Abstract
Human adult mesenchymal stem or stromal cells (h-MSC) therapy has gained considerable attention due to the potential to treat or cure diseases given their immunosuppressive properties and tissue regeneration capabilities. Researchers have explored diverse strategies to promote high h-MSC production without losing functional characteristics or properties. Physical stimulus including stiffness, geometry, and topography, chemical stimulus, like varying the surface chemistry, and biochemical stimuli such as cytokines, hormones, small molecules, and herbal extracts have been studied but have yet to be translated to industrial manufacturing practice. In this review, we describe the role of those stimuli on h-MSC manufacturing, and how these stimuli positively promote h-MSC properties, impacting the cell manufacturing field for cell-based therapies. In addition, we discuss other process considerations such as bioreactor design, good manufacturing practice, and the importance of the cell donor and ethics factors for manufacturing potent h-MSC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The demand for human adult mesenchymal stem or stromal cells (h-MSC) has increased in the past 20 years.91 The tissue regenerative capacity and immunosuppressive potential94 along with the self-renewing and clonogenic characteristics make them uniquely suited for a myriad of clinical applications and cell-based therapies.30,40,57,59 h-MSC have the ability to differentiate into 3 main lineages: adipocytes, osteoblasts, and chondroblasts.1 h-MSC therapies have been proposed as treatment for Alzheimer’s disease using 174 million cells per patient (M-Cells/P), amyotrophic lateral sclerosis (126 M-cells/p), orthopedic diseases (bone and cartilage)(101 M-cells/p), cancer (132 M-cells/p), cardiovascular disease (120 M-cells/p), Crohn’s disease (1508 M-cells/p), diabetes (375 M-cells/p), erectile dysfunction (15 M-cells/p), graft vs. host disease (578 M-cells/p), hematological disease (192 M-cells/p), kidney disease (261 M-cells/p), liver disease (420 M-cells/p), lung disease (451 M-cells/p), lupus (70 M-cells/p), multiple sclerosis (190 M-cells/p), Parkinson’s disease (168 M-cells/p), psoriasis (420 M-cells/p), and spinal cord injury (109 M-cells/p).91
In the year 2000, the consumption of h-MSC for clinical and academic/preclinical work was about 1 × 1011 total cells. Recent reports have shown higher consumption values up to 7 × 1012 total cells, which indicate an exponential increase in the coming years.91 Jon A. Rowley and colleagues have indicated that by 2040 the h-MSC consumption will be focused on five applications:
-
(1)
Therapeutic products with a demand of at least 300 trillion cells;
-
(2)
Tissue engineering with 33,600 transplants and 185,000 limb amputations per year in the USA (278 trillion cells only for bone tissue engineering);
-
(3)
Products derived from h-MSC like raw materials for clinical trials, extracellular vesicles, protein/cytokine production (300 trillion cells);
-
(4)
Systems and synthetic biology where h-MSC will be used in gene silencing, potency, targeting, molecular engineering, and biodistribution;
-
(5)
And Emerging industries, like cosmeceuticals and engineered biomaterials.91
Therefore, the demand for h-MSC could become a big problem if the cell manufacturing field cannot accommodate the production line to supply future needs. Given the high number of patients and the millions of cells per patient required, it is necessary to explore ways in which processes can improve to meet the demand. Expansion methods and technologies employed in the cell manufacturing process, like planar and 3D bioreactors, have been essential to produce higher amounts of h-MSC. However, such methods still fall short to meet the high demand for cells with the expected potency. Thus, there is room to explore new strategies that enhance and support the manufacture chain process to obtain not only large quantities but also high potency in the final cell-based product.
This review, as illustrated in Fig. 1, describes the role of different stimuli on h-MSC behavior for more efficient manufacturing processes by increasing productivity and retaining desired properties of h-MSC will positively impact cell-based therapies. The effect of surface chemistry and physical stimulus in cultures including the type of culture substrates, substrate stiffness, and other aspects of geometry and topography of materials on h-MSC expansion and potency are discussed within the cell manufacturing perspective. Also, the influence of culture parameters and biochemical stimuli such as cytokines, hormones, small molecules, and herbal extracts are discussed as potential strategies to promote cell growth, the reduction in consumption of culture components derived from animal sources, and the refinement of potent immunosuppressive properties expressed in manufactured h-MSC. Finally, ethics factors, sustainable banks for the future, issues, and challenges of good manufacturing practices are briefly discussed.
Response to Physical, Chemical, and Biological Stimuli
Culture Substrates
h-MSC respond to physical and chemical signals presented by the local microenvironment, such as surface chemistry, substrate stiffness, topography, and 3D materials including nanofibers or hydrogels.30,40,79,81 Culture substrates composed of either synthetic or natural polymers together with biophysical cues are a promising strategy for supporting and enhancing the cell manufacturing process. In recent years, natural and synthetic biomaterials have been created, which are capable of mimicking the native extracellular matrix (ECM) through cell organization, mechanical forces, and bioactive molecule delivery.47,115 Interactions with different physical cues require a broad understanding of how h-MSC could be affected by the phenomena mentioned above. For example, mechanical properties of substrates, such as stiffness and elasticity, modulate the behavior of h-MSC during culture and those effects persisted after several rounds of cell expansion.72 This “mechanical memory” state will likely impact cell safety and potency in tissues.42,46 In the next sections, we summarize recent advances and limitations of culture substrates for cell manufacturing applications.
Tissue Culture-Treated Plastic (TCP)
Cell isolation and expansion processes are performed on traditional tissue culture-treated plastic (TCP). TCP has been the preferred choice for cell culture due to its excellent cell adhesive properties, optical transparency, and biocompatibility. Although for most cells high-fold cell expansion is facilitated, TCP substrates have a stiffness and are incapable of supporting matrix-mediated signaling. Several studies have shown that when h-MSC are cultured for extended times on TCP they lose their proliferative capacity and multi-lineage differentiation potential.3,13,47,71,81,94,135 Moreover, after several passages, h-MSC enter into a “senescence” state, which leads to permanent cell cycle arrest. Work by Yang and colleagues shows that h-MSC can develop mechanical memory if expanded on TCP, meaning that cells can store past signals of a culture microenvironment. This behavior was monitored through the activation (nucleus location) or deactivation (cytoplasmic location) of the transcriptional coactivator YAP/TAZ and RUNX2 genes on TCP and soft hydrogels, which affected cell potency after in vivo transplantation.71,135 In addition to transcriptional activity, changes in cell behavior can also be perceived by the loss of the elongated morphology and the appearance of abundant large and flat cell clusters in a culture, both indicators of cell differentiation. For example, Dolley and collaborators studied the expansion of human bone marrow MSCs (h-BMMSC) cultured using a serum-free defined medium on Corning Synthemax surface, TCP, and ECM coatings and compared it to standard culture conditions supplemented with serum.31 Their findings showed that cells seeded in Corning Synthemax surface and ECM coatings presented similar cumulative cell number for all sixty days of testing.31 Both surfaces with serum-free medium reported a production of approximately 1 × 1014 cells in sixty days. However, TCP with serum only yielded 1 × 109 cells in the same time period. Additionally, cells maintained the normal elongated and spindle-like morphology on the different substrates except on TCP. Such changes in cell behavior associated with the use of TCP as the main culture surface limits its continued use in the propagation of h-MSC and has been the main motivation for the engineering of culture substrates. Potential alternative substrates for h-MSC cultures are summarized in the next sections and are grouped based on the physical properties examined.
Stiffness
Mechanical properties impact h-MSC proliferation, maintenance of phenotype, and differentiation.137,140 The stiffness of the culture substrate is one of the significant properties impacting the differentiation potential and phenotype of h-MSC. Stiffness is a measure of stretchability and rigidity of the materials16 and it is typically obtained from the slope of the linear region of the stress-strain curve, “Young’s modulus”, where stress and strain are representing strength and ductility, respectively.12 Cells can exert traction forces generated from cytoskeleton’s tension on the substrate due to its stiffness42 leading to the activation of mechano-transductive signaling that modulates cellular activities.36,93 Thus, the substrate stiffness influences the cell’s adhesion strength and surface spreading.136
The differentiation of h-MSC into different cell lineages is one of the main cellular functions impacted by substrates stiffness. For example, stiff surfaces induce osteogenesis, whereas softer substrates supports adipogenesis and decreases the proliferation rate.75 Therefore, it is vital to consider the mechanical properties of the substrates to avoid undesired changes in cell differentiation during the expansion process.36 Li’s team evaluated different ranges of stiffness to examine the impact on fibrotic cell behavior, which has a direct relationship with the preservation of stem cells characteristics.71 They found that surfaces of low stiffness (2–5 KPa), which fell in the range of those reported for soft tissues, inhibited fibrogenesis as compared to TCP (2 GPA). Moreover, substrates of high stiffness (50–100 kPa) induced cell fibrogenesis71,120 suggesting the potential of soft substrates to preserve the stem cells characteristics. Kureel and colleagues also examined the impact of stiffness in stemness and growth by measuring cell doubling times and differentiation potency in polyacrylamide-based substrates of variable stiffness. The cumulative doubling time of umbilical-cord and bone-marrow derived h-MSC seeded onto a polyacrylamide gel of Young’s modulus of 5 kPa showed an increase of nine times higher population doubling in comparison to h-MSC seeded on TCP. Also, the adipogenic differentiation potential was limited in TCP,65 further supporting the mechano-sensorial capability of h-MSC. Thus, soft substrates represent a good alternative to maintain the differentiation capability and enhanced growth rates; however, the stiffness of the culture substrate needs to be tailored early during the cell expansion process to meet the desired therapeutic application.
Fibrous Scaffolds
Scaffolds represent an ideal structure as a substrate for cell growth, mimicking their environment. Several scaffolds have been created with a fibrous or flat organization, where the mechanical properties in combination with changes in surface morphology/chemistry provide a set of biophysical cues to guide cell behavior through cell-material interactions.119 Fibrous substrates are typically fabricated by phase separation, melt spinning, self-assembly, twisting, braiding, knitting and electrospinning methods.110 Electrospinning is a promising technique where ultrafine fibers are obtained by electrically charging a polymer solution droplet.70 This technique enables the generation of fibrous substrates and controls over the physical parameters including fiber diameter, density, and anisotropy, to generate substrates that mimic the natural fibrous structure and architecture of the native extracellular matrix.6,109,119 Fibrous substrates have been shown to modulate important cellular processes such as cell growth and migration, but little is known about how fibrous substrate could help in the expansion and manufacturing process of h-MSC, since many of the studies have been made with non-human cells. Li and colleagues reported using PLGA electrospun fibers to observe if h-BMMSC had good interactions with the engineered microenvironment. They reported that cells seeded onto electrospun fibers maintain their phenotype, have good adhesion and proliferation, and had a fivefold increment in the total cell number by day ten.70 Similar results were reported by Baker and co-workers using synthetic fibrous material and hydrogels with different stiffness levels composed of methacrylated dextran. Cell proliferation of h-MSC on the stiff hydrogel substrates resulted in a 15% higher return than h-MSC seeded on soft hydrogels, while the soft fibers showed a 10% increase over h-MSC on stiff fibers networks.6 Thus, the alterations observed in the behavior of h-MSC as a consequence of the fibrous or flat state of the substrate indicate that the structure of the material is also an important property to consider in the design of culture substrates for cell manufacture applications.
