Abstract
Information about airborne fungal spore is crucial for health risk assessment and management, especially for patients with allergy and asthma. Nonetheless, such data are rarely available from certain areas of the world, including Southeast Asia. The aim of this study was to gain updated information about airborne fungal spore in Bangkok, the capital city of Thailand. A survey was conducted at five sampling sites in Bangkok, using the Rotorod Sampler® for a period of 1 year. High concentrations of spores were found all year with the peak between August and November. The most prominent spore types were Cladosporium, Nigrospora, Puccinia, Aspergillus/Penicillium, and Fusarium. The spore concentrations were positively and significantly correlated with the amount of rainfall and relative humidity, reaching the maximum level in September. Sensitization rates to Cladosporium, Penicillium, and Aspergillus among Thai atopic patients were approximately 16.6, 13.6, and 13.0%, respectively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
With over one million species described to date, fungi are highly successful organisms that occupy a wide range of ecological niches. They can produce copious amounts of spores with diameters typically < 10 µm and thus can be suspended in the air for an extended period. Several fungal spores had been shown to cause nasal symptoms and affect lower airways, especially by aggravating respiratory diseases, including allergy, rhinosinusitis, and asthma (Raulf et al. 2014). It had been estimated that 2.8–10.7% of total airborne fungal taxa are allergenic (Yamamoto et al. 2012). The World Allergy Organization (WAO) has estimated that incidence of fungal spore sensitization is up to 10% worldwide (Maio et al. 2011). In Thailand, the overall prevalence of major allergic diseases increased significantly from 1995 to 2008, with allergic rhinitis patients increasing from 37.9 to 50.6%, affecting millions of people in Bangkok alone (Pawankar et al. 2012). Yet, information about fungal spores in Thailand is limited.
Types and concentrations of fungal spores depend on climate, which varies significantly in different locations. Even though there have been a number of reports on fungal spores, only a limited number of reports are available from hot and humid areas, especially from Asia Pacific region. To this end, the latest report of airborne fungal spore in Thailand was published over 30 years ago (Dhorranintra et al. 1988). With the rapid development of the city, it is hypothesized that the amount and/or types of fungal spores may have changed. Furthermore, the climate change due to human activities can significantly change fungal spore distribution, both spatially and temporally. Thus, there is a pressing need for more updated information. We report the updated airborne fungal spore distribution in Bangkok, the capital city of Thailand. In addition, the correlation between airborne fungal spores and skin prick test results and meteorological parameters is presented.
2 Materials and methods
2.1 Study area
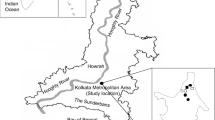
Bangkok is located in Central Thailand (13.7563°N, 100.5018°E) on the Chao Phraya River Delta. As one of the busiest cities in Southeast Asia, Bangkok city has a reported population of over 8 million with about 5300 persons/km2 density (National Statistical Office 2010). Together with the extended Bangkok Metropolitan, the population is over 14.5 million, accounting for more than 22% of the country’s population. With the total area of about 1500 km2, the city of Bangkok is divided into 50 districts. Five districts, each with one sampling site, were chosen to give a good coverage of Bangkok, namely Pathum Wan (southern Bangkok), Phra Khanong (southern Bangkok), Chatuchak (northern Bangkok), Lat Krabang (eastern Bangkok), and Bangkok Noi (northwestern Bangkok) (Fig. 1). The minimum distance between sampling locations was approximately 6 km and the maximum 30 km. Population density (person/km2) varied among the sampling sites Pathum Wan (6287), Phra Khanong (6633), Chatuchak (4891), Lat Krabang (1338), and Bangkok Noi (9838) (Bangkok Metropolitan Administration 2013).
