Abstract
Background
Coronary collateral vessel development (CVD), i.e., arteriogenesis, is regarded as one of the most important mechanisms—along with angiogenesis—to result in protection of the myocardium. Coronary CVD is associated with a reduction in infarct size, future cardiovascular events and improved survival in patients with occlusive coronary artery disease by enhancing regional perfusion in the chronically ischemic myocardium. In the present study, we aimed to investigate the relation of cardiovascular risk factors and hematological parameters with collateral development in patients with severely stenotic (≥95 %) and totally occluded coronary artery disease including at least one major coronary artery.
Materials and methods
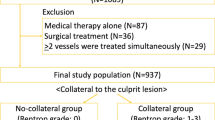
The study population was selected from the patients who underwent coronary angiography between January 2008 and March 2009. Five hundred and two patients who had at least one coronary artery stenosis ≥95 % (368 men; mean age 59 ± 10 years) comprised the study population. Of the 502 patients, 228 had total occlusion in at least one major epicardial coronary artery. Collateral artery grading was performed by using Cohen–Rentrop method to the vessel with coronary artery stenosis of ≥95 % and patients with chronic total occlusions (CTO). Patients with grade 0–1 collateral development were regarded as the poor collateral group, and patients with grade 2–3 collateral development were regarded as the good collateral group.
Results
Two hundred and fifty-eight (51 %) of 502 patients had poor collateral development, and 244 (49 %) had good collateral development. Logistic regression analysis revealed that DM was independently associated with poor CVD in patients with ≥95 % stenosis (p < 0.001). Additionally, female gender and DM were found to be independently associated with poor CVD in patients with CTO (p = 0.005 and p < 0.001, respectively). Monocyte count was found to be independent of CVD neither in patients with ≥95 % stenosis nor in patients with CTO.
Conclusion
Our data show that DM is an independent factor for poor coronary CVD both in patients with severe coronary artery stenosis and in patients with CTO. Female gender or being in post-menopausal period is another negative risk factor for poor CVD in addition to DM in patients with CTO.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arteriogenesis, i.e., the growth of collateral arteries, is regarded as one of the most important mechanisms along with angiogenesis to enhance regional perfusion in the chronically ischemic myocardium [1, 2]. Coronary collateral vessel development (CVD) has been shown to be potentially protective with regard to infarct size, ventricular aneurysm formation, ventricular function, future cardiovascular events and survival in patients with occlusive coronary lesions due to atherosclerosis [3–5]. Cardiovascular risk factors affecting CVD have been evaluated in several clinical studies [6–8]. Diabetes mellitus (DM) has been found to be a negative predictor for the development of functional collateral arteries in patients with coronary artery stenosis >75 % [6].
Monocytes play a pivotal role in arteriogenesis at the cellular level by releasing growth factors, proteases and chemokines, hence mediating cell proliferation and migration as well as structural remodelling of the extracellular compartment [9]. Recently, it has been documented that monocyte number is an independent factor for the development of good collateral arteries in patients with severe coronary artery stenosis ≥95 % in a study with patients without DM [10]. In the present study, we investigated the relation of cardiovascular risk factors and hematological variables—mainly focusing on blood monocyte count—with collateral development in coronary artery disease (CAD) patients with (at least one) severely stenotic (≥95 %) or totally occluded coronary artery (CTO).
Materials and methods
The study population was selected from the patients who underwent coronary angiography bet at the University hospital in Bolu and IMC Hospital in Mersin, Turkey. All patients with at least one major coronary artery stenosis of ≥95 % or with a CTO were consecutively included in the study. Their coronary angiograms were examined for CVD by two experienced interventional cardiologists.
Five hundred and two selected patients who had at least one coronary artery stenosis ≥95 % (368 men; mean age 59 ± 10 years) comprised the study population. Of the 502 patients, 228 had a CTO in at least one major epicardial coronary artery. Total and differential leukocyte counts and biochemical markers obtained at most 2 days before or on the day of coronary angiography were used for analysis. Patients with previous revascularization history of either surgical bypass or percutaneous intervention, evidence of ongoing infection or inflammation, recent acute coronary syndrome either with or without ST-segment elevation (3 months before enrollment), hematological disease or known malignancy were excluded from the study. Biochemical assessments were performed using standard methods. Total and differential leukocyte counts were measured by an automated hematology analyzer (Coulter Gen-S, COULTER Corp, Miami, USA).