Topography
Physical cues of the cellular microenvironment are considered important factors in cell function. These cues directly affect the cells mechano-sensitivity due to the cell-substrate interactions. The substrate topography, including geometry, is based on surface modifications with different shapes to generate mechanical stress in the cells, therefore affecting cell behavior.52 Research performed by Lee J and colleagues showed that geometric cues (different shape and size) on hydrazine-modified polyacrylamide (PA) hydrogels are more favorable to the activation of stemness markers. They evaluated the role of substrate stiffness, such as 0.5 KPa (soft) and 30 KPa (stiff), combined with different geometries, i.e., circle, oval and star, on the maintenance of the h-MSC phenotype. They concluded that soft substrates and micro-patterns can regulate the spreading and cytoskeletal tension, enhancing the expression of h-MSC multipotency markers.69 On the other hand, Seunghan Oh and colleagues were interested in controlling the expansion of undifferentiated h-MSC, as well as regulating their differentiation using variation in surface geometry. They found that TiO2 nanotubes with a specific diameter of 30 nm promotes adhesion without differentiation and strongly enhances cellular activities compared to smooth TiO2 surfaces; however, larger diameters between 70 and 100 nm induce selective differentiation to osteoblast. Therefore, there is a way to enhance cell adhesion during cell expansion, controlling h-MSC fate.88 In addition to geometries, topographical characteristics are perceived by h-MSC and shown to influence behavior by altering gene expression patterns that directly impact cell growth, adhesion, and differentiation.69 McMurray and co-workers examined the impact of nanotopographies as an easy-to-use and easy-to-manufacture surface to maintain multipotent characteristics on bone marrow and adipose-derived h-MSC. They found that polycaprolactone (PCL)-based nanotopographies with 120 nm pits in a square arrangement with a center-center spacing of 300 nm were supportive of cell expansion for up to 8 weeks without losing stem-cell phenotype h-MSC.81 These findings suggest that both geometry and topography can be incorporated into culture surfaces to stimulate a desired phenotype of h-MSC. Additional studies, including a broader pool of h-MSC sources and mechanistic evaluation, are needed to determine its potential applicability to achieve reproducible alterations in the therapeutic potency of h-MSC.
Surface Chemistry
Surface chemistry modification has been studied as a potential option to retain h-MSC expansion without affecting functional characteristics. These modifications include the immobilization of polymers and small molecules on the surface through covalent bonding, electrostatic interaction, and hydrophobic bond methods. These alterations have demonstrated moderate cell adhesion and prevent undesired changes in the phenotype and potency of h-MSC.118,122
However, studies have reported issues about surface chemistry and the effect on h-MSC behavior. For instance, the instability of surface modifications is a significant problem. Cell adhesion is directly related to surface hydrophobicity due to the interaction with serum proteins.26 Curran and co-workers performed a comprehensive study of the impact of functional groups on h-BMMSC behavior. Main functional groups found in biological systems, including methyl (–CH3), hydroxyl (–OH), carboxyl (–COOH), amino (–NH2) and silane (–SH), were evaluated. Results showed that these modifications could enhance or commit the cell to a specific lineage. For example, the –NH2 and –SH-modified surfaces promoted and maintained osteogenesis while the –OH and –COOH-modified surfaces promoted and maintained chondrogenesis. Thus, functional groups can be used to complement traditional cell differentiation methods using culture media preparations to either reduce or replace the need for cytokines and growth factors.26,27,–28 Even though the functional chemistries showed good results for promoting cell differentiation, they are not appropriate for h-MSC expansion from a manufacturing standpoint because of the inability to maintain an undifferentiated state in the bulk population.
An alternative approach is to use polyelectrolyte multilayers to functionalized culture surfaces using natural polymers. Our research group has demonstrated that it is possible to create bioactive surfaces via the layer-by-layer assembly method to improve h-MSC activities and responses.15 Multilayers of heparin and collagen (HEP/COL) were used to prepare the bioactive surface onto TCP to enhance h-MSC response to soluble interferon gamma (IFN-gamma). Multilayers were formed varying the final layer between COL and HEP and supplemented with IFN-gamma (50 ng/mL) in the culture medium. Even though IFN-gamma is a cytokine associated with innate and adaptive immunity, combating viral infections, bacteria, and protozoa,51 it has an antiproliferative effect reported for many kinds of cells.10,15,73,130 The results showed that this polymeric system reduces the antiproliferative effect of IFN-gamma. HEP-ending films supplemented with IFN-gamma presented a better proliferative effect compared with COL-ending films and TCP (surface without HEP/COL multilayers). Furthermore, HEP-ending films supported the high expression of cytokines, including interleukin-6 (IL-6), vascular endothelial growth factor-A (VEGF-A), basic fibroblast growth factor (FGF-2), and colony stimulating factor 1 (M-CSF) as compared with the other conditions examined. Hence, this system may be beneficial in cell manufacturing practices because it was able to present a platform (HEP/COL multilayers + Cytokine/IFN-gamma) which enhanced immunomodulatory properties and therapeutic potential of h-MSC while eliminating the antiproliferative effect offered by IFN-gamma.15 The role of cytokines as a biochemical stimulus on h-MSC manufacturing is further discussed in the next section.
Biochemical Stimulus on h-MSC Manufacturing
Role of Cytokines
Cytokines have demonstrated their potential to stimulate changes in the behavior of human stromal cells, including the promotion of migration,117 proliferation or cell survival,25 differentiation,54 osteogenesis,48 enhancing and inhibiting chondrogenesis,132 neovascularization,37 mineralization,98 tissue repair,92 suppressing cellular senescence,53 immunosuppressive capacity,62 tumorigenesis and angiogenesis,90 along with other effects such as impairing maintenance and altering hematopoietic support.41 Consequently, several studies have demonstrated that cytokines are advantageous for cell manufacturing or h-MSC expansion.
Reduction in Consumption of Culture Components Derived from Animal Sources
Researchers who have used cytokines like IFN-gamma,117 FGF-2,41,107 VEGF-A,38 tumor necrosis factor alpha (TNF)-α,34 and granulocyte-macrophage colony stimulating factor (GM-CSF)95 have identified that their use is crucial for modulating several cellular activities of h-MSC, and their effect can be regulated by their concentration.38 A direct advantage of supplementing cytokines on cultures of h-MSCs is the reduction in consumption of culture components derived from animal sources such as fetal calf serum.17,107 One of the main issues of good manufacturing practices (GMP) in the cell manufacturing field is associated with the selection of the culture medium. The culture medium of choice is generally of a xeno-free source, as animal-derived products could potentially transmit unpredicted viruses or other pathogens.108 Hence, new media formulations on h-MSC expansion have been focused on utilizing non-animal derived products to avoid secondary effects or complications that can compromise cell production.8,64 Lucas G. Chase and colleagues achieved h-MSC expansion using a serum-free medium supplemented with transforming growth factor beta1 (TGF-β1), FGF-2, and recombinant human platelet-derived growth factor-BB (PDGF-BB).17 Results showed that PDGF-BB, FGF-2 individually supplemented, as well as combinations of two factors PDGF-BB/FGF-2, PDGF-BB/TGF-β1, and FGF-2/TGF-β1 enhanced cellular expansion compared with a growth factor-deficient serum-free medium (SFM) or 10% fetal bovine serum-containing medium (SCM). Although these combinations produced promising results, the combination of these three supplements together provided an enhancing effect on h-MSC proliferation showing phenotypic retention.17 Prior studies have also demonstrated that TGF-β1, FGF-2, and PDGF-BB are sufficient to support h-MSC growth in serum-free medium.60,87 Muller examined the proliferative effect of platelet lysate as a supplement, compared with media alone or supplemented with 5% serum-free media containing fresh frozen plasma (FFP) or 10% fetal calf serum (FCS) (standard condition).86 Several concentrations (1–100 Million-platelets/mL) of platelet lysate were evaluated in combination with 2.5% FFP. Results showed that media supplemented with 10% FCS duplicated the proliferative effect compared with media containing 5% FFP. However, platelet lysate supplemented in 2.5% FFP showed a significant advantage in cell proliferation. A concentration of 10 Million-platelets/mL added to 2.5% FFP demonstrated the same proliferative effect as that of h-MSC in 5% FFP. Concentrations of 50 and 100 Million-platelets/mL presented a similar effect compared with h-MSC in 10% FCS. Therefore, it is possible to say that platelet lysate promotes a positive effect on h-MSC proliferation, and additionally minimizes the use of fetal calf serum to maintain the cellular culture. These studies demonstrate how a combination of different cytokines could be useful to significantly reduce or eliminate the use of animal-derived products, while maintaining or enhancing h-MSC properties. The main limitation of current xeno-free media is its cost. Optimization of recombinant cytokine production, as well as the evaluation of multiple cytokine combinations could lead to xeno-free formulations of reduced costs. Also, it is imperative to evaluate substitutes for cytokines such as peptides or other small molecules that can be produced at lower costs.
Self-renewal of h-MSC and Retention of Multilineage Differentiation Ability
Another advantage of using cytokines for h-MSC manufacturing is associated with retention of the multilineage differentiation ability during the process of proliferation.125 Yukio Kato and his team worked on identifying a growth factor that was involved in the self-renewal of h-MSC and the preservation of multilineage differentiation potential.125 Their findings demonstrated that FGF-2, which is a potent mitogen for h-MSC, markedly improved the growth rate of bone-marrow-derived h-MSC in monolayer cultures and the multilineage differentiation ability of h-MSC was maintained throughout numerous mitotic divisions.125 Similarly, Sotiropoulou reported that FGF-2 induces an increase in the proliferation response of h-MSC. However, this cytokine generates an upregulation of human leukocyte antigen (HLA-class I) and promotes low human leukocyte antigen—DR isotype (HLA-DR) expression, which is involved in the regulation of the immune system in humans.114 Although their results showed upregulation of HLA, allogeneic immune responses were weak, compared with the responses provoked by allogeneic peripheral blood mononuclear cells (PBMCs), which consist of monocytes and lymphocytes (T cells, B cells, NK cells). On the other hand, the in vivo immunosuppressive ability of h-MSCs was enhanced when FGF-2 was added at concentrations above 5 ng/mL supporting the use of FGF-2 to stimulate the growth of h-MSCs for immunosuppressive applications. The mechanism of action was further investigated by Young Do Kwon and collaborators that examined the effect of the mitogen-activated protein kinase (MAPK) signaling pathway in the FGF-2 supplemented cultures. MAPKs are known as the main signal transducers for growth factors, cytokines, and stress. They also control cell proliferation and apoptosis.2 Results showed that Jun N-terminal kinase signaling is involved in the FGF-2 induced proliferation and preservation of the multilineage differentiation ability of h-MSC.2 Other cytokines of the same family, such as fibroblast growth factor receptor 1 (FGFR-1), have been demonstrated to induce proliferation, as well as control the maintenance of h-MSC viability.32 The proliferation effect has been shown by inhibiting the cyclin-dependent kinase inhibitors P21waf1 and P27kip.32 Although FGF-2 is known as a potent mediator of proliferation by itself, the effect of FGF-2 and other members of the FGF family should be examined in combination with either cytokine of the same family or other types of cytokines to explore improvements on h-MSC proliferation.
