Abstract
The prevalence of HIV in Thailand continues to increase, especially among men who have sex with other men (MSM). Being stigmatized can result in depression, which can negatively impact antiretroviral medication adherence. This quasi-experimental research study aimed to examine the effects of cognitive-behavioral group therapy using art as a medium on depressive symptoms and medication adherence. Forty-six MSM were assigned (23 × 2) either to a weekly 2-h art-based CBGT group session for a total of 8 weeks or to a no-intervention control group. The experimental group of 23 met in 4 separate small groups. Pre-intervention period analyses indicated no significant differences between the two groups in the key variables examined, together with demographic information including the participants’ ages, education levels, and CD4 (T cells) levels. Measures of depressive symptoms and antiretroviral medication adherence were administered pre- and post-intervention. Using MANOVA, findings suggested that depressive symptom scores among the intervention group were reduced significantly post-treatment (p < .01) and were significantly lower than those of the control group (p < .001). Scores among the experimental group for medication adherence increased significantly pre- to post-treatment (p < .025); however, post-treatment scores were not significantly different between the experimental and control groups. These findings provide initial evidence for the potential effectiveness of art-based CBGT in alleviating depressive symptoms and enhancing antiretroviral medication adherence in MSM with HIV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
HIV and AIDS are still widespread in worldwide populations, including in Southeast Asia. In Thailand, records show that approximately 1,166,543 individuals were affected in 2013, including 447,640 living with HIV and 8959 newly infected patients. Men who have sex with other men (MSM) are among those with the highest prevalence (Bureau of AIDS, TB and STIs 2013) and the HIV infection rate in these individuals is projected to continue increasing (Beyrer et al. 2012).
Antiretroviral therapy, a combination of medications used to treat the HIV virus, generally adds 10 years to life expectancy (Antiretroviral Therapy Cohort Collaboration 2017) and reduces the fatality rate among individuals with HIV. Nevertheless, people who are HIV positive are still affected by the debilitating psychological outcomes that often accompany the disease. These can result from chronic physical health deterioration, lifestyle changes, social stigmatization, and compromised social support (Chan et al. 2005). In addition, individuals often report “double discrimination” stemming from their sexual orientation as well as from their HIV status. For this reason, HIV-infected MSM have been reported to be at higher risk of depression (National AIDS Trust 2003).
Ciesla and Roberts (2001) reported that, compared with the general population, HIV-infected MSM are twice as likely to develop depression, which makes this a topic of concern. Depression has been shown to have serious negative impacts that compromise quality of life (Zimpel and Fleck 2014); depression can lead to immunological decline and acceleration of viral load and disease progression (Evans et al. 2002). More importantly, depression has been shown to be negatively correlated with antiretroviral medication adherence, one of the indicators of successful HIV treatment (Rabkin 2008). Stringent medication adherence has been shown to promote quality of life and longevity in HIV-infected individuals by lowering viral load and enhancing patients’ CD4+ (T cells) levels, which evaluates the functions of the immune system for those who live with HIV. In contrast, partial or non-adherence resulting from retroviral side effects, long-term medication intake, and concerns about being seen by others taking medication, could worsen viral suppression and impair health outcomes in those infected by HIV (Safren et al. 2009). A study by Ammassari et al. (2002) also looked into the relationship between depressive symptoms and medication adherence and found that other factors, such as punctuality of taking medication and attitude toward HIV treatment, were also relevant with regard to medication adherence (Ammassari et al. 2002).
Given the association that has been shown in the literature between depression and medication adherence in HIV-infected individuals, attempts have been made to examine the efficacy of counselling and psychotherapy in addressing this issue (e.g., Himelhoch et al. 2007). Cognitive-behavioral therapy (CBT) is regarded as among the most promising interventions for reducing depressive symptoms in this population (Crepaz et al. 2008).
