alluded to above, the cognitive psychology literature suggests that perceived fluency (i.e., how easily one is able to read and understand a text) is used as a cue for the extent to which one has mastered new material that one is trying to learn (Begg et al. 1989; Rawson and Dunlosky 2002). In a similar way, clinicians likely use the ease with which they are able to listen to and think about patients’ problems as cues for the extent to which they have mastery of the situation, drawing on perceptions that ‘this is going well’ and ‘this is what I expected to happen’ (Cristancho et al. 2017; de Bruin et al. 2017), even if they are as yet uncertain of the end game. A broad set of accrued experiences, the development of automaticity, and processes of encapsulation are likely important factors in determining this perception of fluency (Reber and Greifeneder 2017). With accrued experience, a range of plausible explanatory models, possible actions, and implications of these various possibilities are more likely to arise, in part explaining why seasoned clinicians are likely to feel more comfortable than novices in the face of uncertainty.
The identification of these experience-based cues is represented in the medical education literature under the construct of monitoring. Moulton and colleagues, for example, have described a process of remaining “attentive in automaticity”(Moulton et al. 2010b), combining situational awareness with meta-cognition as a means to “remain aware of the whole situation, to monitor events as they occur, [and] to reflect on alternative possibilities should a decision need to be made” (Dunphy and Williamson 2004, p. 108). Similarly, Eva and Regehr have described a moment-by-moment self-monitoring process regarding one’s factual knowledge as a mechanism for “knowing when to look it up” (Eva and Regehr 2007). This idea of monitoring and staying attentive in automaticity suggests that comfort does not imply a ‘lack of vigilance’ or a ‘relaxed state.’ Rather, comfort without vigilance is akin to automaticity without attention, and might be considered the management equivalent of premature diagnostic closure (Croskerry 2003).
Theory-based cues that influence feelings of comfort with uncertainty
Theory-based cues are those that come from the deliberate application of metacognitive beliefs (Koriat 1997). If, for example, clinicians feel comfortable acting in a state of uncertainty because they “have seen it all before,” or encourage a trainee to carry forward because “there is nothing you can get into here that I cannot get you out of,” they are expressing a view that their accrued experience will enable them to derive an appropriate solution. Studies of experts in other fields suggest that they draw from accrued experiences to quickly surmise a situation (Chase and Simon 1973) and then attempt to make reasonable predictions for how a situation is likely to evolve (de Bruin et al. 2017; Ericsson et al. 2000; Ilgen and Brydges 2017; Koriat 1997). These predictions then contribute to experts feeling comfortable that they can manage whatever arises in a given situation. In short, the theory-based cue for ‘comfort’ is a belief that one has sufficient accrued experience with all of the reasonably probable scenarios, and the ability to control the situation in ways that will avoid instances where evolving situational needs will likely outstrip the resources available.
Clinicians engage in these forms of forward planning in moments of uncertainty by considering a range of management plans and potential outcomes that might result (Moulton et al. 2010c). In contrast to decision-making analyses, where ‘getting the diagnosis right’ is tantamount to high performance (Friedman et al. 2005), forward planning in moments of uncertainty arising from an ill-defined problem instead employs knowledge from accrued experiences with similar problems to predict various potential events that are sufficiently probable. The ability to anticipate, which tends to arise with expertise (Ericsson et al. 2000), allows one to preemptively put resources such as technology or personnel in place (Novick et al. 2015). These resources minimize the risk of reasonably probable events that would lead to situations that exceed a clinician’s abilities given their particular treatment context (LeBlanc et al. 2015; Zilbert et al. 2015a, b). Putting these resources in place, therefore, allows clinicians to move forward with comfort. Discomfort occurs, in contrast, when clinicians can imagine likely scenarios that they perceive to be outside of their knowledge or skills, or if the anticipated problems outstrip the available resources (LeBlanc et al. 2015). This sentiment may ultimately prompt clinicians to consider whether they ask for help (Jin et al. 2012; Novick et al. 2015), look for ways to further disambiguate a problem (Eva and Regehr 2007), or triage the problem to colleagues with different skillsets or resources (Zilbert et al. 2015b).