Other cytokines such as IL-1 beta have also demonstrated an ability to stimulate h-MSC proliferation. Alexey E. Bigildeev and his group investigated the effect of IL-1 beta on h-MSC.9 Specifically, they studied proliferative potential, immunomodulatory properties, and the ability to support early hematopoietic precursor cells of h-MSC cultured in standard conditions or treated with 4 pg/mL human recombinant IL-1 beta. Results showed that IL-1 beta promoted cell expansion and enhanced the potential to maintain a phenotype.9 Interleukin-17 (IL-17), which is a cytokine secreted by TH-17 cells,50 was used by Ki and collaborators to evaluate the effect of supplemented IL-17 at a concentration of 50 ng/mL on h-MSC for up to 8 days.50 Their results suggested that IL-17 promotes the growth of these cells as compared to cells without IL-17 supplementation. Their findings showed that after 2 days of culture, significant differences were observed. In addition, they revealed that the production of reactive oxygen species (ROS) is vital to favor h-MSC proliferation in the presence of IL-17. Accordingly, cytokines have demonstrated to be not only useful to minimize issues in GMP, such as reducing the use of animal-derived products, but also useful to stimulate h-MSC proliferation.
Improving Immunosuppressive Properties
Manufacturing processes are characterized by quality control of the specifications of their products. The quality criterion for the immunosuppressive properties of h-MSC is the cytokine profile and immunomodulatory function. h-MSC have the potential to treat immune-related diseases due to their immunosuppressive properties.62 The interaction of cytokines with h-MSC has positively impacted the cell manufacturing field of h-MSC by improving their intrinsic immunosuppressive properties. Many researchers have demonstrated that the supplementation of IFN-gamma on h-MSC cultures enhances the immunosuppressive properties of h-MSCs in different ways. For example, Keon Hee Yoo and collaborators revealed that IFN-gamma induces indoleamine-2,3-dioxygenase (IDO) expression, which is a crucial modulator in the immunosuppressive pathway in h-MSC, through the IFN-gamma-Janus kinase signal transducer and activator of transcription pathway.62 Therefore, their results provided a convenient and practical way of obtaining functionally qualified h-MSC, which can adequately control the immune response. In addition, their findings recommend that cell therapy based on h-MSC primed with IFN-gamma can be used for the clinical treatment of allogeneic conflicts. Similarly, studies by Todd C. McDevitt also has revealed that IFN-gamma plays a crucial role in stimulating h-MSC immunomodulatory activity.141 Their results showed the IFN-gamma induced expression of IDO, resulting in an augmented and continued suppression of T-cell activation and proliferation.141 This resulted when his team evaluated the microparticle delivery of IFN-gamma within h-MSC spheroids an evaluated their immunomodulatory activity. Consequently, McDevitt and his group concluded that this microparticle-mediated presentation of bioactive IFN-gamma offers a potent methodology to guarantee and maintain immunomodulation of h-MSC. Comparably, James A. Ankrum reported that IFN-gamma enhances IDO expression of cryopreserved h-MSC pretreated at a concentration of 100 ng/mL.14
Other groups also have suggested that h-MSC stimulated with IFN-gamma consistently enhance their immunosuppressive properties.63,101,102,128 Steven R. Bauer reported that immunosuppressive properties could be predicted by the morphological features of IFN-gamma stimulated h-MSC.63 Additionally, Gordana Vunjak-Novakovic reported the influence of IFN-gamma on the proteome and metabolome of therapeutic h-MSC.134 Results highlighted that IFN-gamma at a concentration of 500 U/m encouraged the expression of antipathogenic proteins as well as induced h-MSC to limit inflammation and fibrosis while helping h-MSC survival.134 Jacques Galipeau and his team demonstrated by secretome analysis that IFN-gamma activated h-MSCs has a similar genetic profile as h-MSCs activated in co-culture with PBMCs to increase their potency, and that this behavior is associated with T cell suppression.19
On the other hand, researchers such as S. Jyothi Prasanna and her team have reported that not only IFN-gamma but also TNF-α stimulates the immune properties of human bone marrow (h-BMMSC) and Wharton jelly mesenchymal stem cells (h-WJMSCs).96 Their discoveries reported that h-BMMSC improved suppression of mitogen motivated lymphoproliferation only while h-WJMSCs treated with IFN-gamma were exceptional suppressors of mixed-lymphocyte reactions. Moreover, h-WJMSCs presented a mayor yield than h-BMMSC under the presence of both pro-inflammatory cytokines treatments.96 Hence, it is possible to affirm that the interaction of both cytokines allows the control of the immunosuppressive properties of h-MSC. Likewise, Patrick T. Coate described that the enhancement of immunosuppressive properties of h-MSC could be generated under the influence of the proinflammatory cytokine interleukin-17A.112
The role of cytokines in h-MSC manufacturing is mainly related to the reduction in consumption of abundant culture supplements, enhancement of their proliferative potential, retention of their multilineage differentiation ability, and the enhancement of immunosuppressive properties of h-MSCs. Cytokines can be used to modulate several cellular activities of h-MSCs, and their effect can be regulated by their concentration. In addition, cytokines contribute to minimizing the use of culture components derived from animal sources, which lead to better GMP, offering a safer production. FGF-2 and IFN-gamma have amply been explored to modulate proliferation and immunosuppressive properties of h-MSC, respectively. Hence, it would be interesting to examine the response of these two cytokines working together as a supplement on h-MSC cultures. Another useful alternative would be to evaluate a cocktail composed of diverse cytokines to promote the production of robust h-MSC. The impact of cytokines on h-MSC culture has mostly been evaluated on a bench scale. Preliminary trials must be performed on a larger scale to assess the impact of scalability.
Other Biochemical Agents
Other soluble factors such as hormones,4,8,21,127,138 small molecules,4 and herbal extracts131 also have been linked to the proliferative potential of h-MSC. 17β-Estradiol (E2) is a steroid hormone characterized for its role in the modulation of numerous cell functions.138 Ho Jae Han et al studied the role of E2 on proliferation and the linked signaling pathways using h-MSC. They incubated h-MSC at a concentration of 10−9 M E2. Their findings showed that E2 increased the cell population by approximately 40% in the S phase compared with the control. Moreover, they conjectured that E2 induces proliferative activity via estrogen receptors (ERs) expression in h-MSC. Another hormone, insulin-like growth factor 1 (IGF-1), also has presented abilities to promote cell proliferation of h-MSC.21 An interesting finding was reported by Russell et al who explored the proliferative effect of IGF-1 using a concentration of 100 ng/mL. The results showed that IGF-1 polypeptide improved the proliferation of small cells (5–9 μm), but not cells with a size greater than 13 μm.21 On the other hand, small molecules like GSK3β inhibitor 6-bromoindirubin-3′-oxime (BIO) also has been employed to induce h-MSC proliferation in vitro.49 In this work, Benoit and collaborators evaluated concentrations of 0, 2, 5, and 10 µM of BIO. Their results showed that BIO concentrations in the range of 2–5 µM were the most promising for inducing a proliferative response of h-MSC. Anything above 5 µM resulted in cell death and below 2 µM did not have any significant effect.49 Herbal extracts such as Dhanwantharam Kashaya (DK), which is an artificial herbal preparation commonly used in Ayurvedic medicine,49,131 have been studied on the proliferation of h-MSC.20,126 Warrier and colleagues examined the capacity of DK on the proliferation, viability, and senescence of human Wharton jelly MSCs (h-WJMSCs) in vitro.131 In this study, they treated medium in the absence and presence of DK at a series of concentrations 5, 7.5, 10, 20, 40, and 50 µg/mL. The results showed that DK significantly improved the proliferation of cells, describing a dose-dependent behavior. The maximum effect obtained was at 10 µg/mL.131
Glucocorticoids, which are a class of steroid hormones involved in the metabolism of proteins, carbohydrates, and fats and have anti-inflammatory activity, have contributed positively to the immunomodulatory potency of h-MSC.4 Jeffrey M. Karp and his team reported that it is possible to enhance the performance of h-MSC via the intracellular delivery of steroids.4 Their findings demonstrated that glucocorticoid steroids increase h-MSC expression and activity of IDO. They described that h-MSC treated with glucocorticoids, budesonide, or dexamethasone have a supportive effect on improved IDO expression following IFN-gamma stimulation as well as the ability to restore IDO expression in over-passaged h-MSC. Another alternative that has been used to enhance the immunomodulatory capacity of h-MSC is linked to hypoxic pretreatment by improving the secretion of cytokines and soluble factors associated with immunosuppression response.103 J. Wang examined the effects of hypoxia on the immunomodulatory properties of human gingiva–derived MSCs (h-GMSCs). They found that hypoxia improves the immunomodulatory properties of h-GMSCs by stimulating the production of anti-inflammatory cytokines.55 Numerous other studies reported that hypoxia upregulated the expression of IDO in human adipose tissue-derived h-MSC.99
Many researchers worried about the potential risk of infections as well as immunological reactions that fetal calf serum (FCS) as a supplement may generate. For instance, Karen Bieback and her team investigated the effects of pooled human AB serum (AB-HS) and thrombin-activated platelet-rich plasma (t-PRP) vs. FCS as the standard control medium.64 This study was performed using three separate conditions: 10% FCS, 10% AB-HS, and 10% t-PRP. Results demonstrated that 10% AB-HS and 10% t-PRP offer a significantly robust proliferative effect on h-MSC than FCS does. h-MSC cultured using AB-HS and t-PRP exhibited a 3 times higher expansion compared to cultures with FCS after the first six passages.64
In summary, physical, chemical, and biochemical stimuli are crucial during the production of h-MSCs. One of the most important contributions of biochemical stimulus has been the focus on reducing essential culture components derived from animal sources, which is crucial to eliminate the potential risk of infections that these sources may offer. On the other hand, even though a range of biochemical stimuli have been studied, mainly in an individual manner, showing exceptional results on cell expansion, it is imperative to study further and evaluate the effect of preparing cocktails using combinations of these stimuli. A combination of cytokines or other soluble factors, such as hormones, small molecules, and herbal extracts could be used to create a supportive and robust supplement for fast h-MSC production.