Standard selective coronary angiography with at least four views of the left coronary system and two views of the right coronary artery was performed using the Judkins technique. For the analysis of the effect of multivessel disease on coronary CVD, the number of the diseased vessels was identified according to the number of the major coronary arteries having ≥70 % stenosis by eyeballing.
The following clinical and demographical parameters were recorded: age, sex, hypertension (known hypertension treated with antihypertensive drugs, two or more blood pressure recordings greater than 140/90 mm Hg), diabetes mellitus (known diabetes treated with diet or drugs or both; or either a fasting serum glucose of more than 126 mg/dl or random plasma glucose >200 mg/dl in persons with symptoms of hyperglycemia) and hypercholesterolemia (known treated hypercholesterolemia or serum total cholesterol concentrations higher than 200 mg/dl). All the diabetic patients had been receiving oral anti-diabetic drugs and/or insulin for at least 6 months. Current cigarette smoking was defined as active smoking of at least five cigarettes per day within the past 12 months.
Collateral vessel development grading
Collateral artery grading was performed by using Cohen–Rentrop method [11] to the vessel with coronary artery stenosis of ≥95 %. Collateral grades according to Cohen–Rentrop method were defined as: grade 0, no filling of any collateral vessels; grade 1, filling of side branches of the artery to be perfused by collateral vessels without visualization of epicardial segment; grade 2, partial filling of the epicardial artery by collateral vessels; and grade 3, as complete filling of epicardial artery by collateral vessel. If the patient had more than one vessel with severe stenosis ≥95 %, the highest CVD score was recorded for statistical analysis. Patients with grade 0–1 collateral development were regarded as poor collateral group, and patients with grade 2–3 collateral development were regarded as good collateral group. Of the 122 female patients, 111 (91 %) were in post-menopausal period and 45 (90 %) out of 50 (90 %) female patients in the CTO group were in menopause. Since most of the female patients were in post-menopausal period, all female patients were included in the regression analysis.
Statistical analysis
Continuous variables were given as mean ± SD; categorical variables were defined as percentage. Continuous variables and categorical variables were compared by using unpaired t test and Chi-square test, respectively. Distribution of continuous variables was tested by Kolmogorov–Smirnov test. All continuous variables were shown to be normally distributed. Logistic regression was used to analyze the possible association of cardiovascular risk factors and hematological variables with CVD both in patients with coronary stenosis ≥95 % and in subgroup of patients with chronic total occlusion. Age, gender, DM, hypertension, hyperlipidemia, smoking, whole blood neutrophil, lymphocyte, monocyte, platelet count, mean platelet volume and hemoglobin were included in regression analysis. All tests of significance were two-tailed. Statistical significance was defined as p < 0.05. The SPSS statistical software (SPSS for windows 15, Inc., Chicago, IL, USA) was used for all statistical calculations.
Results
Two hundred and fifty-eight (51 %) of 502 patients had poor CVD, and 244 (49 %) had good CVD (Figs. 1, 2). The clinical, hematological and biochemical characteristics of the patients are shown in Table 1. There were no statistically significant differences in terms of cardiovascular risk factors, biochemical and hematological parameters except DM, which was significantly higher in patients with poor CVD (43 %) than in good CVD (23 %; p < 0.001; Table 1). Logistic regression analysis revealed that DM was the only variable independently associated with poor CVD (Table 2).
The same analysis was carried out for patients with CTO in at least one epicardial coronary artery. Two hundred and twenty-eight had CTO (mean age 59 ± 12 years, Table 3). Of whom, 61 patients had poor CVD and 167 patients had good CVD. Comparison of baseline characteristics and laboratory parameters between two groups (poor and good CVD) showed that presence of diabetes mellitus (p < 0.001) and female gender (p = 0.002) were significantly higher in patients with poor CVD than in patients with CTO (Table 3). These parameters were also found to be independently associated with poor CVD in patients with CTO (Table 4). The number of single-vessel, two-vessel and three-vessel disease was comparable between patients with good and poor CVD (Table 5). The overall severity of the each coronary artery stenosis was comparable between male and female patients (Left anterior descending % stenosis: 73 ± 33 vs. 76 ± 30; p = 0.38, left circumflex % stenosis: 59 ± 40 vs. 52 ± 42; p = 0.10, right coronary artery % stenosis: 66 ± 340 vs. 60 ± 41; p = 0.19, respectively).