CBT is a widely recognized short-term therapy that aims to reshape patterns of thinking or behavior to foster a more constructive outlook. CBT is based on the notion that behavioral and emotional problems are rooted in logical thinking errors or schema, cultivated as a result of negative past experiences. When individuals encounter new situations, unhelpful automatic thoughts become triggered and affect the manner in which they interpret their experiences, the world, and the future (Corey 2009), predisposing them to negative evaluations. Hence, the objective of CBT is to modify and challenge these evaluations and to slowly transform them into more adaptive ones, using both cognitive (e.g., psychoeducation, cognitive restructuring) and behavioral (e.g., behavioral activation) techniques. Offering time-limited, structured, here-and-now treatment, CBT has shown high empirical evidence for the treatment of many psychological problems, such as anxiety and depression (Butler et al. 2006).
With its evident effectiveness, CBT has been delivered in various formats, including with individuals and with groups. Cognitive behavior group therapy (CBGT; Corey 2009) follows a similar approach to that with individuals; however, group CBT can help promote worldview exchanges and provide social reinforcement. Group members practice activities in the group, in dyads and also individually. Additionally, group brainstorming can be employed for problem-solving and group members can exchange views, thereby creating an environment in which members are enabled to support and model to each other ways to deal with problems. The potential for use of CBT group therapy to improve medication adherence in HIV-infected individuals has also been reported to be promising (Safren et al. 2009).
Whereas CBT has been applied to alleviate depressive mood and enhance antiretroviral medication adherence in Western societies, the use of such approaches in Asian countries remains limited. Various concerns have been raised regarding the reasons for hesitation by Asian individuals to disclose their feelings to others, particularly negative ones. Owing to cultural factors in some Asian countries, Asian people may feel more comfortable discussing practical issues, such as financial or academic problems, than private feelings, especially when sharing with a stranger (Williams et al. 2006). For individuals infected with HIV, subsequent stigmatization and discrimination could increase this hesitation to discuss and receive any therapy help or medications, exacerbating the consequences of the disease (Berger et al. 2001).
For this reason, conducting CBT among Asian HIV-infected MSM might require the use of additional tools. Hence, in the current study, we used art as a medium in CBT therapy. Art itself could possibly be used as the linkage between the counselor and the client when the client’s topics are too sensitive to verbally communicate (Gladding and Newsome 2003). Such usage has been deemed compatible with CBT (Leibowitz-Levy 2005). It has been argued that creating art can form a part of the cognitive reworking process. Additionally, Rubin (2005) stated that creating art can function as a way to translate abstract negative thoughts into more concrete thoughts to be targeted in CBT. In terms of therapeutic progress, art can also be used to demonstrate changes that occur in clients after cognitive restructuring, which can be more productive than using words (Rubin 2005).
Although CBT and art therapy have been implemented together for many years, research studies that assess the benefits of the two used together remain limited (Roghanchi et al. 2013). Based on an examination of the literature, the use art as a medium in treating HIV-infected people is even scarcer. Given the premise outlined above, of using art as a medium in delivering CBT, the objective of the present study was to examine the effects of CBGT using art as a medium (CBGT-A) to decrease depressive symptoms and enhance antiretroviral medication adherence in Thai MSM with HIV infection. The study used a quasi-experimental research design with a pretest–posttest control group. We hypothesized that exposure to both therapies together would decrease depression scores and also increase medication adherence.
Methodology
Participants and Procedures
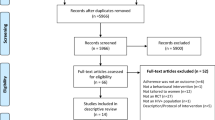
Data collection proceeded after approval was obtained from the ethics review committee for research involving human research subjects of the health science group of Chulalongkorn University. Participants included 46 HIV-infected men who have sex with other men (MSM) who met the inclusion criteria of being 18 years of age or above and taking an antiretroviral medication during the study participation. Exclusion criteria were applied for those identified as having been diagnosed with psychological disorders and had substance abuse issues. Hence, participants in the current study were neither diagnosed with psychological disorders nor engaged in substance abuse.