The climate of Bangkok is classified as a tropical savanna climate and is under the influence of seasonal monsoon winds. The southwest monsoon from mid-May to mid-October brings rainfalls. The rainfall is highest in September with the mean rainfall of 334 mm and mean rainy days of 21.2 days. The northeast monsoon from mid-October to mid-February brings cooler and dryer air from China. Yet, the lowest mean temperature of c 22 °C is experienced in December. The summer (mid-February–mid-May) is hot and generally dry, with occasional summer storm. The hottest month is April with mean minimum of 26.9 °C and maximum of 35.4 °C (Thai Meteorological Department 2010).
2.2 Sampling method
The Rotorod Sampler® Model 20 with fixed sampling head (Multidata LLC, MN 55416, USA) was used for the survey. The sampler was placed on the unobstructed balcony of a residential house at approximately 4 m from the ground, except for the Bangkok Noi site, where the sampler was placed on the seventh floor of a hospital building at approximately 20 m above ground. Two silicone greased rods were attached to the sampling heads at a time, and the motor speed was set at 2400 RPM according to the manufacturer instruction. The sampling device was turned on for 1 h (approximately from 10:00 a.m. to 11:00 a.m.) twice a week throughout the 12-month period of the study (May 2012–April 2013). After exposure, the exposed rods were stored in plastic containers and analyzed by trained readers. This study was done in concurrent, and thus using the same setting, with the airborne pollen survey previously reported (Songnuan et al. 2015).
2.3 Fungal spore identification
The exposed rods were stained with Calberla’s solution, composed of glycerol, ethyl alcohol, water, and basic fuchsine. Fungal spores were identified and counted by five trained readers, and each reader was randomly assigned to analyze rods from all sites. Spore identification was based on physical characteristics seen under a light microscope with 400 × magnification.
Of the two rods exposed at the same time, only one rod was randomly chosen for spore counting. If the rod appeared damaged, the analysis was performed on the other rod. Due to the numerous amounts of fungal spores on the rods, the spore count was performed only within the area of two vertical sweeps (one up and one down) in the middle of cover slip. The fungal spores were then related to the amount of air sampled by the collector rod, expressed as fungal spores per cubic meter of air (spores/m3) according to the Rotorod Sampler® operating instructions.
2.4 Meteorological data
Meteorological data, including daily minimum and maximum temperature, wind speed, rainfall, and relative humidity, of Bangkok were obtained from Thai Meteorological Department http://www.tmd.go.th/climate/climate.php. Data were averaged from two weather stations: Klong Toey (station code 455201) and Bang Na (station code 455301).
2.5 Statistical analysis
To determine the correlation between fungal spore concentrations and meteorological variables, Spearman’s correlation coefficient was determined using the SPSS statistical software, version 18.0.
2.6 Clinical data
Data from routine skin prick test results were obtained between 2010 and 2014 from the Ear, Nose and Throat (ENT) Allergy Clinic, Siriraj Hospital in Bangkok Noi district, Bangkok. The wheal diameter of more than 3 mm with flare was considered a positive result.
3 Results
3.1 Airborne fungal spores and seasonal variation
In total, 968 rods were collected and fungal spores were found in about 93% of all analyzed rods. There was a wide range in the number of spores found in each rod, with most rods having moderate spore counts and a few rods having extremely high counts. Overall, the average concentration of fungal spores calculated from all five sites during the study period was 11,211.89 spores/m3, while the median was only 5076.92 spores/m3. The higher concentrations formed a broad peak from August to November. September was the month with the highest spore concentration (average 20,489.94 spores/m3; median 17,092.3 spores/m3) (Fig. 2) and the highest percentage of rods with > 10,000 spores/m3 (87%) (Fig. 3). The highest calculated spore concentration from one rod was found in November (221,523.08 spores/m3). Relatively low spore concentrations were found in March and April, corresponding to the summer months in Bangkok. The lowest concentration was found in June, with the average of 4208 spores/m3 and median of 2369 spores/m3.