As monocytes have been demonstrated to play a role in collateral formation, we have investigated the monocyte count of our patients with high-grade coronary artery stenosis. The monocyte count was found to be independent of CVD both in patients with ≥95 % stenosis and in patients with CTO (Tables 2, 4, respectively).
Discussion
There are several main findings of our study: (1) There is an independent association between the presence of DM and poor collateral arteries in both patients with ≥95 % stenosis and patients with CTOs, (2) female gender and history of MI are the other independent associates of poor collateral vessel development in patients with CTO along with DM, and (3) monocyte count is independent of the presence of coronary collateral arteries in both patients with ≥95 % stenosis and in patients with CTO.
DM is one of the best documented negative risk factors for the development of collateral arteries. Poor coronary collateral development has been documented in DM by Abaci et al. [6] in patients with more than 75 % stenosis. Moreover, metabolic syndrome was found to be associated with poor CVD [7]. In our study, we have shown that in patients with severe coronary stenosis (≥95 %) and in patients with CTO, DM is a major predictor for poor coronary CVD. On the contrary, Zbinden et al. [8] have reported that the coronary collateral flow index does not differ between diabetic and non-diabetic patients. However, it cannot be excluded that the patient groups differed with regard to the severity of coronary stenosis, although the average stenosis grade was the same in both the diabetic and the non-diabetic cohort, namely 68 %. Therefore, when compared with our novel data presented in this paper, it appears that differences in collateralization between diabetic and non-diabetic patients can only be revealed, if patients with high-grade stenosis (95–100 %) are being compared. Additionally, the method of CVD assessment is another issue to be considered, while comparing the results of Zbinden et al, in which coronary collateral flow index has been used instead of the Cohen–Rentrop [11] coronary angiographic classification method.
Likewise, more controversial reports have been published in literature with different methodology assessing CVD. Werner et al. [12] have assessed the collateral function of CTO by intracoronary Doppler and pressure sensors before and after a balloon angioplasty and have reported no differences in parameters of collateral function between diabetic and non-diabetic patients indicating a similar development of collaterals in CTO. However, the acute recruitment of collateral function after recanalization as assessed during a balloon reocclusion was impaired in diabetic patients with an occlusion of <3 months duration. De Vries et al. [13] evaluated patients with stable CAD scheduled for elective PCI, found that 45 % have functional collaterals assessed by pressure monitoring guide-wire and reported no differences between patients with and without DM. History of angina pectoris and duration and severity of atherosclerotic burden rather than the presence of DM have been reported to be predictor of CVD [14, 15]. Moreover, Kyriakides et al. [16] have reported that type II diabetes does not prevent the recruitment of collateral vessels or the normal reduction in myocardial ischemia on repeated balloon inflations during coronary angioplasty. However, recruitment of collateral vessels during balloon inflation which is an acute situation mainly depends on the preexisted collateral vessels and is driven by shear stress. The most important trigger of arterial remodelling in native as well as collateral vessels is increased tangential fluid shear stress at the endothelial surface. Fluid shear stress is the product of spatial velocity changes between different fluid layers or the fluid and the endothelium and blood viscosity increased adherence of monocytes, which transform into macrophages [17]. Werner et al. [18] have also detected that release of MCP-1 into the collateral circulation appears to be related to increased shear stress but release of bFGF into the collateral circulation is related to the duration of the occlusion and the quality of collateral function. However, release of bFGF is down-regulated in diabetic patients [18].