Participants were recruited from six relevant organizations in Bangkok and vicinity, with two involving public hospitals and four from non-governmental organizations (NGOs). These organizations mostly support individuals with HIV infection, especially gay men, men who have sex with other men and transgender people. The care and support is given in various ways, including facilitating access to HIV tests and treatments, and providing information about HIV infection. As well, the NGOs advocate for HIV protection and protect HIV infected people’s rights to health care services. Additionally, each setting has case managers who contact and enhance social connections among people living with HIV and organizations with special circumstances, and conduct such activities as monthly meetings or excursion camps. After contacting these organizations and informing them of the inclusion criteria, their care and support officers who functioned as gate-keepers helped contact potential participants, who after being informed about the study details indicated whether they would volunteer to participate in the study.
Participants provided written voluntary consent to participate in the study. Prior to and after the intervention period, all participants were asked to complete measures of depressive mood (Center for Epidemiologic Studies Depression Scale; CES-D-10) and antiviral medication adherence (Visual Analog Scale; VAS). Participants from the six settings (mean age 37.96; SD = 9.17) were equally assigned into one of the two groups (i.e., treatment or control), with 23 individuals in each group. Preliminary analyses indicated that there were no significant differences between the two groups on scores for the study variables, including age (t(44) = 1.21, n.s.), education (X2(4, N = 46) = 8.23, n.s.), and CD4+ levels (t(44) = .04, n.s.)
The twenty-three participants in the experimental group were assigned into 4 groups, with five to six participants in each, and they received eight, weekly, two-hour CBT group sessions including art as a medium, that were designed to reduce depressive mood and increase antiviral medication adherence. The groups were conducted by the researcher as a group facilitator, along with well-trained postgraduate-training co-leaders, held at the university or a private psychological clinic, involving a total 16 hours of group participation. The co-leaders had each received postgraduate training in counseling psychology and CBT and had completed an internship of at least 200 hours. The co-leaders helped support the group process.
A requirement for involvement was that, each participant needed to attend at least 6 of the 8 sessions provided. It turned out that 3 participants failed to attend all of the sessions (i.e., each with one session missing); however, they were scheduled an extra appointment to review the missing session material in each case. Hence, all of the participants in the treatment group covered all of the treatment materials.
The non-intervention control group followed the same process, except they did not participate in the CBGT-A, although they still retained contact with the HIV organizational services. After completing the post-period measures, they received a booklet about ways to deal with depression and to increase adherence.
Intervention
The CBGT with art as a medium used in this study was developed based on the main theses of CBT (Beck 2005). Treatment components targeting depressive mood and medication adherence were drawn from the work of Safren et al. (2001), with the application of art as a medium being based on the conceptual work of Malchiodi (2003). Prior to delivery to the groups, the program was reviewed by two therapists experienced in CBT and one dedicated CBGT therapist for appropriateness of its use with individuals infected by HIV; the program was then pilot tested with another six-person HIV voluntary sample, who attended an 8-week group session program. Feedback and information obtained from the pilot group led the researcher to adjust some of the group activities and session plans so that they became most suitable.
As shown below, each CBT-A session in the group program was divided into three phases. The first phase entailed a review of the previous session and a brief introduction and psychoeducation on the topic to be introduced. In the second phase, the session’s main topic—which could be a cognitive or behavioral skill relevant to depressive mood and medication adherence—was addressed in detail, with skill practice applied when appropriate. Finally, in the last phase, homework assignments were given for skill practice and generalization. Opportunity for involving art work in the process was taken wherever possible and relevant.
As for overall plan progression (see Table 1), Session 1 covered an overall group orientation, group rules, and group objectives. Depressive mood was addressed during Sessions 2–5. A technique of behavioral activation was presented, followed by the cognitive techniques of thought monitoring and cognitive restructuring. Sessions 6 and 7 were allocated to addressing medication adherence. The beneficial effects of antiviral medication were delineated and its complications and relevant obstacles identified, together with problem-solving tools. The last session was dedicated to summarization and to focus on relapse prevention. Art was applied within the CBGT activities as the means of making abstract thoughts more tangible. In addition, it was used to help demonstrate changes that might occur in clients after cognitive restructuring (e.g., drawing negative thought vs. new flexible thoughts), which can be more productive than using words (Rubin 2005). As well, in problem-solving, art was seen as a way of conceptualizing adherence for HIV people.