Scaling h-MSC Manufacturing: Strategies to Stimulate Proliferation
The increasing clinical demand for h-MSC requires robust, large-scale production strategies.91 To extensively manufacture cells, two different cell culture systems have been identified: planar or monolayer culture system and the 3D system for h-MSC expansion. Planar systems include T-flasks and multi-layered flasks. 3D systems comprise various bioreactors (wave stirred tank, rotating wall vessel, packed-bed, roller bottle) and microcarrier-based culture systems.59,121 The type of bioreactor has played a significant role in the scaling of h-MSC manufacturing, where their difference in size, geometric design, operational parameters, and the material of fabrication impact cell production. Likewise, cell culture conditions in bioreactors also exert a significant effect on scaling h-MSC manufacturing. In this section, the impact of scaling in h-MSC manufacturing in response to cell culture conditions, and operational parameters of bioreactors will be described.
Influence of Cell Culture Conditions in Bioreactors
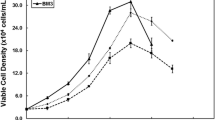
Multiple systems strategies and technologies geared towards maximizing cell culture expansion have been explored. Strategies include the evaluation of culture parameters such as different types of culture medium, serum, pH, glucose concentration, agitation rate, and dissolved oxygen (dO2) concentration.18,35,45,56,66 The impact of bioreactor design and flow conditions or shear stress as a biomechanical parameter in regulating h-MSC proliferation has also been explored.58,85,139 For example, different types of microcarriers with the main goal of obtaining which one might be more useful to improve proliferation have been investigated.33,61 Similarly, other teams have studied the effect of microcarrier concentration.18,56,106 Tristan Lawson and colleagues used a 50 L single-use stirred tank bioreactor to examine the influence of various culture parameters on the proliferation respond.66 First, they identified the optimal pH and dO2 culture set-points. Four distinct pH levels (7.2, 7.4, 7.6, and 7.8) and three dO2 concentrations (20, 50, and 80%) of air saturation were evaluated in cell cultures for 10 days. Results of a single cell donor showed that a pH between 7.4 and 7.6 provided optimal proliferation. A total of 5 × 108 cells were obtained using pH between 7.4 and 7.6 vs. 4 × 108 cells at pH 7.2 and 2 × 108 cells at pH 7.8 for 10 days of culture in 3 L bioreactor cultures. Although dO2 concentrations showed similar growth rates, 80% dO2 was selected to examine the other parameters. Two culture mediums in combination with two types of serums were examined as follows: minimum essential medium-α-based medium (αMEM) or Dulbecco’s modified eagle’s medium (DMEM) with 5% human platelet lysate (h-PL) and αMEM and DMEM supplemented with 10% FBS. Their findings indicate that using αMEM/h-PL a higher cell growth was achieved compared to the other conditions.66
Similarly, Christopher J. Hewitt reported that h-PL containing medium increased the h-MSC growth rate 20% more compared with the FBS supplemented, and this enhanced proliferation rate was consistent across all donors examined.45 In other studies, αMEM has been supported as the preferred media for h-MSC. Allen Kuan-Liang Chen reported that αMEM supported faster h-MSC growth than DMEM, additionally a low glucose concentration (1–1.5 g/mL) was a more favorable condition in which to obtain improved h-MSC growth yield.18 Glucose concentrations between 1 and 1.5 g/mL presented similar cell concentrations of 4.6 × 104 cells/cm2. Higher glucose concentrations of 2 and 2.5 g/L yielded lower cell concentrations of 2 × 104 cells/cm2 and 2.5 × 104 cells/cm2, respectively. Lawson and colleagues used these optimum conditions and monitored h-MSC expansion in a 50 L bioreactor. Results showed that using αMEM/h-PL or DMEM/FBS working at optimum conditions made it possible to achieve between 1 and 1.25 × 1010 cells in 11 days, representing a significantly greater difference in growth compared to the un-optimized conditions, which produced 4 × 109 cells in 11 days. In other words, the optimized conditions increased h-MSC production 2.5 times.66 Likewise, Donghui Jing and collaborators evaluated growth kinetics of h-MSC in a 3 L single-use, stirred-tank bioreactor by using different concentrations of lactic acid, dO2, and pH.56 Results showed that minor concentrations of lactic acid at 1.1 g/L were favorable to promote cell growth. They obtained cell values of 60 × 104 cells for 0 g/L of lactic acid, 70 × 104 cells for 1.1 g/L, and 30 × 104 cells for 1.6 g/L. They noticed that larger concentrations of lactic acid inhibit h-MSC growth. Similarly, pH between 7 and 7.5 was advantageous to promote cell proliferation as compared to low pH (< 6.8) as previously reported by Lawson and colleagues.66 A dO2 concentration between 5 and 10% was found superior to 10% for cell growth.56
Influence of Operational Parameters in Bioreactors
In addition to cell culture conditions, shear stress generated by a fluid flow can also impact cell proliferation response in a biorector.139 Teng Ma and collaborators grew h-MSC in a perfusion bioreactor system to examine the effect of fluid flow. Two flow rates (0.1 and 1.5 mL/min) were examined on h-MSC growth. Results showed that significant (p < 0.05) enhancement in the total amount of cells produced were obtained using a low flow rate139 suggesting that low shear stress is best for h-MSC cultures.
On the other hand, the capacity of cell expansion has been tested by using different cell culture technologies. Kamilla Swiecha and her team studied the stimulus capacity of different bioreactor designs on h-MSC production from 3 different donors.85 They evaluated a multi-layer vessel (ML), a stirred tank bioreactor with microcarriers (STR), a hollow fiber bioreactor (HF), and a packed-bed bioreactor (PB). Results demonstrated that bioreactor designs can offer a positive or negative stimulus for cell expansion. Notably, poor cell expansion was obtained in HF (1 × 104 cells/cm2 for 5 days), while STR (4.5 × 104 cells/cm2 for 7 days), ML (4.25 × 104 cells/cm2 for 6 days) and PB (3.4 × 104 cells/cm2 for 7 days) achieved an analogous level of production with high density expansion.85
Microcarriers have been demonstrated to be a useful support matrix to promote cell growth in bioreactors.5,18,33,56,61,106 For this reason, many researchers have focused on studying the effect on h-MSC production. Andrew Ball and colleagues evaluated diverse microcarrier types to measure their ability to support h-MSC growth including cytodex 1, cytodex 3, fact III, collagen, plastic, plastic plus, proecntin F, and hillex in suspension in a single-use bioreactor.61 Their findings showed that only cytodex 1, cytodex 3, collagen, and hillex produced a robust growth.61 Similarly, Françoise De Longueville and his team studied h-MSC growth profiles in BioBLU 0.3c Single-Use Vessel used in suspension with cytodex 1 and cytodex 3 microcarriers.33 Their results revealed that cytodex 1 promoted cell expansion demonstrating a yield of approximately 42 × 104 cells/mL compared with 15 × 104 cells/mL using cytodex 3 for 10 culture days.33 Other authors also have studied the effect of microcarrier concentration on h-MSC expansion,18,56,106 reporting that h-MSC expansion is dependent on the amount of microcarriers in the bioreactor. Studies by Allen Kuan-Liang Chen demonstrated that h-MSC cultured in spinner flasks at three different concentrations of cytodex 3 can generate distinct cell numbers.18 They examined microcarrier concentrations of 4, 8, and 12 mg/mL, and their results revealed that 8 mg/mL is the optimum concentration to achieve higher h-MSC propagation.18 Other studies have shown that the growth of h-MSC in spinner flasks with proecntin F microcarrier in suspension is more effective using a concentration of 10 g/L compared with 5, 7.5, and 15 g/L.106
In summary, the scaling up of h-MSC manufacturing can be controlled by changing the conditional parameters of the technology used (planar or 3D culture system), varying culture conditions, and using additives. Moreover, it is essential to highlight that for each type of bioreactor there is a different range of optimal working conditions. Thus, operating conditions should be explored in future research to standardize cell culture conditions and operational parameters for each type of bioreactor.
Making Sustainable Banks for the Future
Banking is required to help meet the global demand of the large number of cells required to cover the health industry. In 2011, Cooper and Viswanathan demonstrated that umbilical cord MSCs (UCMSCs) could maintain pluripotency, safety, and efficacy after a prolonged storage period. They tested 5 different samples each with different time points of 1, 6,12, 24 and 36 months and their results showed negligible differences between all the time points in cell count, viability (> 97%) and immunophenotype (> 98) analysis.23 Their research demonstrated that high-quality manufacturing conditions are essential for the future of cell banks development. Also, they indicate that UCMSCs collection procedure is more efficient than other types of h-MSC extraction procedures (e.g. bone marrow extraction which is an invasive and painful procedure),29 without ethical concerns and does not harm mothers nor newborns.22 To ensure quality and safety, the banking procedure is highly dependent on an optimum cryopreservation process to guarantee the long-term storage of cells. The significant factors affecting the cryopreservation process are: (1) optimal cryopreservation media, whether it is needed to use a low concentration of dimethyl sulfoxide (DMSO) or non-DMSO133 in the cryopreservation protocol and, (2) freezing temperature rate123 where controlled-rate freezers111 were developed, but there is a non-uniform temperature distribution. Following all those studies, Lechanteur’s group reported a clinical-grade large-scale expansion and bank of h-MSC during 8 years with 59 validated donors, 464 h-MSC aliquots or bags, and 6 clinical trials of h-MSC infusion. Making sustainable cell banks is time-consuming and challenging, with major challenges in developing a bank with GMP, relevant potency assay, and removing the use of DMSO.68
Importance of the Cell Donor
h-MSC studies generate considerable cell-to-cell variations because of the heterogeneity of cells between donors, tissue of origin and cell populations.80,82,83 Since donor health and age influence the optimal function of the h-MSC, donor-to donor variability represents an essential factor even when working with the same tissue source. Studies have shown that there are age-related effects on functional cells97 while others have shown no effects, even when they focused on osteoprogenitor cells from h-MSC. In 2003, Stenderup reported that age is only associated with a decrease in h-MSC proliferation level without affecting functionality.116 Baxter’s and Mareshi’s groups reported that h-MSC isolation and in vitro expansion from pediatric and adult donors generates negligible differences in cellular functionality except for proliferation rate, where cells from the youngest donor developed a higher growth rate, suggesting enhancement on standard cell expansion protocols for clinical use.7,76 Although there is an apparent effect of donor variability on h-MSC quality, very few studies have investigated the impact of physical and chemical cues with regards to donor variability. Researchers must validate their results with cells from different donors and sources.
h-MSC-based therapies are classified depending on the donor: allogeneic (cells from a healthy donor) or autologous (patient’s own cells).44 Allogeneic therapies currently represent the highest number of h-MSC products with marketing authorization, 9 products from 13 approved.59 The main manufacturing differences are the number of therapeutic doses in each batch and the number of patients treated, positioning allogeneic therapies as the preferred manufacturing process in the future.74 This shows the importance of generating better h-MSC expansion processes due to the required high demand. Current and projected demand does not meet the number of cell donors available.