Social complexities around ‘comfort with uncertainty’
While we have prioritized consideration of cognitive factors that are likely to influence skillful practitioners’ feelings of ‘comfort with uncertainty,’ it is likely that social and social-emotional cues will also play a role. Local and discipline-specific cultures around risk tolerance, reactions to adverse events, and vulnerability to peers are all likely to impact clinicians’ comfort with managing problems independently (Jin et al. 2012; Kennedy et al. 2009b; Luu et al. 2012; Novick et al. 2015), particularly when considering how patients or colleagues retrospectively judge each other’s actions or inactions (Leung et al. 2012; Novick et al. 2015). Similarly, the design of the health system in which one works will determine the external resources that clinicians have available—such as when backup from another clinician is easily accessible (Williams et al. 2007) or when tests are more readily available (Plebani 1999)—as well as the external pressures they are managing (Cristancho et al. 2013b).These social-cultural influences on ‘comfort’ warrant attention in future work; however, the focus of this paper is on the cognitive aspects of this phenomenon, so we will leave it to others to elaborate these aspects of ‘comfort.’
Discussion
This review has explored the premise that ‘comfort with uncertainty’ can be deconstructed in ways that provide new insights into how clinicians navigate the interconnected complexities of diagnosis and management in practice. Exploring how comfort is established and used within this framework illustrates the iterative and cyclical nature of clinical reasoning in complex settings (Cristancho et al. 2016) whereby comfort enables action and the ease with which one is able to act provides comfort. When working within settings where patients’ problems are ill-defined or incompletely conceptualized (i.e., where the cause of the problem is uncertain), clinicians harness action-oriented categorizations of problems and “pragmatic empiricism” (Atkinson 1984, p. 954) to get started with their management approaches, then couple these approaches with ongoing forward planning and intensive monitoring to clarify and re-conceptualize the situation at hand. Becoming comfortable in maintaining uncertainty in these settings is important because uncertainty serves as a catalyst for ongoing skepticism about working hypotheses, thereby setting an expectation that these tentative hypotheses will be continually revised. Remaining uncertain additionally triggers clinicians to put resources in place to minimize risk around problems that remain sufficiently possible.
Implications for educators
How might this model of ‘comfort with uncertainty’ inform how educators support the development of clinical reasoning in trainees? We offer three preliminary educational implications that follow from this exploration of ‘comfort with uncertainty.’ First, to exist in this conceptual space of ‘informed speculation’ clinicians must adopt a deliberatively iterative and flexible construction of how patients’ problems are defined, approached, and managed. To get students into a mindset where ‘comfort with uncertainty’ is possible thus requires educators to first disabuse their trainees of the notion that clinical knowledge exists in a binary format of ‘knowing’ and ‘not knowing’ (Ilgen et al. 2016). We believe that widely-used formulations for teaching clinical reasoning that are centered around diagnosis may contribute to learners’ challenges (Bordage and Lemieux 1991; Bowen 2006). These models implicitly suggest that ‘not knowing’ precludes taking action, while ‘knowing’ provides license for unwavering certitude when moving forward. Shifting our instructional models towards an emphasis on ‘comfort with uncertainty’ would instead teach students that skillful clinicians use problem-definition and problem-solving in parallel (Cristancho et al. 2017), treating possible diagnoses as merely provisional conceptual frameworks that facilitate action, and using responses to these actions as a means to further clarify their understanding of their patients’ problems.
Second, we believe our treatment of the terms ‘comfort’ and ‘discomfort’ can help trainees better identify the limits of what is safe to do (Kennedy et al. 2009a, b; Novick et al. 2015; Stewart 2008), and better understand that safety will be facilitated by forward planning and monitoring. Educators can reinforce forward planning skills by prompting trainees to preemptively consider the resources they may need if any number of anticipated high-risk events were to take place (e.g. “what will we do if X happens?”; Moulton et al. 2010a). Further, consistent with Koriat’s work (Koriat 1997; Koriat et al. 2005), educators can encourage trainees to monitor for cues that might signal that they are ‘on track’ or that they are veering into dangerous territory where conditions are beyond their abilities to control or manage (Moulton et al. 2010b).