Instruments
Two instruments were administered in the current study. They were: 1) The Center for Epidemiologic Studies-Depression Scale (CES-D-10; Radloff 1977) and 2) the Visual Analog Scale (VAS; Gift 1989), which was used for medication adherence. With its visual analog nature, the VAS did not require any translation. The CES-D-10 was translated using Brislin’s back-translation procedure (1970). Then, the Index of Item Objective Congruence (IOC; Rovinelli and Hambleton 1976) was then calculated to assess its content validity. The outcomes showed that the CES-D-10 received a satisfactory index score.
Then, the CES-D-10 was piloted among 102 HIV-infected Thai individuals. The pilot outcomes were satisfactory, both in terms of its internal consistency (i.e., Cronbach’s alpha) and discriminant validity. For the latter, each CES-D-10 item score for individuals with overall scores higher than the 73th percentile was significantly different from the item scores of those with scores lower than the 27th percentile. For the VAS, whereas the aforementioned reliability and validity analyses were not applicable, its concurrent validity was assessed and supported by its positive correlation with another HIV adherence measure, the Morisky Medication Adherence Scale (MMAS; Morisky et al. 1986). Information about the two measures administered is as follows:
Depressive symptoms were measured using the CES-D-10 originally developed by Radloff (1977). Participants reported the frequency with which they experienced depressive psychological and behavioral symptoms in the previous week that are described in 10 statements, using a four-point scale (e.g., “I felt that everything I did was an effort,”). Item scores range from 0 (Rarely or None of the time) to 3 (All of the time). After relevant scoring reversal, the total CES-D-10 score was calculated, with the score for each item summed and averaged. A higher CES-D-10 score indicates higher depressive symptoms, whereas a lower score indicates lower depressive symptoms (sample α = .81, high internal consistency and αpre = .76, αpost =.79).
Antiretroviral medication adherence was assessed by the VAS, initially used in HIV contexts by Walsh et al. (1998). Participants rated the extent to which they agreed with responses to a question (e.g., “How much of your prescribed HIV medication have you taken in 1 month?) on a 10-point scale, across a continuum ranging from 0 (Taken no medication) to 10 (Taken every single dose of medication). Participants then responded to two additional questions: “How accurately have you taken your prescribed HIV medication on time?”, scored from 0 (Taken medication completely late) to 10 (Taken medication on time), and “How is your attitude toward taking medication?”, ranging from gradients of negative to positive attitudes. The total VAS score was calculated, with the score for each item summed and then averaged. A higher VAS score indicates higher medication adherence, whereas lower scores indicate lower adherence (r = .63, p < .01 and αpre = .76, αpost =.80).
Statistical Analysis
SPSS for Windows (version 15) was used for data analysis. Repeated measures multivariate analysis of variance (repeated measures MANOVA) and between-group MANOVA were performed to examine changes in depressive symptoms and antiretroviral medication adherence scores pre- and post-treatment, and to compare these scores between the control and treatment groups.
Results
A between-groups MANOVA was first conducted prior to the intervention period to confirm that scores for depressive symptoms and medication adherence were not different between the treatment and control groups. Results showed no statistically significant differences in either study variable: V = .068, F(2,43) = 1.56, p = .222. At pre-treatment time, the average score for depressive symptoms in the treatment group was 9.48 (SD = 5.24), which was not significantly different from that of the control group (M = 10.52, SD = 4.41): F(1,44) = .534, p = .469 (see Table 2). As for antiretroviral medication adherence, the scores at pre-treatment time were 26.57 (SD = 3.96) for the treatment group and 27.65 (SD = 2.92) for the control group members (see Table 3), with these showing no significant difference: F(1,44) = 1.121, p = .296. The post-test scores of the CES-D-10 and the VAS were then used in the subsequent statistical analysis, where a repeated-measure MANOVA was engaged to investigate for an interactional effect and for the pre- and post-score differences of the CES-D-10 and the VAS.