In the last decade, studies evaluating the effects of DM on development of CVD vessels have focused on monocyte-mediated mechanisms as monocytes are key players in arteriogenesis [19]. It is important to note that the function of monocytes appears to be critical. Monocyte dysfunction has been clearly demonstrated in patients with DM [20, 21]. As recently demonstrated, the cellular response of monocytes to VEGF-A is attenuated in diabetic patients secondary to a downstream signal transduction defect [21]. These data suggest that monocytes are important in arteriogenesis. The process of arteriogenesis seems to be critically dependent on monocytes and on proper monocyte function [1, 22, 23] as their ability to migrate might be critical for the arteriogenic response. Previous studies have shown that monocytes/macrophages in particular accumulate in the surrounding tissue of collateral vessels after arterial occlusion due to ICAM-1/Mac-1-dependent mechanisms [24, 25]. These macrophages are potent sources of cytokines and growth factors such as TNF-α, VEGF and FGF-2 [1, 26] that are required for natural adaptive arteriogenesis. Moreover, increased chemoattraction of monocytes/macrophages (e.g., by exogenously applied MCP-1) leads to an accelerated arteriogenic response, whereas lack of circulating monocytes reduces collateral artery growth [1, 27]. Recent experimental studies suggest a direct, functional correlation between collateral artery growth after occlusion of a main artery and the concentration of circulating monocytes [27, 28]. Moreover, Heil et al. [27] have reported that arteriogenesis is stimulated by increasing the number of circulating monocytes. However, almost all the studies documenting a direct correlation between monocyte number and arteriogenesis have evaluated this relation shortly after an acute occlusion of the infarct-related artery. Therefore, one interpretation could be that arteriogenesis might correlate with the number of monocytes recruited from the circulation. We have tested this hypothesis in the current study. We have to reject this hypothesis, as there was no correlation between monocyte number and coronary CVD.
On the other hand, the functional status of monocytes during the acute phase of arteriogenesis immediately following the acute occlusion of the artery might be different from the chronic phase of occlusion. Since none of the patients had MI <3 months, our study population represents an established steady-state phase of arteriogenesis in which monocytes might be functionally more silent compared with acute occlusion phase of arteriogenesis. In essence, the arteriogenesis process has finished in our patients as the typical stimuli of arteriogenesis are absent under these conditions.
Another important finding of our study is that female gender is an independent factor for poor CVD in patients with CTO. In line with this observation, women are known to have a higher in-hospital mortality after MI and percutaneous coronary interventions than men [29, 30]. The differences in clinical course of women and men are not in the scope of our study. Meanwhile, it is important to note that women show another difference in terms of CVD. In accordance with previous reports [29, 30] showing that women have a poorer prognosis than men, female gender is an independent predictor of poor CVD in patients with CTO. This may partially explain why women have increased mortality after acute MI. A few animal studies tested the role of gender and estrogen on arteriogenesis. Kyriakides et al. [31] reported that gender does not influence angiogenesis and arteriogenesis in a rabbit model of chronic hind limb ischemia. However, they have found that estrogen withdrawal induced by oophorectomy negatively affects angiogenesis and arteriogenesis. Similarly, Lamping et al. [32] have found that ovariectomized rabbits had significantly impaired arteriogenesis, compared with ovariectomized rabbits with estrogen treatment. Recently, Mouquet et al. [33] reported that collateral circulation is less developed in women with CTO. Therefore, we speculate that withdrawal of estrogen due to menopause might have a negative effect on arteriogenesis. The exact pathophysiological mechanisms, however, remain to be elucidated.
There are some issues need to be addressed as limitations. We have assessed the severity and extent of CAD by eyeballing. Pressure and Doppler-derived intracoronary collateral measurements are regarded as the reference method for clinical assessment of coronary collateral flow [17]. Ineligibility of intravascular ultrasound and collateral flow measurement systems were the main reasons for not including those methods. However, considerable amount of patients with total occlusion has partially eliminated this limitation in terms of determining lesion severity. Another limitation is that type of DM, length of DM and treatment duration have not been recorded in our database, and therefore, further analysis regarding those variables could not be done.
In conclusion, we have demonstrated that DM is an independent denominator for poor CVD both in patients with severe coronary artery stenosis and in patients with CTO. Besides DM, female gender in menopause is the other negative predictor of poor CVD in patients with CTO.