Lastly, we would encourage clinical preceptors to reflect upon the underpinnings of their own ‘comfort’ in uncertain situations. As Koriat argues, cues such as ‘comfort’ are enabled by the rich accrual of experiences and beliefs about how these experiences prepare clinicians to take action (Koriat 1997; Koriat et al. 2005). So, just because this impulse is triggered in a preceptor does not mean that a trainee should feel the same way. Trainees’ abilities to imagine the multitude of possible downstream scenarios are limited given their lack of prior exposure to similar problems (thus restricting forward planning) and novices’ lack of automaticity and limited attentional reserves are likely to impair their abilities to self-monitor (Moulton et al. 2010b). Taken together, it is not at all surprising that supervisors frequently feel ‘out of sync’ with their trainees (Moulton et al. 2010a) as learners’ ‘discomfort with uncertainty’—manifested as behaviors such as hesitation (Ott et al. 2018)—is a developmentally appropriate response for their stage of training. Educational programs that encourage students to generically ‘tolerate’ uncertainty (Cooke et al. 2017) deemphasize the importance of self-monitoring, encourage a lack of vigilance, or prompt trainees to fall back into models where diagnostic certainty is necessary for action (Ilgen et al. 2016). These pitfalls risk premature closure around problems that are still ill-defined and risk over-testing in ways that are not patient-centered. Instead, we would encourage supervisors to use these ‘out of sync’ instances as critical opportunities for learning. Working within a framework of ‘comfort with uncertainty’ allows supervisors and trainees to instead speculate together about the possible downstream events that pose risk to their patients (thereby enriching skills in forward planning), while concurrently considering the specific actions that allow them to move forward safely while continually monitoring their progress in these settings.
Implications for research
Further development of this framework and the proposed educational innovations requires a more robust understanding of how skillful clinicians recognize the boundaries between comfort and discomfort in moments of uncertainty. Doing so would help to better define instances where problems can be managed within the confines of clinicians’ existing cognitive, emotional, and environmental resources, and when help is needed. Existing research examines how established clinicians preemptively steer clear of problems that are likely to misalign with their skillset (Zilbert et al. 2015a, b), but there has been less work directed toward understanding how clinicians’ moment-to-moment appraisals of comfort are both enacted and acted upon, as well as when they reach the limits of their comfort. Koriat’s dual-basis view of metacognitive judgments may provide helpful scaffolding to categorize the types of cues that clinicians use in the moment (Koriat 1997; Koriat et al. 2005), and these can ultimately be linked to downstream events as a means to illustrate whether or not these cues are predictive for desired outcomes (de Bruin et al. 2017).
Further, as a supplement to research exploring how clinicians manage uncertainty effectively, there is need for an exploration of how this framework is conceptualized by novices, and how it aligns with their lived experiences. How do learners define the edges of their zones of practice while still learning the practice itself? How are the edges of a novice’s comfort zone experienced in the context of working with different supervisors and in different settings? Are lived experiences of discomfort viewed as limitations of practice or opportunities for learning? Are such perceptions derived from the implicit messages they receive from their training programs and clinical preceptors? How novices respond in moments of uncertainty or moments of discomfort will determine the extent to which they engage in entrustable practice and learning (Ten Cate et al. 2016) or hide their feelings in a manner that could compromise patient safety (Moulton et al. 2010a). Research in this respect could thus probe learners to determine how they manage problems in the context of ongoing uncertainty while simultaneously navigating the tensions between learning, risk, and emerging independence.