Repeated measures MANOVA were then conducted to examine the multivariate interaction effect for the two study variables (depressive symptoms and medication adherence). A significant multivariate interaction effect was found: V = .194, F(2,43) = 5.161, p < .05, f = .49. Subsequent univariate analyses revealed an interaction effect of the group*time condition for both depressive symptoms (F(1,44) = 7.046, p < .05) and antiretroviral medication adherence (F(1,44) = 5.405, p < .05), as illustrated in Figs. 1 and 2. This suggests that depressive symptoms scores were more drastically reduced in the CBGT group, but were slightly increased in the control group, and adherence scores in the CBGT group appeared to be increased, whereas a decreased trend was observed in control group scores.
To examine the sources of an interaction effect for each study variable (Figs. 1 and 2), paired t-test and independent t-tests were conducted to examine changes in scores pre- and post-treatment for each group, and to compare post-treatment scores between the treatment and control groups. For depressive symptoms, scores were significantly lower post-treatment within the intervention group: t(22) = 2.89, p < .01. This decrease was not observed in the control group: t(22) = .78, p = .221. In comparison, post-treatment depressive symptom scores in the intervention group were also significantly lower than those in the control group: t(44) = 3.85, p < .001.
In terms of antiretroviral medication adherence, a significant increase was observed post-treatment in the treatment group: t(22) = 2.39, p < .025 (M pre- = 26.57, SD pre- = 3.96 vs. M post- = 28.48, SD post- = 2.09). No such increase was observed in the control group: t(22) = .988, p = .33. However, in comparison, post-treatment antiretroviral medication adherence scores were not statistically different between the groups: t(44) = 1.44, p = .079.
Discussion
The current study aimed to assess the efficacy of cognitive-behavioural group sessions using art as a medium, in treating depressive symptoms and increasing antiretroviral medication adherence in a Thai population of MSM diagnosed with HIV. Whereas additional studies are required to clarify the efficacy of art-based CBGT in enhancing medication adherence, the current findings reiterate the potential usefulness of art-based CBGT in reducing depressive symptoms in MSM, consistent with previous empirical evidence (Himelhoch et al. 2007; Spies et al. 2013).
Based on past reports (Jacobson et al. 2001), two elements from the current CGBT-A intervention were regarded as key in helping to alleviate depressive symptoms. The first is behavioral techniques, particularly Behavioral Activation (BA). BA was selected based on empirical evidence that depressive mood leads individuals to reduce engagement in daily routines. Such reduction leads individuals with depressive mood to become socially isolated, have reduced levels of positive mood and have low medication adherence (Rabkin 2008). Behavioral Activation, which has been a key fundamental component of CBT, has been proven to enhance positive feelings of self-worth (Hopko et al. 2015). The MSM people chose BA activities based on their lifestyles such as walking, shopping, singing or doing household chores, etc., which report changes in not only mood but also physical conditioning. Physical symptoms commonly accompanying depressive mood, such as sleeping difficulties, can be alleviated with increased daily activities (Kingdon and Dimech 2008). Consequently, positive changes in the behavioral domain are also fundamental for subsequent changes in emotional and physical changes.
More importantly, positive attitude assists in subsequent cognitive restructuring, the second therapeutic component. As a result, participants become equipped with a broad array of cognitive strategies. Psychoeducation was conducted to assist participants to learn about the role of cognition in their emotions and behaviors. Participants also learned to monitor their thoughts and search for negative ones, such as the unfairness of job placement, the inability to find a long-term relationship or the stigmatization of being HIV infected. Then, they practiced evaluating and adjusting thoughts that contribute to depressive mood in the group, in dyads, and individually (Hopko et al. 2015).