The concentrations of fungal spores were variable among the collection sites. The year-round prevalence of fungal spores was highest in Bangkok Noi (average 14,331.70 spores/m3, median 9815.38 spores/m3), which was about 2–3 times higher than in Phra Khanong where the lowest concentration was found (average 7497.75 spores/m3; median 2707.69 spores/m3) (Fig. 4). Bangkok Noi also had the highest frequency of rods with spore concentrations between 10,000 and 100,000 spores/m3 (almost 50%). Low correlation coefficients were exhibited between spore concentrations among different sites, with the highest value of 0.30 (p value < 0.01) between Bangkok Noi and Phra Khanong, which are not geographically adjacent districts (data not shown).
3.2 Spore types
In this survey, fungal spores were classified into 21 groups based on their morphological appearance under the microscope. Aspergillus and Penicillium spores had indistinguishable appearance and thus were grouped together. Fungal spores that could not be identified were grouped as the “unknown fungus.” When only a mycelium fragment was found, it was noted in the “mycelium fragment” category. Among all collected fungal spores, Cladosporium spore was found with the highest concentration, with the average of 5535.66 spores/m3 and the maximum of more than 200,000 spores/m3 (Table 1). Cladosporium spore contributed about 49.37% of all fungal spores found during the study period. Puccinia, Nigrospora, Aspergillus/Penicillium, and Fusarium spores were the top five types of most commonly found spores, each contributing approximately 7.89–9.94% of the total spore count, with the average concentration ranging between 884.97 and 1113.99 spores/m3. Yeast, Curvularia, Alternaria, Helminthosporium, and Pithomyces spores comprised between 1.04 and 4.51% of the total spore count (116.78–505.24 spores/m3). Together, all other known spore types, including Papularia, black yeast, Torula, Tetraploa, Spegazzinia, Microsporum, Scapularia, Peltularia, and Bipolaris contributed about 2.16%. Mycelium fragment contributed about 0.14% of the total count, and 2.78% of fungal spores could not be identified.
Even though Cladosporium spore was present in the highest average concentration, it was only observed in 62.17% of all rods. The presence of Cladosporium spore was also highly variable among the five sampling sites, ranging between 27.55% in Lad Krabang and 96.19% in Bangkok Noi (Fig. 6). The most frequently observed fungal spore was Nigrospora, which was present in 88.72% of all rods, followed by Fusarium (72.35%) and Puccinia (72.35%). Moreover, Nigrospora spore was frequently observed (> 70% of all rods) at all five sampling sites.
From August to October was the period in which fungal spores were the most abundant, although high levels of some fungal spore types could be found in other periods (Fig. 5). Interestingly, Cladosporium spore was low in abundance in this period; instead, it was highly abundant in November–April. Nigrospora was present in most rods year-round. On the other hand, Aspergillus/Penicillium had a high prevalence in August–October and was present in fewer than 50% of the rods and in low concentration for the rest of the year. High prevalence of multiple fungal spores was frequently found in Bangkok Noi and Chatuchak, of which the top most species were the combination of Nigrospora, Fusarium, Puccinia, Cladosporium, Curvularia, and Aspergillus/Penicillium (Fig. 6).
3.3 Meteorological information
Climatic data during the survey period are shown in Table 2. The minimum temperature was between 19.7 and 24.6 °C, and the maximum temperature was between 35.2 and 40.1 °C. Wind velocity was between 15 and 27 km/h. These meteorological parameters were not significantly correlated with the amount of airborne fungal spore. However, the amount of rainfall (7.4–601.1 mm) and relative humidity (67–85%) were found to be positively and significantly correlated with the amount of fungal spores with correlation coefficients of 0.890 and 0.719, respectively (p value < 0.01). In September, when the fungal spores were found to be at the highest concentration, both the rainfall and relative humidity were also at their maximum levels (Fig. 7).
Statistical analysis also showed the significant correlations between rainfall and relative humidity with some fungal spores including Alternaria, Cladosporium, Fusarium, and Helminthosporium, respectively (p value < 0.05). Amount of Aspergillus/Penicillium, Curvularia, Nigrospora, and Puccinia spores did not significantly correlate with any meteorological variables.