Finally, if comfort and discomfort reflect holistic cognitive frameworks that guide the management of uncertainty, what does it mean for learners to be ‘overconfident,’ and how do supervisors identify these attributes in trainees? In past work, definitions of over- and under-confidence were based upon retrospective alignment or misalignment with measures of diagnostic accuracy as determined by expert consensus (Friedman et al. 2005; Potchen 2006), pathology results (Dreiseitl and Binder 2005), or autopsy findings (Landefeld et al. 1988). Our definition of confidence is likely to change if we move away from a goal of ‘getting a diagnosis right’ towards ‘taking a reasonable next step while attending to and anticipating varied responses to management plans.’ Thus, unearthing the roots of trainees’ ‘comfort’ might help to further elaborate what faculty members mean when they say trainees are ‘over-confident’ in uncertain settings. This will help us understand the behaviors that give supervisors the perception that trainees are acting as “cowboys” (taking undue risk) or being overly “timid” (risk-intolerant) in settings of uncertainty (Cassell 1991; Zilbert et al. 2015b).
Conclusion
‘Comfort with uncertainty’ describes instances where clinicians have the confidence to act on a problem (or wait and observe) while lacking full confidence in their understanding of the underlying cause of the issue. This framework provides a new model for exploring and conceptualizing the critical cognitive and environmental cues that impact moment-to-moment decision-making. By focusing on the influences that shape individuals’ comfort, the management of uncertainty can focus on planning and enacting defensible clinical actions even when downstream outcomes remain unknown.
Notes
The word “experience” is used in the English language to represent the process of personally observing, encountering, or undergoing something as well as the knowledge or practical wisdom gained from what one has observed, encountered, or undergone. For the purposes of clarifying these two meanings, we will use ‘lived experience’ to describe experiences in the moment, and ‘accrued experience’ to represent the historical accumulation of such moments.
For Koriat, the term “experience-based cue” describes what we have been labeling as ‘lived experiences’ in the moment.
References
Atkinson, P. (1984). Training for certainty. Social Science and Medicine, 19, 949–956.
Babrow, A. S., Kasch, C. R., & Ford, L. A. (1998). The many meanings of uncertainty in illness: Toward a systematic accounting. Health Communcation, 10, 1–23.
Barbalet, J. M. (1993). Confidence: time and emotion in the sociology of action. Journal for the Theory of Social Behaviour, 23, 229–246.
Begg, I., Duft, S., Lalonde, P., Melnick, R., & Sanvito, J. (1989). Memory predictions are based on ease of processing. Journal of Memory and Language, 28, 610–632.
Bordage, G., & Lemieux, M. (1991). Semantic structures and diagnostic thinking of experts and novices. Academic Medicine, 66, S70–S72.
Bowen, J. L. (2006). Educational strategies to promote clinical diagnostic reasoning. New England Journal of Medicine, 355, 2217–2225.
Cassell, J. (1991). Expected miracles: Surgeons at work. Philadelphia: Temple University Press.
Chase, W. G., & Simon, H. A. (1973). The mind’s eye in chess. In W. G. Chase (Ed.), Visual information processing (pp. 215–281). New York: Academic Press.
Cooke, G., Tapley, A., Holliday, E., Morgan, S., Henderson, K., Ball, J., et al. (2017). Responses to clinical uncertainty in Australian general practice trainees: a cross-sectional analysis. Medical Education, 51, 1277–1288.
Cristancho, S. M., Apramian, T., Vanstone, M., Lingard, L., Ott, M., Forbes, T., et al. (2016). Thinking like an expert: surgical decision making as a cyclical process of being aware. American Journal of Surgery, 211, 64–69.
Cristancho, S. M., Apramian, T., Vanstone, M., Lingard, L., Ott, M., & Novick, R. J. (2013a). Understanding clinical uncertainty: What is going on when experienced surgeons are not sure what to do? Academic Medicine, 88, 1516–1521.
Cristancho, S. M., Vanstone, M., Lingard, L., LeBel, M. E., & Ott, M. (2013b). When surgeons face intraoperative challenges: A naturalistic model of surgical decision making. American Journal of Surgery, 205, 156–162.
Cristancho, S., Lingard, L., Forbes, T., Ott, M., & Novick, R. (2017). Putting the puzzle together: The role of ‘problem definition’ in complex clinical judgement. Medical Education, 51, 207–214.