Particularly in this latter component, art was used to increase the concreteness of participants’ thoughts, (Malchiodi 2005), An example of this is shown in Fig. 3. This participant left his home because of his disease, but when he returned his mother had passed away. His guilt feelings, self-blame, and negative thoughts are portrayed in Fig. 3 with the crying face and black coloring. Going through a cognitive restructuring process in the group activated alternative thoughts that he could not turn back time, but he had faith in his God and he could live his life helping other people who suffer from this disease. It gradually lessened his negative feelings and, hence, his drawing on the right of the Figure shows a smiling face with a cross at the forehead (in bright red color in the original drawing). Both behavioral and cognitive strategies were then integrated during relapse prevention sessions, where strategies to assist participants in combating depression in the future were presented.
While not as dramatic as the findings regarding depressive mood alleviation, the present findings do offer an initial indication of the potential effectiveness of CBGT-A in enhancing antiretroviral medication adherence among HIV-infected MSM in Thailand. Issues in regard to medical adherence could be as a result of retroviral side-effects, long-term medication intake, and concerns about being seen by others taking their medication (Safren et al. 2009). CGBT helps individuals to view these challenges within the context of the benefits of medication, to strengthen their adherence. Again, art was used to increase the clarity of the various abstract concepts introduced (Rosum and Malchiodi 2003) during evaluation of the drawbacks and benefits of antiretroviral medication, as shown in Fig. 4. The disadvantage of taking the medication, which participants often experience, such as retroviral side-effects and boredom of long-term intake, is shown in the left side of the Figure. It illustrates a desperate man facing down in front of a black wall that blocked his path to overcome the obstacles of antiretroviral medication. The right side image (the picture was colored vividly in the original), represents an awareness of the beneficial value of taking medication. It highlights food and water that is necessary in helping the flowers to bloom and grow.
In addition to cognitive strategies (i.e., cognitive restructuring), problem-solving was engaged in, which involved elements of behavioral strategies (D’Zurilla and Nezu 2010). Hence, in addition to assisting participants to change their views regarding their medication, behavioral skills were practiced in regard to the consumption of medication in public, handling the curiosity of acquaintances, etc., with this involving role-playing and assertiveness training. The HIV participants were help to recognize that they could manage their medical routine and how to respond whenever they were asked about their medication.
Contributions and Implications
Findings from the current study provide initial empirical evidence for the effectiveness of CBGT-A in alleviating depressive symptoms and enhancing antiretroviral medication adherence among MSM with HIV infection in Thailand. The mechanisms for these changes have been previously outlined. Whereas additional supporting evidence is required, the current program is seen as a promising means to provide psychological intervention for MSM with HIV infection within HIV supportive organizations. Possible adaption of the program in other groups of individuals infected with HIV (e.g., HIV-positive mothers or migrant workers) who do not receive support from non-governmental organizations should be considered, since some contextual disparities could be found among these individuals. Additionally, the current study findings attest to the benefits of using art as a medium in CBT and could pave the way for such usage in similar contexts.
Limitations and Future Directions
Despite these benefits, the current findings should be viewed in consideration of the study’s limitations. Akin to other intervention studies (Robatmili et al. 2015) where a non-intervention control group was employed, it is impossible to totally rule out the possibility that changes observed might result from the study group dynamic, rather than resulting from the outlined treatment component. Moreover, as the study was conducted with MSM people living with HIV who had contacted and received care and support from supportive organizations in Bangkok and vicinity, it may not be applicable to other groups of HIV infected individuals who have not obtained access to similar care and support.
As with other studies using self-report measures, use of these instruments present potential limitations. Despite assurance of response anonymity, responses that reflect concern about stigma cannot be completely ignored. Alternative methods of data collection, particularly for measurement of adherence, should help address this concern. Additionally, whereas participants in the current study reported experiencing depressive mood symptoms, this remained at sub-clinical levels. Extending the program for use with clinically depressed populations would further test its efficacy and, hopefully, help enhance the benefits of CBGT-A in supporting MSM with HIV infection in Asia and other countries where emotional expression of HIV-related issues are sensitive and severely limited.
References
Ammassari, A., Trotta, M. P., Murri, R., Castelli, F., Narciso, P., Noto, P., ... Antinori, A. (2002). Correlates and predictors of adherence to highly active antiretroviral therapy: overview of published literature. JAIDS Journal of Acquired Immune Deficiency Syndromes, 31, S123-S127.