Issues and Challenges on Good Manufacturing Practice of h-MSC
GMP for h-MSC production involves all the processes starting from the donor selection and continuing until the specific clinical application. Because of the extended process there are many potential sources of error. Hence, a relevant issue on GMP is related to the operational part of cell manufacturing that minimizes the steps prone to human error (i.e., contamination issues), which can affect the production and general assessment of cell potency and safety. For these reasons, process automation is implemented in cell manufacturing as a strategy to control process variables to minimize variability associated to manual handling.124 An example of automation in cell culture is a closed automated Quantum® cell expansion system.43,67,100 This system consists of a robust automated hollow fiber bioreactor system and it is used to eliminate manual cell culture processes such as feeding and harvesting.57 The system provides a constant and controlled environment to maintain an adequate feeding rate of cells, eliminating waste and exchanging gases until the process finishes.39,67,78 Chantal Lechanteur and her team demonstrated that the Quantum® device produces therapeutic h-MSC of high-quality standards.67 Cells showed excellent immunosuppressive and differentiation capacities, and this device performed an excellent scalable and reproducible production. The total cell yield was increased by approximately 12 times in 7 days. Although this automated technology has been proven advantageous for the manufacturing of h-MSC,43,67,84 still the amount of cells generated is not sufficient to support the high demand of h-MSC for clinical studies, which continues to increase from year to year.43 Thus, other strategies that further stimulate cell growth must be combined to increase total cell yields while retaining a high cell quality.
Another challenge of GMP is the expansion of h-MSC in xeno-free culture conditions. The use of xeno-free components minimizes the risks of transmitting unpredicted pathogens from cell-based products.108 As previously mentioned, researchers have begun to work with human blood-derived products to avoid the use of media supplemented with animal-derived products. Their results have demonstrated that human blood-derived products, such as h-PL or t-PRP, produce larger amounts of cells as compared to FBS or FCS.8,64,104,105 Expansion of h-MSCs can be achieved in xeno-free culture conditions, however, xeno-free culture does not necessarily guarantee production of high-quality h-MSCs. Novel technologies should be implemented in each phase of the manufacturing process to continuously assess cell quality and segregate those that do not meet the quality standard to eliminate cells not favorable for clinical applications. Markers of cell quality must be identified, and detection strategies for those markers must be placed. Lastly, manufacturing processes should take advantage of both physical and biochemical cues to enhance cell quality, potency, and clinical efficacy.
Ethics Factors of Manufacturing
Despite the promising therapeutic potential of h-MSC,129 the clinical application of h-MSCs raises some ethical and safety concerns. The un-predictive nature of h-MSC in response to external stimuli as well as the lack of methods to track and remove these cells after delivery have been the main point of discussion in the clinical field due to the potential long term safety implications.11,77,113 Within the context of cell manufacturing, one of the main challenges of h-MSC studies is the lack of scientific rigor.24 Published studies in basic science typically evaluate a limited amount of h-MSC sources and donors, and thereby do not account for donor-to-donor variability, interactions associated to the tissue source, and the potential implications of demographic data such as age, race, ethnicity, and gender. This issue impairs the generalizability of the study outcomes and could lead to unforeseen changes in cell behavior during the manufacturing process and post-cell delivery to patients, compromising cell potency and safety. This problem is further exacerbated by the lack of regulatory standards for both pre-clinical and clinical interventions using h-MSC. Thus, while standards for h-MSCs are developed by regulatory agencies,77 it is advisable for researchers to increase the scientific rigor of their studies as much as possible within the constraints of their budget and design their pre-clinical studies to meet or exceed the standards established for drug development.
Another safety concern in the cell manufacturing process is the use of animal-derived products in cell culture. The supplementation of animal-derived factors can contain pathogenic entities such as prions that can be passed to the cell and represents unknown/increased health risks. Several studies have moved towards xeno-free culture conditions,89 but such approaches are cost-prohibited for basic research and scale-up processes, decreasing the affordability of manufactured therapies. This challenge may be addressed through the design of synthetic substrates with added capabilities for intrinsic stimulation of cell adherence and growth in h-MSC cultures.
Conclusions
Researchers have explored different mechanisms involved in the manufacturing process in hopes of increasing the scale of the h-MSC expansion and production. Because of the implementation of biochemical, chemical, and physical stimulus during the cell culture, researchers have discovered clear correlations between their use and an increase in the cell’s productive properties. However, these discoveries have yet to be translated to larger scales relevant to the manufacturing process. The impact of culture conditions is relevant at larger scales, and other process considerations must be considered (such as reactor design, flow conditions, etc.) when translating these stimuli. There are many available alternatives to promote h-MSC expansion, enhance potency, and ultimately produce more clinically relevant cells. These alternatives include modification of cell culture substrate, the addition of cytokines or small molecules, or combination of both. However, the effect of these alternatives must be explored at larger scales. These processes still need optimization. Moreover, the community must develop standards in each step of the h-MSC manufacturing process for cell therapies from the isolation step to final infusion on the patients, to guarantee high therapeutic potential.
References
Aggarwal, S., and M. F. Pittenger. Human mesenchymal stem cells modulate allogeneic immune cell responses. Blood 105:1815–1822, 2005.
Ahn, H.-J., W.-J. Lee, K. Kwack, and Y. D. Kwon. FGF2 stimulates the proliferation of human mesenchymal stem cells through the transient activation of JNK signaling. FEBS Lett. 583:2922–2926, 2009.
Anderson, H. J., J. K. Sahoo, R. V. Ulijn, and M. J. Dalby. Mesenchymal stem cell fate: applying biomaterials for control of stem cell behavior. Front. Bioeng. Biotechnol. 4:38, 2016.
Ankrum, J. A., R. G. Dastidar, J. F. Ong, O. Levy, and J. M. Karp. Performance-enhanced mesenchymal stem cells via intracellular delivery of steroids. Sci. Rep. 4:4645, 2014.
Badenes, S. M., T. G. Fernandes, C. A. V. Rodrigues, M. M. Diogo, and J. M. S. Cabral. Microcarrier-based platforms for in vitro expansion and differentiation of human pluripotent stem cells in bioreactor culture systems. J. Biotechnol. 234:71–82, 2016.
Baker, B. M., B. Trappmann, W. Y. Wang, M. S. Sakar, I. L. Kim, V. B. Shenoy, J. A. Burdick, and C. S. Chen. Cell-mediated fibre recruitment drives extracellular matrix mechanosensing in engineered fibrillar microenvironments. Nat. Mater. 14:1262–1268, 2015.
Baxter, M. A., R. F. Wynn, S. N. Jowitt, J. E. Wraith, L. J. Fairbairn, and I. Bellantuono. Study of telomere length reveals rapid aging of human marrow stromal cells following in vitro expansion. Stem Cells 22:675–682, 2004.
Bieback, K., A. Hecker, A. Kocaömer, H. Lannert, K. Schallmoser, D. Strunk, and H. Klüter. Human alternatives to fetal bovine serum for the expansion of mesenchymal stromal cells from bone marrow. Stem Cells 27:2331–2341, 2009.
Bigildeev, A. E., E. A. Zezina, I. N. Shipounova, and N. J. Drize. Interleukin-1 beta enhances human multipotent mesenchymal stromal cell proliferative potential and their ability to maintain hematopoietic precursor cells. Cytokine 71:246–254, 2015.
Borsellino, N., M. Crescimanno, C. Flandina, V. Leonardi, L. Rausa, and N. D’Alessandro. Antiproliferative and chemomodulatory effects of interferon-gamma on doxorubicin-sensitive and -resistant tumor cell lines. Anticancer Drugs 4:265–272, 1993.
Bredenoord, A. L., H. Clevers, and J. A. Knoblich. Human tissues in a dish: the research and ethical implications of organoid technology. Science 355:eaaf9414, 2017.
Bronner, F., and M. C. Farach-Carson. Bone Formation. Berlin: Springer, 2004.
Bruder, S. P., N. Jaiswal, and S. E. Haynesworth. Growth kinetics, self-renewal, and the osteogenic potential of purified human mesenchymal stem cells during extensive subcultivation and following cryopreservation. J. Cell. Biochem. 64:278–294, 1997.
Burand, A. J., O. W. Gramlich, A. J. Brown, and J. A. Ankrum. Function of cryopreserved mesenchymal stromal cells with and without interferon-γ prelicensing is context dependent. Stem Cells 35:1437–1439, 2017.
Castilla-Casadiego, D. A., J. R. García, A. J. García, and J. Almodovar. Heparin/collagen coatings improve human mesenchymal stromal cell response to interferon gamma. ACS Biomater. Sci. Eng. 5:2793–2803, 2019.
Chabay, R. W., and B. A. Sherwood. Matter and Interactions (4th ed.). New York: Wiley Global Education, 2015.
Chase, L. G., U. Lakshmipathy, L. A. Solchaga, M. S. Rao, and M. C. Vemuri. A novel serum-free medium for the expansion of human mesenchymal stem cells. Stem Cell Res. Ther. 1:8, 2010.
Chen, A. K.-L., Y. K. Chew, H. Y. Tan, S. Reuveny, and S. K. W. Oh. Increasing efficiency of human mesenchymal stromal cell culture by optimization of microcarrier concentration and design of medium feed. Cytotherapy 17:163–173, 2015.
Chinnadurai, R., D. Rajan, M. Qayed, D. Arafat, M. Garcia, Y. Liu, S. Kugathasan, L. J. Anderson, G. Gibson, and J. Galipeau. Potency analysis of mesenchymal stromal cells using a combinatorial assay matrix approach. Cell Rep. 22:2504–2517, 2018.
Choi, J. H., S. Y. Lyu, H. J. Lee, J. Jung, W. B. Park, and G. J. Kim. Korean mistletoe lectin regulates self-renewal of placenta-derived mesenchymal stem cells via autophagic mechanisms. Cell Prolif. 45:420–429, 2012.
Collins, J. M., P. H. Goldspink, and B. Russell. Migration and proliferation of human mesenchymal stem cells is stimulated by different regions of the mechano-growth factor prohormone. J. Mol. Cell. Cardiol. 49:1042–1045, 2010.
Cooper, K., A. SenMajumdar, and C. Viswanathan. Derivation, expansion and characterization of clinical grade mesenchymal stem cells from umbilical cord matrix using cord blood serum. Int. J. Stem. Cells 3:119–128, 2010.
Cooper, K., and C. Viswanathan. Establishment of a mesenchymal stem cell bank. Stem Cells Int. 2011:905621, 2011.
Cote, D. J., A. L. Bredenoord, T. R. Smith, M. Ammirati, J. Brennum, I. Mendez, A. S. Ammar, N. Balak, G. Bolles, I. N. Esene, T. Mathiesen, and M. L. Broekman. Ethical clinical translation of stem cell interventions for neurologic disease. Neurology 88:322–328, 2017.
Croitoru-Lamoury, J., F. M. J. Lamoury, M. Caristo, K. Suzuki, D. Walker, O. Takikawa, R. Taylor, and B. J. Brew. Interferon-γ regulates the proliferation and differentiation of mesenchymal stem cells via activation of indoleamine 2,3 dioxygenase (IDO). PLoS ONE 6:e14698, 2011.