Croskerry, P. (2003). The importance of cognitive errors in diagnosis and strategies to minimize them. Academic Medicine, 78, 775–780.
de Bruin, A., Dunlosky, J., & Cavalcanti, R. (2017). Monitoring and regulation of learning in medical education: The need for predictive cues. Medical Education, 51, 575–584.
Djulbegovic, B., Hozo, I., & Greenland, S. (2011). Uncertainty in clinical medicine. In F. Gifford (Ed.), Philosophy of medicine (pp. 299–356). Amsterdam: North Holland.
Dogra, N., Giordano, J., & France, N. (2007). Cultural diversity teaching and issues of uncertainty: the findings of a qualitative study. BMC Medical Education, 7, 1–13.
Dreiseitl, S., & Binder, M. (2005). Do physicians value decision support? A look at the effect of decision support systems on physician opinion. Artificial Intelligence in Medicine, 33, 25–30.
Dunphy, B. C., & Williamson, S. L. (2004). In pursuit of expertise. Toward an educational model for expertise development. Advances in Health Sciences Education, 9, 107–127.
Ericsson, K. A., Patel, V., & Kintsch, W. (2000). How experts’ adaptations to representative task demands account for the expertise effect in memory recall: Comment on Vicente and Wang (1998). Psychological Review, 107, 578–592.
Eva, K. W., & Regehr, G. (2005). Self-assessment in the health professions: A reformulation and research agenda. Academic Medicine, 80, S46–S54.
Eva, K. W., & Regehr, G. (2007). Knowing when to look it up: A new conception of self-assessment ability. Academic Medicine, 82, S81–84.
Fargason, C. A. J., Evans, H. H., Ashworth, C. S., & Capper, S. A. (1997). The importance of preparing medical students to manage different types of uncertainty. Academic Medicine, 72, 688–692.
Fox, R. (1957). Training for certainty. In R. K. Merton, G. Reader, & P. L. Kendall (Eds.), The student physician. Cambridge: Harvard University Press.
Friedman, C. P., Gatti, G. G., Franz, T. M., Murphy, G. C., Wolf, F. M., Heckerling, P. S., et al. (2005). Do physicians know when their diagnoses are correct? Implications for decision support and error reduction. Journal of General Internal Medicine, 20, 334–339.
Geller, G. (2013). Tolerance for ambiguity: An ethics-based criterion for medical student selection. Academic Medicine, 88, 581–584.
Grant, M. J., & Booth, A. (2009). A typology of reviews: an analysis of 14 review types and associated methodologies. Health Information and Libraries Journal, 26, 91–108.
Hartmann, W. H. (1998). Preparing medical students to “Manage Uncertainty”. Academic Medicine, 73, 116–117.
Ilgen, J. S., & Brydges, R. (2017). Cues for self-regulation: it’s difficult to make predictions, especially about the future. Medical Education, 51, 566–568.
Ilgen, J. S., Eva, K. W., & Regehr, G. (2016). What’s in a label? Is diagnosis the start or the end of clinical reasoning? Journal of General Internal Medicine, 31, 435–437.
Jha, S. (2014). Stop hunting for zebras in Texas: End the diagnostic culture of “Rule-Out”. BMJ: British Medical Journal, 348, g2625.
Jin, C. J., Martimianakis, M. A., Kitto, S., & Moulton, C. A. (2012). Pressures to “measure up” in surgery: Managing your image and managing your patient. Annals of Surgery, 256, 989–993.
Kennedy, T. J., Regehr, G., Baker, G. R., & Lingard, L. (2009a). Preserving professional credibility: Grounded theory study of medical trainees’ requests for clinical support. BMJ: British Medical Journal, 338, b128.
Kennedy, T. J., Regehr, G., Baker, G. R., & Lingard, L. A. (2009b). ‘It’s a cultural expectation…’ The pressure on medical trainees to work independently in clinical practice. Medical Education, 43, 645–653.