References
Arras M, Ito WD, Scholz D, Winkler B, Schaper J, Schaper W (1998) Monocyte activation in angiogenesis and collateral growth in the rabbit hindlimb. J Clin Invest 101:40–50
Khmelewski E, Becker A, Meinertz T, Ito WD (2004) Tissue resident cells play a dominant role in arteriogenesis and concomitant macrophage accumulation. Circ Res 95:E56–E64
Billinger M, Kloos P, Eberli FR et al (2002) Physiologically assessed coronary collateral flow and adverse cardiac ischemic events: a follow up study in 403 patients with coronary artery disease. J Am Coll Cardiol 40:1545–1550
Habib GB, Heibig J, Forman SA et al (1991) Influence of coronary collateral vessels on myocardial infarct size in humans: results of phase I thrombolysis in myocardial infarction (TIMI) trial. The TIMI investigators. Circulation 83:739–746
Hansen JF (1989) Coronary collateral circulation: clinical significance and influence on survival in patients with coronary artery occlusion. Am Heart J 117:290–295
Abaci A, Oğuzhan A, Kahraman S, Eryol NK, Unal S, Arinç H, Ergin A (1999) Effect of diabetes mellitus on formation of coronary collateral vessels. Circulation 99:2239–2242
Turhan H, Yasar AS, Erbay AR, Yetkin E, Sasmaz H, Sabah I (2005) Impaired coronary collateral vessel development in patients with metabolic syndrome. Coron Artery Dis 16:281–285
Zbinden R, Zbinden S, Billinger M, Windecker S, Meier B, Seiler C (2005) Influence of diabetes mellitus on coronary collateral flow: an answer to an old controversy. Heart 91:1289–1293
Heil M, Eitenmüller I, Schmitz-Rixen T, Schaper W (2006) Arteriogenesis versus angiogenesis: similarities and differences. J Cell Mol Med 10:45–55
Kocaman SA, Arslan U, Tavil Y, Okuyan H, Abaci A, Cengel A (2008) Increased circulating monocyte count is related to good collateral development in coronary artery disease. Atherosclerosis 197:753–756
Rentrop KP, Cohen M, Blanke H, Phillips RA (1985) Changes in collateral channel filling immediately after controlled coronary artery occlusion by an angioplasty balloon in human subjects. J Am Coll Cardiol 5:587–592
Werner GS, Jandt E, Krack A, Schwarz G, Mutschke O, Kuethe F, Ferrari M, Figulla HR (2004) Growth factors in the collateral circulation of chronic total coronary occlusions: relation to duration of occlusion and collateral function. Circulation 110:1940–1945
de Vries J, Anthonio RL, van den Heuvel AF, Tan ES, Jessurun GA, de Smet BJ, DeJongste MJ, Zijlstra F (2007) Incidence and angiographic predictors of collateral function in patients with stable coronary artery disease scheduled for percutaneous coronary intervention. Catheter Cardiovasc Interv 70:197–202
Fujita M, Nakae I, Kihara Y, Hasegawa K, Nohara R, Ueda K, Tamaki S, Otsuka K, Sasayama S (1999) Determinants of collateral development in patients with acute myocardial infarction. Clin Cardiol 22:595–599
Nathoe HM, Koerselman J, Buskens E, van Dijk D, Stella PR, Plokker TH, Doevendans PA, Grobbee DE, de Jaegere PP (2006) Determinants and prognostic significance of collaterals in patients undergoing coronary revascularization. Am J Cardiol 98:31–35
Kyriakides ZS, Psychari S, Chrysomallis N, Georgiadis M, Sbarouni E, Kremastinos DT (2002) Type II diabetes does not prevent the recruitment of collateral vessels and the normal reduction of myocardial ischaemia on repeated balloon inflations during angioplasty. Heart 87:61–66
Seiler C (2010) The human coronary collateral circulation. Eur J Clin Invest 40:465–476
Werner GS, Richartz BM, Heinke S, Ferrari M, Figulla HR (2003) Impaired acute collateral recruitment as a possible mechanism for increased cardiac adverse events in patients with diabetes mellitus. Eur Heart J 24(1134):1142