Curran, J. M., R. Chen, and J. A. Hunt. Controlling the phenotype and function of mesenchymal stem cells in vitro by adhesion to silane-modified clean glass surfaces. Biomaterials 26:7057–7067, 2005.
Curran, J. M., R. Chen, and J. A. Hunt. The guidance of human mesenchymal stem cell differentiation in vitro by controlled modifications to the cell substrate. Biomaterials 27:4783–4793, 2006.
Curran, J. M., R. Stokes, E. Irvine, D. Graham, N. A. Amro, R. G. Sanedrin, H. Jamil, and J. A. Hunt. Introducing dip pen nanolithography as a tool for controlling stem cell behaviour: unlocking the potential of the next generation of smart materials in regenerative medicine. Lab Chip 10:1662–1670, 2010.
D’Ippolito, G., P. C. Schiller, C. Ricordi, B. A. Roos, and G. A. Howard. Age-related osteogenic potential of mesenchymal stromal stem cells from human vertebral bone marrow. J. Bone Miner. Res. 14:1115–1122, 1999.
Discher, D. E., D. J. Mooney, and P. W. Zandstra. Growth factors, matrices, and forces combine and control stem cells. Science 324:1673–1677, 2009.
Dolley-Sonneville, P. J., L. E. Romeo, and Z. K. Melkoumian. Synthetic surface for expansion of human mesenchymal stem cells in xeno-free, chemically defined culture conditions. PLoS ONE 8:e70263, 2013.
Dombrowski, C., T. Helledie, L. Ling, M. Grünert, C. A. Canning, C. Michael Jones, J. H. Hui, V. Nurcombe, A. J. van Wijnen, and S. M. Cool. FGFR1 signaling stimulates proliferation of human mesenchymal stem cells by inhibiting the cyclin-dependent kinase inhibitors p21Waf1and p27Kip1. Stem Cells 31:2724–2736, 2013.
Dufey, V., A. Tacheny, M. Art, U. Becken, and F. De Longueville. Expansion of human bone marrow-derived mesenchymal stem cells in BioBLU 0.3 c single-use bioreactors. Appl. Note 305:1–8, 2016.
Egea, V., L. von Baumgarten, C. Schichor, B. Berninger, T. Popp, P. Neth, R. Goldbrunner, Y. Kienast, F. Winkler, M. Jochum, and C. Ries. TNF-α respecifies human mesenchymal stem cells to a neural fate and promotes migration toward experimental glioma. Cell Death Differ. 18:853–863, 2011.
Eibes, G., F. dos Santos, P. Z. Andrade, J. S. Boura, M. M. A. Abecasis, C. L. da Silva, and J. M. S. Cabral. Maximizing the ex vivo expansion of human mesenchymal stem cells using a microcarrier-based stirred culture system. J. Biotechnol. 146:194–197, 2010.
Engler, A. J., S. Sen, H. L. Sweeney, and D. E. Discher. Matrix elasticity directs stem cell lineage specification. Cell 126:677–689, 2006.
Fan, W., R. Crawford, and Y. Xiao. The ratio of VEGF/PEDF expression in bone marrow mesenchymal stem cells regulates neovascularization. Differentiation 81:181–191, 2011.
Fiedler, J., F. Leucht, J. Waltenberger, C. Dehio, and R. E. Brenner. VEGF-A and PlGF-1 stimulate chemotactic migration of human mesenchymal progenitor cells. Biochem. Biophys. Res. Commun. 334:561–568, 2005.
Frank, N. D., M. E. Jones, B. Vang, and C. Coeshott. Evaluation of reagents used to coat the hollow-fiber bioreactor membrane of the Quantum® Cell Expansion System for the culture of human mesenchymal stem cells. Mater. Sci. Eng. C Mater. Biol. Appl. 96:77–85, 2019.
Gilbert, P. M., K. L. Havenstrite, K. E. G. Magnusson, A. Sacco, N. A. Leonardi, P. Kraft, N. K. Nguyen, S. Thrun, M. P. Lutolf, and H. M. Blau. Substrate elasticity regulates skeletal muscle stem cell self-renewal in culture. Science 329:1078–1081, 2010.
Goedhart, M., A. S. Cornelissen, C. Kuijk, S. Geerman, M. Kleijer, J. D. van Buul, S. Huveneers, M. H. G. P. Raaijmakers, H. A. Young, M. C. Wolkers, C. Voermans, and M. A. Nolte. Interferon-gamma impairs maintenance and alters hematopoietic support of bone marrow mesenchymal stromal cells. Stem Cells Dev. 27:579–589, 2018.
Guilak, F., D. M. Cohen, B. T. Estes, J. M. Gimble, W. Liedtke, and C. S. Chen. Control of stem cell fate by physical interactions with the extracellular matrix. Cell Stem Cell 5:17–26, 2009.
Hanley, P. J., Z. Mei, A. G. Durett, M. da Graca Cabreira-Hansen, M. Klis, W. Li, Y. Zhao, B. Yang, K. Parsha, O. Mir, F. Vahidy, D. Bloom, R. B. Rice, P. Hematti, S. I. Savitz, and A. P. Gee. Efficient manufacturing of therapeutic mesenchymal stromal cells with the use of the Quantum Cell Expansion System. Cytotherapy 16:1048–1058, 2014.
Heathman, T. R. J., A. W. Nienow, M. J. McCall, K. Coopman, B. Kara, and C. J. Hewitt. The translation of cell-based therapies: clinical landscape and manufacturing challenges. Regener. Med. 10:49–64, 2015.
Heathman, T. R. J., A. Stolzing, C. Fabian, Q. A. Rafiq, K. Coopman, A. W. Nienow, B. Kara, and C. J. Hewitt. Scalability and process transfer of mesenchymal stromal cell production from monolayer to microcarrier culture using human platelet lysate. Cytotherapy 18:523–535, 2016.
Heo, S.-J., N. L. Nerurkar, B. M. Baker, J.-W. Shin, D. M. Elliott, and R. L. Mauck. Fiber stretch and reorientation modulates mesenchymal stem cell morphology and fibrous gene expression on oriented nanofibrous microenvironments. Ann. Biomed. Eng. 39:2780–2790, 2011.
Heo, S.-J., S. E. Szczesny, D. H. Kim, K. S. Saleh, and R. L. Mauck. Expansion of mesenchymal stem cells on electrospun scaffolds maintains stemness, mechano-responsivity, and differentiation potential. J. Orthop. Res. 36:808–815, 2018.
Ho, S. S., N. L. Vollmer, M. I. Refaat, O. Jeon, E. Alsberg, M. A. Lee, and J. Kent Leach. Bone morphogenetic protein-2 promotes human mesenchymal stem cell survival and resultant bone formation when entrapped in photocrosslinked alginate hydrogels. Adv. Healthc. Mater. 5:2501–2509, 2016.
Hoffman, M. D., M. Takahata, and D. S. M. Benoit. 6-Bromoindirubin-3′-oxime (BIO) induces proliferation of human mesenchymal stem cells (hMSCs). In: 2011 IEEE 37th Annual Northeast Bioengineering Conference (NEBEC), 2011.
Huang, H., H. J. Kim, E.-J. Chang, Z. H. Lee, S. J. Hwang, H.-M. Kim, Y. Lee, and H.-H. Kim. IL-17 stimulates the proliferation and differentiation of human mesenchymal stem cells: implications for bone remodeling. Cell Death Differ. 16:1332–1343, 2009.
Ijzermans, J. N. M., and R. L. Marquet. Interferon-gamma: a Review. Immunobiology 179:456–473, 1989.
Ingber, D. E. Mechanical control of tissue growth: function follows form. Proc Natl Acad Sci USA 102:11571–11572, 2005.
Ito, T., R. Sawada, Y. Fujiwara, Y. Seyama, and T. Tsuchiya. FGF-2 suppresses cellular senescence of human mesenchymal stem cells by down-regulation of TGF-β2. Biochem. Biophys. Res. Commun 359:108–114, 2007.
Ito, T., R. Sawada, Y. Fujiwara, and T. Tsuchiya. FGF-2 increases osteogenic and chondrogenic differentiation potentials of human mesenchymal stem cells by inactivation of TGF-beta signaling. Cytotechnology 56:1–7, 2008.
Jiang, C. M., J. Liu, J. Y. Zhao, L. Xiao, S. An, Y. C. Gou, H. X. Quan, Q. Cheng, Y. L. Zhang, W. He, Y. T. Wang, W. J. Yu, Y. F. Huang, Y. T. Yi, Y. Chen, and J. Wang. Effects of hypoxia on the immunomodulatory properties of human gingiva-derived mesenchymal stem cells. J. Dent. Res. 94:69–77, 2015.
Jing, D., N. Sunil, S. Punreddy, M. Aysola, D. Kehoe, J. Murrel, M. Rook, and K. Niss. Growth kinetics of human mesenchymal stem cells in a 3-L single-use, stirred-tank bioreactor. BioPharm Int. 26:28–38, 2013.
Jones, M., M. Varella-Garcia, M. Skokan, S. Bryce, J. Schowinsky, R. Peters, B. Vang, M. Brecheisen, T. Startz, N. Frank, and B. Nankervis. Genetic stability of bone marrow-derived human mesenchymal stromal cells in the Quantum System. Cytotherapy 15:1323–1339, 2013.
Jossen, V., R. Pörtner, S. C. Kaiser, M. Kraume, D. Eibl, and R. Eibl. Mass production of mesenchymal stem cells—impact of bioreactor design and flow conditions on proliferation and differentiation. Cells Biomater. Regener. Med. 2014. https://doi.org/10.5772/59385.
Jossen, V., C. van den Bos, R. Eibl, and D. Eibl. Manufacturing human mesenchymal stem cells at clinical scale: process and regulatory challenges. Appl. Microbiol. Biotechnol. 102:3981–3994, 2018.
Jung, S., A. Sen, L. Rosenberg, and L. A. Behie. Identification of growth and attachment factors for the serum-free isolation and expansion of human mesenchymal stromal cells. Cytotherapy 12:637–657, 2010.
Kehoe, D., A. Schnitzler, J. Simler, A. DiLeo, and A. Ball. Scale-up of human mesenchymal stem cells on microcarriers in suspension in a single-use bioreactor. BioPharm Int. 25:28–38, 2012.
Kim, D. S., I. K. Jang, M. W. Lee, Y. J. Ko, D.-H. Lee, J. W. Lee, K. W. Sung, H. H. Koo, and K. H. Yoo. Enhanced immunosuppressive properties of human mesenchymal stem cells primed by interferon-γ. EBioMedicine 28:261–273, 2018.
Klinker, M. W., R. A. Marklein, J. L. Lo Surdo, C.-H. Wei, and S. R. Bauer. Morphological features of IFN-γ–stimulated mesenchymal stromal cells predict overall immunosuppressive capacity. Proc Natl Acad Sci 114:E2598–E2607, 2017.
Kocaoemer, A., S. Kern, H. Klüter, and K. Bieback. Human AB serum and thrombin-activated platelet-rich plasma are suitable alternatives to fetal calf serum for the expansion of mesenchymal stem cells from adipose tissue. Stem Cells 25:1270–1278, 2007.