3.4 Sensitization of Thai atopic patients to fungal spores
The ENT Allergy Clinic at Siriraj Hospital, located in Bangkok Noi district, has performed routine skin prick test (SPT) for patients with rhinitis symptoms using crude extracts from several airborne allergens, including three different fungal species, i.e., Cladosporium, Penicillium, and Aspergillus. Out of 1863 patients who had SPT done between 2010 and 2014, 1296 (69.6%) had a positive reaction (wheal diameter ≥ 3 mm with flare) to at least one airborne allergen and was diagnosed with allergic rhinitis (AR). Among this, 215 (16.6%) showed sensitization to Cladosporium, 176 (13.6%) to Penicillium, and 168 (13.0%) to Aspergillus (Fig. 8). The numbers of patients sensitized to different fungal species were positively correlated with each other, with the correlation coefficient between 0.90 and 0.94.
4 Discussion
This study reports the most updated information on airborne fungal spore distribution and seasonal variation from Bangkok, Thailand, in over three decades. Until now there have been few airborne fungal spore reports from hot and humid areas, including from Southeast Asia. The lack of such information is concerning because airborne fungal spores can lead to several respiratory diseases such as allergy and asthma, of which the incidences are constantly increasing, especially among children.
The average fungal spore concentration in Bangkok was found to be high at above 10,000 spores/m3. Even in the months with low spore counts, the concentrations remained above 2000 spores/m3, most likely exceeding the threshold of 500 CFU/m3 set by WHO and ACGIH guidelines (Salonen et al. 2015). In addition, spore count of > 1000 spores/m3 is regarded as significant for clinical correlation of diseases (Targonski et al. 1995). The most abundant spore types based on average concentration were Cladosporium, Nigrospora, Fusarium, Puccinia, and Aspergillus/Penicillium, respectively. However, based on the frequency of occurrence, Nigrospora spore was the most abundant and Curvularia spore should also be considered as highly prevalent, as it is present in more than 50% of the analyzed rods. In comparison, the previous report of outdoor fungi in Bangkok in 1982 also found Aspergillus, Cladosporium, and Curvularia as major spore types, along with yeast and white fungi (Bunnag et al. 1982a). Similar major spore types were also found in neighboring countries and in other parts of the world, including Singapore (Lim et al. 1998), Malaysia (Ho et al. 1995), Taiwan (Wu et al. 2007), Japan (Takanori 1997), Saudi Arabia (Hasnain et al. 2012), and Portugal (Oliveira et al. 2010). Cladosporium was found to be the most prominent fungal spore type in the temperate region (Goncalves et al. 2010).
Significant correlation was found between fungal spore concentration and two related meteorological variables: amount of rainfall and relative humidity. Based on the average and median concentrations, frequency of occurrence, and date of maximum concentration, most spore types reached their peaks in the months with high rainfall and high humidity. This is in agreement with several other studies (Herrero et al. 2006; Katial et al. 1997). Interestingly, a previous study from Thailand found that the spores were high in the winter months and low during the rainy season, which could be due to the seasonal shift or the different collection methods (Bunnag et al. 1982a). On the other hand, some studies found a negative correlation with RH and rainfall or significant correlations with other meteorological variables, including lowest and highest temperature or wind speed (Hasnain et al. 2012; Oliveira et al. 2010; Reyes et al. 2016). This discrepancy might be due to the difference in the overall climate and the genera and species of the observed fungi. With the global climate change, higher RH and precipitation are likely, which can result in greater fungal growth (Jalbert and Golebiowski 2015). Thus, vigilant control of possible fungal sources is needed.