Kitchener, K. S. (1983). Cognition, metacognition, and epistemic cognition: a three-level model of cognitive processing. Human Development, 4, 222–232.
Koriat, A. (1997). Monitoring one’s own knowledge during study: A cue-utilization approach to judgments of learning. Journal of Experimental Psychology: General, 126, 349–370.
Koriat, A., Bjork, R. A., Sheffer, L., & Bar, S. K. (2005). Predicting one’s own forgetting: the role of experience-based and theory-based processes. Journal of Experimental Psychology: General, 133, 643–656.
Landefeld, C. S., Chren, M. M., Myers, A., Geller, R., Robbins, S., & Goldman, L. (1988). Diagnostic yield of the autopsy in a University hospital and a community hospital. New England Journal of Medicine, 318, 1249–1254.
Lazarus, R. S. (1991). Emotion and adaptation. New York: Oxford University Press.
Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal, and coping. New York: Springer.
LeBlanc, V. R. (2009). The effects of acute stress on performance: implications for health professions education. Academic Medicine, 84, S25–33.
LeBlanc, V. R., McConnell, M. M., & Monteiro, S. D. (2015). Predictable chaos: a review of the effects of emotions on attention, memory and decision making. Advances in Health Sciences Education, 20, 265–282.
Leung, A., Luu, S., Regehr, G., Murnaghan, M. L., Gallinger, S., & Moulton, C. A. (2012). “First, do no Harm”: Balancing competing priorities in surgical practice. Academic Medicine, 87, 1368–1374.
Levine, D. N. (1985). The flight from ambiguity: Essays in social and cultural theory. Chicago: University of Chicago Press.
Light, D. (1979). Uncertainty and control in professional training. Journal of Health and Social Behavior, 20, 310–322.
Lingard, L., Garwood, K., Schryer, C. F., & Spafford, M. M. (2003). A certain art of uncertainty: case presentation and the development of professional identity. Social Science and Medicine, 56, 603–616.
Lipshitz, R., & Strauss, O. (1997). Coping with uncertainty: A naturalistic decision-making analysis. Organizational Behavior and Human Decision Processes, 69, 149–163.
Luther, V. P., & Crandall, S. J. (2011). Commentary: Ambiguity and uncertainty: Neglected elements of medical education Curricula? Academic Medicine, 86, 799–800.
Luu, S., Patel, P., St-Martin, L., Leung, A. S., Regehr, G., Murnaghan, M. L., et al. (2012). Waking up the next morning: surgeons’ emotional reactions to adverse events. Medical Education, 46, 1179–1188.
Mishel, M. H. (1988). Uncertainty in Illness. Image: The Journal of Nursing Scholarship, 20, 225–232.
Mishel, M. H. (1990). Reconceptualization of the uncertainty in illness theory. Image: The Journal of Nursing Scholarship, 22, 256–262.
Moulton, C. A., Regehr, G., Lingard, L., Merritt, C., & Macrae, H. (2010a). Operating from the other side of the table: control dynamics and the surgeon educator. Journal of the American College of Surgeons, 210, 79–86.
Moulton, C. A., Regehr, G., Lingard, L., Merritt, C., & MacRae, H. (2010b). Slowing down to stay out of trouble in the operating room: remaining attentive in automaticity. Academic Medicine, 85, 1571–1577.
Moulton, C. A., Regehr, G., Lingard, L., Merritt, C., & Macrae, H. (2010c). ‘Slowing down when you should’: Initiators and influences of the transition from the routine to the effortful. Journal of Gastrointestinal Surgery, 14, 1019–1026.
Novick, R. J., Lingard, L., & Cristancho, S. M. (2015). The call, the save, and the threat: Understanding expert help-seeking behavior during nonroutine operative scenarios. Journal of Surgical Education, 72, 302–309.
Ott, M., Schwartz, A., Goldszmidt, M., Bordage, G., & Lingard, L. (2018). Resident hesitation in the operating room: Does uncertainty equal incompetence? Medical Education, 52, 851–860.