Antiretroviral Therapy Cohort Collaboration. (2017). Survival of HIV-positive patients starting antiretroviral therapy between 1996 and 2013: A collaborative analysis of cohort studies. The Lancet HIV, 4(8), e349-e356.
Beck, A. T. (2005). The current state of cognitive therapy: a 40-year retrospective. Archives of General Psychiatry, 62(9), 953–959.
Berger, B. E., Ferrans, C. E., & Lashley, F. R. (2001). Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Research in Nursing & Health, 24(6), 518–529.
Beyrer, C., Baral, S. D., Van Griensven, F., Goodreau, S. M., Chariyalertsak, S., Wirtz, A. L., & Brookmeyer, R. (2012). Global epidemiology of HIV infection in men who have sex with men. The Lancet, 380(9839), 367–377.
Brislin, R. W. (1970). Back-translation for cross-cultural research. Journal of Cross-Cultural Psychology, 1(3), 185–216.
Bureau of AIDS, TB and STIs. (2013). Getting to zero. Retrieved December 1, 2013 from www.aidsstithai.org/contents/download/579.
Butler, A. C., Chapman, J. E., Forman, E. M., & Beck, A. T. (2006). The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clinical Psychology Review, 26(1), 17–31.
Chan, I., Kong, P., Leung, P., Au, A., Li, P., Chung, R., ... Yu, P. (2005). Cognitive-behavioral group program for Chinese heterosexual HIV-infected men in Hong Kong. Patient Education and Counseling, 56 (1), 78–84.
Ciesla, J. A., & Roberts, J. E. (2001). Meta-analysis of the relationship between HIV infection and risk for depressive disorders. American Journal of Psychiatry, 158(5), 725–730.
Corey, G. (2009). Cognitive behavior therapy (8th ed.). Belmont: Thomson Brooks/Cole.
Crepaz, N., Passin, W. F., Herbst, J. H., Rama, S. M., Malow, R. M., Purcell, D. W., & Wolitski, R. J. (2008). Meta-analysis of cognitive-behavioral interventions on HIV-positive persons’ mental health and immune functioning. Health Psychology, 27(1), 4–14.
D’Zurilla, T. J., & Nezu, A. M. (2010). Problem-solving therapy. Handbook of Cognitive-Behavioral Therapies, 3, 197–225.
Evans, D. L., Ten Have, T. R., Douglas, S. D., Gettes, D. R., Morrison, M., Chiappini, M. S., ... Wang, Y. L. (2002). Association of depression with viral load, CD8 T lymphocytes, and natural killer cells in women with HIV infection. American Journal of Psychiatry, 159(10), 1752–1759.
Gift, A. G. (1989). Visual analogue scales: Measurement of subjective phenomena. Nursing Research, 38(5), 286-288.
Gladding, S. T., & Newsome, D. W. (2003). Art in counseling. In C. A. Malchiodi (Ed.), Handbook of art therapy (pp. 72–81). New York: Guiford Press.
Himelhoch, S., Medoff, D. R., & Oyeniyi, G. (2007). Efficacy of group psychotherapy to reduce depressive symptoms among HIV-infected individuals: a systematic review and meta-analysis. AIDS Patient Care and STDs, 21(10), 732–739.
Hopko, D. R., Ryba, M. M., McIndoo, C., & File, A. (2015). Behavioral activation. In A. M. Nezu & C. M. Nezu (Eds.), The Oxford handbook of cognitive and behavioral therapies. New York: Oxford University Press.
Jacobson, N. S., Martell, C. R., & Dimidjian, S. (2001). Behavioral activation treatment for depression: Returning to contextual roots. Clinical Psychology: Science and Practice, 8(3), 255–270.
Kingdon, D., & Dimech, A. (2008). Cognitive and behavioural therapies: the state of the art. Psychiatry, 7(5), 217–220.