It has long been known that airborne fungal spores can cause a number of respiratory diseases, including allergy and asthma. For example, Aspergillus and Penicillium were significantly associated with asthma in children (Reponen et al. 2012). Allergic sinusitis is associated with Alternaria, Aspergillus, Bipolaris, Chrysosporium, and Curvularia (Brook 2011). Five years of SPT results showed that Thai allergic rhinitis patients have 7–24% sensitization to three tested major fungal spores. Incidences of sensitization to Cladosporium spore were slightly higher than those of Penicillium and Aspergillus spores, which could reflect the fact that Cladosporium spore was the most abundant spore type. Nonetheless, the sensitization rates of these three spore types were significantly correlated. A previous study from Thailand showed comparable fungal spore sensitization rates (Pumhirun et al. 1997). Similarly, in Singapore it was reported that Cladosporium spore elicited positive SPT results in approximately 16.5% of allergic rhinitis patients, which was lower than the rate of sensitivity to Curvularia, Pithomyces, Bipolaris, and Tetraploa (Chew et al. 2000). Skin sensitivity to Cladosporium and Aspergillus was found in 5 and 3.4% of asthmatic atopic patients, respectively, in Thessaloniki, Greece (Gioulekas et al. 2004). No information about sensitization to other major spore types, including Nigrospora and Puccinia, is available, suggesting that much more research is needed to gain more complete knowledge of fungal spore sensitization. It was previously reported that spore concentration of more than 3000 spores/m3 of Cladosporium and more than 100 spores/m3 of Alternaria can evoke allergic symptoms (Twaroch et al. 2015). If this is the case, then patients with Cladosporium allergy could have symptoms year-round, except between June and October, when the lower concentration was found. Nonetheless, patients may develop symptoms all year because clinical data suggest significant overlap between sensitization to Cladosporium and Aspergillus/Penicillium, which peaked in July–November. Further study should include children, since it had been previously demonstrated that fungus sensitization is more prevalent in children. Alternaria sensitivity was shown to increase in childhood and decline with age (Twaroch et al. 2015).
The rate of sensitization to fungal spores compared to that of other airborne allergens was considerably low, especially when compared to house dust mite (> 70% of allergic rhinitis patients or > 40% of adult asthmatic patients) (Daengsuwan et al. 2003; Pumhirun et al. 1997). The low rate of sensitization to fungal spores was similarly found in the previous study in Thailand (Bunnag et al. 1982b). This was previously noted, and the possible explanation was because the commercially available extract was from species different from those locally found or that the extract may be of poor quality. Thus, the actual number of patients sensitized to fungal spores may be much higher. An alternative hypothesis was that the fungus-induced asthma was due to non-allergic mechanism (Reponen et al. 2012; Twaroch et al. 2015). Nonetheless, for those who are strongly affected by fungus allergy, the immunotherapy is not very effective and with side effects (Twaroch et al. 2015). Patients must rely on avoidance as the best option. Therefore, local fungal spore monitoring and proper managements should be recommended, especially in areas where children and sensitized individuals often reside, such as schools and hospitals. A number of allergenic fungi, including Cladosporium and Alternaria, thrive on agricultural fields. In fact, decomposing plant debris is a larger reservoir of allergenic fungi than the soils (Weikl et al. 2015). Therefore, crop waste management can play a key role in reducing airborne fungal spores, especially in an agriculture-based country like Thailand.
5 Conclusion
Updated information on airborne fungal spores in the areas of Bangkok Metropolitan since the last survey 35 years ago had been reported herein. The majority of spore counts were found during the rainy months, and their amounts were correlated with rainfall and relative humidity. The most prominent spore types were Cladosporium, Puccinia, Nigrospora, Aspergillus/Penicillium, and Fusarium. However, the prevalence of positive skin test with several fungal extracts was not as high as expected, probably due to the limited availability of good-quality extracts to determine the broad spectrum of fungal sensitization. Therefore, more types of fungal extracts should be produced, especially the abundant fungal types, in order to precisely diagnose the patient’s sensitization.
References
Bangkok Metropolitan Administration. (2013). Statistical Profile of Bangkok Metropolitan Administration 2013. Retrieved September 19, 2016, from Strategy and Evaluation Department Bangkok Metropolitan Administration. http://www.bangkok.go.th/main/backoffice/upload_editor/file/stat2013(ENG).pdf. Accessed 10–12 July 2013.