Waltenberger J (2001) Impaired collateral vessel development in diabetes: potential cellular mechanisms and therapeutic implications. Cardiovasc Res 49:554–560
Waltenberger J, Lange J, Kranz A (2000) Vascular endothelial growth factor-A-induced chemotaxis of monocytes is attenuated in patients with diabetes mellitus: a potential predictor for the individual capacity to develop collaterals. Circulation 102:185–190
Tchaikovski V, Olieslagers S, Böhmer FD, Waltenberger J (2009) Diabetes mellitus activates signal transduction pathways resulting in vascular endothelial growth factor resistance of human monocytes. Circulation 120:150–159
Czepluch FS, Waltenberger J (2008) Monocyte function rather than number is a prerequisite for the stimulation of collateral growth. Atherosclerosis 196:485–486
Schaper W (1993) Coronary collateral development: concepts and hypotheses. In: Schaper W, Schaper J (eds) Collateral circulation: heart, brain, kidney, limbs. Kluwer Academic Publishers, Boston, pp 41–64
Hoefer IE, van Royen N, Rectenwald JE et al (2004) Arteriogenesis proceeds via ICAM-l/Mac-1-mediated mechanisms. Circ Res 94:1179–1185
Hoefer IE, Grundmann S, van Royen N, Voskuil M, Schirmer SH, Ulusans S, Bode C, Buschmann IR, Piek JJ (2005) Leukocyte subpopulations and arteriogenesis: specific role of monocytes, lymphocytes and granulocytes. Atherosclerosis 181:285–293
Ito WD, Arras M, Winkler B, Scholz D, Schaper J, Schaper W (1997) Monocyte chemotactic protein-1 increases collateral and peripheral conductance after femoral artery occlusion. Circ Res 80:829–837
Heil M, Ziegelhoeffer T, Pipp F et al (2002) Blood monocyte concentration is critical for the enhancement of collateral artery growth (arteriogenesis). Am J Physiol Heart Circ Physiol 283:H2411–H2419
Bergmann CE, Hoefer IE, Meder B, Roth H, van Royen N, Breit SM, Jost MM, Aharinejad S, Hartmann S, Buschmann IR (2006) Arteriogenesis depends on circulating monocytes and macrophage accumulation and is severely depressed in op/op mice. J Leukoc Biol 80:59–65
Vaccarino V, Parsons L, Every NR, Barron HV, Krumholz HM (1999) Sex-based differences in early mortality after myocardial infarction. National Registry of myocardial infarction 2 participants. N Engl J Med 341:217–225
Lansky AJ, Hochman JS, Ward PA, Mintz GS, Fabunmi R, Berger PB, New G, Grines CL, Pietras CG, Kern MJ, Ferrell M, Leon MB, Mehran R, White C, Mieres JH, Moses JW, Stone GW, Jacobs AK, American College of Cardiology Foundation; American Heart Association (2005) Percutaneous coronary intervention and adjunctive pharmacotherapy in women: a statement for healthcare professionals from the American Heart Association. Circulation 111:940–953
Kyriakides ZS, Petinakis P, Kaklamanis L, Lyras T, Sbarouni E, Karayannakos P, Iliopoulos D, Kremastinos DT (2003) Gender does not influence angiogenesis and arteriogenesis in a rabbit model of chronic hind limb ischemia. Int J Cardiol 92:83–91
Lamping KG, Christensen LP, Tomanek RJ (2003) Estrogen therapy induces collateral and microvascular remodeling. Am J Physiol Heart Circ Physiol 285:H2039–H2044
Mouquet F, Cuilleret FJ, Susen S, Ennezat PV, Letourneau T, Doevendans PAM et al (2009) Collateral vessel formation in patients with documented coronary occlusion: role of gender, smoking and of their combination. Eur Heart J 30(Abstract Supplement):357
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yetkin, E., Topal, E., Erguzel, N. et al. Diabetes mellitus and female gender are the strongest predictors of poor collateral vessel development in patients with severe coronary artery stenosis. Angiogenesis 18, 201–207 (2015). https://doi.org/10.1007/s10456-015-9460-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10456-015-9460-y