Plebani, M. (1999). The clinical importance of laboratory reasoning. Clinica Chimica Acta, 280, 35–45.
Potchen, E. J. (2006). Measuring observer performance in chest radiology: some experiences. Journal of the American College of Radiology, 3, 423–432.
Rawson, K. A., & Dunlosky, J. (2002). Are performance predictions for text based on ease of processing? Journal of Experimental Psychology. Learning, Memory, and Cognition, 28, 69–80.
Reber, R., & Greifeneder, R. (2017). Processing fluency in education: How metacognitive feelings shape learning, belief formation, and affect. Educational Psychologist, 52, 84–103.
Rensink, R. A., O’Regan, J. K., & Clark, J. J. (1997). To see or not to see: The need for attention to perceive changes in sciences. Psychological Science, 8, 368–373.
Schön, D. A. (1983). The reflective practitioner: How professionals think in action. New York: Basic Books.
Schraw, G., Dunkle, M. E., & Bendixen, L. D. (1995). Cognitive processes in well-defined and ill-defined problem solving. Applied Cognitive Psychology, 9, 523–538.
Schwartz, S., & Griffin, T. (1986). Medical thinking: The psychology of medical judgment and decision making. New York: Springer.
Simons, D. J., & Chabris, C. F. (1999). Gorillas in our midst: sustained in attentional blindness for dynamic events. Perception, 28, 1059–1074.
Simpkin, A. L., & Schwartzstein, R. M. (2016). Tolerating uncertainty: The next medical revolution? New England Journal of Medicine, 375, 1713–1715.
Simpson, D. E., Dalgaard, K. A., & O’Brien, D. K. (1986). Student and faculty assumptions about the nature of uncertainty in medicine. Journal of Family Practice, 23, 468–472.
Smith, C. S., & Paauw, D. S. (2000). When you hear hoof beats: four principles for separating zebras from horses. Journal of the American Board of Family Practice, 13, 424–429.
Stewart, J. (2008). To call or not to call: A judgement of risk by pre-registration house officers. Medical Education, 42, 938–944.
Ten Cate, O., Hart, D., Ankel, F., Busari, J., Englander, R., Glasgow, N., et al. (2016). Entrustment decision making in clinical training. Academic Medicine, 91, 191–198.
White, G., & Williams, S. (2017). The certainty of uncertainty: Can we teach a constructive response? Medical Education, 51, 1200–1202.
Williams, R. G., Silverman, R., Schwind, C., Fortune, J. B., Sutyak, J., Horvath, K. D., et al. (2007). Surgeon information transfer and communication: Factors affecting quality and efficiency of inpatient care. Annals of Surgery, 245, 159–169.
Zilbert, N. R., Murnaghan, M. L., Gallinger, S., Regehr, G., & Moulton, C. A. (2015a). Taking a chance or playing it safe: Reframing risk assessment within the surgeon’s comfort zone. Annals of Surgery, 262, 253–259.
Zilbert, N. R., St-Martin, L., Regehr, G., Gallinger, S., & Moulton, C. A. (2015b). Planning to avoid trouble in the operating room: Experts’ formulation of the preoperative plan. Journal of Surgical Education, 72, 271–277.
Acknowledgements
The authors wish to thank Alisha Brown, MD, Joshua Jauregui, MD, Laura Welsh, MD, and Bjorn Watsjold, MD for their constructive critiques.
Funding
This review was supported by an award from the Society of Directors of Research in Medical Education (SDRME).
Author information
Authors and Affiliations
Corresponding author
Additional information
These findings were reported at the 2018 Annual Meeting of the Society of Directors of Research in Medical Education (SDRME) in Louisville, KY.
Rights and permissions
About this article
Cite this article
Ilgen, J.S., Eva, K.W., de Bruin, A. et al. Comfort with uncertainty: reframing our conceptions of how clinicians navigate complex clinical situations. Adv in Health Sci Educ 24, 797–809 (2019). https://doi.org/10.1007/s10459-018-9859-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10459-018-9859-5