Brook, I. (2011). Microbiology of sinusitis. Proceedings of the American Thoracic Society, 8(1), 90–100.
Bunnag, C., Dhorranintra, B., & Plangpatanapanichya, A. (1982a). A comparative study of the incidence of indoor and outdoor mold spores in Bangkok, Thailand. Annals of Allergy, 48, 333–339.
Bunnag, C., Dhorranintra, B., & Plangpatanapanichya, A. (1982b). The incidence of airborne molds and the relationship with skin sensitivity test. Siriraj Hospital Gazette, 34, 883–890.
Chew, F. T., et al. (2000). Evaluation of the allergenicity of tropical pollen and airborne spores in Singapore. Allergy, 55(4), 340–347.
Daengsuwan, T., Lee, B. W., Visitsuntorn, N., Charoenratanakul, S., Ruangrak, S., Jirapongsananuruk, O., et al. (2003). Allergen sensitization to aeroallergens including Blomia tropicalis among adult and childhood asthmatics in Thailand. Asian Pacific Journal of Allergy and Immunology, 21, 199.
Dhorranintra, B., Bunnag, C., & Limsuvan, S. (1988). Survey of airborne fungal spores in Thailand. Allergy, 8(1), 51–55.
Gioulekas, D., Balafoutis, C., Damialis, A., Papakosta, D., Gioulekas, G., & Patakas, D. (2004). Fifteen years’ records of airborne allergenic pollen and meteorological parameters in Thessaloniki, Greece. International Journal of Biometeorology, 48, 128–136.
Goncalves, F. L., Bauer, H., Cardoso, M. R., Pukinskas, S., Matos, D., Melhem, M., et al. (2010). Indoor and outdoor atmospheric fungal spores in the Sao Paulo metropolitan area (Brazil): Species and numeric concentrations. International Journal of Biometeorology, 54(4), 347–355.
Hasnain, S. M., Akhter, T., & Waqar, M. A. (2012). Airborne and allergenic fungal spores of the Karachi environment and their correlation with meteorological factors. Journal of Environmental Monitoring, 14(3), 1006–1013.
Herrero, A. D., Ruiz, S. S., Bustillo, M. G., & Morales, P. C. (2006). Study of airborne fungal spores in Madrid, Spain. Aerobiologia, 22(2), 133.
Ho, T. M., Tan, B. H., Ismail, S., & Bujang, M. K. (1995). Seasonal prevalence of air-borne pollen and spores in Kuala Lumpur, Malaysia. Asian Pacific Journal of Allergy and Immunology, 13(1), 17–22.
Jalbert, I., & Golebiowski, B. (2015). Environmental aeroallergens and allergic rhino-conjunctivitis. Current opinion in Allergy and Clinical Immunology, 15(5), 476–481.
Katial, R. K., Zhang, Y., Jones, R. H., & Dyer, P. D. (1997). Atmospheric mold spore counts in relation to meteorological parameters. International Journal of Biometeorology, 41(1), 17–22.
Lim, S. H., Chew, F. T., Dali, S. D. B. M., Tan, H. T. W., Lee, B. W., & Tan, T. K. (1998). Outdoor airborne fungal spores in Singapore. Grana, 37(4), 246–252.
Maio, S., Cerrai, S., Simoni, M., Sarno, Giuseppe, Baldacci, S., & Viegi, G. (2011). Environmental risk factors: Indoor and outdoor pollution. In R. Pawankar, G. W. Canonica, S. T. Holgate, & R. F. Lockey (Eds.), WAO white book on allergy. Milwaukee: World Allergy Organization.
National Statistical Office. (2010). The 2010 Population and Housing Census. Retrieved September 19, 2016, from National Statistical Office, Ministry of information and Communication Technology. http://popcensus.nso.go.th/file/popcensus-10-01-56-E.pdf. Accessed 10–12 July 2013.