Leibowitz-Levy, S. (2005). The role of brief–term interventions with South African child trauma survivors. Journal of Psychology in Africa, 15(2), 155–163.
Malchiodi, C. A. (2003). Handbook of art therapy. New York: Guiford Press.
Malchiodi, C. A. (2005). Expressive therapies. New York: Guiford Press.
Morisky, D. E., Green, L. W., & Levine, D. M. (1986). Concurrent and predictive validity of a self-reported measure of medication adherence. Medical Care, 24(1), 67–74.
National AIDS Trust. (2003). Fact sheet 4.1 HIV/AIDS stigma and discrimination: Gay men. Retrieved November 1, 2014, from www.nat.org.uk/HIV-Facts.aspx. Accessed 1 Dec 2013.
Rabkin, J. G. (2008). HIV and depression: 2008 review and update. Current HIV/AIDS Reports, 5(4), 163–171.
Radloff, L. S. (1977). The CES-D scale a self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401.
Robatmili, S., Sohrabi, F., Shahrak, M. A., Talepasand, S., Nokani, M., & Hasani, M. (2015). The effect of group logotherapy on meaning in life and depression levels of Iranian students. International Journal for the Advancement of Counselling, 37(1), 54–62.
Roghanchi, M., Mohamad, A. R., Mey, S. C., Momeni, K. M., & Golmohamadian, M. (2013). The effect of integrating rational emotive behavior therapy and art therapy on self-esteem and resilience. The Arts in Psychotherapy, 40(2), 179–184.
Rosum, A. L., & Malchiodi, C. A. (2003). Cognitive-behavioral approaches. In C. A. Malchiodi (Ed.), Handbook of art therapy (pp. 72–81). New York: Guilford Press.
Rovinelli, R. J., & Hambleton, R. K. (1976). On the use of content specialists in the assessment of criterion-referenced test item validity. Laboratory of Psychometric and Evaluation Research Report No. 24.
Rubin, J. A. (2005). Artful therapy. Hoboken, NJ: John Wiley & Sons.
Safren, S. A., Otto, M. W., Worth, J. L., Salomon, E., Johnson, W., Mayer, K., & Boswell, S. (2001). Two strategies to increase adherence to HIV antiretroviral medication: life-steps and medication monitoring. Behaviour Research and Therapy, 39(10), 1151–1162.
Safren, S. A., O'Cleirigh, C., Tan, J. Y., Raminani, S. R., Reilly, L. C., Otto, M. W., & Mayer, K. H. (2009). A randomized controlled trial of cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected individuals. Health Psychology, 28(1), 1–10.
Spies, G., Asmal, L., & Seedat, S. (2013). Cognitive-behavioural interventions for mood and anxiety disorders in HIV: a systematic review. Journal of Affective Disorders, 150(2), 171–180.
Walsh, J. C., Dalton, M., & Gazzard, B. G. (1998). Adherence to combination antiretroviral therapy assessed by anonymous patient self-report. Aids, 12(17), 2361–2363.
Williams, M. M., Foo, K. H., & Haarhoff, B. A. (2006). Cultural considerations in using cognitive behaviour therapy with Chinese people: a case study of an elderly Chinese woman with generalised anxiety disorder. New Zealand Journal of Psychology, 35(3), 153–162.
Zimpel, R. R., & Fleck, M. P. (2014). Depression as a major impact on the quality of life of HIV-positive Brazilians. Psychology, Health & Medicine, 19(1), 47–58.
Acknowledgments
We thank Analisa Avila, ELS, of Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This research project was approved by the review committee at the Faculty of Psychology, Chulalongkorn University, and conforms to the provision of the Declaration of the Helsinki whereby informed consent for study participation was obtained and participant anonymity was preserved.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sahassanon, P., Pisitsungkagarn, K. & Taephant, N. The Effect of Cognitive-Behavioral Group Therapy Using Art as a Medium on Depressive Symptoms and HIV Antiretroviral Medication Adherence. Int J Adv Counselling 41, 530–543 (2019). https://doi.org/10.1007/s10447-019-09377-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10447-019-09377-7