Kureel, S. K., P. Mogha, A. Khadpekar, V. Kumar, R. Joshi, S. Das, J. Bellare, and A. Majumder. Soft substrate maintains proliferative and adipogenic differentiation potential of human mesenchymal stem cells on long-term expansion by delaying senescence. Biology Open 8:bio039453, 2019.
Lawson, T., D. E. Kehoe, A. C. Schnitzler, P. J. Rapiejko, K. A. Der, K. Philbrick, S. Punreddy, S. Rigby, R. Smith, Q. Feng, J. R. Murrell, and M. S. Rook. Process development for expansion of human mesenchymal stromal cells in a 50 L single-use stirred tank bioreactor. Biochem. Eng. J. 120:49–62, 2017.
Lechanteur, C. Large-scale clinical expansion of mesenchymal stem cells in the GMP-compliant, closed automated quantum® cell expansion system: comparison with expansion in traditional T-flasks. Int. J. Stem Cell Res. Ther. 4:1000222, 2014.
Lechanteur, C., A. Briquet, O. Giet, O. Delloye, E. Baudoux, and Y. Beguin. Clinical-scale expansion of mesenchymal stromal cells: a large banking experience. J. Transl. Med. 14:145, 2016.
Lee, J., A. A. Abdeen, A. S. Kim, and K. A. Kilian. Influence of biophysical parameters on maintaining the mesenchymal stem cell phenotype. ACS Biomater. Sci. Eng. 1:218–226, 2015.
Li, W.-J., C. T. Laurencin, E. J. Caterson, R. S. Tuan, and F. K. Ko. Electrospun nanofibrous structure: a novel scaffold for tissue engineering. J. Biomed. Mater. Res. 60:613–621, 2002.
Li, C. X., N. P. Talele, S. Boo, A. Koehler, E. Knee-Walden, J. L. Balestrini, P. Speight, A. Kapus, and B. Hinz. MicroRNA-21 preserves the fibrotic mechanical memory of mesenchymal stem cells. Nat. Mater. 16:379–389, 2017.
Litwack, G. Stem Cell Regulators. New York: Academic Press, 2011.
Maher, S., A. Romero-Weaver, A. Scarzello, and A. Gamero. Interferon: cellular executioner or white knight? Curr. Med. Chem. 14:1279–1289, 2007.
Malik, N. N., and M. B. Durdy. Cell therapy landscape. Transl. Regener. Med. 2015:87–106, 2015.
Mao, A. S., J.-W. Shin, and D. J. Mooney. Effects of substrate stiffness and cell-cell contact on mesenchymal stem cell differentiation. Biomaterials 98:184–191, 2016.
Mareschi, K., I. Ferrero, D. Rustichelli, S. Aschero, L. Gammaitoni, M. Aglietta, E. Madon, and F. Fagioli. Expansion of mesenchymal stem cells isolated from pediatric and adult donor bone marrow. J. Cell. Biochem. 97:744–754, 2006.
Marks, P., and S. Gottlieb. Balancing safety and innovation for cell-based regenerative medicine. N. Engl. J. Med. 378:954–959, 2018.
Martin-Manso, G., and P. J. Hanley. Using the quantum cell expansion system for the automated expansion of clinical-grade bone marrow-derived human mesenchymal stromal cells. Methods Mol. Biol. 1283:53–63, 2015.
McBeath, R., D. M. Pirone, C. M. Nelson, K. Bhadriraju, and C. S. Chen. Cell shape, cytoskeletal tension, and RhoA regulate stem cell lineage commitment. Dev. Cell 6:483–495, 2004.
McLeod, C. M., and R. L. Mauck. On the origin and impact of mesenchymal stem cell heterogeneity: new insights and emerging tools for single cell analysis. Eur. Cell. Mater. 34:217–231, 2017.
McMurray, R. J., N. Gadegaard, P. M. Tsimbouri, K. V. Burgess, L. E. McNamara, R. Tare, K. Murawski, E. Kingham, R. O. C. Oreffo, and M. J. Dalby. Nanoscale surfaces for the long-term maintenance of mesenchymal stem cell phenotype and multipotency. Nat. Mater. 10:637–644, 2011.
Mindaye, S. T., J. Lo Surdo, S. R. Bauer, and M. A. Alterman. The proteomic dataset for bone marrow derived human mesenchymal stromal cells: effect of in vitro passaging. Data Brief 5:864–870, 2015.
Mindaye, S. T., M. Ra, J. L. Lo Surdo, S. R. Bauer, and M. A. Alterman. Global proteomic signature of undifferentiated human bone marrow stromal cells: evidence for donor-to-donor proteome heterogeneity. Stem Cell Res. 11:793–805, 2013.
Mizukami, A., M. S. de Abreu Neto, F. Moreira, A. Fernandes-Platzgummer, Y.-F. Huang, W. Milligan, J. M. S. Cabral, C. L. da Silva, D. T. Covas, and K. Swiech. A fully-closed and automated hollow fiber bioreactor for clinical-grade manufacturing of human mesenchymal stem/stromal cells. Stem Cell Rev. 14:141–143, 2018.
Mizukami, A., T. D. Pereira Chilima, M. D. Orellana, M. A. Neto, D. T. Covas, S. S. Farid, and K. Swiech. Technologies for large-scale umbilical cord-derived MSC expansion: experimental performance and cost of goods analysis. Biochem. Eng. J. 135:36–48, 2018.
Müller, I., S. Kordowich, C. Holzwarth, C. Spano, G. Isensee, A. Staiber, S. Viebahn, F. Gieseke, H. Langer, M. P. Gawaz, E. M. Horwitz, P. Conte, R. Handgretinger, and M. Dominici. Animal serum-free culture conditions for isolation and expansion of multipotent mesenchymal stromal cells from human BM. Cytotherapy 8:437–444, 2006.
Ng, F., S. Boucher, S. Koh, K. S. R. Sastry, L. Chase, U. Lakshmipathy, C. Choong, Z. Yang, M. C. Vemuri, M. S. Rao, and V. Tanavde. PDGF, TGF-β, and FGF signaling is important for differentiation and growth of mesenchymal stem cells (MSCs): transcriptional profiling can identify markers and signaling pathways important in differentiation of MSCs into adipogenic, chondrogenic, and osteogenic lineages. Blood 112:295–307, 2008.
Oh, S., K. S. Brammer, Y. S. J. Li, D. Teng, A. J. Engler, S. Chien, and S. Jin. Stem cell fate dictated solely by altered nanotube dimension. Proc. Natl. Acad. Sci. USA 106:2130–2135, 2009.
Oikonomopoulos, A., W. K. van Deen, A.-R. Manansala, P. N. Lacey, T. A. Tomakili, A. Ziman, and D. W. Hommes. Optimization of human mesenchymal stem cell manufacturing: the effects of animal/xeno-free media. Sci. Rep. 5:16570, 2015.
Oka, N., A. Soeda, A. Inagaki, M. Onodera, H. Maruyama, A. Hara, T. Kunisada, H. Mori, and T. Iwama. VEGF promotes tumorigenesis and angiogenesis of human glioblastoma stem cells. Biochem. Biophys. Res. Commun. 360:553–559, 2007.
Olsen, T. R., K. S. Ng, L. T. Lock, T. Ahsan, and J. A. Rowley. Peak MSC—are we there yet? Front. Med. 5:178, 2018.
Pagnotto, M. R., Z. Wang, J. C. Karpie, M. Ferretti, X. Xiao, and C. R. Chu. Adeno-associated viral gene transfer of transforming growth factor-β1 to human mesenchymal stem cells improves cartilage repair. Gene Ther. 14:804, 2007.
Parandakh, A., A. Anbarlou, M. Tafazzoli-Shadpour, A. Ardeshirylajimi, and M.-M. Khani. Substrate topography interacts with substrate stiffness and culture time to regulate mechanical properties and smooth muscle differentiation of mesenchymal stem cells. Colloids Surf. B Biointerfaces 173:194–201, 2019.
Pittenger, M. F., A. M. Mackay, S. C. Beck, R. K. Jaiswal, R. Douglas, J. D. Mosca, M. A. Moorman, D. W. Simonetti, S. Craig, and D. R. Marshak. Multilineage potential of adult human mesenchymal stem cells. Science 284:143–147, 1999.
Ponte, A. L., T. Ribeiro-Fleury, V. Chabot, F. Gouilleux, A. Langonné, O. Hérault, P. Charbord, and J. Domenech. Granulocyte-colony-stimulating factor stimulation of bone marrow mesenchymal stromal cells promotes CD34 cell migration via a matrix metalloproteinase-2-dependent mechanism. Stem Cells Dev 21:3162–3172, 2012.
Prasanna, S. J., S. Jyothi Prasanna, D. Gopalakrishnan, S. R. Shankar, and A. B. Vasandan. Pro-inflammatory cytokines, IFNγ and TNFα, influence immune properties of human bone marrow and wharton jelly mesenchymal stem cells differentially. PLoS ONE 5:e9016, 2010.
Quarto, R., D. Thomas, and C. T. Liang. Bone progenitor cell deficits and the age-associated decline in bone repair capacity. Calcif. Tissue Int. 56:123–129, 1995.
Rifas, L. T-cell cytokine induction of BMP-2 regulates human mesenchymal stromal cell differentiation and mineralization. J. Cell. Biochem. 98:706–714, 2006.
Roemeling-van Rhijn, M., F. K. F. Mensah, S. S. Korevaar, M. J. Leijs, G. J. V. M. van Osch, J. N. M. Ijzermans, M. G. H. Betjes, C. C. Baan, W. Weimar, and M. J. Hoogduijn. Effects of hypoxia on the immunomodulatory properties of adipose tissue-derived mesenchymal stem cells. Front. Immunol. 4:203, 2013.
Russell, A. L., R. C. Lefavor, and A. C. Zubair. Characterization and cost-benefit analysis of automated bioreactor-expanded mesenchymal stem cells for clinical applications. Transfusion 58:2374–2382, 2018.
Ryan, J. M., F. Barry, J. M. Murphy, and B. P. Mahon. Interferon-γ does not break, but promotes the immunosuppressive capacity of adult human mesenchymal stem cells. Clin. Exp. Immunol. 149:353–363, 2007.
Salem, B., S. Miner, N. F. Hensel, M. Battiwalla, K. Keyvanfar, D. F. Stroncek, A. P. Gee, P. J. Hanley, C. M. Bollard, S. Ito, and A. John Barrett. Quantitative activation suppression assay to evaluate human bone marrow—derived mesenchymal stromal cell potency. Cytotherapy 17:1675–1686, 2015.
Saparov, A., V. Ogay, T. Nurgozhin, M. Jumabay, and W. C. W. Chen. Preconditioning of human mesenchymal stem cells to enhance their regulation of the immune response. Stem Cells Int. 2016:3924858, 2016.