Oliveira, M., Ribeiro, H., Delgado, L., Fonseca, J., Castel-Branco, M., & Abreu, I. (2010). Outdoor allergenic fungal spores: Comparison between an urban and a rural area in Northern Portugal. Journal of Investigational Allergology and Clinical Immunology, 20(2), 117–128.
Pawankar, R., Bunnag, C., Khaltaev, N., & Bousquet, J. (2012). Allergic rhinitis and its impact on asthma in Asia Pacific and the ARIA update 2008. World Allergy Organization Journal, 5(Suppl 3), S212–S217.
Pumhirun, P., Towiwat, P., & Mahakit, P. (1997). Aeroallergen sensitivity of Thai patients with allergic rhinitis. Asian Pacific Journal of Allergy and Immunology, 15, 183–185.
Raulf, M., et al. (2014). Monitoring of occupational and environmental aeroallergens—EAACI Position Paper. Concerted action of the EAACI IG Occupational Allergy and Aerobiology & Air Pollution. Allergy, 69(10), 1280–1299.
Reponen, T., et al. (2012). Infant origins of childhood asthma associated with specific molds. Journal of Allergy and Clinical Immunology, 130(3), 639–644.
Reyes, E. S., de la Cruz, D. R., & Sánchez, J. S. (2016). First fungal spore calendar of the middle-west of the Iberian Peninsula. Aerobiologia, 32(3), 529–539.
Salonen, H., Duchaine, C., Mazaheri, M., Clifford, S., Lappalainen, S., Reijula, K., et al. (2015). Airborne viable fungi in school environments in different climatic regions—A review. Advances in Atmospheric Sciences, 104, 186–194.
Songnuan, W., Bunnag, C., Soontrapa, K., Pacharn, P., Wangthan, U., Siriwattanakul, U., et al. (2015). Airborne pollen survey in Bangkok, Thailand: A 35-year update. Asian Pacific Journal of Allergy and Immunology, 33(3), 253–262.
Takanori, T. (1997). Airborne fungal colony-forming units in outdoor and indoor environments in Yokohama, Japan. Mycopathologia, 139(1), 23–33.
Targonski, P. V., Persky, V. W., & Viswanathan, R. (1995). Effect of environmental molds on risk of death from asthma during the pollen season. Journal of Allergy and Clinical Immunology, 95(5), 955–961.
Thai Meteorological Department. (2010). Climatological data for the period 1981–2010. Retrieved September 19, 2016, from Thai Meteorological Department. http://climate.tmd.go.th/content/file/75. Accessed 10–12 July 2013.
Twaroch, T. E., Curin, M., Valenta, R., & Swoboda, I. (2015). Mold allergens in respiratory allergy: From structure to therapy. Allergy, Asthma & Immunology Research, 7(3), 205–220.
Weikl, F., Radl, V., Munch, J. C., & Pritsch, K. (2015). Targeting allergenic fungi in agricultural environments aids the identification of major sources and potential risks for human health. Science of the Total Environment, 529, 223–230.
Wu, Y. H., Chan, C. C., Rao, C. Y., Lee, C. T., Hsu, H. H., Chiu, Y. H., et al. (2007). Characteristics, determinants, and spatial variations of ambient fungal levels in the subtropical Taipei metropolis. Atmospheric Environment, 41(12), 2500–2509.
Yamamoto, N., Bibby, K., Qian, J., Hospodsky, D., Rismani-Yazdi, H., Nazaroff, W. W., et al. (2012). Particle-size distributions and seasonal diversity of allergenic and pathogenic fungi in outdoor air. ISME Journal, 6(10), 1801–1811.
Acknowledgements
Funding was provided by the National Research Council of Thailand and the Faculty of Medicine Siriraj Hospital.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Songnuan, W., Bunnag, C., Soontrapa, K. et al. Airborne fungal spore distribution in Bangkok, Thailand: correlation with meteorological variables and sensitization in allergic rhinitis patients. Aerobiologia 34, 513–524 (2018). https://doi.org/10.1007/s10453-018-9527-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10453-018-9527-5