Schallmoser, K., C. Bartmann, E. Rohde, A. Reinisch, K. Kashofer, E. Stadelmeyer, C. Drexler, G. Lanzer, W. Linkesch, and D. Strunk. Human platelet lysate can replace fetal bovine serum for clinical-scale expansion of functional mesenchymal stromal cells. Transfusion 47:1436–1446, 2007.
Schallmoser, K., E. Rohde, C. Bartmann, A. C. Obenauf, A. Reinisch, and D. Strunk. Platelet-derived growth factors for GMP-compliant propagation of mesenchymal stromal cells. Biomed. Mater. Eng. 19:271–276, 2009.
Schirmaier, C., V. Jossen, S. C. Kaiser, F. Jüngerkes, S. Brill, A. Safavi-Nab, A. Siehoff, C. van den Bos, D. Eibl, and R. Eibl. Scale-up of adipose tissue-derived mesenchymal stem cell production in stirred single-use bioreactors under low-serum conditions. Eng. Life Sci. 14:292–303, 2014.
Schmidt, A., D. Ladage, T. Schinköthe, U. Klausmann, C. Ulrichs, F.-J. Klinz, K. Brixius, S. Arnhold, B. Desai, U. Mehlhorn, R. H. G. Schwinger, P. Staib, K. Addicks, and W. Bloch. Basic fibroblast growth factor controls migration in human mesenchymal stem cells. Stem Cells 24:1750–1758, 2006.
Sensebé, L., M. Gadelorge, and S. Fleury-Cappellesso. Production of mesenchymal stromal/stem cells according to good manufacturing practices: a review. Stem Cell Res. Ther. 4:66, 2013.
Shao, Z., X. Zhang, Y. Pi, X. Wang, Z. Jia, J. Zhu, L. Dai, W. Chen, L. Yin, H. Chen, C. Zhou, and Y. Ao. Polycaprolactone electrospun mesh conjugated with an MSC affinity peptide for MSC homing in vivo. Biomaterials 33:3375–3387, 2012.
Shi, Y., Y. Wang, P. Zhang, and W. Liu. Fibrous scaffolds for tissue engineering Inflammation and Regeneration. Biomaterials 34:023–032, 2014.
Shu, Z., X. Kang, H. Chen, X. Zhou, J. Purtteman, D. Yadock, S. Heimfeld, and D. Gao. Development of a reliable low-cost controlled cooling rate instrument for the cryopreservation of hematopoietic stem cells. Cytotherapy 12:161–169, 2010.
Sivanathan, K. N., S. Gronthos, D. Rojas-Canales, B. Thierry, and P. T. Coates. Interferon-gamma modification of mesenchymal stem cells: implications of autologous and allogeneic mesenchymal stem cell therapy in allotransplantation. Stem Cell Rev. 10:351–375, 2014.
Sobel, M. E., and S. R. Wolman. Ethical considerations in the use of human tissues in research. Cytometry 38:192–193, 1999.
Sotiropoulou, P. A., S. A. Perez, M. Salagianni, C. N. Baxevanis, and M. Papamichail. Characterization of the optimal culture conditions for clinical scale production of human mesenchymal stem cells. Stem Cells 24:462–471, 2006.
Spoliti, M., P. Iudicone, R. Leone, A. De Rosa, F. R. Rossetti, and L. Pierelli. In vitro release and expansion of mesenchymal stem cells by a hyaluronic acid scaffold used in combination with bone marrow. Muscles Ligaments Tendons J. 2:289–294, 2012.
Stenderup, K., J. Justesen, C. Clausen, and M. Kassem. Aging is associated with decreased maximal life span and accelerated senescence of bone marrow stromal cells. Bone 33:919–926, 2003.
Strojny, C., M. Boyle, A. Bartholomew, P. Sundivakkam, and S. Alapati. Interferon gamma-treated dental pulp stem cells promote human mesenchymal stem cell migration in vitro. J. Endod. 41:1259–1264, 2015.
Studeny, M., F. C. Marini, R. E. Champlin, C. Zompetta, I. J. Fidler, and M. Andreeff. Bone marrow-derived mesenchymal stem cells as vehicles for interferon-beta delivery into tumors. Cancer Res. 62:3603–3608, 2002.
Su, N., P.-L. Gao, K. Wang, J.-Y. Wang, Y. Zhong, and Y. Luo. Fibrous scaffolds potentiate the paracrine function of mesenchymal stem cells: a new dimension in cell-material interaction. Biomaterials 141:74–85, 2017.
Talele, N. P., J. Fradette, J. E. Davies, A. Kapus, and B. Hinz. Expression of α-smooth muscle actin determines the fate of mesenchymal stromal cells. Stem Cell Rep. 4:1016–1030, 2015.
Tavassoli, H., S. N. Alhosseini, A. Tay, P. P. Y. Chan, S. K. W. Oh, and M. E. Warkiani. Large-scale production of stem cells utilizing microcarriers: a biomaterials engineering perspective from academic research to commercialized products. Biomaterials 181:333–346, 2018.
Teramura, Y., and H. Iwata. Cell surface modification with polymers for biomedical studies. Soft Matter 6:1081–1091, 2010.
Thirumala, S., S. Zvonic, E. Floyd, J. M. Gimble, and R. V. Devireddy. Effect of various freezing parameters on the immediate post-thaw membrane integrity of adipose tissue derived adult stem cells. Biotechnol. Prog. 21:1511–1524, 2005.
Thomas, R. J., A. D. Hope, P. Hourd, M. Baradez, E. A. Miljan, J. D. Sinden, and D. J. Williams. Automated, serum-free production of CTX0E03: a therapeutic clinical grade human neural stem cell line. Biotechnol. Lett. 31:1167–1172, 2009.
Tsutsumi, S., A. Shimazu, K. Miyazaki, H. Pan, C. Koike, E. Yoshida, K. Takagishi, and Y. Kato. Retention of multilineage differentiation potential of mesenchymal cells during proliferation in response to FGF. Biochem. Biophys. Res. Commun. 288:413–419, 2001.
Udalamaththa, V. L., C. D. Jayasinghe, and P. V. Udagama. Potential role of herbal remedies in stem cell therapy: proliferation and differentiation of human mesenchymal stromal cells. Stem Cell Res. Ther. 7:110, 2016.
Unger, C., H. Skottman, P. Blomberg, M. S. Dilber, and O. Hovatta. Good manufacturing practice and clinical-grade human embryonic stem cell lines. Hum. Mol. Genet. 17:R48–R53, 2008.
Valencic, E., E. Piscianz, M. Andolina, A. Ventura, and A. Tommasini. The immunosuppressive effect of Wharton’s jelly stromal cells depends on the timing of their licensing and on lymphocyte activation. Cytotherapy 12:154–160, 2010.
Volarevic, V., B. S. Markovic, M. Gazdic, A. Volarevic, N. Jovicic, N. Arsenijevic, L. Armstrong, V. Djonov, M. Lako, and M. Stojkovic. Ethical and safety issues of stem cell-based therapy. Int. J. Med. Sci. 15:36–45, 2018.
Wall, L., F. Burke, J. F. Smyth, and F. Balkwill. The anti-proliferative activity of interferon-γ on ovarian cancer: in vitro and in vivo. Gynecol Oncol 88:S149–S151, 2003.
Warrier, S. R., N. Haridas, S. Balasubramanian, A. Jalisatgi, R. Bhonde, and A. Dharmarajan. A synthetic formulation, Dhanwantharam kashaya, delays senescence in stem cells. Cell Prolif. 46:283–290, 2013.
Wehling, N., G. D. Palmer, C. Pilapil, F. Liu, J. W. Wells, P. E. Müller, C. H. Evans, and R. M. Porter. Interleukin-1β and tumor necrosis factor α inhibit chondrogenesis by human mesenchymal stem cells through NF-κB-dependent pathways. Arthritis Rheum. 60:801–812, 2009.
Windrum, P., T. C. M. Morris, M. B. Drake, D. Niederwieser, T. Ruutu, and EBMT Chronic Leukaemia Working Party Complications Subcommittee. Variation in dimethyl sulfoxide use in stem cell transplantation: a survey of EBMT centres. Bone Marrow Transpl. 36:601–603, 2005.
Wobma, H. M., M. A. Tamargo, S. Goeta, L. M. Brown, R. Duran-Struuck, and G. Vunjak-Novakovic. The influence of hypoxia and IFN-γ on the proteome and metabolome of therapeutic mesenchymal stem cells. Biomaterials 167:226–234, 2018.
Yang, C., M. W. Tibbitt, L. Basta, and K. S. Anseth. Mechanical memory and dosing influence stem cell fate. Nat. Mater. 13:645–652, 2014.
Yeung, T., P. C. Georges, L. A. Flanagan, B. Marg, M. Ortiz, M. Funaki, N. Zahir, W. Ming, V. Weaver, and P. A. Janmey. Effects of substrate stiffness on cell morphology, cytoskeletal structure, and adhesion. Cell Motil. Cytoskelet. 60:24–34, 2005.
Yim, E. K. F., and M. P. Sheetz. Force-dependent cell signaling in stem cell differentiation. Stem Cell Res. Ther. 3:41, 2012.
Yun, S. P., M. Y. Lee, J. M. Ryu, C. H. Song, and H. J. Han. Role of HIF-1α and VEGF in human mesenchymal stem cell proliferation by 17β-estradiol: involvement of PKC, PI3K/Akt, and MAPKs. Am. J. Physiol. Cell Physiol. 296:C317–C326, 2009.
Zhao, F., R. Chella, and T. Ma. Effects of shear stress on 3-D human mesenchymal stem cell construct development in a perfusion bioreactor system: experiments and hydrodynamic modeling. Biotechnol. Bioeng. 96:584–595, 2007.
Zhao, W., X. Li, X. Liu, N. Zhang, and X. Wen. Effects of substrate stiffness on adipogenic and osteogenic differentiation of human mesenchymal stem cells. Mater. Sci. Eng. C Mater. Biol. Appl. 40:316–323, 2014.
Zimmermann, J. A., M. H. Hettiaratchi, and T. C. McDevitt. Enhanced Immunosuppression of T cells by sustained presentation of bioactive interferon-γ within three-dimensional mesenchymal stem cell constructs. Stem Cells Transl. Med. 6:223–237, 2017.
Acknowledgments
This work was financially supported by the Engineering Research Center for Cell Manufacturing Technologies (CMaT) of the National Science Foundation under Grant No. EEC-1648035, and by the “Programa de Apoyo Institucional Para la Formación en Estudios de Posgrados en Maestrías y Doctorados de La Universidad del Atlántico, Colombia” by providing DCC a scholarship. Supported by PR-INBRE an Institutional Development Award (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health under Grant Number P20 GM103475.
Disclosure
The authors declare that no competing financial interests exist.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Stefan M. Duma oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Castilla-Casadiego, D.A., Reyes-Ramos, A.M., Domenech, M. et al. Effects of Physical, Chemical, and Biological Stimulus on h-MSC Expansion and Their Functional Characteristics. Ann Biomed Eng 48, 519–535 (2020). https://doi.org/10.1007/s10439-019-02400-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-019-02400-3